Micro 8 | Gram-Positive Bacteria II
1/66
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
67 Terms
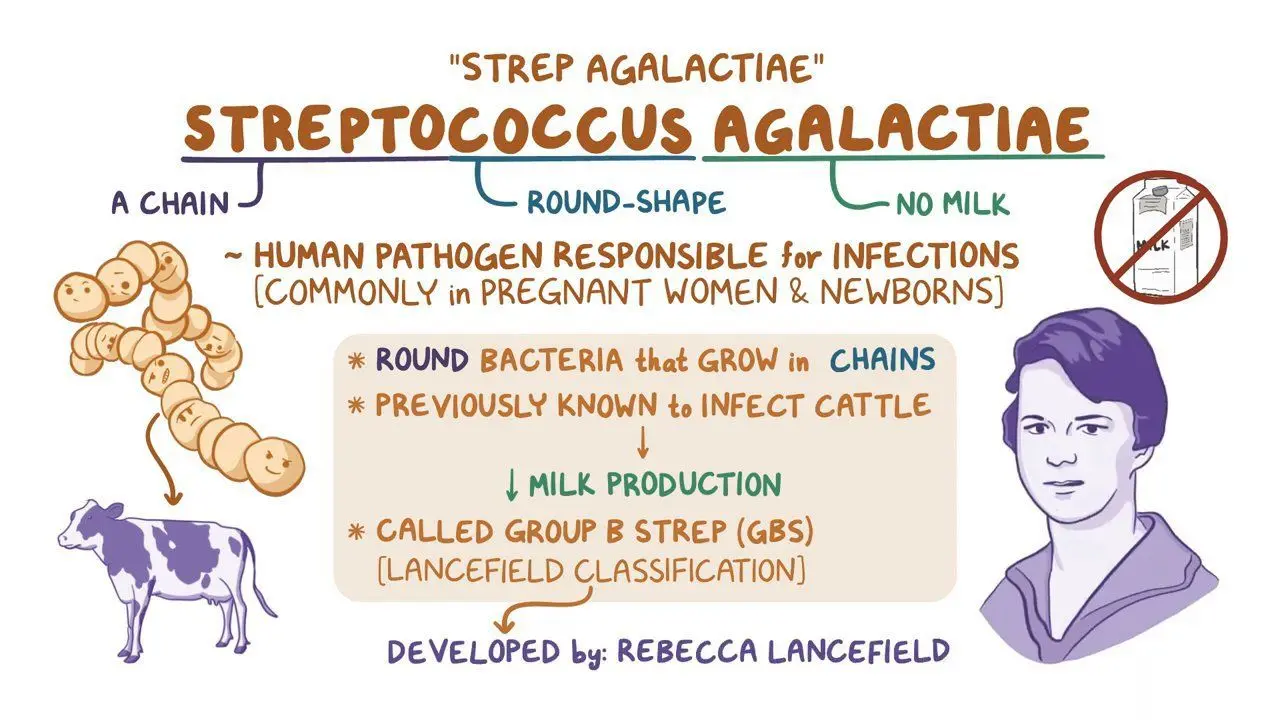
What is Streptococcus agalactiae commonly known as?
Group B Streptococcus
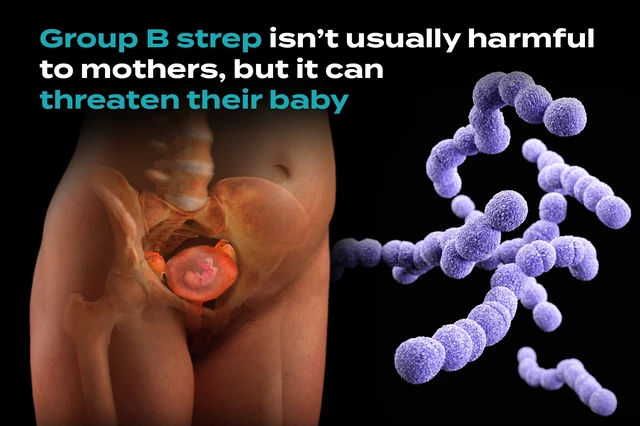
What is Streptococcus agalactiae?
A type of bacteria commonly found in the vaginal and intestinal tracts of healthy adults, particularly women. It can cause infections, especially in newborns, pregnant women, and individuals with weakened immune systems.
Where is Streptococcus agalactiae (Group B Strep) commonly found?
In the vaginal and oral flora of 15–40% of adult women.
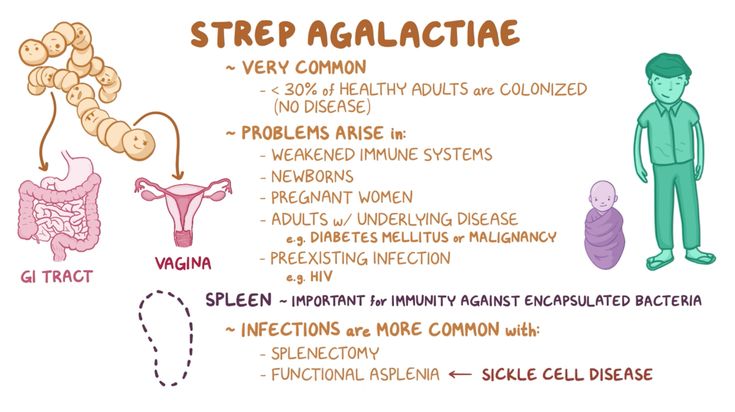
Presentation of early-onset neonatal disease caused by GBS?
Respiratory distress occurring at birth to 7 days, with high mortality.
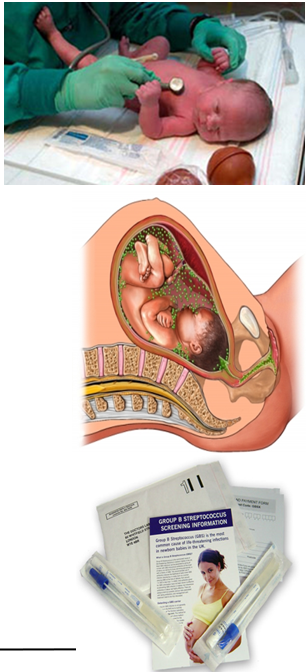
Presentation of late-onset neonatal disease caused by GBS?
Meningitis occurring at 7 days to 4 months, causing neurological damage and up to 20% fatality.
How can GBS neonatal diseases be prevented?
By screening pregnant women treating positives with intrapartum antibiotics.
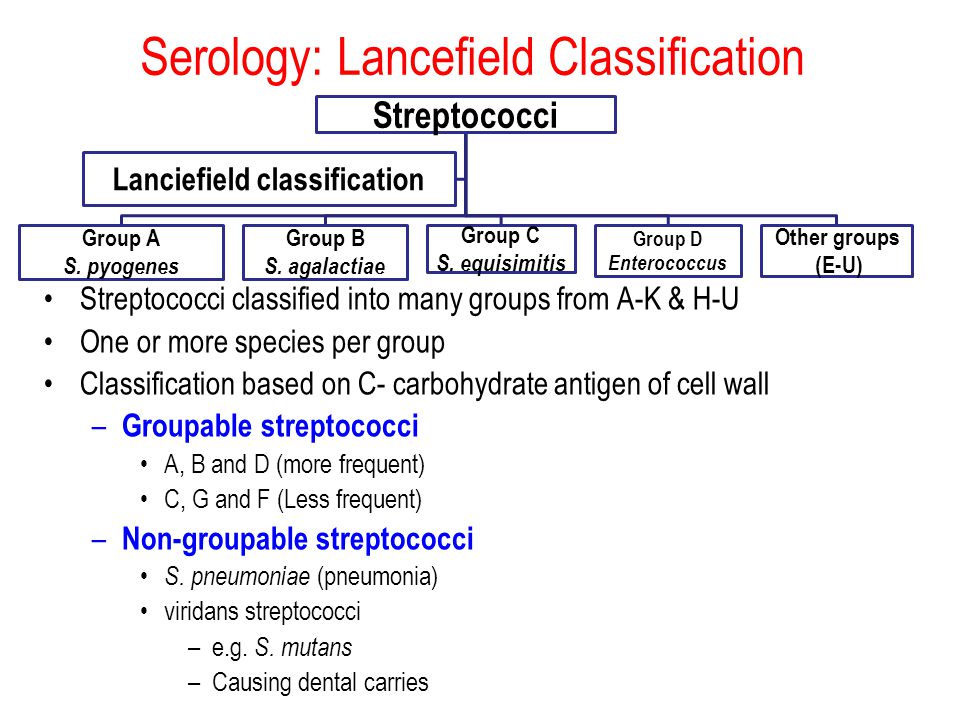
What Lancefield antigen is associated with S. agalactiae?
Group B antigen.
How does the polysaccharide capsule help S. agalactiae?
It inhibits phagocytosis.
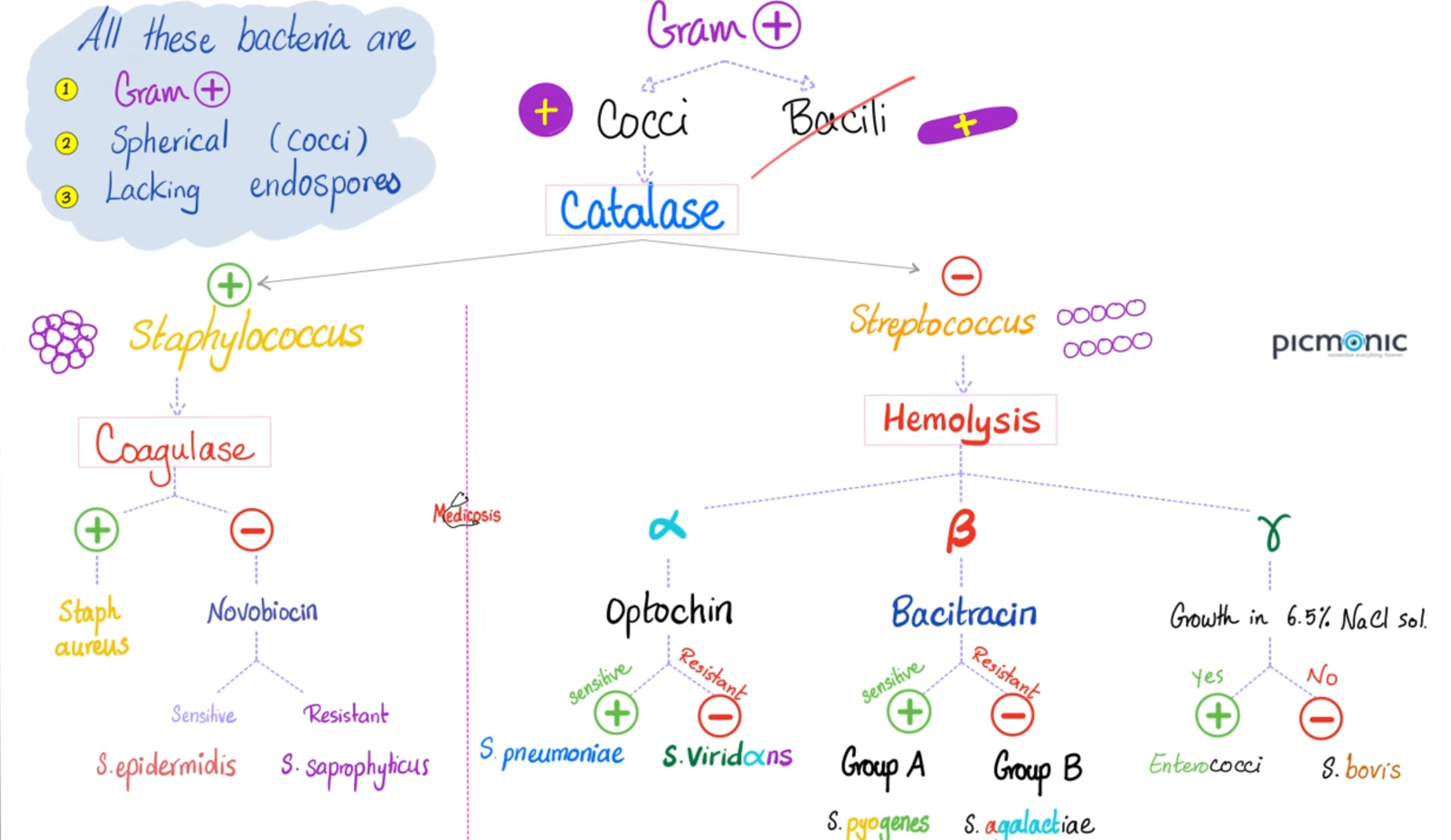
What is the shape and Gram stain of S. agalactiae?
Gram-positive cocci in chains.
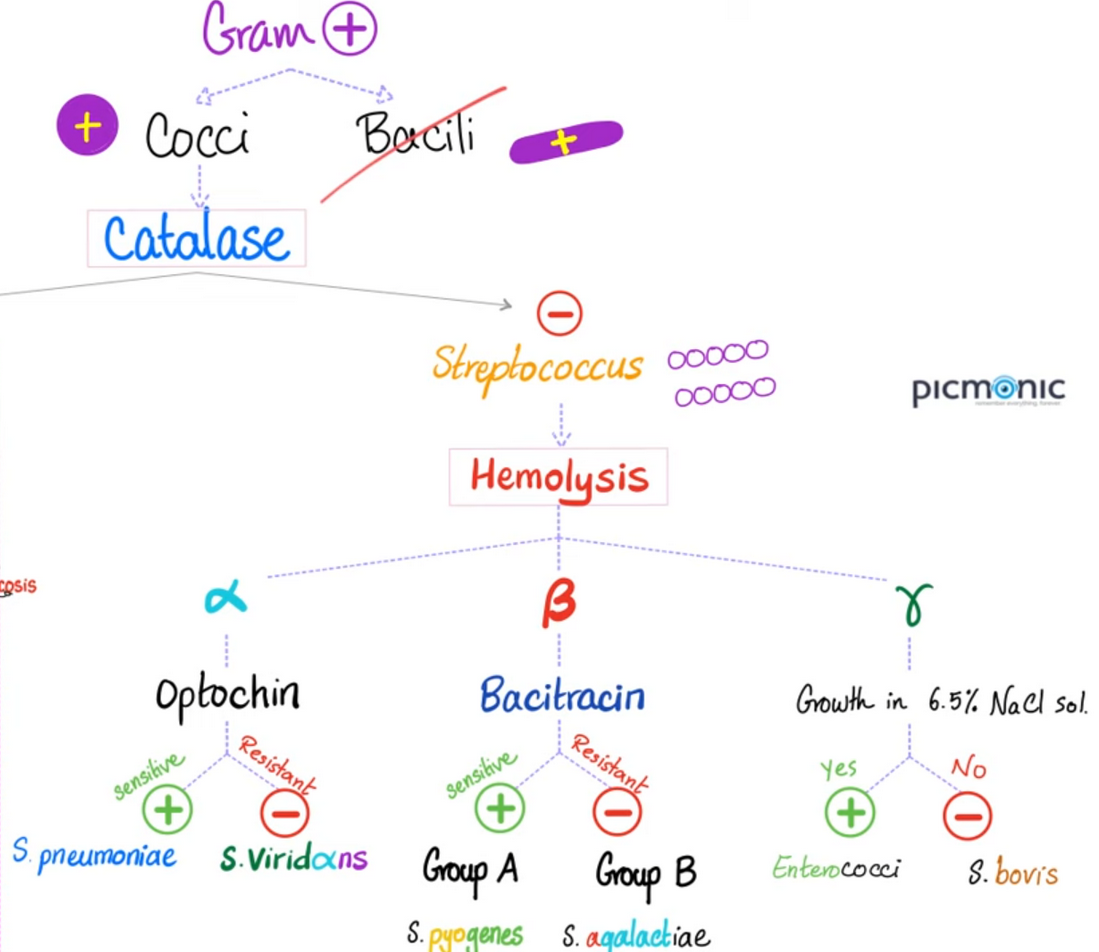
Is S. agalactiae catalase-positive or catalase-negative?
Catalase-negative.
Is S. agalactiae bacitracin-sensitive or bacitracin-resistant?
Bacitracin-resistant.
What type of hemolysis do Viridans Streptococci show?
α-hemolysis, which turns blood agar greenish.
What diseases are caused by different viridans streptococci species?
S. mutans: Dental caries and endocarditis.
S. mitis and S. salivarius: Endocarditis following dental procedures or oral trauma.
S. gallolyticus: Endocarditis, particularly in patients with colon cancer or GI trauma.
Where do Viridans Streptococci commonly colonize?
The nasopharynx, oropharynx, and GI tract.
What are the two main human pathogens among Enterococcus spp.?
E. faecalis and E. faecium
Where do Enterococcus spp. commonly colonize?
The GI tract
What makes Enterococcus spp. significant in healthcare settings?
They are among the top 5 causes of healthcare-associated infections, especially with urinary catheter use.
What are the key virulence factors of Enterococcus spp.?
Natural resistance to penicillin G and cephalosporins – enhances spread when antibiotic treatment eliminates other bacterial flora
Polysaccharide capsule for immune evasion
Natural or acquired antibiotic resistance.
Who is at higher risk of Enterococcus infections?
Patients with frequent or recent hospitalizations, weakened immune systems, or exposure to medical devices like catheters.
What causes Enterococcus infections?
The spread of endogenous bacteria to new sites, often after antibiotics kill normal flora.
What are the two most common diseases caused by Enterococcus?
Urinary tract infections and bloodstream infections (bacteremia).
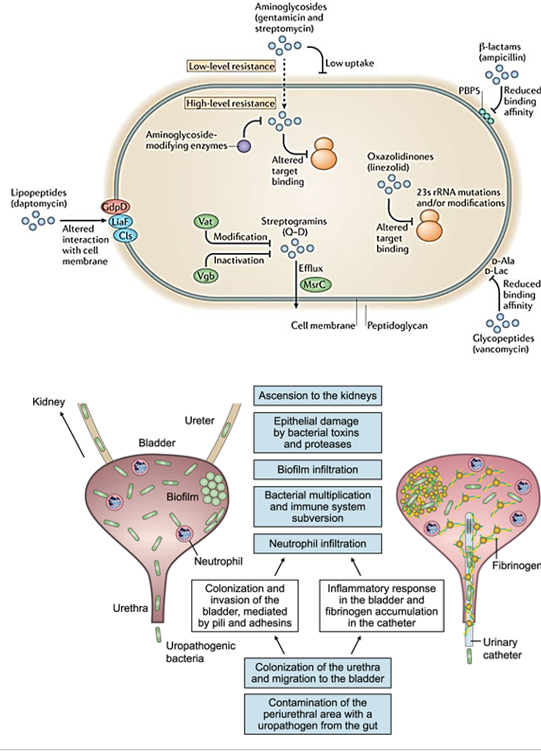
What medical device is associated with Enterococcus-caused UTIs?
Urinary catheters
What is bacteremia?
A bloodstream infection caused by bacteria entering the blood.
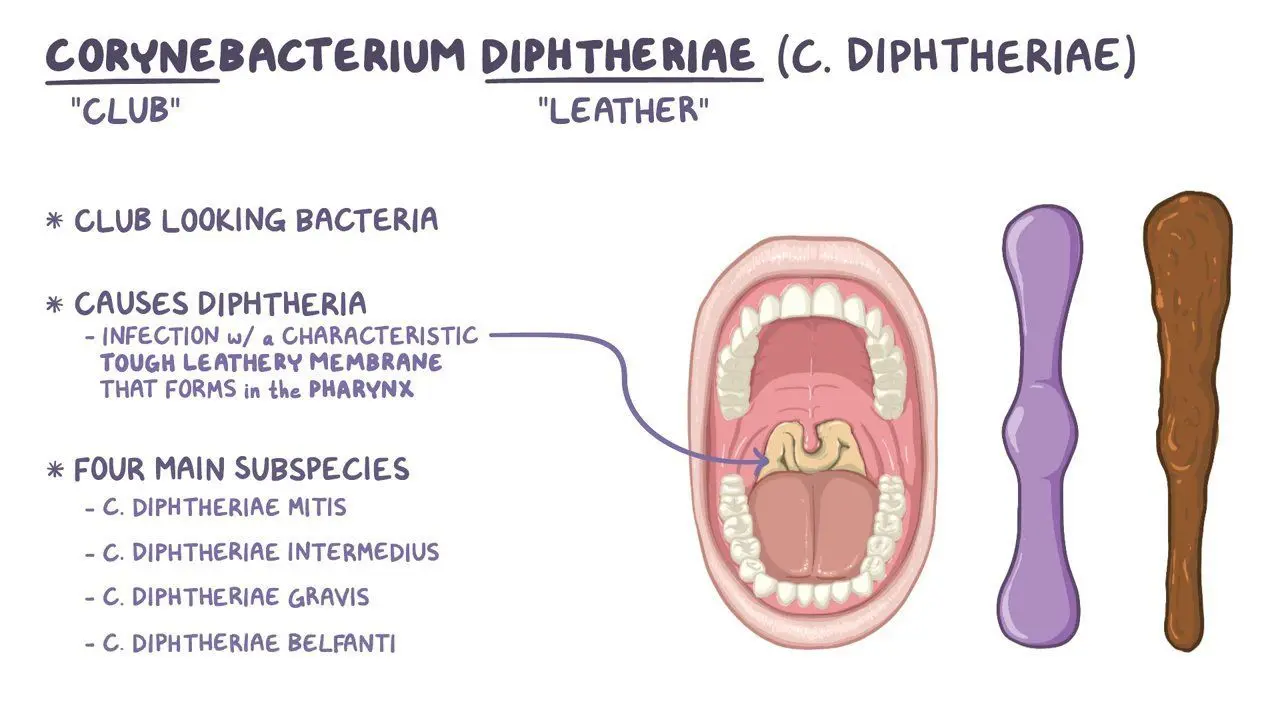
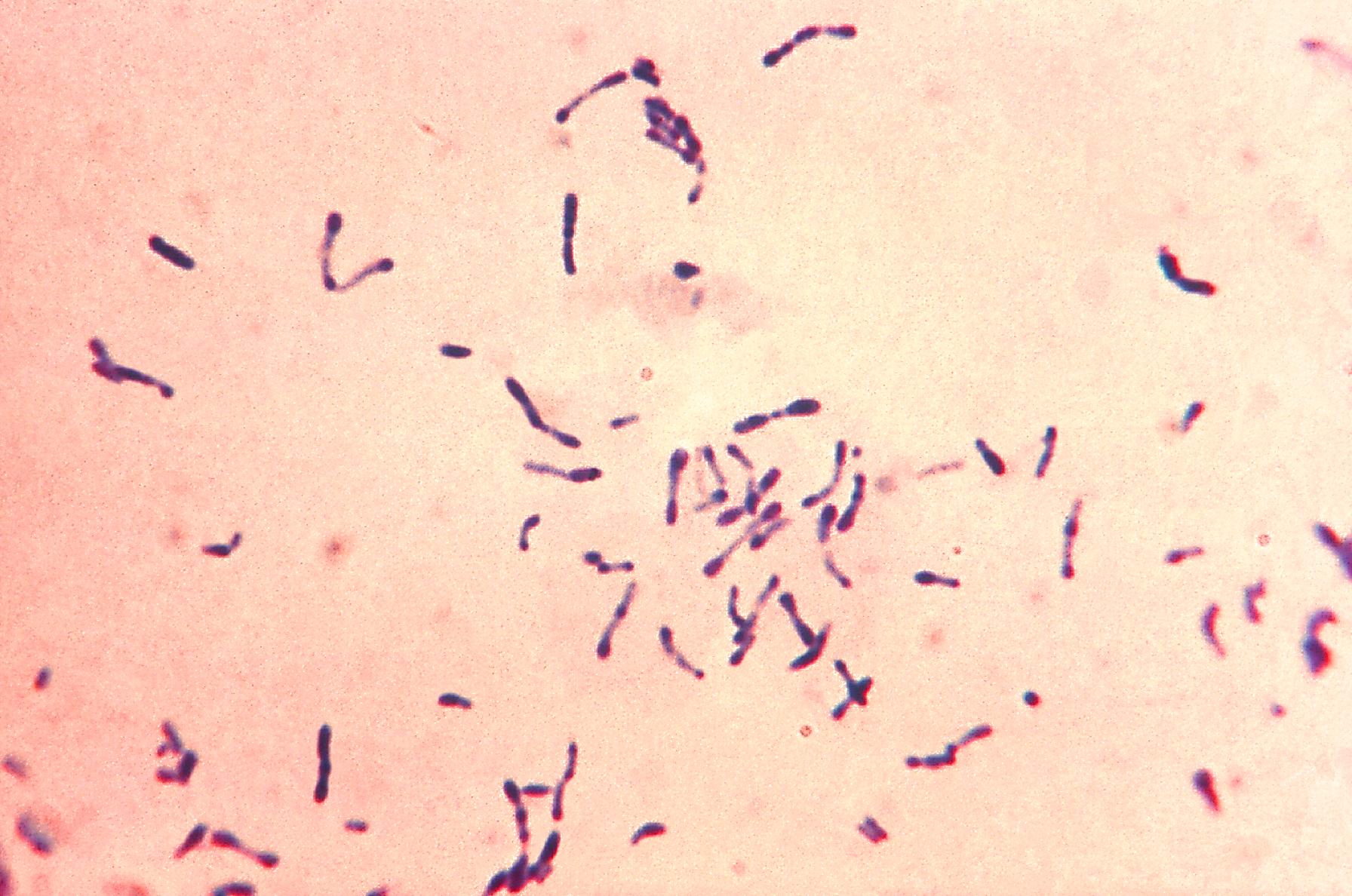
What type of bacteria is Corynebacterium diphtheriae?
Gram-positive bacilli with club-shaped rods
How is C. diphtheriae transmitted?
Through respiratory droplets.
What is the key clinical sign of diphtheria?
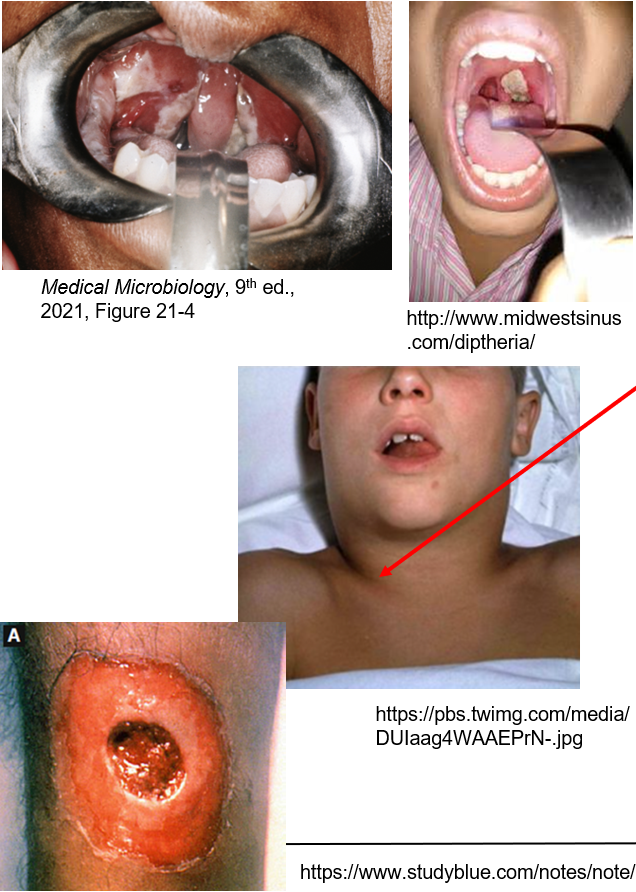
A grayish-white coating on the tonsils, uvula, or palate that bleeds when scraped & “bull neck” (swollen neck).
What risk factors are associated with diphtheria?
Lack of vaccination or travel to endemic regions.
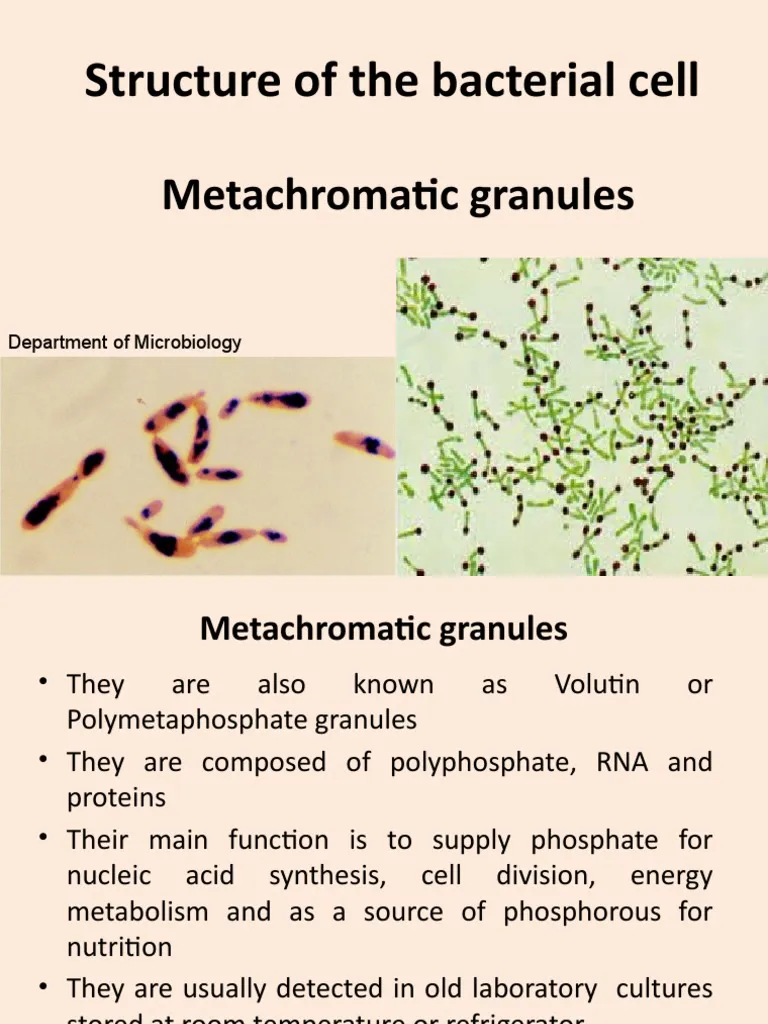
How can you identify Corynebacterium diphtheriae on a stain?
With metachromatic (blue and red) granules when stained with methylene blue
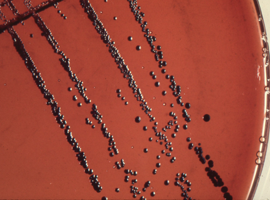
How can you identify C. diphtheriae on a culture
By its metachromatic granules and growth as black colonies on cysteine-tellurite agar.
What are metachromatic granules?
Granules that stain blue and red, characteristic of C. diphtheriae.
How does C. diphtheriae spread in the body?
Via the diphtheria toxin; Classic A-B Toxin
What does the B subunit of the diphtheria toxin do?
It binds to the DT receptor and triggers endocytosis, releasing the A subunit.
What is the role of the A subunit in the diphtheria toxin?
It ADP-ribosylates EF-2, blocking protein synthesis, causing cell damage and death.
What causes the "bull neck" appearance in diphtheria?
Local edema (swelling) in the neck.
How can diphtheria be prevented?
Through the DTaP vaccine, which includes the DT toxoid.

What type of bacteria is Listeria monocytogenes?
Gram-positive bacilli, facultative intracellular aerobe, grows in macrophages.
What unique conditions does Listeria monocytogenes grow in?
It grows well at 4°C and in high salt conditions.
Who is at high risk for Listeria monocytogenes infection?
Neonates, pregnant women, elderly individuals, and people with weakened immune systems.
What does CAMP activity indicate in Listeria monocytogenes?
CAMP activity shows better hemolysis when Listeria is grown with β-hemolytic S. aureus.
What type of motility is seen in Listeria monocytogenes?
Tumbling motility in broth culture.
How does Listeria monocytogenes infect macrophages?
It uses special proteins, Internalins A and B, to help it get inside immune cells called macrophages.
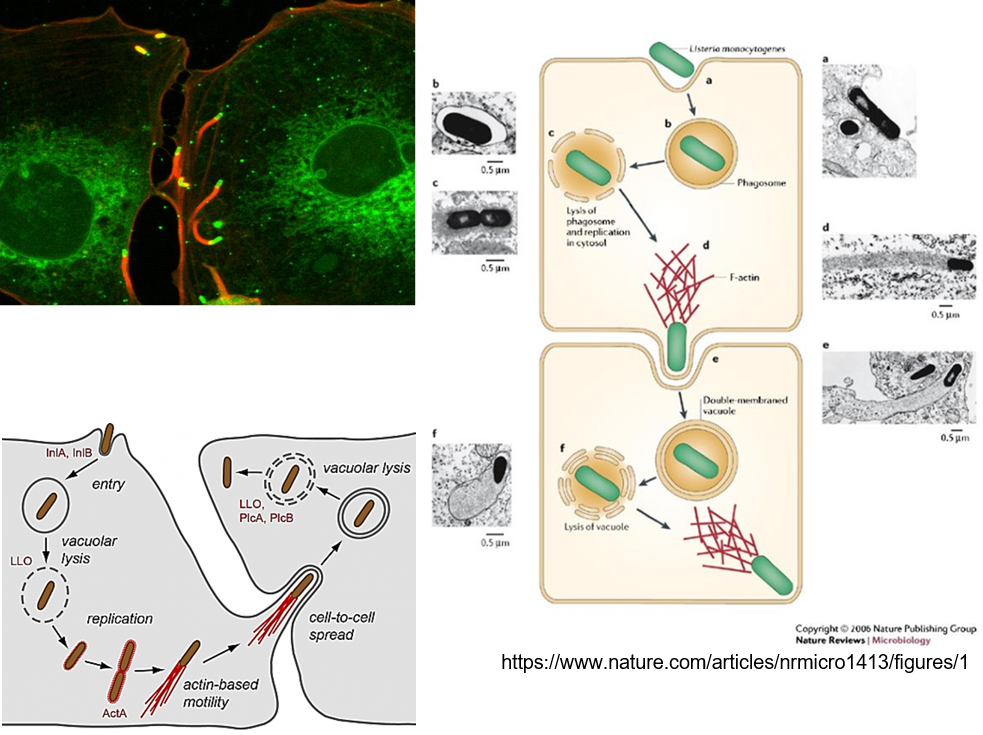
How does Listeria monocytogenes escape the phagolysosome?
It uses listeriolysin O (LLO) and phospholipase C (PlcA, PlcB) to prevent destruction.
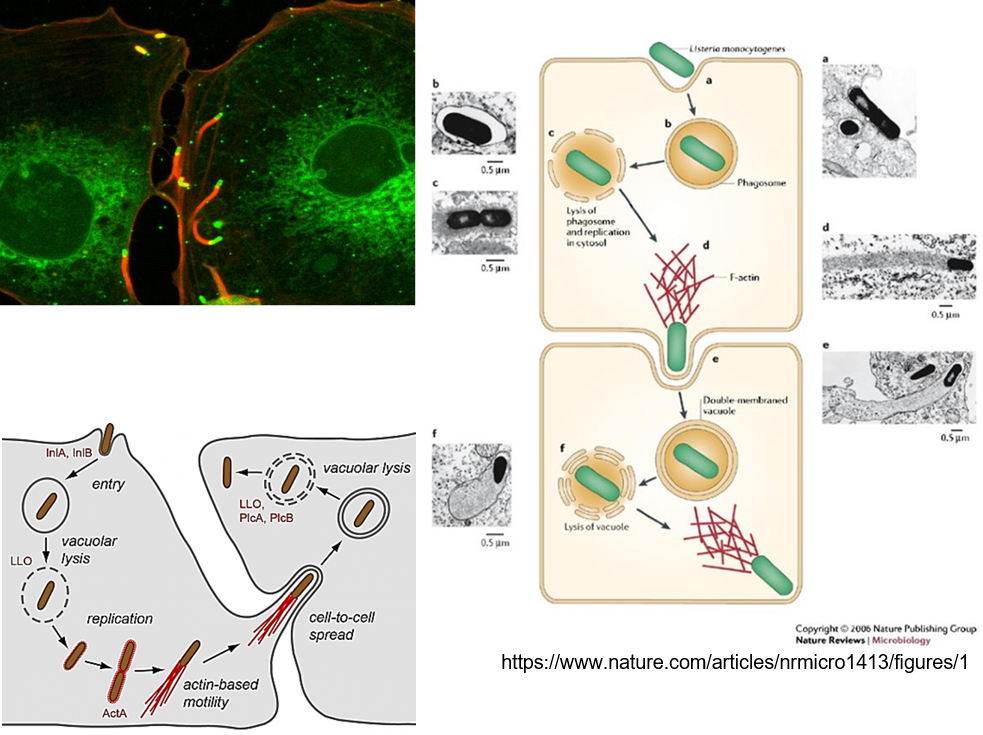
What is the function of the ActA protein in Listeria monocytogenes?
ActA reorganizes actin to form "rocket tails," enabling movement and cell-to-cell spread.
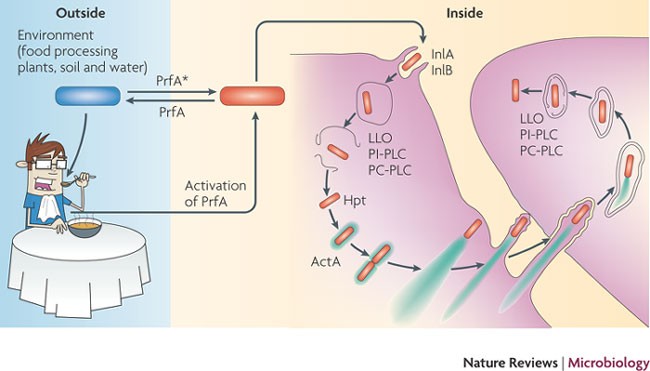
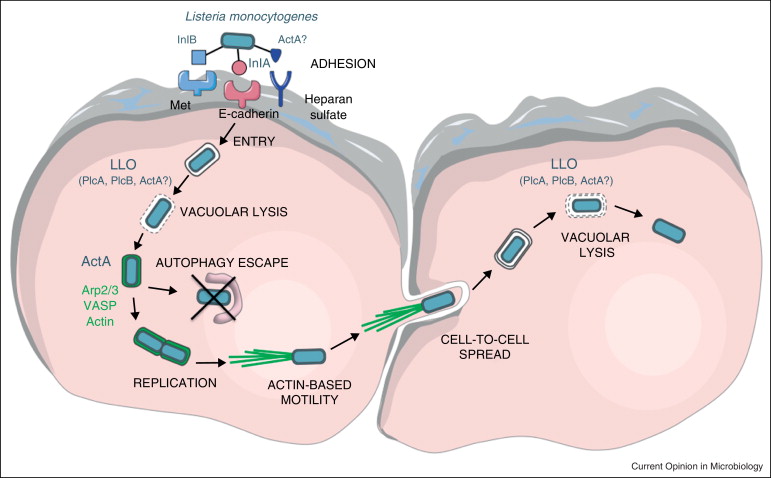
How does Listeria monocytogenes avoid immune defenses?
By using Internalins A and B to survive inside cells.
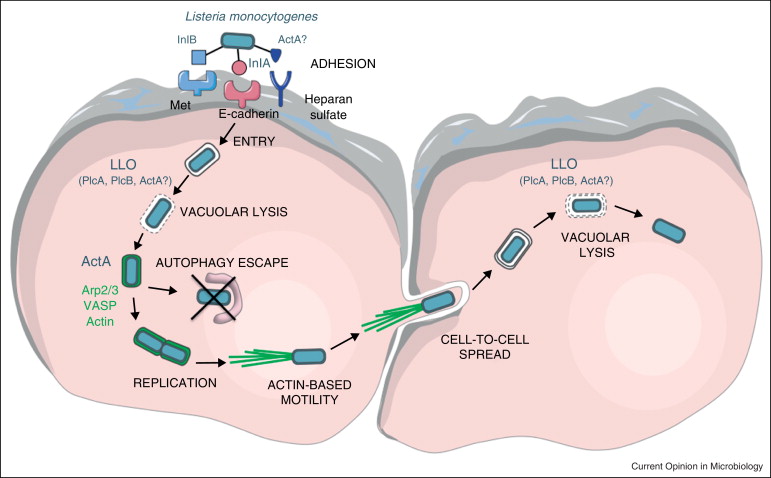
What helps Listeria monocytogenes escape destruction inside cells?
It uses Listeriolysin O (LLO), Phospholipase C (PLC A/B), and ActA.
Where can Listeria monocytogenes grow easily?
In cold temperatures and high salt environments.
What are the two forms of L. monocytogenes infections in neonates?
Early-onset (infection in the womb)
Late-onset (infection after birth).
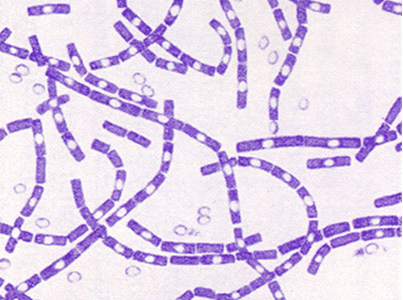
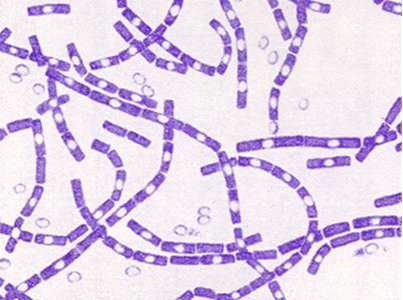
Which bacteria is a gram-positive, spore-forming rod (appearing in "boxcar" chains).
Bacillus anthracis
What symptoms does Bacillus cereus cause?
It causes vomiting or diarrhea, depending on the type of toxin.
How is Bacillus cereus transmitted?
It is transmitted through contaminated food.
What causes the emetic form of Bacillus cereus?
Caused by heat-stable enterotoxin from spores that germinate in food (e.g., rice, pasta).
What causes the diarrheal form of Bacillus cereus?
Heat-labile toxin produced when spores germinate in the intestine.
What foods are associated with the emetic form of Bacillus cereus?
Foods like rice and pasta held at warm temperatures.
How is Bacillus anthracis transmitted?
Spores enter through breaks in the skin, inhalation, or ingestion.
Sources include animals (goats, cattle, sheep) or occupational hazards (butchers, shepherds).
No person-to-person transmission; potential for bioterrorism.
Which bacteria has the potential to be used for bioterrorism?
Bacillus anthracis
What makes B. anthracis spores significant?
They are very tough and hard to inactivate.

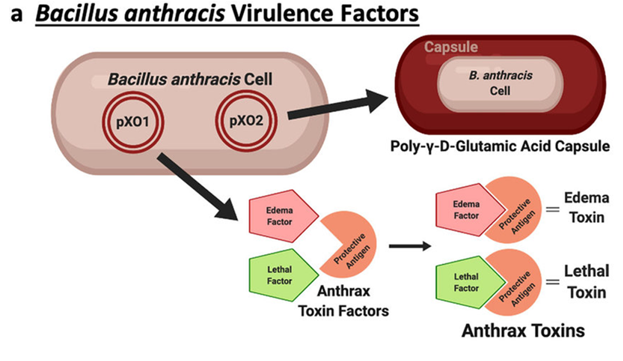
What is unique about the capsule of B. anthracis?
It is made of poly-D-glutamic acid.
Poly-D-glutamic acid capsule is a protective layer made of protein (not sugars, unlike most bacterial capsules) and is unique to Bacillus anthracis. It helps the bacteria evade the immune system by resisting phagocytosis (being "eaten" by immune cells).
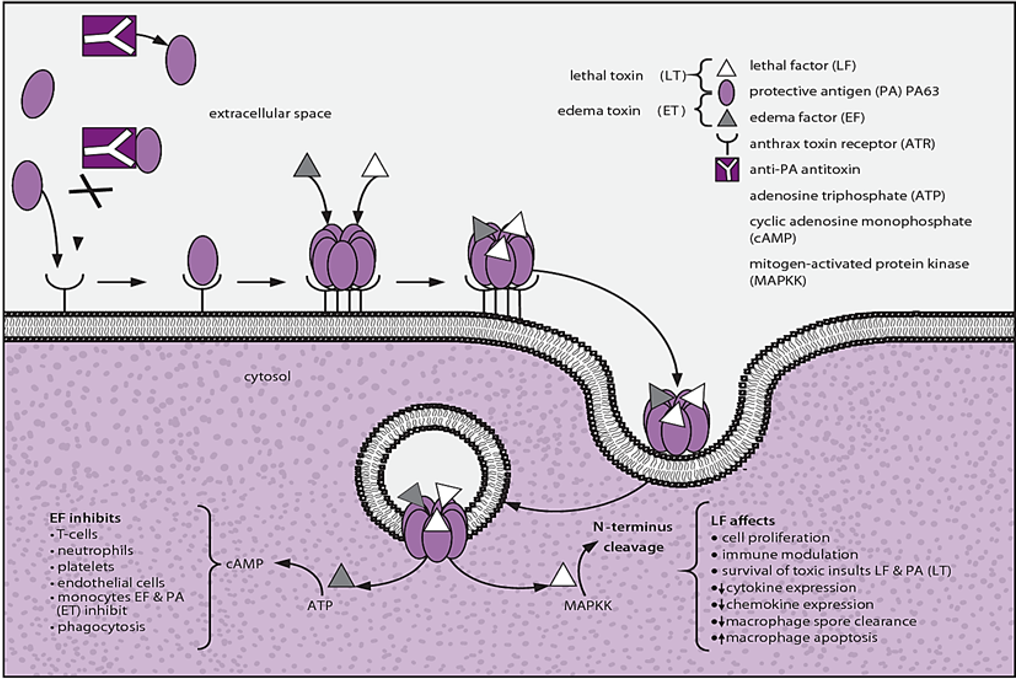
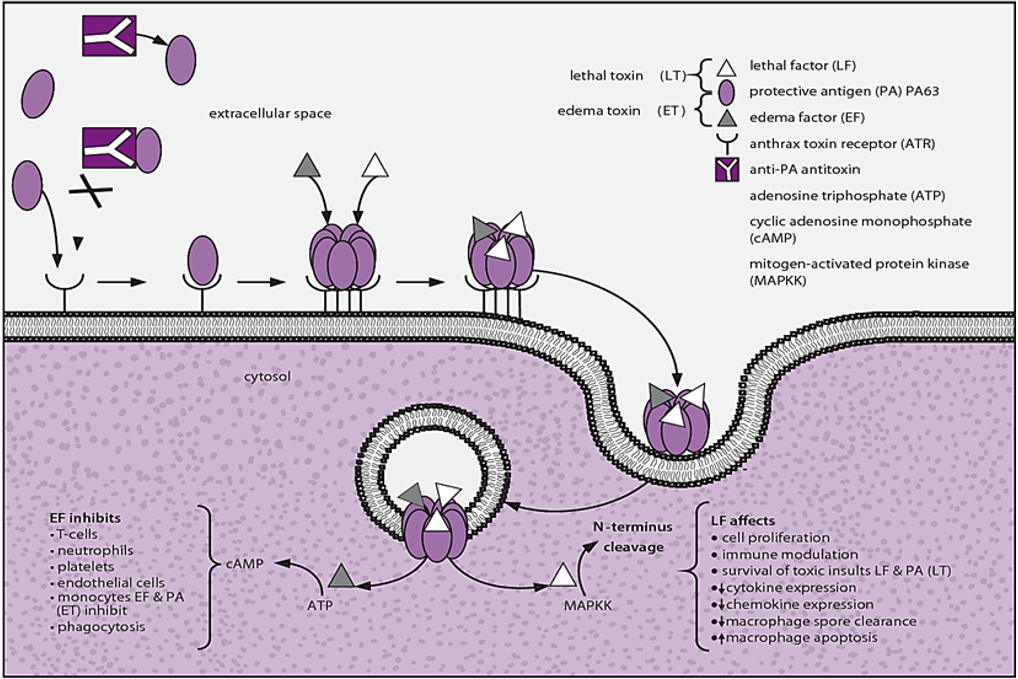
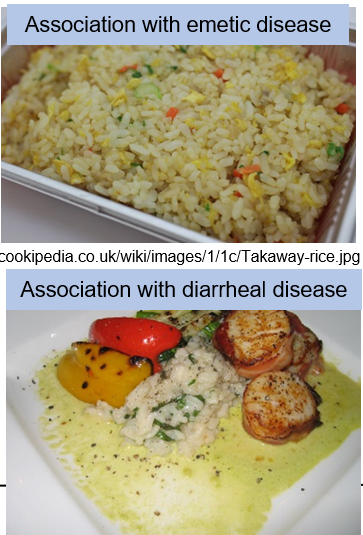
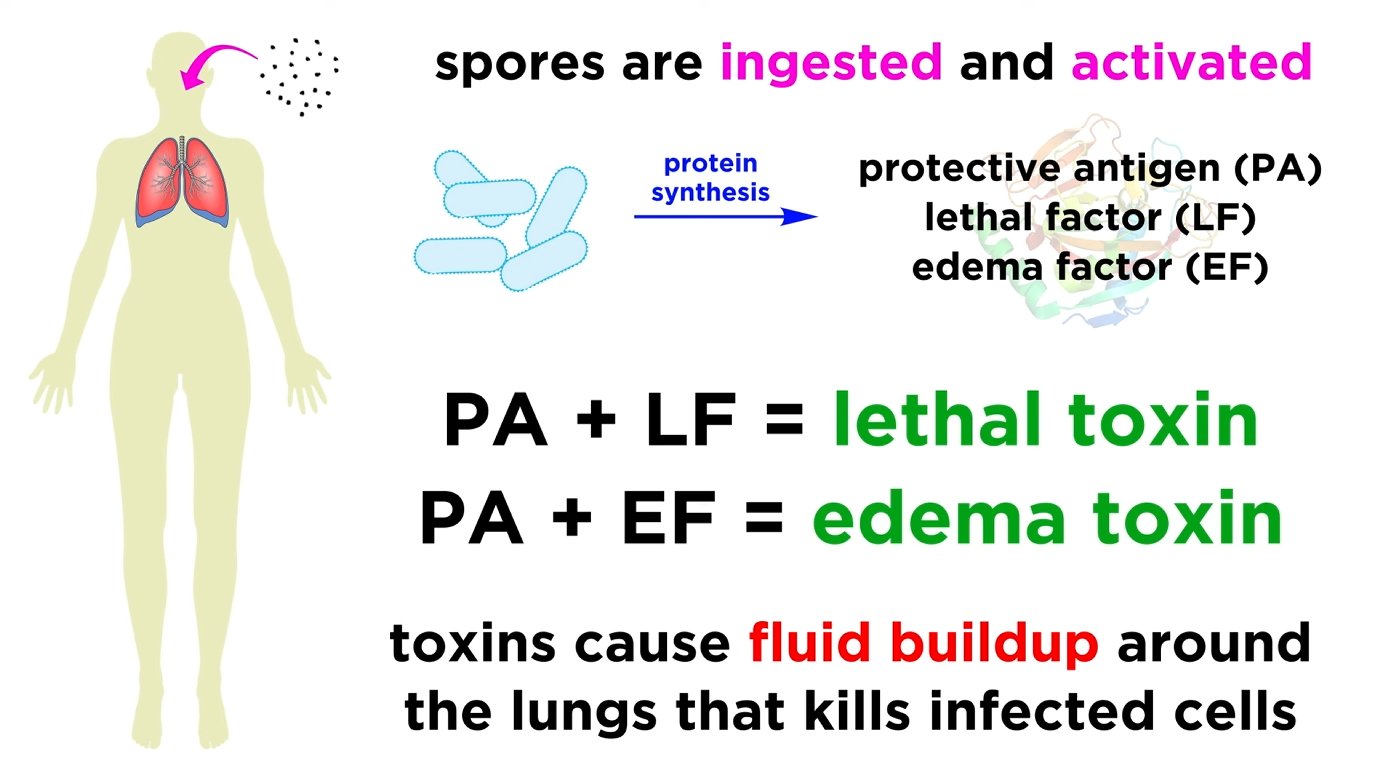
Three exotoxins then form 2 functional toxins formed by B. anthracis exotoxins. What are they?
Lethal Toxin (PA + LF)
Edema Toxin (PA + EF).
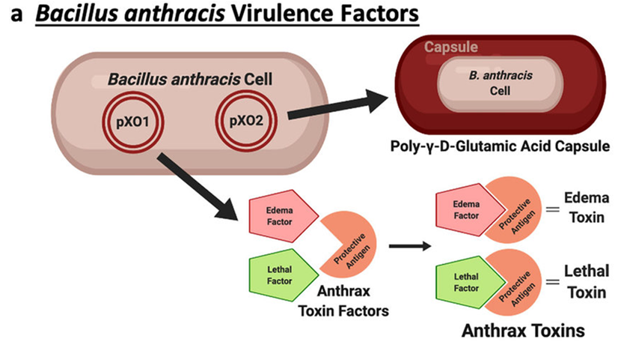
What does Protective Antigen do?
It binds to cell receptors and acts as a docking site for LF and EF toxins.
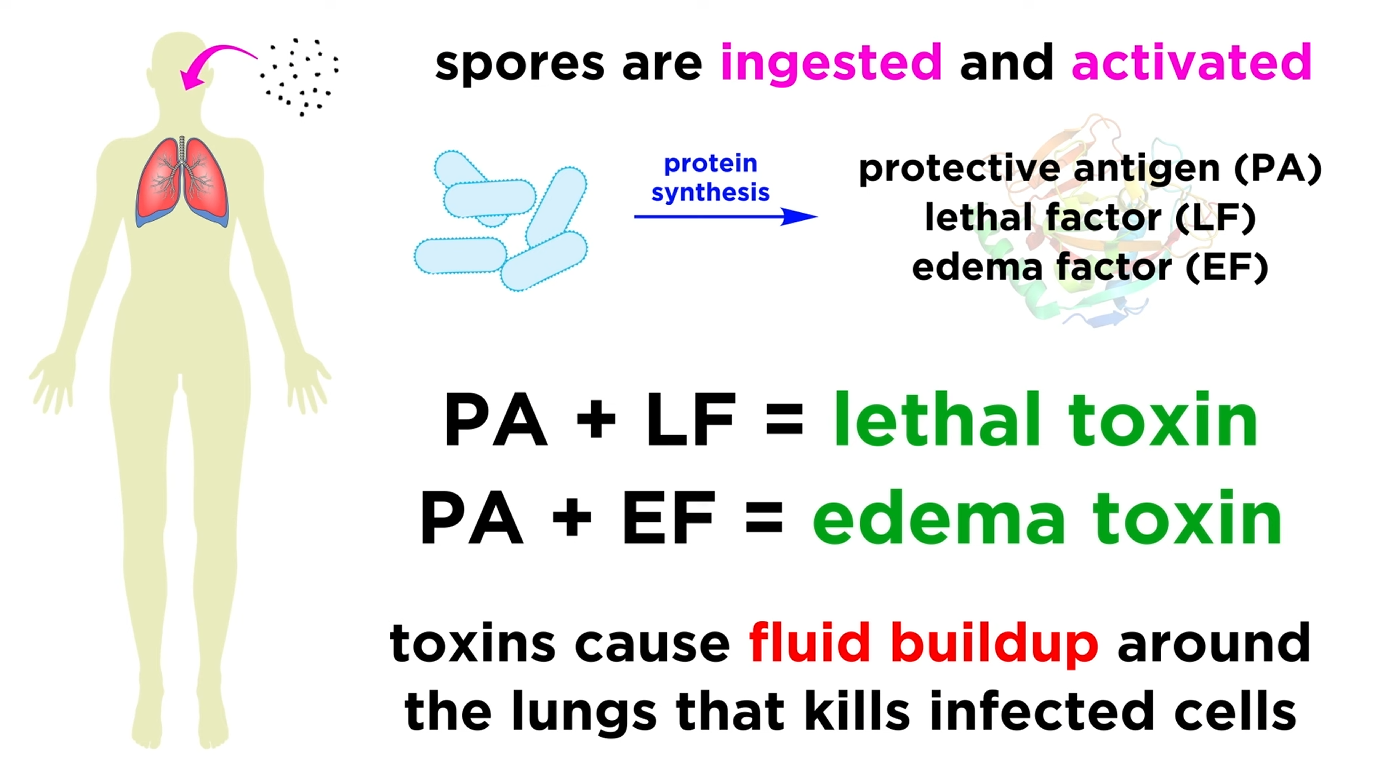
What are the toxic effects of Lethal Factor and Edema Factor?
EF: Increases intracellular cAMP, causing edema.
LF: Activates macrophages, leading to cytokine storm, apoptosis, and tissue necrosis.
Most common form of Anthrax?
Cutaneous Anthrax
When do symptoms occur in Cutaneous Anthrax?
Shortly after spores or vegetative cells enter a break in the skin.

Explain the disease process of cutaneous anthrax
Starts with a painless papule surrounded by vesicles.
Quickly progresses to an ulcer with a black eschar (tissue necrosis) and swelling (edema).
Rarely leads to bloodstream infection or death.

What is a characteristic symptom of Cutaneous Anthrax?
An ulcer with a black eschar and swelling (edema).

How do you contract Pulmonary Anthrax?
By inhaling aerosolized spores into the nasal passages or lungs.
What is the hallmark feature of Pulmonary Anthrax?
Mediastinitis, which is inflammation and enlargement of the mediastinal lymph nodes.