Lecture 14: Memory and Vaccines
1/46
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
47 Terms
Immunological Memory
The adaptive immune system’s ability to retain recognition of a specific antigen after initial exposure.
B- and T-cells that have the machinery to recognise a particular antigen are retained as memory cells.
These memory cells survive long-term after the infection is cleared.
If the same antigen is encountered again, they enable a faster and stronger immune response.
Phases of Protective Immunity
Protective immunity offers increased protection against pathogens that are encountered more than once.
Follows a three-phase progression:
Initial adaptive immune response – activates effector cells and produces antibodies.
Protective immunity – high levels of circulating effector cells and antibodies above a protective threshold, making them readily detectable.
Memory responses – over time, effector levels fall below the threshold, but protection is maintained by long-lived memory B and T cells that respond rapidly upon re-exposure.
Immune Response: First Vs Second Infection
First Infection: Ab and T-cell response takes time to peak and then gradually tapers off.
Second Infection: The Ab and T-cell response is much greater, with a steeper and higher peak, due to the memory of the immune system.
Features of Immunological Memory
Primary adaptive response to infection is often slow and weak.
Secondary exposure to the same pathogen: greater response
Secondary exposure is more rapid and better (has higher affinity and avidity of Abs) – has done the learning
Key Features Associated with Immune cells involved in memory, and Their Contribution to Immune Response
Adaptive Immune System (Acquired Immunity):
Expansion of clones of cells with re-arranged antigen receptor genes specific to the primary antigen encountered.
T-cells with antigen-specific TcR
B-cells with antigen-specific BcR/Ig
Enhanced Migration & Re-stimulation:
Increased adhesion molecules and rapid effector function allow for efficient circulation and movement to target sites for mounting an immune response.
Survival:
Maintenance of memory clones, which are responsive to growth and survival cytokine signals, ensures their presence for future immune responses.
Generation of Memory B-Cells
Increased numbers of antigen-specific memory B cells
Already undergone antibody class switch and affinity maturation
Can re-enter germinal centers during secondary immune responses to undergo additional somatic hypermutation and affinity maturation – helps produce more specific BCR
Not yet differentiated into a plasma cell (possible though)
Require help from CD4+ Th cells for secretion of Ab – don’t work in isolation
Maintenance of Memory T-Cells
Activation-Induced Cell Death (AICD):
Most activated (effector) T-cells are programmed to die after an immune response.
AICD helps regulate the immune response by ensuring that T-cells do not over-respond and cause damage.
Memory Cell Survival & Maintenance:
IL-15 and IL-7 are crucial for memory T-cell survival.
These cytokines promote homeostatic proliferation from stromal cells, ensuring the memory T-cells are maintained for future immune responses.
Memory T-Cells
Express high levels of IL-7R for survival and genes like bcl-2 for cell longevity.
High levels of adhesion molecule expression of CD44 to facilitate movement around the body.
Low expression of CD69, a marker for effector cells, indicates a resting state.
Memory cells located at the site of infection allow for a faster immune response without needing to travel.
Types of Memory T-Cells
Tissue-resident memory cells: Located at the site of infection (e.g., lungs during a cold) for immediate response.
Central memory cells: Adapted for recirculation through lymphoid tissue.
Effector memory cells: Ready to rapidly enter inflamed tissues for a quick response.
Useful to have memory cells at the site of infection – don’t have to travel to evoke a response
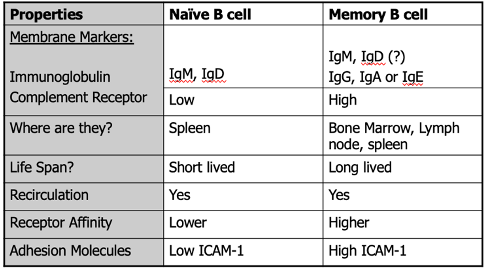
Features of Naive vs Memory B-Cells
Immunological Memory – Spanish Flu
32/32 patients born before 1915 who had Spanish flu in 1918/1919 had serum antibodies that bound to H1N1 haemagglutinin protein.
Had 90 years of B-cell memory against the Spanish flu – potential for immune memory to be lifelong
Memory B cells were isolated.
90 years of B cell memory!
Studies have also shown persistence of memory to smallpox 75 years post-vaccine
Importance of Immune Memory
It is a hallmark of adaptive and acquired immunity that allows for faster, stronger, and more specific immune responses upon re-exposure to pathogens.
Without Memory, acquired, antigen-specific immunity would be less effective.
Memory helps prevent prolonged risk during the primary immune response, which can be slower and weaker.
Acquired immune memory contributes to an increased healthy lifespan by offering quicker and more robust defences against recurring infections.
Protection From Immunisation and Vaccination
Immunisation (Vaccination) provides immunity to a pathogen before naturally encountering it protecting against illness without suffering the disease.
It prevents infection and its consequences (e.g., sickness or complications), generating immune memory for long-term protection.
Vaccination vs. Natural Infection:
Natural infection involves risking illness, whereas vaccination gives you information about the infection without causing harm, generating immune memory, helping you live longer with better immunity.
Variolation
Conducted for smallpox → Observations seen in the 1500s in Anceinet Iran, China, India
It involves ‘bursting’ of pustules and taking its contents and using it as an inoculum to treat someone else
Based on the idea that if the virus has been through an individual, then it had been weakened → would give an individual a weakened form of the virus (along with some immunity by passing on some Abs)
Concept of vaccine predates the discovery of the immune system, determined from observations
Mary Wortley Montagu
Introduced vaccination in 1717 to the UK → found out about the variolation process and brought it back to the UK
Risky → 1% death rate
Edward Jenner (1796)
Developed the first smallpox vaccine using the cowpox virus (vaccinia).
The word "vacca" is Latin for cow, reflecting the use of cowpox in the vaccine.
Jenner's Observation:
Noticed that people who had cowpox were resistant to smallpox.
Used variolation (introducing the virus to a person) on a child, which successfully protected them from smallpox.
Luis Pasteur (1879)
Developed vaccines based on preparations of weakened forms of pathogens- e.g. rabies and anthrax
Created weakened forms of a virus by passing them through different animals to create weaker/ attenuated viruses that could then be used to inoculate people
Modern Vaccines
Modern vaccines have been highly successful:
Work by generating protective antibodies & inducing T cell & B cell memory.
Vaccine Design
Requires 2 components
Antigens: From the target pathogen, either provided directly or generated by the recipient’s body.
Infection Signal: Activates the host immune system to respond.
Live and attenuated vaccines naturally provide both antigens and an infection signal.
Some vaccine platforms may require a boost to provide the infection signal - ADJUVANT
Some vaccines require multiple boosters to produce the most effective immune response.
6 main designs in widespread use
Live Attenuated Infection Vaccines
i. Related, less harmful infection:
Vaccinia (cowpox) is related to Variola (smallpox)
BCG bacteria (bovine tuberculosis) are related to Mycobacterium tuberculosis.
Highly effective, rarely found in nature, and dangerous to immunocompromised patients.
ii. Live attenuated pathogen:
Sabin oral Polio, MMR, chickenpox
Highly effective, with some risk of disease in immunocompromised patients
Killed or Inactivated Infection Vaccines
Salk Polio virus
Lower risk of disease, but can occur due to improper activation
May need boosters
Inactivating Viruses
Inactivated crudely via
Heat
Chemicals e.g. formaldehyde, beta propiolactone
Radiation
This preserves antigen structure, but the pathogen cannot replicate
Types of Modern Vaccines: Protein Subunit Vaccines
Use purified or recombinant protein components from the pathogen (e.g., Hepatitis B, Novavax vaccine for SARS-Cov-2).
These vaccines use the antigens that best stimulate the immune system.
May be combined with boosting agents (like bacterial stimuli) to enhance the immune response.
This allows the virus to be administered in various forms, such as in vaccines for HiB meningitis.
Types of Modern Vaccines: Recombinant Viral-Vectored Vaccines
Create a pathogen/virus that we haven’t been exposed to, e.g. non-pathogenic animal virus, and take out components and add in antigenic features that will stimulate a response to a virus
Bioengineered virus to express target pathogen antigens in vivo
widely investigated with good safety: e.g. Ebola vaccine
Often use non-human virus as carrier, e.g. simian adenovirus is used in AZ/Oxford Sars-Cov-2 vaccine
Can cause reactivity to carrier virus, so cannot use the same carrier repeatedly = poor response
Types of Modern Vaccines: Virus Like Particles
Highly effective, closely resembles live virus, but non-infectious – use of fake virus to transport components to the cells required
can contain multiple antigenic components.
e.g. Human papillomavirus (HPV) – Gardasil – helped to eradicate cervical cancer
Types of Nucleic Acid-Based mRNA Vaccines
Can encode many antigens (even the whole genome of pathogens!)
Antigen-encoding mRNA (or DNA) is complexed with a carrier such as lipid nanoparticles to be delivered into target cells
The antigen will then be transiently expressed by those cells, causing an immune response.
mRNA will naturally be degraded by protein-based nucleases, ribozymes → not continually expressed
Non-infectious and quick to manufacture and bulk up – good for booster shots
Can be tricky to store as it requires cold chain – must have the infrastructure to transport and store
e.g. SARS-Cov-2 vaccine made by Moderna and
mRNA Vaccines
Used for cancer – 2024 showed success in trails for lung cancer, melanoma, and other solid tumors as they’re easy to manipulate
Adjuvants
“Helper” chemicals boost immune responses to an antigen
Stimulate inflammation and antigen presentation to activate antigen-specific T cells
e.g. Oil/Water emulsion, Alum (Aluminium Hydroxide), TLR ligands, liposomes
Can increase immune responses, BUT can cause adverse immune pathology, including organ damage, septic shock, and autoimmunity.
Factors Affecing Vaccine Efficacy
Depends on the individual’s MHC type; not all antigens are immunogenic in every person.
Some pathogens mutate rapidly or go through multiple life cycle stages, making it difficult to target them effectively.
May be avoided using multivalent vaccines
Multivalent Vaccines
Deliver a variety of antigenic epitopes with an adjuvant to trigger a range of protective immune responses
May be useful for infections that mutate rapidly e.g. flu and viruses that cause common colds and COVID-19
Mucosal Vaccines
Delivered through the nose or throat as a sniffable or inhalable formulation
Designed to target specific tissue where a tissue-resident memory response is required - may be more effective in protecting against mucosal-based infections
May be more effective than conventional vaccines( systemic but not a tissue-targeted/ specific response)
Potential virus blocking for e.g. respiratory viruses
Potentially more durable i.e. long-term memory
Used for e.g. flu and investigated now for COVID-19 with some countries using
Benefit of Mucosal Vaccine Delivery
Combining vaccines with this delivery system can help target complex or difficult-to-target infections, such as RSV (Respiratory Syncytial Virus).
Recent Example:
The recent roll-out of the RSV vaccine demonstrates the potential effectiveness
Why are some diseases difficult to target with a vaccine?
Many diseases are caused by complex pathogens that have difficult-to-understand lifecycles, making it challenging to develop a vaccine.
TB has a long latent phase, which makes it difficult to identify infected individuals and target them with a vaccine.
The MMR vaccine is heat-sensitive and cannot be transported effectively to hot climates, limiting its accessibility.
Lack of an Effective Vaccine for TB and HIV
Tuberculosis
Around a quarter of the global population is infected with TB.
There is no effective vaccine currently available for TB.
TB research is limited/ poor because TB often remains latent, due to granulomas formed by macrophages
HIV and TB Coinfection:
Approximately 40 million people have HIV, and 25% of these individuals have latent TB.
5–10% of people with latent TB will develop active TB (10.8 million cases).
Individuals with HIV have a 16-fold increase in the risk of developing active TB.
Why Do So Many Diseases Lack Vaccines
Lack of understanding of the infection's life cycle or immune response to pathogen
In some cases, diseases have a complex life cycle with stage-specific immune responses (e.g., malaria).
Poor models to study certain diseases.
Limited understanding of the immune response to the pathogen and its major antigens.
Pathogens like HIV undergo frequent antigen variability, making it hard to create a universal vaccine.
Lab Model Limitations: difficulties mimicking the human immune response in labs.
Animal models (e.g., monkeys) are restricted and raise ethical concerns.
Transport/ lack of medical centres/ trained staff, e.g. poor infrastrucutre and storage issues, especially for vaccines requiring a cold chain.
High costs of vaccines, make them inaccessible for many populations.
Even if vaccines are available, they may not be accessible to everyone due to financial or technological constraints.
Why is there a lack of research into certain diseases?
Recent epidemics of neglected tropical diseases and zoonotic infections highlight the need for more research and infrastructure into these areas.
Some diseases, like the Zika virus, lack enough funding for research.
There is an increase in the number of zoonotic infections, which include diseases like Marburg virus.
Examples of Zoonotic Infections
Ebola, Monkeypox, Bird Flu (H5N1), and SARS-Cov-2 are examples of diseases transmitted from animals to humans
One Health
A concept that emphasises the interconnection between people, animals, plants, climate, and their shared environment to achieve optimal health outcomes.
Reasons for Rise in Vaccine Hesitancy and Decline in Vaccine Uptake
Socioeconomic factors
Social influences
Trust
Accessibility
Confidence- in healthcare/technology etc
Complacency- perception of risk is skewed
Convenience- difficulties accessing services etc
Communication-how accessible services/info
Context- recognising cultural needs
6 Themes Surrounding Vaccine Trust
1. Control: the idea that we can take back control of our own bodies through alternative means– the idea of being natural
2. Parenting style: philosophies that shun mainstream medicine, opting for “natural” remedies.– the idea that nature is best (wellbeing market)
3. The Past: previous bad healthcare experiences or a bad experience around vaccination shape perceptions. = hesitancy; ill near the time of vaccine and have linked the two
4. Risk: misunderstandings about the risks of vaccination versus the risks of disease.
5. Fear of chemicals: the fear that the vaccine will introduce toxic chemicals – dialogue with the use of mercury in the vaccine
6. Distrust of government agencies and corporations
Population (Herd) Immunity
A certain proportion of the population must be immune (through infection or vaccination) to protect others from a pathogen, especially those who cannot be vaccinated (e.g. due to age or allergies).
Helps control the spread of infection and protects vulnerable individuals.
Effectiveness depends on:
The virulence of the pathogen.
The susceptibility of the population.
Example: The MMR vaccine requires a high level of __________ to be effective in preventing outbreaks.
Andrew Wakefield
Hypothesised in 1998 that MMR was linked to autism.
His work was proven fraudulent, unethical, and the work was retracted, and he was disbarred
His legacy persists, and the rise of vaccine hesitancy and the “anti-vax movement has contributed to a reduction in vaccine uptake
Multiple studies have been conducted since (over 1 million children).
No study has replicated his findings
Measles cases in Europe have risen 30-fold, and there have been alarms about growing numbers of cases in England
1 in 5 children are currently unprotected against measles, due to hesitancy and low vaccine uptake
The World Health Organisation has said vaccine hesitancy is one of the 10 biggest global threats to health.
Measles Case Reugence
Outbreaks in Ireland and the US – particularly in areas of low vaccination uptake
Problematic as the MMR vaccine requires a large population to be vaccinated to achieve herd immunity
Largely occurred in response to Andrew Wakefield
Misinformation
False or inaccurate information—getting the facts wrong
Occurs accidentally - Social and general media play a critical role in its spread
Disinformation
False information which is deliberately intended to mislead—intentionally misstating facts
This can be a VERY lucrative initiative e.g. alt cures, sponsorship speaker fees
Social and general media play a critical role in its spread
Disinformation Dozen
12 people are responsible for almost two-thirds of anti‑vaccine content circulating on social media platforms
Vaccine Messaging and Misinformation: Pro-Vaccine vs Anti-Vaccine
Pro-vaccine groups have a simple message:
→ “Vaccines work and save lives.”Anti-vaccine narratives are more varied and emotionally driven, including:
→ Concerns about children’s health
→ advocate alternative medicine
→ Belief in conspiracy theoriesThese messages fuel hesitancy and play into concerned narratives.
Anti-vaccine content spreads more widely, appearing across more Facebook clusters than pro-vaccine messages.
Algorithms amplify this disinformation by rewarding content that gets clicks, reactions, and shares, making it more visible and influential.