EXAM FOUR ANATOMY
1/250
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
251 Terms
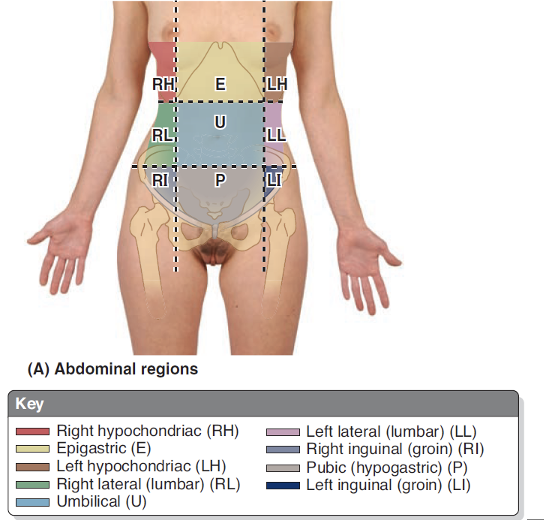
Abdominal Quadrants
RH – Small intestine, right kidney, gallbladder, liver
LH – Pancreas, left kidney, colon, spleen
E – Adrenal glands, spleen, pancreas, duodenum, liver, stomach
RL – Right colon, liver, gallbladder
LL – Left kidney, descending colon
U – Duodenum, ileum, jejunum, umbilicus
RI – Cecum, appendix
LI – Sigmoid colon, descending colon
P – Female reproductive organs, sigmoid colon, urinary bladder
What are the layers of the fascia of the abdominal wall? (Superficial to Deep)
Skin → Camper Fascia → Scarpa Fascia → Superficial Investing Fascia → External Oblique → Intermediate Investing Fascia → Internal Oblique → Deep Investing Fascia → Transversus Abdominus → Transversalis Fascia → Extraparitoneal Fat → Parietal Peritoneum
Where is a potential space for fluid to accumulate in the abdomen?
Between the membranous layer and the deep fascia covering the rectus abdominus and external oblique muscle is a potential space where fluid can accumulate.
External Oblique
O: external surfaces of 5th-12th ribs
I: Linea alba, pubic tubercle, and anterior half of iliac crest
N: Thoracoabdominal N.
V:
Internal Oblique
O: thoracolumbar fascia, anterior iliac crest, inguinal ligament
I: Inferior borders of 10th-12th ribs, linea alba, pubis via conjoint tendon
N: Thoracoabdominal N.
V:
Transversus Abdominis
O: Internal surfaces of 7th-12th costal cartilages, thoracolumbar fascia, iliac crest, inguinal ligament
I: Linea alba, pubic crest, pubis via conjoint tendon
N: Thoracoabdominal N.
V: Lower posterior intercostal and subcostal arteries, superior and inferior epigastric arteries, superficial and deep circumflex arteries, posterior lumbar arteries
Rectus Abdominis
O: Pubic symphysis and pubic crest
I: Xiphoid process and 5th-7th costal cartilages
N: Thoracoabdominal N.
V:
Pyramidalis
O: Body of pubis
I: linea alba
N: Illiohypogastric N.
V:
What are the actions of the abdominal muscles?
Provides support for the region while allowing expansion
Helps protect the abdominal viscera from injury
Compresses abdominal viscera to maintain or increase intra-abdominal pressure. Especially helpful during respiration, coughing and burping
Produces the necessary force for action such as defecation, micturition, vomiting, and parturition
Actions to help move the trunk
Flexion of trunk – External and Internal obliques, Rectus abdominis
Rotation of trunk – External and Internal obliques
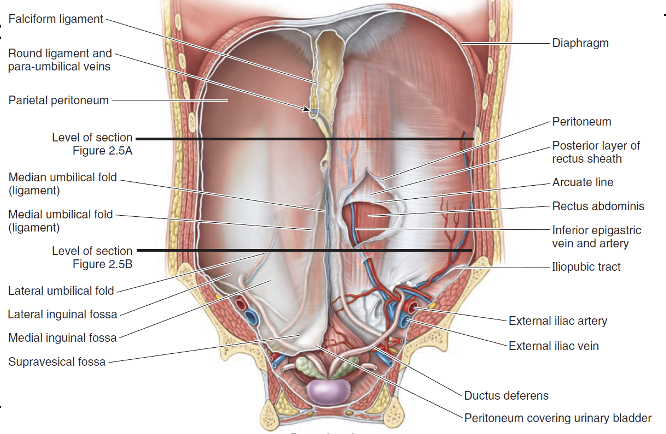
Umbilical Peritoneal Folds
1. Median umbilical fold – from apex of bladder to umbilicus, covers median umbilical ligament and has urachus
2. Medial umbilical folds – lateral to median umbilical folds, cover medial umbilical ligaments which has umbilical artery which becomes medial umbilical ligament
3. Lateral umbilical folds – lateral to the medial umbilical folds, cover inferior epigastric vessels
The thoracoabdominal nerves come from what spinal branches?
T7-T11
In the case that there is a blockage in either vena cava what anastomoses will provide collateral circulation?
The superficial and deep anastomoses provide collateral circulation in the event that there is a blockage in either vena cava.
Where do nodes drain in relation to the transumbilical plane?
Superficial lymphatics accompany the superficial veins
Those above the transumbilical plane drain to the axillary lymph nodes, or some may drain to parasternal nodes
Those below the transumbilical plane drain to the superficial inguinal lymph nodes
Where do the deep lymphatics of the anterolateral abdominal wall drain to?
Deep lymphatics accompany the deep veins of the abdominal wall and drain to the external iliac, common iliac and right and left lumbar lymph nodes.
What is inside the Inguinal Canal? (Male & Female)
Spermatic Cord or Round ligament of the uterus
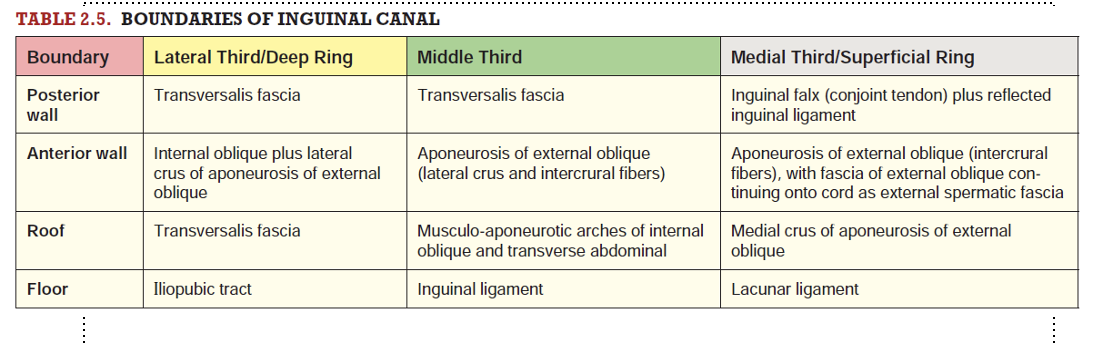
What are the borders of the Inguinal Canal?
Two walls, Floor and Roof:
Anterior wall – formed by external oblique aponeurosis
Posterior wall – formed by tranversalis fascia
Roof – lateral portion is tranversalis fascia, central portion by musculo-aponeurotic arches of internal oblique and transversus abdominis muscles, medial portion formed by medial crus and intercrural fibers
Floor – lateral portion formed by iliopubic tract, central portion by superior surface of inguinal ligament, medial portion by the lacunar ligament
Direct Hernias
Less common
Predisposing factor: Weakness of anterior abdominal wall in inguinal triangle
Coverings: Peritoneum plus tranversalis fascia
Rarely enters scrotum
Herniating bowel passes medial to inferior epigastric vessels through superficial ring
Indirect Hernias
More common
Predisposing factor: Patency of processus vaginalis
Coverings: peritoneum plus all three fascial coverings of cord/round ligament
Commonly passes into scrotum/labium majus
Herniating bowel passes lateral to the inferior epigastric vessels through the deep inguinal ring
Explain the process of relocation in regards to fetal testes and ovaries.
Fetal testes relocate from dorsal abdominal wall to the deep inguinal rings during the 9th to 12th fetal weeks. Final location of the testis in the scrotum usually occurs before or shortly after birth
Fetal ovaries relocate during the 12th week
What are some key features of the peritoneal cavity?
Contains leukocytes and antibodies to help resist infection
Completely closed in males
In females, - communication pathway to exterior of body through uterine tubes, uterine cavity and vagina
Potential source of infection from exterior
What is the difference of pain sensation in regards to the parietal and visceral regions?
Parietal
Sensitive to pressure, pain, heat, cold
Pain is well localized
Visceral
Insensitive to touch, heat, cold and laceration, stimulated by stretching and chemical irritation
Pain is poorly localized; referred to the dermatomes of the spinal ganglia that provide the sensory fibers
Describe the areas of referred pain; foregut, midgut, hindgut.
Pain from foregut derivatives (pharynx, esophagus and stomach) is experienced inepigastric region
Pain from midgut derivatives (sm. Intestine, cecum, appendix, and ascending colon) - umbilical region
Pain from hindgut derivatives (descending and sigmoid colons) - pubic regions
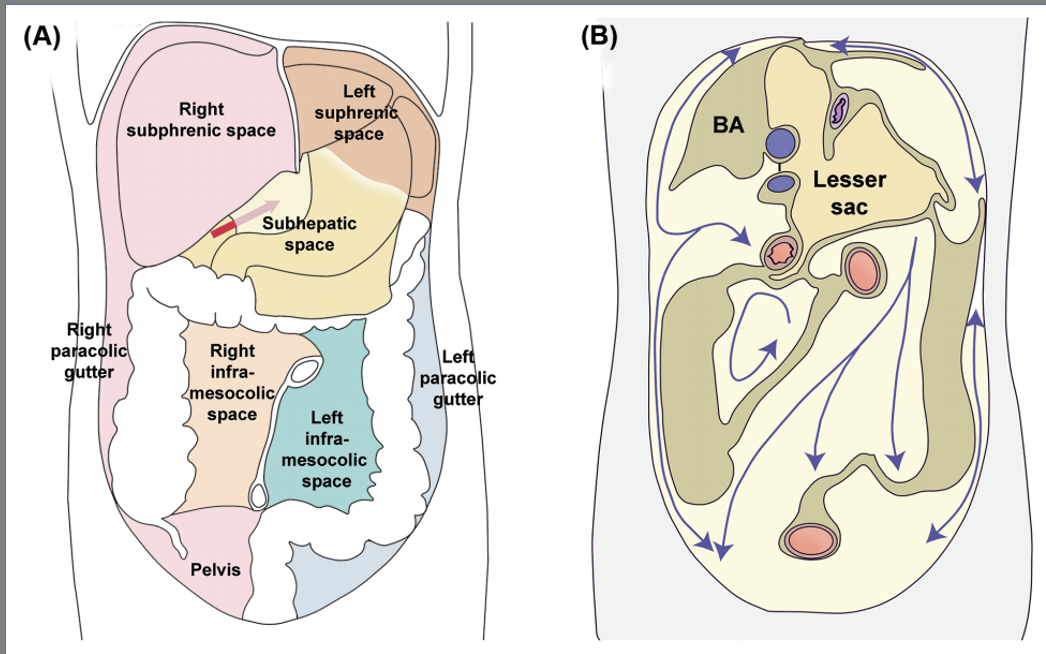
What does the supracolic compartment contain?
Stomach, Liver, Spleen
What does the infracolic compartment contain?
Small intestine, ascending/descending colon
Explain the relationship between the abdominal organs and their location in regards to the peritoneum.
Liver: The liver is almost completely enveloped by peritoneum, forming a structure known as the "hepatogastric ligament" that connects it to the lesser curvature of the stomach. The peritoneum over the liver is known as the "coronary ligament."
Pancreas: The pancreas has a retroperitoneal location, meaning it is situated behind the peritoneum. However, the head of the pancreas is covered by peritoneum and is in close proximity to the duodenum.
Spleen: The spleen is intraperitoneal, meaning it is covered by peritoneum, but it is not suspended by a mesentery.
Kidneys: The kidneys are retroperitoneal, meaning they are situated behind the peritoneum.
Stomach: The stomach is intraperitoneal, and it is suspended by a double layer of peritoneum known as the "greater omentum."
Duodenum: The first part of the duodenum is retroperitoneal, while the remaining parts (second, third, and fourth) are intraperitoneal.
Small Intestine (Jejunum and Ileum): The jejunum and ileum are suspended by a mesentery known as the "mesentery proper."
Cecum and Appendix: The cecum and appendix are intraperitoneal and are suspended by the "mesoappendix."
Colon (Ascending, Transverse, Descending, Sigmoid): The ascending and descending colon are retroperitoneal, while the transverse and sigmoid colon are intraperitoneal and have mesenteries known as the "transverse mesocolon" and "sigmoid mesocolon."
Rectum: The upper part of the rectum is retroperitoneal, while the lower part is intraperitoneal.
What is the purpose of the “small bowel mesentery”?
The small bowel mesentery, or "mesentery proper," is a double layer of peritoneum that supports the jejunum and ileum. It contains blood vessels, lymphatic vessels, and nerves. The superior mesenteric artery and vein, along with lymphatic vessels and nerves, travel within the mesentery, supplying the small intestine. The mesentery allows for mobility of the small intestine within the abdominal cavity, facilitating digestion and absorption of nutrients.
How is the colon organized in the abdomen?
The ascending and descending colon have retroperitoneal attachments, which means they are fixed to the posterior abdominal wall. This attachment provides stability to these parts of the colon and prevents them from excessive movement.
What is the significance of the paracolic gutters?
Right and Left paracolic gutters
Can be sites of passage for infections fluids from different compartments
Ex: Fluid from an affected appendix can travel up the right paracolic gutter to the hepatorenal recess
Peritonitis
•Infection or inflammation
•Bacterial contamination or gut trauma
•If widespread can be lethal
Peritoneal Adhesions
Damage to peritoneum (infection, stab wounds, abdominal operations)
Release of fibrin - replaced by fibrous scar tissue
Limit movement of viscera
Chronic pain or emergency complications
Adhesiotomy
Peritoneal Dialysis
Peritoneal dialysis (PD) is a medical procedure used to treat individuals with kidney failure, a condition in which the kidneys can no longer adequately filter waste and excess fluid from the blood. PD involves the use of the peritoneum, a membrane that lines the abdominal cavity, as a natural filter for waste removal.
In peritoneal dialysis, a sterile dialysate solution (a mixture of water, electrolytes, and glucose) is introduced into the peritoneal cavity through a catheter surgically placed in the abdominal wall. The peritoneum acts as a semi-permeable membrane, allowing waste products and excess fluid from the bloodstream to diffuse into the dialysate solution.
Describe the component making up each 1/3 of the esophagus.
Upper 1/3 skeletal muscle
Lower 1/3 smooth muscle
Middle 1/3 both
Where does the esophagus pass through the diaphragm?
Passes through thoracic diaphragm - T10
Emerges through the right crus of diaphragm before terminating at the cardiac opening of the stomach
What is significant about the lower esophageal sphincter?
Transition from stratified squamous epithelium of the abdominal esophagus to simple columnar epithelium of the stomach
Continuous irritation → metaplasia (Barrett’s esophagus) → esophageal adenocarcinoma
What supplies the thoracic and abdominal esophagus?
Arterial supply to the esophagus is from thoracic and abdominal sources
Thoracic esophagus
small branches of thoracic aorta
Abdominal esophagus
Branches from left gastric artery (celiac trunk)
Branches from left inferior phrenic artery (abdominal aorta)
Venous drainage of the esophagus
Blood above the diaphragm → drains to azygous vein → drains to superior vena cava
Blood below the diaphragm → drains to left gastric vein → drains to portal venous system
(The left gastric vein and its anastomoses are the usual suspect in an alcoholic that presents with painless hematemesis)
Innervation of the esophagus
The esophagus is innervated by the esophageal plexus coming from the right and left vagus nerves as well as the afferent fibers that pass through the sympathetic trunk and splanchnic nerves.
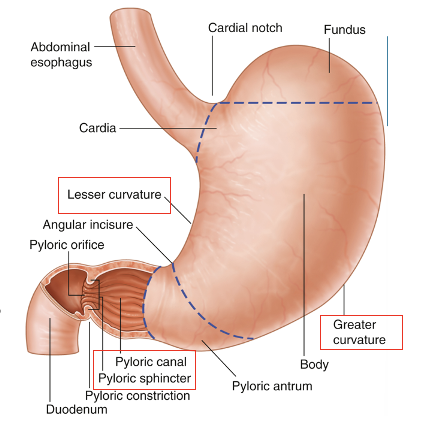
What are the four regions of the stomach?
Divided into 4 regions:
Cardia – surrounds the opening of the esophagus into the stomach
Fundus – above the level of the cardial orifice
Body – largest region
Pylorus – most distal end of stomach; transition to small intestine
More stomach features
Greater curvature – faces inferiorly and is an attachment for greater omentum
Lesser curvature – faces superiorly and is an attachment for lesser omentum
Pyloric canal – ends in a smooth-muscle pyloric sphincter that controls movement of stomach contents into the duodenum
Muscle layers of the stomach
Longitudinal = outermost muscle layer
Circular
Oblique = innermost muscle layer
Stomach’s anatomical relationship to: liver, spleen, pancreas, transverse colon
Liver: superior & to the right of stomach
Hepatogastric ligament – attaches lesser omentum to liver'
Spleen: Lies against the posterior abdominal wall to the left of the stomach
Pancreas: Lies posterior
Transverse Colon: Attached to greater omentum & greater curvature by transverse mesocolon
Parasympathetic & Sympathetic Innervation of the Stomach
Parasympathetic
From anterior & posterior vagal trunks and their branches
Sympathetic
From T6-T9 segments of spinal cord
Passes to celiac plexus via greater splanchnic nerves
Function of the spleen
Acts as a filter for old RBCs
Filters blood for immune system
Storage for specialized white blood cells and platelets
What is the location of the spleen?
Lies in the left upper quadrant against the diaphragm – in the area of ribs 10-12; usually not palpable
Phrenico-colic Ligament
connects left colic flexure to diaphragm; contacts lower pole of the spleen
Gastrosplenic Ligament
Connects spleen to stomach
(Contains short gastric vessels & left gastro-omental vessels)
Splenorenal Ligaments
Connects spleen to left kidney
(contains splenic artery and vein)
Branches of the splenic artery
Pancreatic branches – enter its superior border
Left gastro-omental artery – anastomoses w/ right gastro-omental
Short gastric arteries – supplies fundus of stomach
Splenic branches – enter hilum of spleen
Spleen venous drainage
Splenic vein joins the superior mesenteric vein to form the portal vein
Spleen Lymph drainage
Lymphatic fluid from spleen drains to pre-aortic nodes near the origin of the celiac trunk (celiac nodes)
Spleen Innervation
Parasympathetic: Vagus N.
Sympathetic: T6-T8
Pain in the left shoulder
Kehr’s sign
Splenic Rupture: Kehr's sign is most commonly associated with a ruptured spleen, often due to trauma or injury. When the spleen ruptures, it can release blood into the abdominal cavity, causing irritation to the diaphragm and resulting in referred pain in the left shoulder.
Function of liver
Largest gland in the body
Except for fat, nutrients absorbed through GI tract are conveyed to liver by portal venous system
Stores glycogen, produces bile
Subphrenic recesses
superior extensions of peritoneal cavity; separated into right and left by falciform ligament
Sub hepatic space
portion of supracolic compartment inferior to liver
Hepatorenal Recess
extension of subhepatic space; communicates with right subphrenic recess
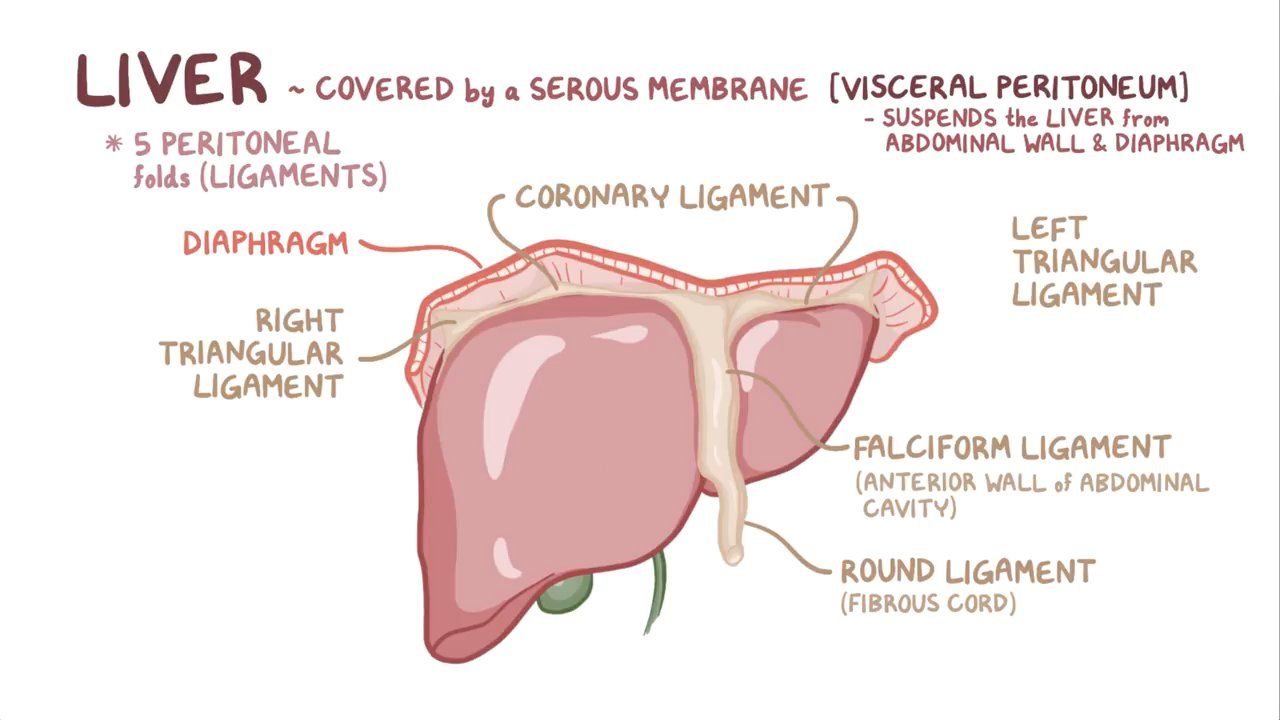
Ligaments of the liver
Coronary ligament – reflection of peritoneum from diaphragm to anterior and posterior portions of the liver
Falciform ligament – separates the left and right lobes
Left triangular ligament – where anterior and posterior portions of the coronary ligament meet on the left side
Right triangular ligament – where anterior and posterior portions of the coronary ligament meet on the right side
Bare area – portion of liver not covered with visceral peritoneum
What makes up the portal triad? What encloses it?
Portal triad = hepatic artery proper, common bile duct, and portal vein
Lesser omentum encloses portal triad
Hepatoduodenal ligament
Hepatogastric ligament
What makes the caudate lobe of the liver unique?
Caudate lobe may be considered a third liver as it receives vessels from both sides
Describe the venous drainage of the liver.
Right hepatic vein – drains V-VIII
Intermediate hepatic vein drains IV, V, VIII
Left hepatic vein drains II-IV
These veins connect to IVC and help hold the liver in place
Caudate lobe veins drain caudate lobe directly to IVC
Liver Lymph Drainage
Anterior superficial drain to hepatic then celiac nodes then cisterna chyli
Posterior superficial drain to phrenic and posterior mediastinal then the right lymphatic and thoracic ducts
Innervation of the liver
Parasympathetic: Anterior and Posterior Vagal Trunks
Sympathetic: Celiac Plexus
Four anastomoses of the portal venous system
Esophageal Vein → Gastric veins
Superior Rectal Vein → Inferior Rectal Vein
Paraumbilical Veins → Epigastric Veins
Colon veins
When portal circulation through liver is diminished or obstructed (e.g., liver disease), blood from alimentary tract can still reach right side of heart through IVC by way of these collateral routes.
Describe the steps to bile and blood flow through the hepatocytes.
Blood flows into sinusoids from vein and artery
Hepatocytes detoxify the blood and produce bile
Blood flows to central veins and then to hepatic veins
Bile flows through bile canaliculi to the interlobular biliary duct then to larger collecting bile ducts which merge to form right and left hepatic ducts
Hepatic ducts combine to form the common hepatic duct
Common hepatic duct joins with cystic duct to form the bile duct
Arterial supply of the hepatic ducts
Cystic artery supplies the proximal part
Right hepatic artery supplies the middle part
Posterior superior pancreaticoduodenal artery and gastroduodenal artery supplies the rectoduodenal part
Venous drainage of hepatic ducts
Proximal part drains to liver directly
Distal part empties into hepatic portal vein
Lymph drainage of bile duct
Can drain to cystic lymph nodes, lymph nodes of the omental foramen and hepatic lymph nodes which then drains to celiac lumph nodes
Parts of the gallbladder
Fundus – wide end that often projects from inferior border of liver
Body – main portion that connects to the visceral side of the liver
Neck – Narrow tapering end toward the porta hepatis, connects to the cystic duct
Cystic duct – connects neck of gallbladder to common hepatic duct
Cystohepatic triangle (of Calot) – triangle formed by common hepatic duct, cystic duct and visceral surface of liver
Arterial/Venous supply of the gallbladder
cystic artery
Neck of gallbladder and cystic duct – cystic veins
Fundus and body – drain into liver
Lymph drainage of the gallbladder
cystic/hepatic → celiac
Innervation of the gallbladder
Celiac plexus – sympathetic and visceral afferent
Vagus – parasympathetic
Right phrenic – somatic afferent
Alcoholic & Nonalcoholic Liver Disease
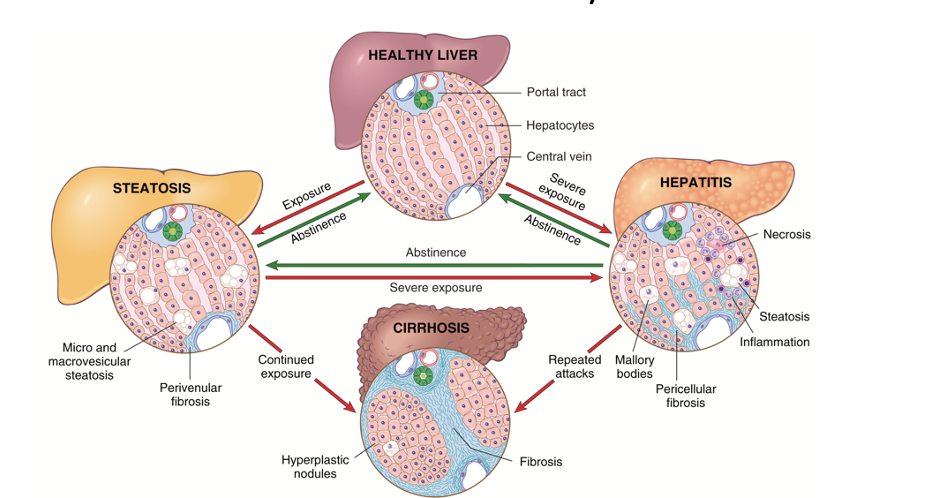
Portal Hypertension
Portal hypertension arises when there is diminished flow through the portal venous system, which may occur because of obstruction at the prehepatic, intrahepatic, or posthepatic level. While it can occur in acute liver failure, portal hypertension is more commonly seen with chronic liver failure. In acute liver failure, the obstruction is usually intrahepatic, and its major clinical consequences are ascites and hepatic encephalopathy. In chronic liver disease, portal hypertension develops over months to years, and its effects are more complex and widespread
Cholestasis
Cholestasis is a condition caused by extrahepatic or intrahepatic obstruction of bile channels or by defects in hepatocyte bile secretion. Can be reversed if obstruction is removed.
Cholestatic hepatocytes (1) are enlarged and are associated with dilated canalicular spaces (2). Apoptotic cells (3) may be seen, and Kupffer cells (4) frequently contain regurgitated bile pigments. (B) Cholestasis, showing the characteristic accumulation of bile pigments in the cytoplasm.
Cholelithiasis
Composed mainly of cholesterol crystals
Pigment stones are brown or black made up of insoluble calcium bilirubinate salts. They form when bile contains a high concentration of unconjugated bilirubin
Can form in gallbladder, cystic duct, or bile duct
Become symptomatic when they are large enough to cause mechanical injury to gallbladder or obstruction of biliary tract
Ultrasound and CT scans are used for locating stones
What are the four parts of the duodenum?
Superior
Short, mobile, ampulla
Descending
longer (7–10 cm), runs vertically along right sides of L2 and L3, curving around head of the pancreas; lies to right and parallel to IVC
bile duct and main pancreatic ducts enter its posteromedial wall via hepatopancreatic ampulla.
Inferior
6–8 cm long, crosses anterior to the IVC and aorta and posterior to the superior mesenteric artery and vein at level of L3
Ascending
short (~ 5 cm) and begins left of L3 and rises superiorly as far as superior border of the L2, 2–3 cm to left of midline. Passes on left side of aorta to reach inferior border of body of pancreas. Here, it curves anteriorly to join the jejunum at the duodenojejunal junction, which takes the form of an acute angle, the duodenojejunal flexure. The flexure is supported by the attachment of suspensory muscle of the duodenum (ligament of Treitz).
The suspensory muscle – slip of skeletal muscle from the diaphragm and a fibromuscular band of smooth muscle from the third and fourth parts of duodenum. The muscle passes posterior to pancreas and splenic vein and anterior to left renal vein.
Widens the angle of the duodenojujunal flexure and facilitates movement of the intestinal contents
Upper GI bleed
Blood supply of the duodenum
supraduodenal & superior pancreaticoduodenal a. supplies parts ½
inferior pancreaticoduodenal (anterior & posterior) aa., supplies parts 3 and 4
Lymphatics of the Duodenum
Anterior lymphatic vessels → pancreaticoduodeal lymph nodes (along the superior and inferior pancreatiocuodeanl arteries) → Pyloric lymph nodes (along the gastroduodeal artery)
Posterior lymphatic vessels → superior mesenteric lymph
Innervation of the Duodenum
Parasympathetic – Vagus (X)
Sympathetic – Greater and Lesser Splanchnic nerves by way of celiac and superior mesenteric plexuses and peri-arterial plexuses
Jejunum vs. Ileum
Jejunum is mainly in abdominal cavity (LUQ), where terminal Ileum begins in pelvis and ascends to medial aspect of cecum. The jejunum represents the proximal two-fifths and begins at the duodenojejunal flexure. It is mostly in the left upper quadrant of the abdomen and is larger in diameter and has a thicker wall than the ileum (this is going to be very slight) although it is shorter than the illeum. The Jejunum has prominent and numerous plicae circulares. Less prominent arterial arcades and longer vasa recta (straight arteries) The illeum has peyer’s patches
Arterial & Venous supply of the jejunum and illeum
SMA & SMV
Jejunum & Illeum Innervation
Sympathetic - T8-10
Parasympathetic - Posterior Vagal Trunks
Visceral afferent fibers - Insensitive to most pain stimuli such as cutting or burning but is very sensitive to distension (abdominal pins or intestinal cramps)
Peristalsis
Rhythmic contraction of the GI tract pushes food bolus along
Enteric nervous system: regulates and controls peristalsis and GI secretions, independently of the para- and sympathetic systems
Succinctly, the myenteric and submucosal plexuses are interconnected and regulate GI tract activity, from peristalsis to secretomotor functionality. They’re also interconnected with the sympathetic and parasympathetic systems.
Sigmoid Colon
characterized by S-shaped loop of variable length, links descending colon and rectum.
Extends from iliac fossa to third sacral segment, where it joins the rectum.
The termination of the teniae coli indicates the rectosigmoid junction.
Usually has a relatively long mesentery (sigmoid mesocolon) and has considerable freedom of movement, especially its middle part.
The left ureter and the division of the left common iliac artery lie retroperitoneally posterior to the apex of the root of the sigmoid mesocolon.
Blood supply to the large intestine
Ascending colon
SMA -> ileocolic -> colic
SMA -> ileocolic -> anterior cecal
SMA -> ileocolic -> posterior cecal
SMA -> right colic
Transverse colon
SMA -> right colic
SMA -> middle colic
IMA -> left colic
Descending colon
IMA -> left colic
Sigmoid colon
IMA -> sigmoidal aa.
Innervation of the Colon
The innervation to the colon is dependent on embryological origin:
•Midgut-derived structures - ascending colon and proximal 2/3 of the transverse colon receive sympathetic, parasympathetic and sensory supply via nerves from the superior mesenteric plexus.
•Hindgut-derived - distal 1/3 of the transverse colon, descending colon and sigmoid colon receive their sympathetic, parasympathetic and sensory supply via nerves from the inferior mesenteric plexus:
Parasympathetic innervation - pelvic splanchnic nerves
Sympathetic innervation - lumbar splanchnic nerves.
Appendicitis
Inflammation of the appendix
LOWER RIGHT QUADRANT PAIN, fever, n & v, appetite loss
Chief causes are fecal impaction and infection
Acute appendicitis is an emergent condition
300,000 or so hospitalizations annually in the US
Removal common
Used to be considered vestigial/non-functional
Now understood to play important role in immunity
Ischemic Bowel Disease
Disruption of blood flow to a specific segment of the intestines can produce ischemic bowel disease
Decreased bowel sounds, interruption of peristalsis, pain, etc. as a result of avascular necrosis of the bowel
Vascularization of the GI tract tends to be well-collateralized – facilitates surgical repair
LEFT COLIC FLEXURE IS MOST COMMON FOR VASCULAR BLOCKAGE
Celiac Disease
Immune-mediated pathology triggered by the ingestion of gluten.
Pediatric celiac disease
Symptoms develop between 6 and 24 months
Irritability, abdominal distension, anorexia, diarrhea, weight loss, muscle wasting, failure to thrive
Affects male and female children equally
Adults
Manifests between 30-60
Can have extended periods of time with no symptoms
Symptoms include anemia (due to iron deficiency and less commonly, B12 and folate deficiency), diarrhea, bloating and fatigue.
Bariatric Surgery
The duodenal switch is a weight-loss operation that modifies your stomach and your small intestine. It combines a gastrectomy (removal of part of your stomach) with an intestinal bypass, which makes the path your food takes through your intestines shorter.
If the head of the pancreas was injured what would we be most concerned about damaging?
Bile Duct
If the neck of the pancreas was injured what would we be most concerned about damaging?
Hepatic Portal Vein
If the body of the pancreas was injured what would we be most concerned about damaging?
Aorta
If the tail of the pancreas was injured what would we be most concerned about damaging?
Left Kidney
What branches of the splenic artery supply the pancreas?
Greater Pancreatic A. & Dorsal Pancreatic A.
What branches of the gastroduodenal artery supply the pancreas?
Anterior and posterior superior pancreaticoduodenal arteries
What branches of the SMA supply the pancreas?
Anterior and posterior inferior pancreaticoduodenal arteries
Describe the path of drainage in regards to pancreatic veins.
Pancreatic/Pancreatico-Duodenal Veins → Splenic & SMV → Hepatic Portal Vein
Pancreaticosplenic nodes (Neck, Body, Tail) drain to
Pyloric Nodes
Pyloric and/or Pancreaticoduodenal Nodes (Head) drain to
Pyloric → Hepatic