MBS Physiology Module 2
1/159
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
160 Terms
What structural feature electrically couples cardiac muscle cells?
Gap junctions in intercalated discs.
What are desmosomes responsible for in cardiac muscle?
Mechanical strength and force transmission between cells.
How many nuclei are typically found in a cardiac myocyte?
One per cell.
What allows cardiac muscle to function as a syncytium?
Electrical coupling via gap junctions.
What is the main reason cardiac muscle cannot undergo tetanus?
Prolonged refractory period (~250 ms).
What is the main source of ATP for cardiac muscle under normal conditions?
Oxidation of fatty acids.
What percentage of cardiac ATP comes from glycolysis?
Less than 2%.
What ion's influx is essential for initiating contraction in cardiac muscle?
Calcium (Ca²⁺).
What triggers calcium-induced calcium release in cardiac myocytes?
Influx of extracellular Ca²⁺ during action potential.
What initiates the cardiac action potential in a healthy heart?
The depolarization of cardiac pacemaker cells, primarily in the sinoatrial (SA) node.
Which current is responsible for the pacemaker potential in the SA node?
The funny current (I_f), which is a mixed current carried by sodium (Na⁺) and potassium (K⁺) ions.
What causes the depolarization (Phase 0) in SA node cells?
Opening of voltage-gated Ca²⁺ channels.
Which neurotransmitter slows heart rate by activating M2 receptors?
Acetylcholine, released by the vagus nerve, binds to M2 muscarinic receptors in the heart, decreasing heart rate.
What is the primary depolarizing ion in ventricular action potentials?
Sodium (Na⁺).
What defines the plateau phase of a cardiac action potential?
The plateau phase is defined by a balance between depolarization due to calcium (Ca²⁺) influx and repolarization due to potassium (K⁺) efflux, prolonging the action potential and allowing for effective contraction.
What phase of the ventricular AP represents repolarization?
Phase 3 (due to K⁺ efflux).
What defines the Absolute Refractory Period (ARP)?
No AP can be initiated regardless of stimulus size.
What defines the Relative Refractory Period (RRP)?
A second AP can be triggered by a larger-than-normal stimulus.
What part of the ECG corresponds to ventricular depolarization?
The QRS complex, which represents the electrical activity associated with the contraction of the ventricles.
What is the effect of increased cAMP on HCN channels in SA node?
Increased cAMP enhances the opening of HCN channels, leading to an increased heart rate by promoting the influx of Na+ ions during diastolic depolarization.
How does acetylcholine affect AV node conduction?
Slows it by inhibiting Ca²⁺ and increasing K⁺ currents.
What is cardiac output (CO)?
CO = Heart Rate (HR) × Stroke Volume (SV).
What role do arterioles play in peripheral resistance?
Arterioles regulate blood flow and maintain peripheral resistance through vasoconstriction and vasodilation, thus influencing blood pressure and distribution of blood to tissues.
According to Poiseuille’s Law, resistance is inversely proportional to what power of radius?
The fourth power (r⁴).
What type of flow is disrupted by obstructions or rough surfaces?
Laminar flow → becomes turbulent.
Turbulent flow is disrupted by obstructions or rough surfaces, leading to increased resistance and energy loss.
What determines velocity of flow in vessels with varying diameter?
Inversely proportional to cross-sectional area.
What is the formula for flow (Q)?
Flow = ΔP / R (pressure difference / resistance).
What vessel types serve as a blood volume reservoir?
viens
What is the physiological significance of the AV node delay?
Allows ventricles time to fill before contraction.
What causes Korotkoff sounds during blood pressure measurement?
Turbulent blood flow (bruits).
What is the primary function of the cardiovascular system?
To circulate blood, delivering oxygen and nutrients to tissues and removing waste products. This requires synchronized contraction of atria and ventricles through electrical activation.
Describe the path of blood flow through the heart.
Blood flows:
body →
right atrium →
right ventricle →
lungs (pulmonary circulation) →
left atrium →
left ventricle →
body (systemic circulation).
What structural features allow arteries to act as pressure reservoirs?
Arteries have thick, elastic walls. During systole, they stretch; during diastole, they recoil to maintain blood pressure.
How do veins function as volume reservoirs?
Veins are thin-walled, highly distensible, and contain valves. They store a large volume of blood and aid in venous return to the heart.
What is the SA node and what is its role in cardiac function?
The SA node is the pacemaker of the heart. It initiates action potentials that set the heart rate by spontaneously depolarizing.
What causes the unstable resting potential in the SA node?
Opening of HCN (If) channels which allow Na⁺ influx during hyperpolarization (Phase 4), gradually depolarizing the membrane.
What ion influx is responsible for depolarization in SA node action potentials?
Ca²⁺ influx through voltage-gated Ca²⁺ channels during Phase 0.
What ends the SA node action potential?
K⁺ efflux (Phase 3), repolarizing the membrane.
How do autonomic signals regulate SA node activity?
Epinephrine increases cAMP to enhance HCN activity (faster HR); ACh activates M2 receptors to reduce cAMP and open K⁺ channels (slower HR).
What is the conduction sequence of electrical activity through the heart?
SA node →
internodal tracts →
AV node →
Bundle of His →
left/right bundle branches →
Purkinje fibers.
What is the physiological significance of the AV node delay?
It allows complete ventricular filling before contraction.
Describe Phase 0 in atrial and ventricular myocytes.
Rapid Na⁺ influx through voltage-gated Na⁺ channels causes depolarization.
What is the plateau phase (Phase 2) and why is it important?
Balance of Ca²⁺ influx and K⁺ efflux; prolongs depolarization and allows time for contraction.
What causes repolarization (Phase 3) in ventricular action potentials?
Ca²⁺ channels close, and K⁺ efflux dominates.
What maintains resting potential (Phase 4) in ventricular cells?
Balanced Na⁺/Ca²⁺ inward and K⁺ outward currents at ~ –85 mV.
What is the effective refractory period (ERP)?
Includes ARP and early repolarization; a weak Na⁺ current exists, but not enough for propagation.
What is the supranormal period (SNP)?
The cell is more excitable than normal because the membrane potential is closer to threshold.
What does the ECG measure?
The summed electrical activity of the heart, detected as voltage differences on the skin.
What do the components of the ECG represent?
P wave = atrial depolarization;
QRS = ventricular depolarization;
T wave = ventricular repolarization.
How is heart rate calculated from the ECG?
HR = 60 / R-R interval in seconds.
What is the difference between flow rate and velocity?
Flow rate = volume/time (e.g., mL/min);
velocity = distance/time (e.g., cm/min), dependent on vessel diameter.
What determines velocity of flow in the vasculature?
Velocity = Flow / Cross-sectional area.
Narrower vessels → higher velocity
What is the main driving force of blood flow?
Pressure gradient (ΔP). Flow occurs from high to low pressure.
What is Poiseuille’s Law and its key relationship?
R∝r41. A small increase in radius greatly reduces resistance.
What is total peripheral resistance (TPR)?
Sum of all vascular resistances; mainly determined by arterioles.
Why are arterioles considered resistance vessels?
They have smooth muscle to constrict/dilate, significantly impacting blood flow and pressure.
What causes turbulent blood flow?
Obstructions,
sharp turns,
or rough surfaces disrupt laminar flow, increasing resistance.
What are Korotkoff sounds and what do they indicate?
Audible signs of turbulent flow during BP measurement; used to determine systolic/diastolic pressure.
What phase of the cardiac cycle involves ventricular filling?
Diastole — the relaxation phase during which the heart fills with blood.
What is the formula for stroke volume (SV)?
SV = End Diastolic Volume (EDV) - End Systolic Volume (ESV)
What is the formula for ejection fraction (EF)?
EF = SV / EDV; normal range is 50–70%.
What is the equation for cardiac output (CO)?
CO = SV × HR
What mechanical event immediately follows electrical depolarization in the heart?
Ventricular contraction (systole).
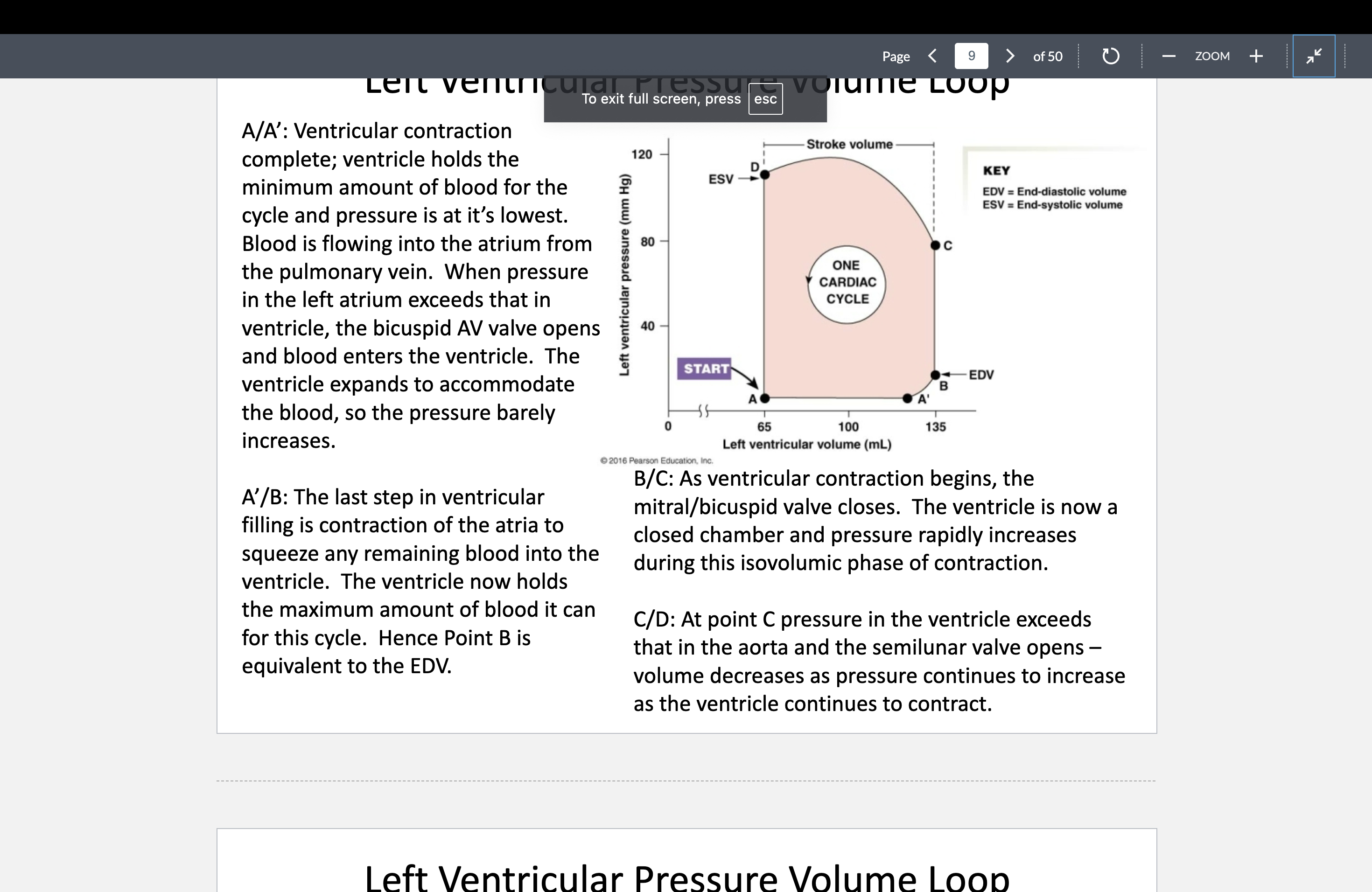
What does point B on a pressure-volume loop represent?
End Diastolic Volume (EDV) — the volume in the ventricle just before systole begins.
What happens during the isovolumic contraction phase?
Ventricular pressure rises with no volume change; mitral valve closes but semilunar valve hasn’t opened yet.
How does increased preload affect the PV loop?
It increases EDV and stroke volume; the loop widens to the right.
What does increased afterload do to the PV loop?
It raises ventricular pressure, reduces SV, and increases ESV.
What change in the PV loop reflects increased contractility?
Higher pressure and decreased ESV; the loop shifts left and becomes taller.
What is the Frank-Starling Law of the Heart?
The more the heart fills (increased EDV), the stronger the contraction and the more it pumps.
What is preload?
The amount of passive stretch in the myocardium at the end of diastole (i.e., EDV).
What is afterload?
The pressure the left ventricle must overcome to eject blood, represented by aortic pressure.
What is contractility also known as?
Inotropism — the intrinsic ability of cardiac cells to contract at a given leng
How does sympathetic stimulation affect contractility?
It increases contractility via β₁-receptor activation and cAMP-mediated calcium handling.
Where are baroreceptors located?
Carotid sinus and aortic arch.
What do baroreceptors sense?
Changes in arterial pressure via stretch.
What happens when baroreceptor firing increases?
Increased parasympathetic tone, decreased HR and CO, and vasodilation to reduce MAP.
How does the body respond to decreased MAP (e.g., hemorrhage)?
Increased sympathetic activity → ↑ HR, ↑ contractility, vasoconstriction, and ↑ venous return.
Which nerves carry baroreceptor signals?
Carotid sinus → glossopharyngeal nerve; aortic arch → vagus nerve.
What is the simplified formula for mean arterial pressure (MAP)?
MAP = CO × TPR
How can MAP be estimated from SP and DP?
MAP ≈ DP + (SP - DP)/3
What is the normal range for MAP?
70–110 mm Hg
What is the critical minimum MAP to perfuse tissues?
At least 60 mm Hg
What is TPR and what factors affect it?
Total Peripheral Resistance; affected by vessel length, diameter, and blood viscosity
What effect do cardiac glycosides like digoxin have?
Increase contractility by inhibiting Na⁺/K⁺ ATPase and increasing intracellular Ca²⁺.
What is the result of decreased venous return on cardiac output?
Decreased preload → decreased CO (via Frank-Starling mechanism).
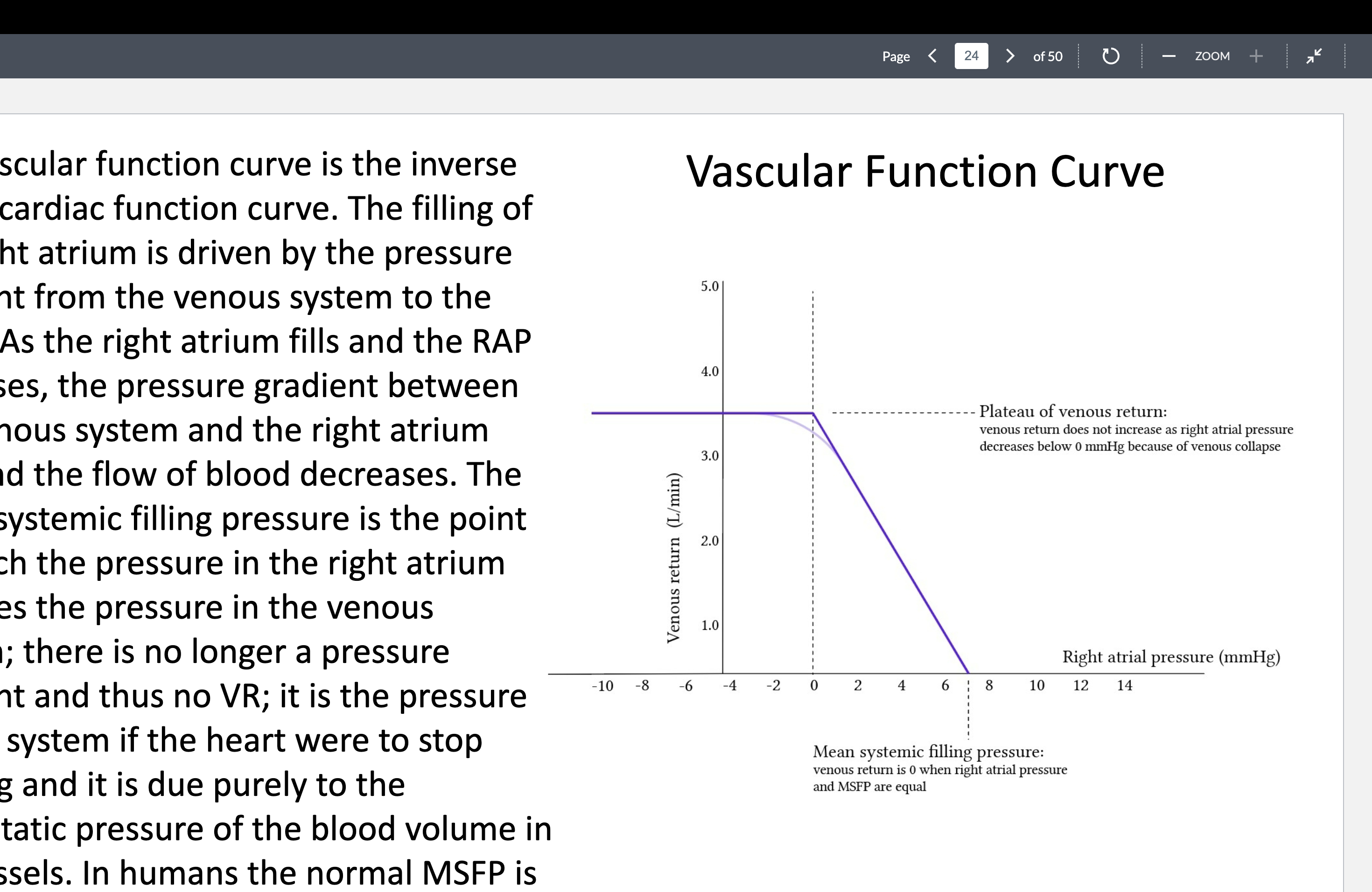
What is mean systemic filling pressure (MSFP)?
The pressure in the system if the heart stops; around 7 mm Hg, reflects stressed blood volume.
What is the equilibrium point on cardiac and vascular function curves?
The point where venous return equals cardiac output (VR = CO).
How does norepinephrine affect arterioles?
Binds α-receptors → vasoconstriction; increasing TPR and MAP.
How do baroreceptors respond to a rapid rise in blood pressure?
↑ Stretch → ↑ baroreceptor firing → ↑ parasympathetic, ↓ sympathetic → ↓ HR, ↓ contractility, ↓ MAP
What happens to cardiac output (CO) and venous return (VR) during increased afterload?
Afterload ↑ → stroke volume ↓ → CO ↓ → VR may decrease due to reduced forward flow
What is the Wiggers diagram used for?
To illustrate the timing of pressure, volume, electrical, and valve events in the cardiac cycle.
Which part of the PV loop is isovolumetric relaxation?
After the aortic valve closes and before the mitral valve opens (D → A phase)
How do the cardiac and vascular function curves interact?
The point where they intersect is where CO = VR; this is the system’s steady-state operating point.
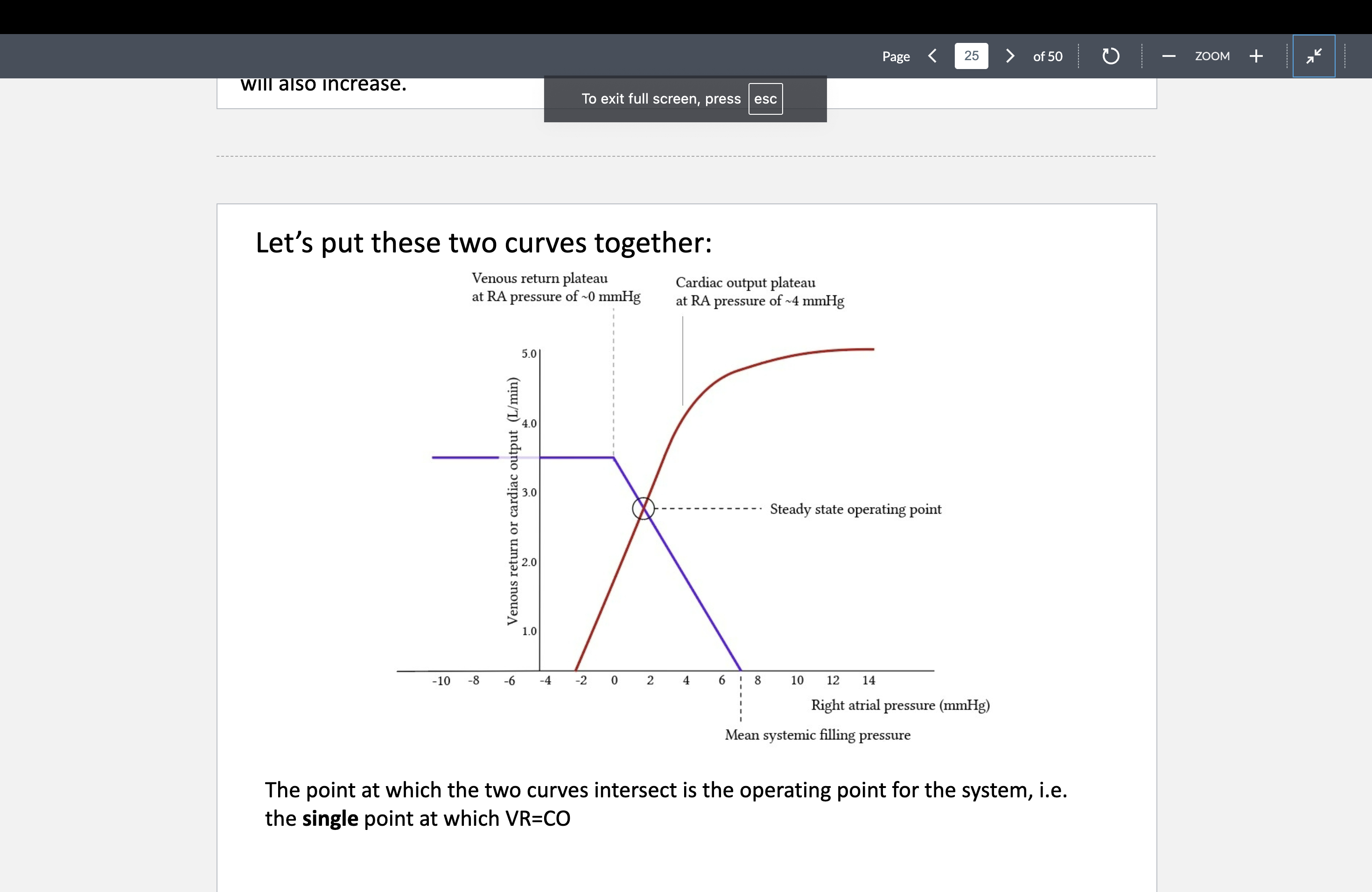
What does the flat part of the vascular function curve represent?
When RAP is too negative, veins collapse → venous return plateaus
What is a positive inotrope, and name an example?
Increases contractility; e.g., digoxin, β₁ agonists (norepinephrine)
What causes negative inotropy?
Parasympathetic stimulation (ACh), acidosis, anoxia, or catecholamine depletion
Why is maintaining a MAP ≥ 60 mm Hg essential?
To ensure adequate tissue perfusion, especially to the brain (avoids syncope and neuronal death)
What happens if MAP is < 60 mm Hg for too long?
Organ ischemia/infarction, especially cerebral hypoperfusion → syncope, brain damage
How do hormones like epinephrine affect blood pressure?
Bind α₁ (vasoconstriction) and β₂ receptors (vasodilation in skeletal muscle/liver)
How does the kidney indirectly regulate MAP?
Via hormones that affect water/salt retention and blood volume (e.g., renin-angiotensin system)