Meg/Surg: CJMM, Pain, sleep, infection, fluids/electrolytes
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
25 Terms
Airborne Precautions
Private room
required with monitored negative airflow (with appropriate number of air exchanges and air discharge to outside or through N95 mask [HEPA filter]); keep door(s) closed
Special respiratory protection:
• Wear PAPR for known or suspected TB
• Susceptible people not to enter room of patient with known or suspected measles or varicella unless immune caregivers are not available
• Susceptible people who must enter room must wear PAPR or N95 mask (HEPA filter a )
Transport:
Patient to leave room only for essential clinical reasons, wearing surgical mask
![<p>Private room </p><ul><li><p>required with monitored negative airflow (with appropriate number of air exchanges and air discharge to outside or through N95 mask [HEPA filter]); keep door(s) closed</p></li></ul><p></p><p>Special respiratory protection:</p><p>• Wear PAPR for known or suspected TB</p><p>• Susceptible people not to enter room of patient with known or suspected measles or varicella unless immune caregivers are not available</p><p>• Susceptible people who must enter room must wear PAPR or N95 mask (HEPA filter a )</p><p></p><p>Transport: </p><ul><li><p>Patient to leave room only for essential clinical reasons, wearing surgical mask</p></li></ul><p></p>](https://knowt-user-attachments.s3.amazonaws.com/1ed687db-6d15-4c2e-bba6-e63832f75a06.png)
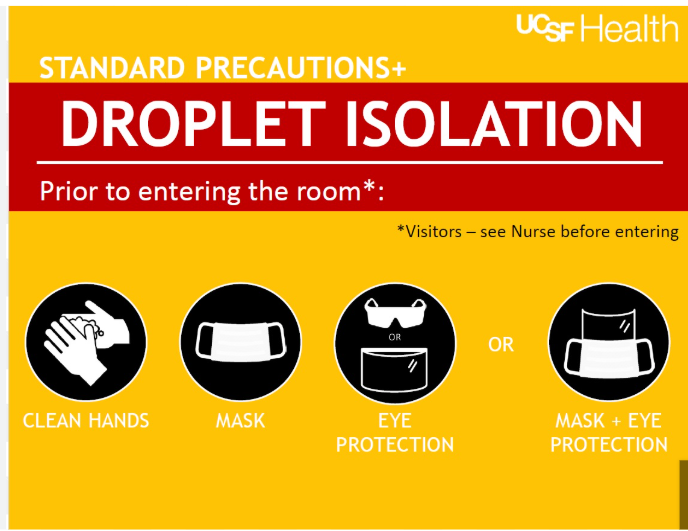
Droplet Precautions
Private room preferred
if not available, may cohort with patient with same active infection with same microorganisms if no other infection present; maintain distance of at least 3 feet from other patients if private room not available
Mask
Required when working within 3–6 feet of patient
Transport
Same as for Airborne Precautions
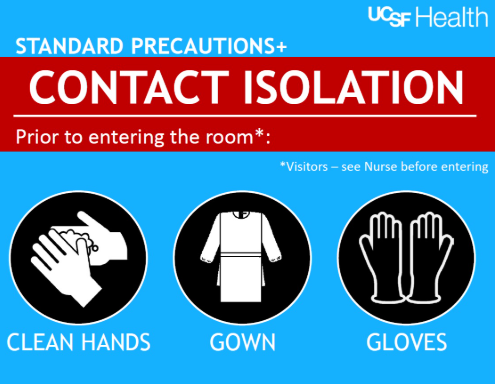
Contact Precautions
Private room preferred
if not available, may cohort with patient with same active infection with same microorganisms if no other infection present
PPE
Wear gloves when entering room
Wash hands with antimicrobial soap before leaving patient’s room
Wear gown to prevent contact with patient or contaminated items or if patient has uncontrolled body fluids; remove gown before leaving room
Transport
Patient to leave room only for essential clinical reasons; during transport, use needed precautions to prevent disease transmission
Dedicated equipment for this patient only
(or disinfect after use before taking from room)
concept: infection
Defined
Categories of Infection
Sepsis
Common Risk Factors for Infection
Physiologic Consequences of Infection:
Localized infection:
systemic infection:
Assessment of Infection
Health Promotion Strategies to Prevent Infection
Interventions to Manage Patients With Infection
Defined:
the invasion of pathogens (harmful microbes) into the body that multiply and cause disease or illness. The primary interrelated concepts are pain, immunity, inflammation, and tissue integrity.
Classification of Infection:
an be classified by type of microorganism, by extent of its spread throughout the body, or by the length of time that the infection exists, acute or chronic, localized (one area) or systemic (whole body, can lead to sepsis).
• Bacteria
• Viruses
• Fungi
• Parasites or protozoa
Sepsis:
is a life-threatening condition that occurs when the body's immune system overreacts to an infection, leading to widespread inflammation and organ damage
Common Risk Factors for Infection:
• immunocompromised individuals
• Have chronic illnesses (comorbidities)
• Are of advanced age: because immune function declines as part of normal aging
• Are very overweight or obese
• Live in a crowded or unsanitary environment
• Ingest contaminated food or water
• Have impaired tissue integrity: (causing an interruption in the body’s first line of defense against infection)
• Are exposed to individuals who have highly contagious infections: such as influenza or tuberculosis
• Experience continuous or frequent stress
Physiologic Consequences of Infection:
depend on whether it is localized or systemic.
Localized infection:
typically causes inflammation: Signs and symptoms of inflammation include redness/hyperpigmentation, warmth, pain, and swelling.
If localized infection is not treated or does not respond to treatment, it may spread and affect the entire body, causing a systemic infection
systemic infection:
affects the entire body, the response of the body is also systemic.
fever and an increased white blood cell count (WBC), also known as leukocytosis.
If the infection is not treated or does not respond to treatment, the patient may become septic and experience decreased perfusion, causing hypotension and eventually organ failure (septic shock).
Assessment of Infection:
take a thorough history to determine the patient’s risk for and exposure to infection.
Observe for signs and symptoms of local infection if visible, such as redness/hyperpigmentation, warmth, pain, and swelling.
Elevated temperature may be present in patients who have systemic infection.
Ask about changes in elimination, including urinary burning and urgency, diarrhea, and nausea/vomiting. These changes may be indications of urinary or GI system infection.
Monitor laboratory test results, including:
Elevated WBC count with differential (especially lymphocytes and neutrophils)
Increased erythrocyte sedimentation rate (ESR)
Increased C-reactive protein
Positive culture and sensitivity
Positive antigen testing for infectious agents
Health Promotion Strategies to Prevent Infection:
Health promotion related to infection may be categorized as primary and secondary prevention
Primary prevention includes measures to prevent infection, such as immunizations against common illnesses and boosters as needed
Secondary prevention involves screening for existing infection, such as when sexually transmitted infections (STIs) are suspected or the patient is at a high risk for STIs
Interventions to Manage Patients With Infection:
if infection not able to be self treated at home with rest fluids and OTC drugs:
• Antimicrobial drug therapy (type depends on type of pathogen)
• Increased fluids and electrolyte replacement
• Sufficient rest
• Adequate nutrition
concept: Pain
Definition of Pain
Categories of Pain
Common Risk Factors for Pain
Physiologic and Psychosocial Consequences of Pain
Assessment of Pain
Health Promotion Strategies to Prevent Pain
Interventions to Manage Patients With Pain
Patient education
Definition of Pain
Pain is generally defined as an unpleasant sensory and emotional experience.
Because pain is a subjective symptom, nurses and other health care professionals must respect the patient’s description of pain.
Categories of Pain
Pain can be categorized by duration as acute or persistent (chronic).
Acute pain is short-lived, temporary, and typically confined to an injured area of the body (localized). It serves a biologic purpose to activate the sympathetic nervous system and other physiologic responses.
Persistent (chronic) pain does not serve this purpose and tends to last more than 3 months. It is often described as diffuse and not confined to one area of the body. The two major types of persistent pain are persistent cancer pain and persistent noncancer pain
Pain can also be categorized by its underlying mechanism into nociceptive and neuropathic pain.
Nociceptive pain results from skin or organ damage or inflammation.
Neuropathic pain involves a set of mechanisms related to the nervous system with or without tissue damage
Common Risk Factors for Pain
Anyone is at risk for pain, and many adults have experienced one or more types of pain sometime in their lives.
Specific risk factors include individuals who experience acute trauma or have chronic diseases
Physiologic and Psychosocial Consequences of Pain
Patients experiencing acute pain usually have one or more sympathetic nervous system signs and symptoms including nausea, vomiting, diaphoresis (sweating), increased blood pressure, increased respiratory rate, increased pulse, and dilated pupils. Fight or flight!!!
This “flight or fight” reaction does not occur in patients with persistent pain. Persistent pain can cause psychosocial issues, including anxiety and depression.
Assessment of Pain: PQRST
P: what makes the pain worse and better
Q: describe the pain
R: where is the pain or point to the pain and does it spread
S: on a scale from 0-10 (0 being no pain, 10 being the worst pain imaginable)
T: How long does the pain last and low long they have been experiencing it
Health Promotion Strategies to Prevent Pain
Acute pain is often unavoidable.
Avoiding high-risk activities can help prevent trauma from accidental injury and thus prevent severe acute pain.
After surgery or a trauma event, acute pain must be well controlled to prevent persistent pain that may last for months or years.
Interventions to Manage Patients With Pain
Nursing and collaborative management of pain may be categorized by pharmacologic and nonpharmacologic interventions.
Evidence-based pharmacologic interventions involve a variety of analgesics and are determined on the basis of severity, type, and source of pain.
Analgesics may be divided into nonopioid drugs and opioid drugs.
Nonopioid drugs may be used without concern related to abuse or addiction; however, they have side and adverse effects that require careful monitoring.
Patient education
teach patients to take drug therapy for persistent pain on a continuous regimen basis for the best control.
Persistent cancer pain often requires opioids at the end of life to provide comfort and prepare for a “good death.”
Nonpharmacologic patient-centered interventions depend on the patient’s preferences.
Pure (Full) Opioid Agonists:
Bind mainly to mu receptors in the CNS → produce analgesia.
First-line opioids for moderate to severe nociceptive pain.
No dose ceiling → higher doses = more pain relief (dosing adjusted to pain severity).
Can cause euphoria, so they carry abuse potential, but abuse is rare when used correctly for pain.
Examples: morphine, fentanyl, hydromorphone, oxycodone, oxymorphone, hydrocodone.
Common Sources of Postoperative Infections:
Surgical Site: The most common source is the surgical incision itself. Contamination can occur during the operation from the patient's own skin flora, surgical instruments, or the operating room environment.
Urinary Tract: Catheterization during surgery and in the postoperative period can introduce bacteria, leading to a urinary tract infection (UTI).
Respiratory Tract: Patients may develop pneumonia due to atelectasis (collapsed lung tissue), immobility, or aspiration.
Intravenous (IV) Sites: IV catheters are a direct portal of entry for bacteria, leading to phlebitis or a bloodstream infection (sepsis).
Other Sources:
Implanted devices: Prosthetic joints, pacemakers, and other implanted devices can become colonized with bacteria.
Drains and tubes: Surgical drains, nasogastric tubes, and other tubes can be a source of infection.
Signs and Symptoms of Postoperative Infections: Surgical Site Infection (SSI):
Postoperative infections may not manifest immediately. The onset is often delayed, occurring several days after surgery. The signs and symptoms vary depending on the site of infection.
Redness (Erythema): The area around the incision is red and warm to the touch.
Swelling (Edema): The incision and surrounding tissues are swollen.
Pain: Increased or worsening pain at the surgical site.
Purulent Drainage: The presence of pus, which may be yellow, green, or brown and may have a foul odor.
Fever: A temperature greater than 100.4°F (38°C).
Signs and Symptoms of Postoperative Infections: Urinary Tract Infection (UTI):
Dysuria: Painful urination.
Urinary Frequency and Urgency: The need to urinate frequently and urgently.
Cloudy or Foul-Smelling Urine: A change in the appearance or odor of the urine.
Lower Abdominal Pain: Discomfort in the lower abdomen or suprapubic area.
Signs and Symptoms of Postoperative Infections: Respiratory Infection (Pneumonia):
Fever: Elevated body temperature.
Cough: Productive or non-productive cough.
Sputum Production: The production of purulent or colored sputum.
Shortness of Breath (Dyspnea): Difficulty breathing.
Increased Respiratory Rate (Tachypnea): Rapid breathing.
Signs and Symptoms of Postoperative Infections: Bloodstream Infection (Sepsis):
High Fever and Chills: A sudden spike in temperature.
Hypotension: Low blood pressure.
Tachycardia: Rapid heart rate.
Confusion or Altered Mental Status: Changes in the patient's cognitive function.
Generalized Malaise: A general feeling of being unwell
Basic Nursing Interventions for Preventing and Recognizing Infection: Hand Hygiene
The single most important intervention.
Nurses must perform hand hygiene before and after all patient contact, dressing changes, and handling of sterile equipment.
Basic Nursing Interventions for Preventing and Recognizing Infection: Wound Care
Maintain aseptic technique during dressing changes: This includes using sterile gloves, instruments, and dressings.
Assess the wound for signs of infection (REEDA: Redness, Edema, Ecchymosis (bruising or discoloration), Drainage, Approximation).
Basic Nursing Interventions for Preventing and Recognizing Infection: IV Catheter Care
Use aseptic technique during insertion and maintenance of IV catheters.
Inspect the site for redness, swelling, and tenderness.
Change dressings when needed
Basic Nursing Interventions for Preventing and Recognizing Infection: Foley Catheter Care
Maintain a closed drainage system.
Perform daily perineal care and keep the catheter secured to prevent movement and irritation.
Remove the catheter as soon as it is no longer medically necessary.
Basic Nursing Interventions for Preventing and Recognizing Infection: Respiratory Care
Early Ambulation: Encourage the patient to get out of bed as soon as possible. Ambulation improves lung expansion and prevents atelectasis.
Incentive Spirometry: Instruct the patient on the proper use of an incentive spirometer. This helps with deep breathing and lung expansion.
Coughing and Deep Breathing: Encourage the patient to cough and deep breathe every 1-2 hours while awake to clear secretions and prevent pneumonia.
Basic Nursing Interventions for Preventing and Recognizing Infection: Nutrition and Hydration
Encourage Adequate Nutrition: Proper nutrition, especially protein and Vitamin C, is essential for wound healing and immune function.
Promote Hydration: Adequate fluid intake helps maintain kidney function and flushes the urinary tract, preventing UTIs.
Basic Nursing Interventions for Preventing and Recognizing Infection: Patient and Family Education
Educate the patient and family on the signs and symptoms of infection to look for at home.
Instruct them on proper wound care and hygiene.
Teach them the importance of completing the full course of antibiotics, if prescribed.
surgical incision normal vs not normal (infection risk)
assess for
normal
not normal
infection can cause
Assess the tissue integrity of the incision on a regular basis, at least every 8 hours, for redness/hyperpigmentation, increased warmth, swelling, tenderness or pain, and the type and amount of drainage
Normal:
Some drainage change from
sanguineous (bloody)
serosanguineous (yellowish mixed with light red or pale pink)
serous (serumlike or yellow)
is normal during the first few days.
Crusting on the incision line is normal, as is a pink color to the line itself, which is caused by inflammation from the surgical procedure.
Slight swelling under the sutures or staples is also normal.
Not normal
Serosanguineous drainage continuing beyond the fifth day after surgery, or in an increasing amount, is a sign of possible dehiscence, and the surgeon should be notified increased risk of infection
Redness/hyperpigmentation or swelling of or around the incision line, excessive tenderness or pain on palpation, and/or purulent or odorous drainage indicates surgical site infection (SSI) and must be reported to the surgeon.
Impaired healing and a breakdown of the surgical wound with loss of tissue integrity may be caused by infection
a “left-shift” or “bandemia,”
An increase in the band cells (immature neutrophils) in the white blood cell differential count
is an indication of infection.
postoperative phase are: Potential for infection and delayed healing due
wound location
decreased mobility
drains and drainage
tubes
Preventing Wound Infection and Delayed Healing: wound care
Wound care includes
reinforcing the dressing
changing the dressing
assessing the wound for healing and infection
Preventing Wound Infection and Delayed Healing: drains
Drains:
caring for drains including
emptying drainage containers and reservoirs
measuring drainage and documenting findings
place absorbent pads under and around the exposed drain
Preventing Wound Infection and Delayed Healing: drug therapy
A patient at risk for wound infection may have received antibiotic therapy with drugs that are effective against organisms common to the specific surgical site both before and during surgery.
The need for these antibiotics is reevaluated at 24 hours after surgery.
If signs or symptoms of infection are not present, the antibiotic is discontinued at that time.
If signs or symptoms of wound infection are present, they are documented to justify continuation of antibiotic therapy.
wound infection risks:
Wound dehiscence
wound Evisceration
is a partial or complete separation of the outer wound layers, sometimes described as a splitting open of the wound.
is the total separation of all wound layers and protrusion of internal organs through the open wound