quizze- lines
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
44 Terms
Peripheral Intravenous Cannula (PIVC)
Inserted into a peripheral vein in the upper or
lower limb
• Generally hand, arm or cubital fossa
• Fluids, medications & blood products
• 14g -24g
• Size required dependent on use
• Max 72 hrs
• If surrounding skin inflamed or swollen do not
use.
Peripheral Arterial Line
Inserted in critical care areas for acute monitoring of
blood pressure
• Used for arterial blood sampling
• Inserted into radial artery, less commonly femoral artery
• Seldinger technique
• Caution when transferring patients so as not to dislodge
• If dislodged medical team notified immediately &
pressure applied to arterial site.
Definition of CVAD
Central venous access devices (CVADs) are
devices that are inserted into the body through a
vein and terminate at or close to the heart, or in
one of the great vessels
Depending on the CVAD, they can be inserted into one of the peripheral veins of the
upper extremities or into the ___ or ___
subclavian, jugular vein
CVADs enable the administration of:
fluids
• blood products
• medication
• Chemotherapy
• Contrast
• parental nutrition
• Other therapies to the bloodstream
Non-tunnelled CVADs
Central venous catheters (CVCs)
o Peripherally inserted central catheters (PICCs)
o Vascath dialysis catheters
Tunnelled CVADs
Hickman catheters
o Dialysis catheters (eg.Permacath)
o Portacath
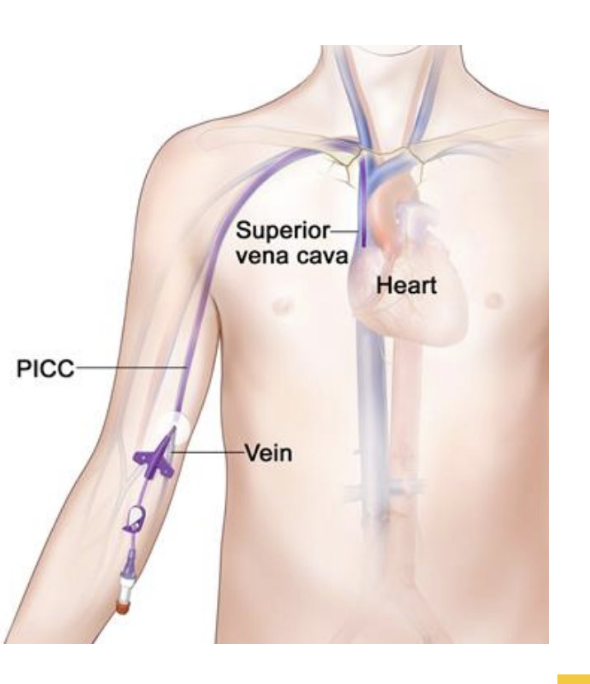
Peripherally Inserted Central Catheters (PICCs)
A PICC line is a central venous access
catheter that is inserted into a peripheral
vein in the upper arm
• Medium to long term access
• 1-3 lumens
• Size: 4F, 5F, 6F (depending on no.
lumens)
• Administration of central venous fluids,
medications and TPN.
PICC LINE insertion sites
basilic vein preferable choice,
usually the largest
• brachial vein preferable choice,
sometimes difficult to puncture as it
can be close to or beneath the
artery
• Cephalic vein less common as it is
usually quiet small.
Tip of catheter sits in the superior
vena cava
PICC insertion Fluoroscopy
• Ultrasound
• Local anaesthetic
• Needle
• Wire
• Sheath
• PICC catheter
• Fluoro screen to confirm
placement
• Secured with statlock and positive
pressure bungs
//
Can be inserted bedside
(ICU)
• Placement confirmed with
ECG or mobile chest xray
• Less reliable
PICC Complications- insertion
haematoma
• Infection
• pneumothorax
• Arterial puncture
PICC Complications- Positional
Catheter dislodgement
• Catheter tip migration
• Thrombus
• Occlusion
• Systemic Infection (Central line
associated Bloodstream infection)
Power PICC use in CT
The Power PICC is a purple central venous catheter that has
been approved by the FDA for power injection of contrast
• 4Fr single lumen can be injected at 4mls/see,
• 5Fr single lumen at 7 mls/sec
• 5F double lumen at 5 mls/sec
at a Maximum Injector Pressure limit of 325 psi
Accessing a PICC for CT
• Prior to first use, ensure that position of the tip has been confirmed and the
device is suitable to use.
• Scrub the hub for 15 sec prior to access.
• A CVAD must be aspirated before use
• Contrast can only be power injected through the purple lumen.
• Additional lumens should be labelled ‘no CT’
Positive-pressure valve: Needleless access device
• Enables forward displacement of fluid to prevent thrombus
formation at the lumen opening.
• must be primed before use
• Internal mechanism displaces fluid upon disconnection of a
syringe resulting in a small bolus of fluid from the distal end of
the lumen tip.
• This reduces the risk of catheter occlusion when not in use.
Flushing a PICC
CVADs should be flushed utilizing a ‘pulsatile’ flushing technique. This
involves pushing 1mL of fluid,
pausing, pushing another 1mL etc. This creates a turbulent flow
clearing the lumen more effectively than a straight flush.
Never use excessive force when attempting to flush a CVAD regardless
of syringe size.
A PICC should NOT be flushed using a syringe smaller than 10mls.
Smaller syringes generate greater pressures which can rupture the device
Central Venous Catheter (CVC)
Also known as a Central Line
• Inserted in the internal jugular, subclavian or femoral veins
• Inserted at bedside with ultrasound
• Administration of Medications, blood, TPN.
• Short term access < 10 - 14 days
typically 20-30cm long
• Used for short-term central venous access.
• A CVC may have up to five lumens and may
be antiseptic or antibiotic coated.
• CVCs that are not in use should be flushed
once every 12 hours to help prevent
blockages
CVC insertion
ultrasound
• Sterile field, gloves, gown and mask
• Seldinger central line kit
• Saline flush
• Chlorhexidine
• Lignocaine Suture
• Scalpel
• Sterile dressing
• Pressure bag to attach to monitoring
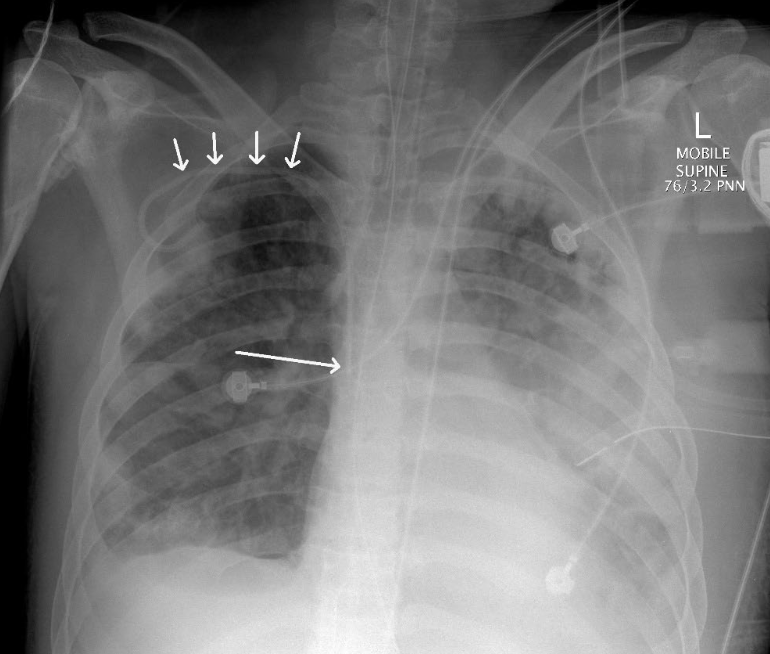
CVC Ideal final position
Distal to brachiocephalic
venous anastomoses,
proximal to right atrium
Inferior border of the
right main bronchus
shadow
CVC complications
• Infection as catheters inserted into the body make it easier for
bacteria from the skin to enter the bloodstream;
• Thrombus Blood clots forming in the catheter;
• Pneumothorax (collapsed lung) caused by the needle accidentally
piercing the lung during insertion;
• Air embolism caused by air entering the bloodstream through the
catheter. This occurs rarely but is a serious medical emergency.
• Damage to the blood vessel
• Migration of the catheter
CVC – power injection
• Devices specifically designed for power-injection are
available
• Depends on brand
• generally rated for pressures of 300 psi and flow-rates
of up to 10 ml s−1
.
• Always check external labelling.
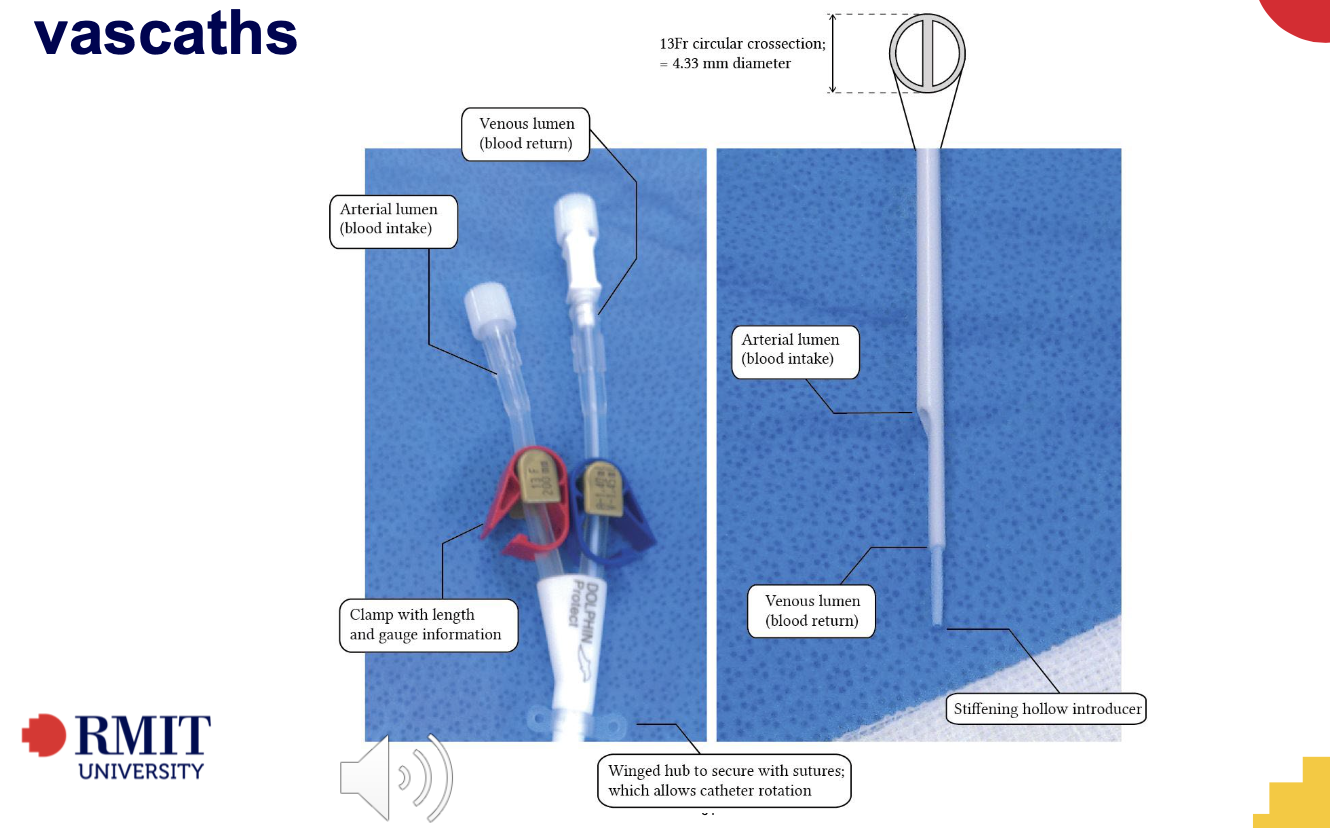
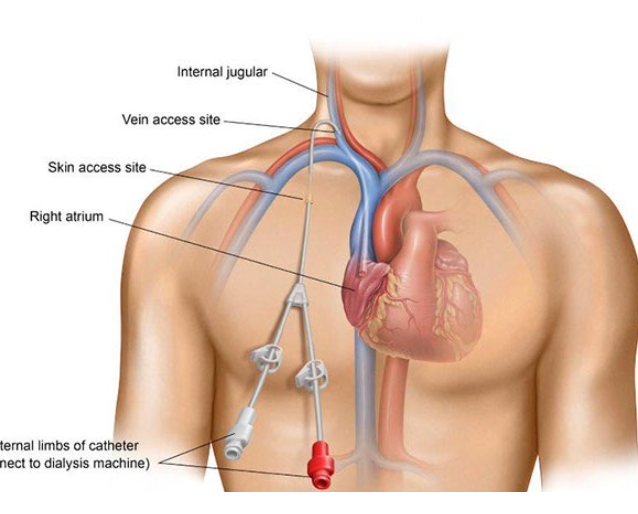
Vascath
• A vascath is a non-tunnelled central venous access device (CVAD),
• Used for short term access
• For dialysis and stem cell collection via apheresis.
• Vascaths are large-bored devices, 13.5F
• Inserted in the subclavian vein, the internal jugular (IJ) vein or the femoral vein.
• Vascaths are usually ‘locked’ with high concentrations of heparin to prevent lumen
blockage and remain clamped when not in use.
• Vascaths should only be accessed by trained dialysis and apheresis staff for these
procedures.
• Usually 1.2 mls heparin per lumen
• It is recommended that vascaths do not remain insitu for longer
than 7 days.
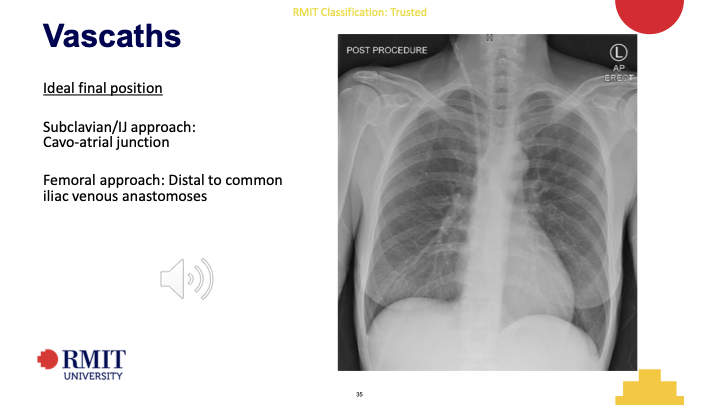
Vascath Ideal final position
Subclavian/IJ approach:
Cavo-atrial junction
Femoral approach: Distal to common
iliac venous anastomoses
Tunneled CVADs
Permacaths
• Hickmans
• Ports
Advantages of tunnelled CVADs include:
Lower infection rate
• Longer duration
• Less mispositioning
Tunnelled CVAD insertion
• US is used to puncture the jugular vein followed by
wire and small sheath.
• A small pocket is made in the chest wall, and the
catheter is tunned through, under the skin until it
emerges at the jugular puncture site.
• It is then inserted thought the sheath into the
jugular vein.
Permcaths
A permacath ( or permcath) is a type
tunnelled central venous access
device.
• It is a split catheter – this means that
the two lumens have unequal
lengths
• One opening is a few cm distal to
the other to give a staggered
opening
• Permacaths are used for dialysis
• Long term access (months - years)
• Wide bore catheter, 14.5 F
• Various lengths 19cm -31cm
• Sutured in place
• Inserted by a radiologist in angio
• Given the patient’s dependence on this therapy, these devices must not
be accessed outside of dialysis unless urgent access is required and this
has been authorized by a medical lead.
• Dialysis catheters must only be accessed by renal trained clinicians.
• Be aware that dialysis catheters are usually ‘locked’ with high
concentrations of heparin to prevent blockages.
Non-accessible cap:
To deter inappropriate access of dialysis-
dedicated devices by clinicians who are
not dialysis-trained.
Hickmans
A large bore vascular access device commonly inserted into
the subclavian vein and tunneled through subcutaneous
tissue prior to exiting the body.
Commonly used for stem cell transplant, chemotherapy or when long-
term central venous access is required.
Anchored subcutaneously via a cuff attached
to the catheter.
• Sutured insitu
• Wide bore 9.5, 12F
• May be single, double or triple lumen.
• heparin-locked when not in use.
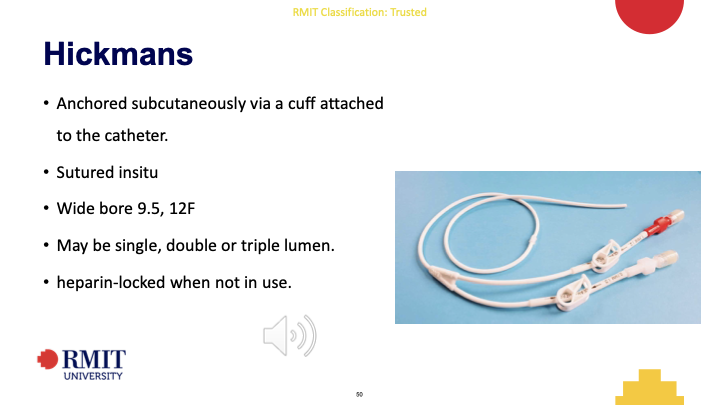
Hickmans Insertion
Inserted by radiologists on angio suit
• Inserted under local anesthetic with conscious sedation
• Tunneled catheter
• Cut to length internally
• Cuff sits at skin entry site.
• Flushed with 5mls 50,000 heparin per lumen
• Closed bung attached
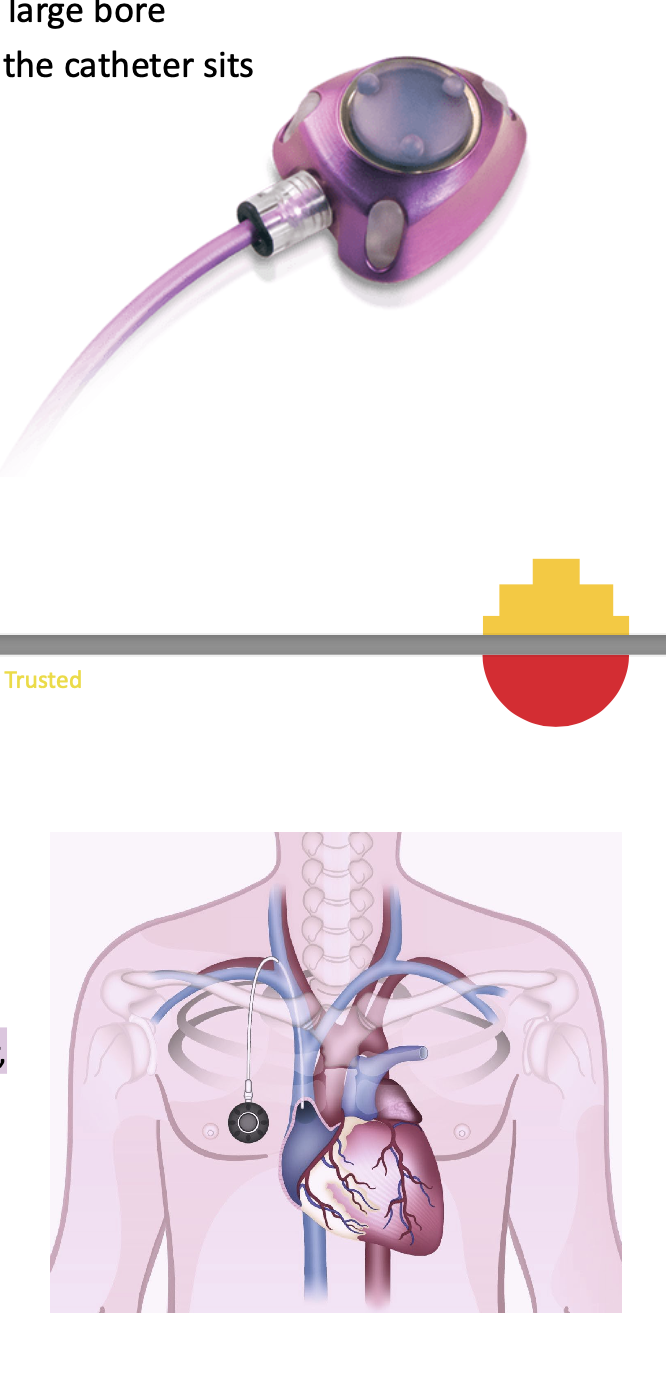
Portacath
A totally implanted vascular access device. Made up of a
silicone covered chamber that is attached to a large bore
catheter. The chamber sits under the skin and the catheter sits
in a central vessel.
• Commonly used when long-term central venous
access is required.
• 6F, 8F size
• Single lumen ports are the most common, however,
double lumen ports are available that have two
separate chambers.
• Inserted in the chest or upper arm.
• heparin-locked when not in use.
A port must be accessed with a specially
designed, non-coring needle (a port-specific
needle that will not damage the port
chamber).
Different non-coring needles are required for
pressure injectable ports – these are labelled
with how many mls/sec can be injected.
These specialised non-coring needles can be
used with any port, whether pressure
injectable or not
Portacath indications
Long term intravenous use
• Administration of chemotherapy
• Intravenous medications and fluids
• TPN
• Blood products
• Repeat blood sampling
Portacath insertion
Inserted in angio by an interventional radiologist.
• Two small cuts (incisions) will be made in the skin.
• The first is to access the IJV
• The 2nd is made to create a pocket under the skin for the
port.
• It will be about 3–4cm long. If the port is being put into a
vein in your chest, the incisions are made on your upper
chest.
• If the port is being put into a vein in your arm, they will be
on the inner side of your arm.
• The tube attached to the port will be tunnelled under the
skin and inserted into the IJV
Portacath – Power injection
nNot all ports are power injectable
• Important to check prior to use
• Ports can be accessed by appropriately trained nurses and medical staff
• Once accessed can be used by any staff appropriately trained to administer IV medications
• Different non-coring needles are required for pressure injectable ports
• these are labelled with how many mls/sec can be injected.
• These specialised non-coring needles can be used with any port, whether pressure injectable or
Tunnelled catheter complications insertion
Insertion
Puncture site haematoma
Infection
Perforation
Kinked catheter
Pneumothorax
Tunnelled catheter complications Positioning
Fibrin sheath
Too proximal – Brachiocephalic venous
thrombosis
Too Distal – arrhythmia
Tubes & Drains
NG tube
• ET tube
• ICC
• Nephrostomy
• Biliary drain
Nasogastric Tube
A NG tube is a soft flexible tube passed through the nose, down the throat and into the
stomach, it is used for the:
• Suction of gastric contents
• Delivering nutritional support and medications
• Gastric washout prior to surgery
NGT Complicatiosn and ideal pos
Complications
• Aspiration
• Intracranial perforation
• Pneumothorax
Ideal position
Dual purpose – Distal
to the gastro-
oesophageal junction,
proximal to duodenum
For feeds only – Third
part of duodenum
(Horizontal segment)
Endotracheal Tube
Ventilation of respiratory compromised
patients
• Various sizes 6,8,10,12F
• Anchored externally to the mouth or nose
• Inserted by anaesthetist/ trained medical
• Positioned at least 4 cm proximal to
tracheal carina (usually 6-8 cms)
Endotracheal Tube complications
Aspiration
• Pharyngeal perforation
• Oesophageal Intubation
• Malpositioning too high/low
• Over inflated balloon
Intercostal Catheter (ICC)
An intercostal catheter (ICC) or chest tube is put in between
the ribs into the space located between the lung and the chest
wall (pleural space).
• The chest tube drains the air or fluid/blood from the pleural
space.
Chylothorax: Collection of lymph fluid in the pleural space
Haemothorax: Collection of blood in the pleural space
Pneumothorax: Collection of air in the pleural space
• Chest drains should not be clamped unless ordered by medical staff
icc Ideal final position
To evacuate air – Most non-
dependant portion of the
lung
To evacuate fluid – Most
dependant portion
Surgical drains
Jackson-Pratt drain (JP drain) commonly placed post operatively to
drain fluid/blood from surgical site
• Nephrostomy is a drain tube inserted into the renal collecting system
to drain urine away from the urethra and bladder.
• Percutaneous biliary drainage catheter is inserted into the bile ducts in
the liver via a direct puncture through the abdominal wall
When transferring patients always be very careful to check for drains
and attachments.
Lines, tubes & Drains cont.
Oxygen
• Urinary catheter
• PIVC
• Art lines
• CVADS
• Ventilated patients
• Chest drains
• Feeding tubes
• Surgical drains
overview
ETT
NGT
Central line
Right subclavian CVC
Vas Cath
ICC x 4