Module 3: Immunology
1/18
Earn XP
Description and Tags
Workbook Q&A CPAT3201
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
19 Terms
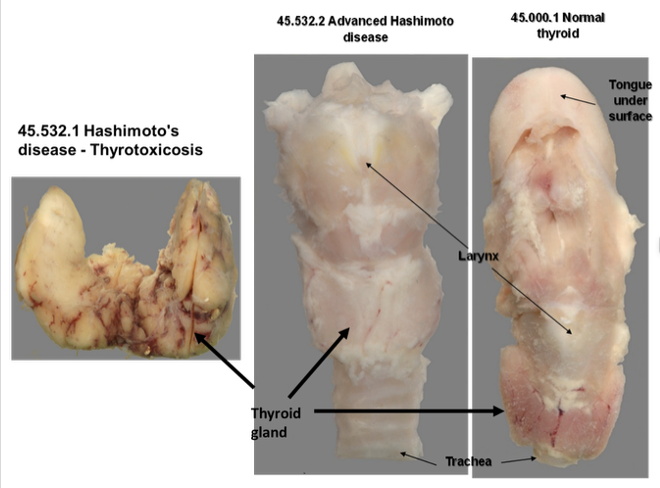
Describe the appearance of specimen 45.532.2, compared to the normal
The thyroid is markedly reduced in size, compared to the normal.
Note: During the early phase of Hashimoto’s disease (45.532.1), the thyroid gland is typically enlarged owing to the inflammatory response to autoantigens in the thyroid (i.e. thyroid peroxidase & thyroglobin) and an initial hypertrophy period to compensate for lack of responsiveness to TSH in producing T4 & T3. In the setting of advanced disease, immune-mediated destruction of the thyroid results atrophic thyroiditis - global reduction in size of the thyroid.
Are there any areas of obvious or specific abnormality?
The reduction in size is diffuse with no obvious abnormality.
This woman complained of an episode of several months where she suffered from palpitations and intolerance of heat 5-6 years ago. Why might this be? (Hashimoto thyroiditis)
Often the onset of Hashimoto disease is accompanied by an episode of thyrotoxicosis - a hypermetabolic state caused by elevated circulating levels of free T 3 and T 4 with diminished levels of TSH and decreased radioactive iodine uptake.
Two factors are thought to initial transient thyrotoxicosis in Hashimoto’s disease - hypertrophy of the thyroid due to immune-mediated disruption of thyroid follicles and death of thyrocytes releasing bursts of thyroid hormones into the bloodstream.
How are the mechanisms of Hashimoto’s disease different from that of Grave’s disease?
The autoimmune mechanisms are probably very similar. However the antibody products of the autoimmune reaction are, in the case of Grave?s disease, stimulatory and in the case of Hashimoto, blocking in function. In addition, the follicular cells in Hashimoto disease may be destroyed by the cytotoxic responses seen in this disease.
Is there a genetic disposition to Hashimoto’s disease? If so, in what way?
There is a genetic disposition to this autoimmune disease. In particular, studies from monozygotic twins implicate the Major Histocompatibility Complex (MHC) class II haplotypes, DR3 and DR5.
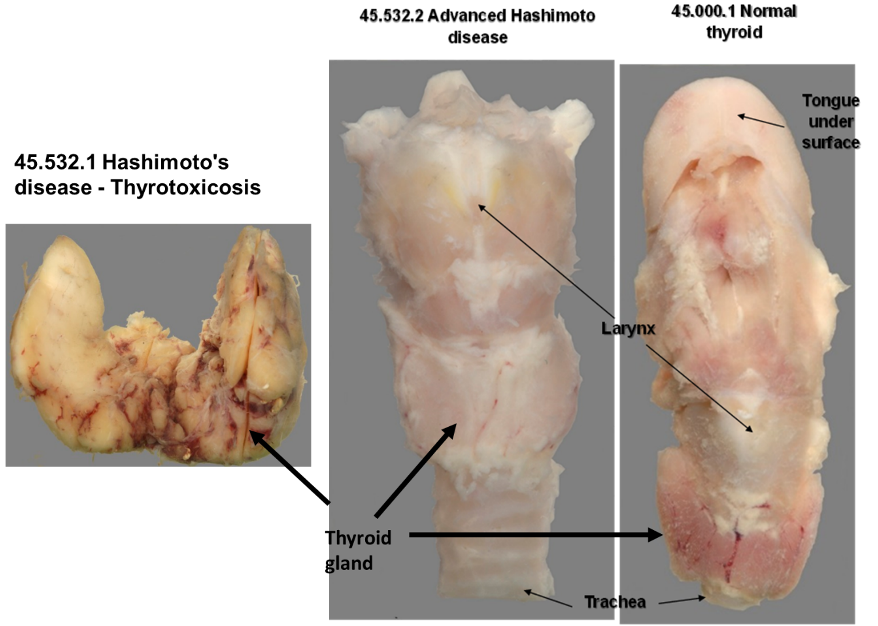
Describe the appearance of these specimens (Rheumatic fever) - Are there any areas of obvious or specific abnormality?
13.552.3: The mitral valve is extremely thickened (opaque) and calcified (normally the leaflets should be translucent and thin) and the thickened leaflets are fused, causing stenosis of the aperture. This would have caused a diastolic murmur in life. This valve was probably also incompetent (it could not close properly and would have leaked) and this would have caused a systolic murmur in life. The resistance to blood flow would have been the reason for the left ventricular hypertrophy also seen in this specimen. The endocardium shows some opacity, indicating thickening, due to the same process of disease.
13.552.5: In addition to thickening, fusing and calcification of the mitral valve causing stenosis, as seen in the previous specimen, the aortic valve is also thickened and calcified in this specimen. In addition, the chordae tendinae are thickened also (compared to the chordae on the right side). The tricuspid valve in this specimen is dilated and was probably incompetent, since it is clear that the leaflets of this valve do not meet in the centre. This would have caused a systolic murmur in life.
This man had an episode where blood and protein were detected in the urine. Why might this be? (Rheumatic fever)
Vegetations that frequently grow on the altered leaflets of the valves (mitral or aortic) on the left side of the heart can come loose and travel as emboli to any organs supplied by arteries. Sometime these emboli are infected. If an embolus is lodged in one of the small vessels of the kidney, the destruction of the tissue, due to tissue death (infarction) from the loss of blood supply, will result in some bleeding which will drain into the urine.
How is the pathogenesis of Rheumatic fever different from that of Rheumatoid Arthritis?
Rheumatic fever is associated with previous infection by group A Streptococcal organisms, while the initiating event causing Rheumatoid arthritis is unknown. However, both are autoimmune diseases.
What factors predispose people to Rheumatic fever?
Genetic predisposition, low socioeconomic status, crowded living conditions, throat infections with group A streptococcal organisms and poor access to health support (e.g., antibiotics for bacterial throat infections).

Describe the appearance of this specimen - are there any areas of obvious or specific abnormality?
99.554.2: The joint surface where the patella meets the femur is roughened and the area of joint interface is significantly reduced. The synovium has proliferated and encroached on the area of the joint surfaces. The synovium is rough and shaggy as a result of this proliferation. There is evidence of some bleeding into the joint itself - this can be inferred from the dark blue colour seen through the synovium around the joint.
What are the principal immunological mechanism(s) involved in the pathogenesis of Rheumatoid Arthritis?
Many theories exist as to the initiating events of this disease. They include cross-reactivity to virus infections in the immunological response to self. It is thought that individuals are genetically predisposed to this disease. What is clear is that there is both an innate and superimposed adapative immunological response and that citrullination of fibrin is a key factor which drives a DAMP-mediated immunological response from neutrophils and macrophages. The ongoing adaptive immune response in which neutrophils, lymphocytes (B and T cells) and macrophages are important mediators of inflammation and damage to self? i.e., this is autoimmunity. CD4+ve T cells are prominent. Various factors produced by the immune cells encourage breakdown of cartilage via increased levels of induced metalloproteinases and resorption of bone via increased activity of osteoclasts. The end-result is destruction of the joint surfaces and eventually the joint space.

In what way is the tissue in the section abnormal?
There are tissue projections in the synovium where there should be a flat surface. There are large numbers of inflammatory cells, including lymphocytes, macrophages, giant cells and neutrophils in the connective tissue where there should be none. There are larger numbers of blood vessels in the connective tissue than there should be. There should be no fibrin on the surface of the synovium

How does the appearance of the histology relate to the function of the joint in the clinical disease?
The proliferation of the synovial tissue inhibits joint movement physically by getting in the way of movement. The proliferating synovial tissue also invades the joint space and the joint surfaces and, with the inflammatory process, erodes the joint surfaces and the bone beneath it.
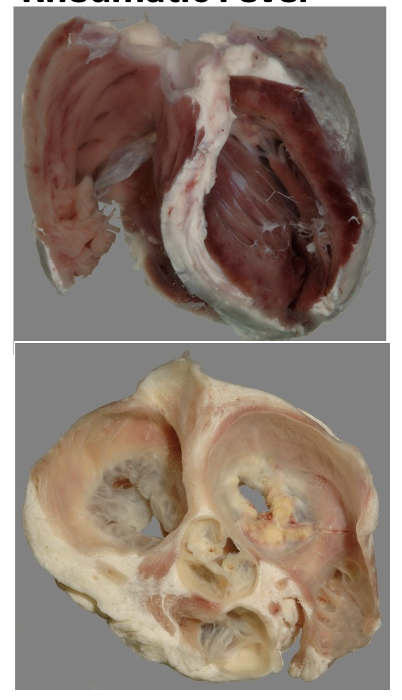
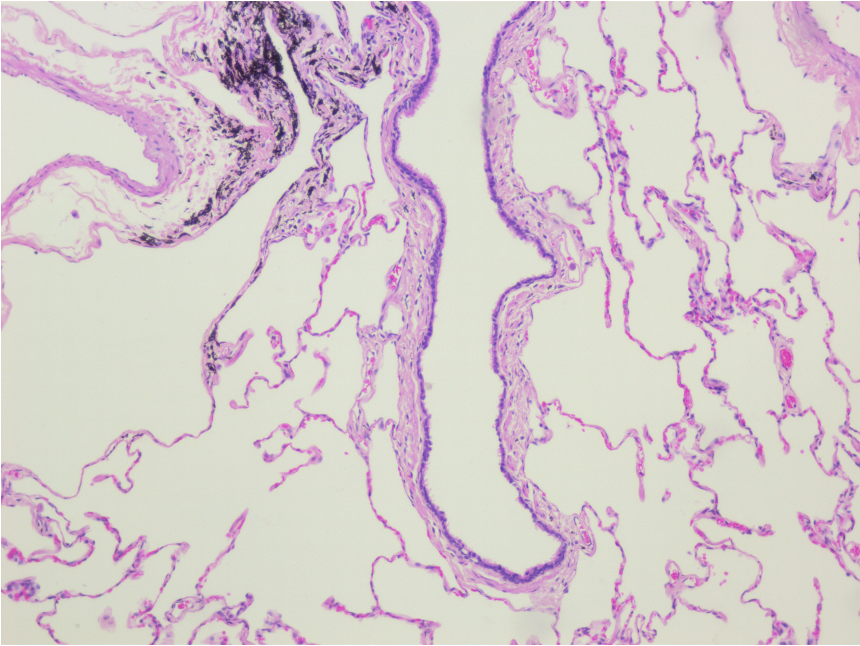
10x magnification of normal alveoli
10x magnification showing a bronchiole. How would you differentiate between a bronchus and a bronchiole?
By the presence of submucosa and cartilage rings in the cross section
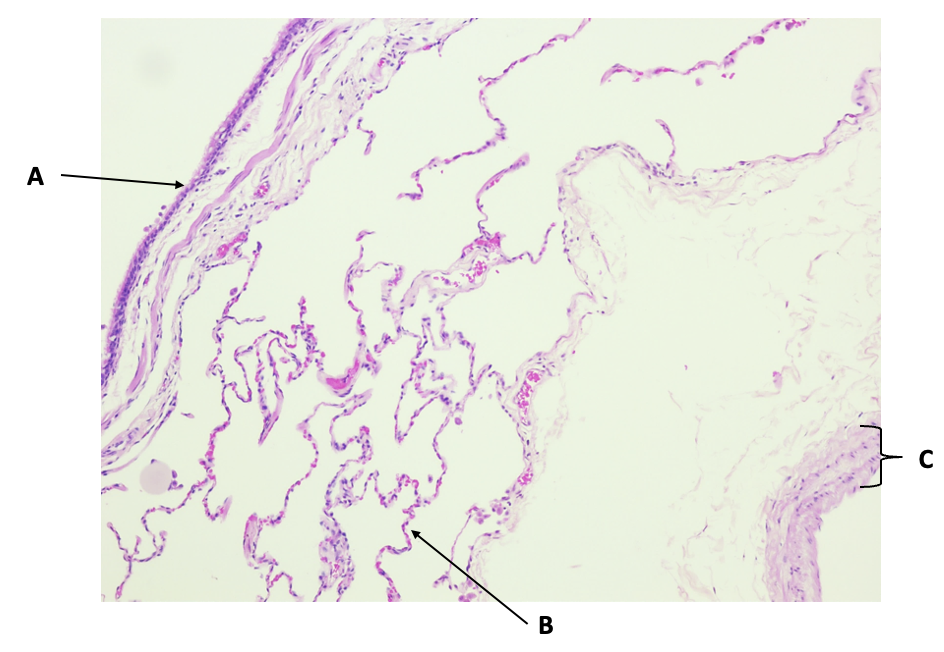
Annotate the features of a normal lung
A. Bronchiolar wall
B. Alveolar wall
C. Blood vessel wall
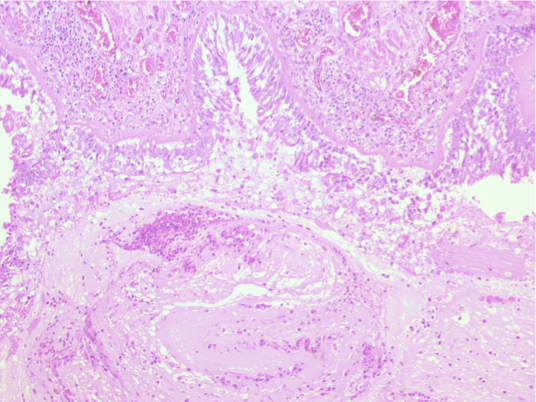
Insert at 10x magnification: section of asthmatic bronchi showing epithelium that has been sloughed off and a mucus plug in the lumen. Label the basement membrane, epithelium, mucus plug and inflammatory cells in the mucus.
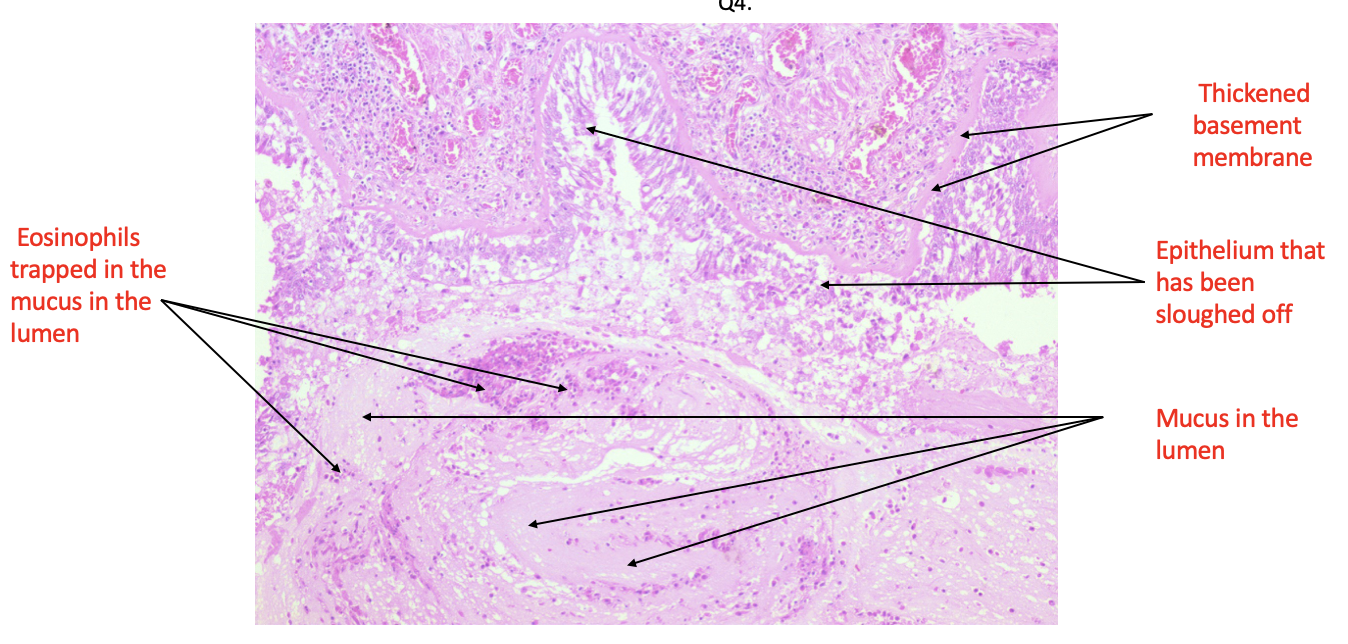
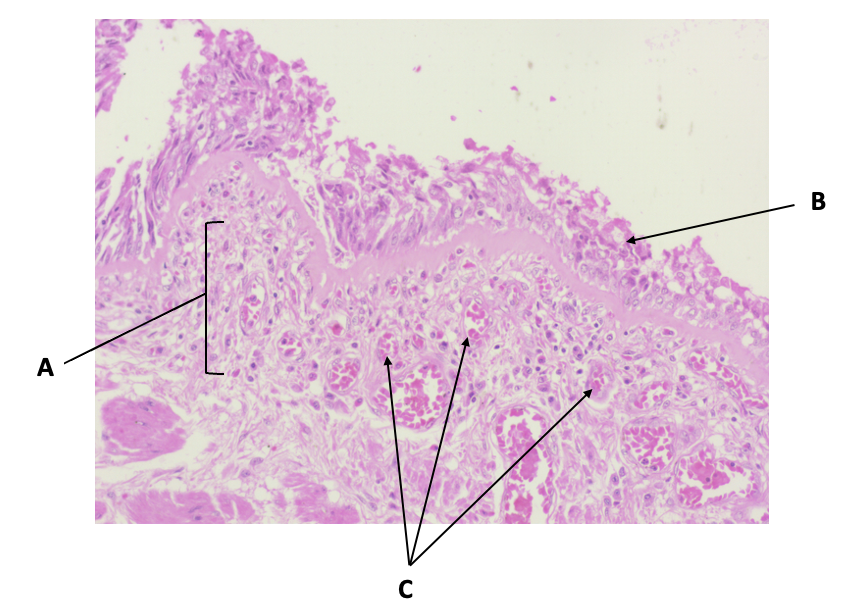
Annotate the section of an asthmatic lung with reference to its appearance compared to a normal lung
A. Inflammatory/immune cell infiltration (eosinophils, B cells)
B. Epithelium being sloughed off
C. Increased blood vessels (neovascularisation)

Section of asthmatic lung at low magnification: annotate and describe the following features
A. Muscularis mucosae (hypertrophy and hyperplasia)
B. Serous part of the acinus (component of submucous glands)
C. Mucus part of the acinus (component of submucous glands)
D. Lumen