A+P TEST 2: SKELETAL TISSUE
1/117
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
118 Terms
How many bones are you born with?
270
What are the two regions of the skeleton
Axial skeleton and appendicular skeleton
How many bones do you have by adulthood
206
What are the different shapes of bones?
Long, Short, Flat and Irregular bones
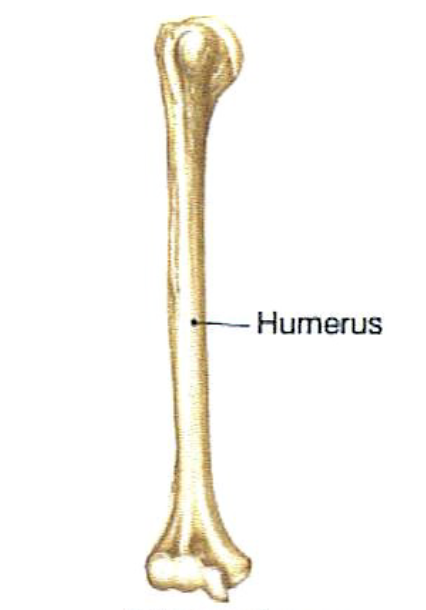
Long bones
Longer than wide
All limb bones except → patella, wrist bones and ankle bones
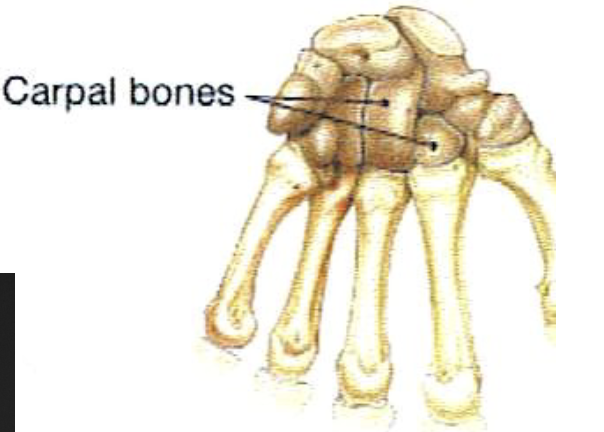
Short Bones
-Cubed shaped
Wrist and ankle bones
Sesamoid bones which includes the patella
Flat Bones
Thin, flattened and curved
Sternum
Scapulae
Ribes
Most of the skull bones
Irregular bones
Do not fit any of the other bone classification
vertebrae
hip bones
Compact Bone
external layer
appears to be solid and smooth
relatively dense
covers areas where there may be spongy bone
Spongy Bone
honeycomb structure (mesh like )
Open spaces between the traceculae are filled with marrow
Spicules : delicate slivers of bone , spines or rods
Trabeculae
small needle-like or flat pieces
Contain irregularly arranged lamellae and osteocytes interconnected by Canaliculi
Aligned along stress lines
Diaphysis
Shaft that forms the axis of the bone
Medullary Cavity
central canal surrounded by a collar of compact bone , contain bone marrow
True or False: The Shaft of the Long bone is thicker
TRUE
Epiphyses
bone ends
surface is covered by articular cartilage
Thin layer of compact bone
Interior contains spongy bone
In childhood the epiphyses and the diaphysis are separated by an
Epiphyseal plate, which become fused to form an epiphyseal line in adulthood
Metaphysis
refers to the epiphyseal plate or epiphyseal line
Periosteum
Double layered membrane that surrounds the bone
What are the two layers of the periosteum
Fibrous layer —> outer layer consisting of dense irregular connective tissue
Osteogenic layer —> inner layer of the periosteum consisting of osteoblasts and osteoclasts
The periosteum is richly supplied by…
Lymphatic vessels, nerve fibers and blood vessels
Perforating Fibers
Tuffs of collagen fibers that extends from fibrous layer to the bone
Endosteum
Delicate connective tissue membrane
-covers trabeculae of spongy bone
covers canal system of compact bone
True or false, bone marrow is present in spongy bone
True
Where is red bone marrow ( red marrow cavities) found
In the trabecular cavities of long and short bones
In infants what bone marrow is present ?
Red bone marrow In spongy bone
Where is blood produced in bones
in the head of the femur and humerus and flat bones and some some irregular bones
True or false: Yellow marrow can’t convert back to red marrow cavities during anemia
False
Osteogenic cells
Endosteum / periosteum
Gives rise to osteoblast
Osteoblast
synthesizes organic matter of matrix \ later hardens
Reinforces bone
Secrete osteocalcin ( insulin secretion)
Osteocytes
Former osteoblast
matured bone cells that occupy lacunae at junctions of lamellae
Trapped in matrix they produced ( lacunae)
Canaliculi - connect lacunae
cytoplasmic process
Reabsorbs / deposits bone matrix
Osteoclast
Bone dissolving ( crush, chew) surface of bone
Developed from bone cell stem cells
Bone remodeling
Why does the ruffed border face the bone
To increase the surface area of the osteoclast and resorption bays
What’s makes up bone ?
Osteoid and hydroxyapatite’s
Osteoid
Makes up 1/3 of matrix ( mass)
Ground substance and collagen fibers
Hydroxyapatites
Calcium phosphate
Gives bone exceptional hardness
Osteon or Haversian system
Structural unit of compact bone
Osteon
Elongated cylinder that runs parallel to the long axis of the bone
Weight bearing pillars
Growth rings called lamella
Haversian or central canal
Runs through the Osteon and contains small blood vessels
Perforating canals ( volkmann)
Run perpendicular to and interconnect the central canal
Concentric lamellae
Layers of matrix around central canal
Interstitial lamellae
Incomplete lamellae lying between Osteons
Circumferential lamellae
Located deep to the periosteum and endosteum
Canaliculi
Tiny canals that connect osteocytes to each other and to central canals
Intermembranous Ossification
Process of developing bone from fibrous membrane
Forms the flat bones : clavicles and the cranial bones of the skull
Frontal, temporal , occipital, and parietal
Before 8 weeks what does the skeleton look like
Fibrous membrane
Mesenchyme
Sheet of vascular tissue
What do the mesenchyme cell do
The mesenchyme condenses, the cells of mesenchyme line up around the vessels
Become osteoblast
Secrete Osteoid tissue
soft collagenous
Resemble bone but not calcified
What happens during mineralization of intramembranous ossification
Osteoid tissue hardens and continues to trap vessels and osteoblast in the hardening matrix
Process is occurring in adjacent tissue ; forms periosteum
Hardening matrix starts to take shape of trabeculae
Osteoblast are constantly depositing bone
fill in the spaces between trabeculae
create zone of compact bone
give rise to flat bone
Endochondral ossification
Occurs in all other bones beside the clavicle
Begins in the second month of development
Patterns are made of hyaline cartilage
Primary ossification center
Usually the center of cartilage shaft where ossification begins
Stage 1 of endochondral ossification
Mensenchymal cells form hyaline cartilage covered in perichondrium
Perichondrium produces chondrocytes and model grow in thickness
Stage 2a of endochondral ossification
Perichondrium becomes vascularized and becomes periosteum
Osteoblast are produced and deposit collar of bone around diaphysis of cartilage model
Bone collar signals primary ossification center to form ~9 week fetus
Stage 2b of Endochondral Ossification
In the primary ossification center, chondrocytes hypertrophy → signaling surrounding matrix to calcify
Chondrocytes becomes trapped by impermeable matrix
Chondrocytes can’t get nutrients, and die ; creating cavities
Stage 3 of endochondral ossification
Cavities invaded by periosteal bud
Bud contains arteries, veins, nerves, Osteogenic cells and osteoclast
Osteogenic cells become osteoblast
secrete Osteoid on calcified cartilage and makes early spongy bone
~ week 12 fetus
Stage 4 of endochondral ossification
Osteoclast break down bone in center of diaphysis → forms medullary cavity
Diaphysis elongate as cartilage at epiphyses grow, calcifies and is dissolved by osteoclast
Secondary ossification center forms in one or both epiphyses
Bone at birth
Stage 5 of endochondral ossification
Periosteal buds enters second ossification and begins to form spongy bone
Secondary ossification is similar to primary ossification but no medulla cavity is formed
Childhood to adolescence
Stage 6 of endochondral ossification
Epiphyses ossify
The only cartilage remaining in the bone is articular cartilage
Late to early teens , early twenties
Interstitial growth
Growth in length occurs due to active cartilage at the epiphyseal plate ( elongation due to cartilage growth )
Growth from within
What is the growth zone in bone ?
Epiphyseal plate
Replaces bone, multiplies, and it’s only SOME
Closure when cartilage is gone → epiphyseal line
Appositional growth ( width
Osteoid tissue deposition on the surface of bone
Continuous growth of diameter and thickness
Intramembranous ossification
Osteoblast secrete Osteoid tissue → become trapped in calcified tissue
Circumferential lamellae
Osteocytes in endosteum enlarge marrow cavity
What is required for growth in length of bone
Epiphyseal cartilage in epiphyseal plate
What are the five zones of the epiphyseal plate
Reserve cartilage ( resting)
Proliferation (growth)
Cell hypertrophy
Calcification
Bone deposition ( ossification)
Resting ( reserve cartilage)
Resting chondrocytes
Proliferation ( growth) zone
Chondrocytes undergo mitosis
Cell hypertrophy zone
Chondrocytes become bigger
Lacunae wall thin ; begins to erode
Calcification zone
Matrix become temporary calcified
Chondrocytes die
Near end of adolescence; chondroblast divide
Less often
When the epiphyseal plate start to this
It’s then replaced by bone
epiphyseal plate closure occur when….
Epiphysis and diaphysis are fused
When does bone lengthening stops ?
In females ~ 18 years of age and in male ~21 years of age
Achondroplastic dwarfism
Chondrocytes in the proliferation and hypertrophic zone fail to grow
What can influence or modify bone growth?
Nutrition and hormones
lack of calcium, protein, and other nutrients during growth and development can cause bones to be small
Vitamin D in bone
Necessary for absorption of calcium from intestine
Can be eaten or manufactured in the body
Vitamin C in bone
Necessary for collagen synthesis by osteoblast
Lack of vitamin c cause wounds not to heal, teeth to fall out
Growth Hormone (GH)
Infancy / childhood
From anterior pituitary
Stimulate interstitial cartilage growth and appositional bone growth
Thyroid Hormone
required for growth of all tissues
Modulates GH = proper proportions
Sex hormones
Such as estrogen and testosterone
Causes growth at puberty
Causes closure of epiphyseal plate and the cessation of growth
To much GH =
gigantism
Too little GH or TH
some type of dwarfism
Bone remodeling
constant bone deposit and bone resorption
Process is coordinated by osteoblast and osteoclast
Controlled by hormonal and mechanical stress
If deposition =resorption , bone mass….
Remains the same
About how much of you bone mass is recycled each week
5-7%
trabecular bone is replaced every 3-5 years
Cortical bone is replaced every 10 years
What is calcium required for
Nerve impulses
Muscle contraction
Blood clotting
Mitosis
Hypocalcemia
Too little calcium→ can cause hyperexcitability or muscle spasm
Hypercalcemia
Too much calcium → non responsiveness ( muscle and nerves)
Bone deposition
Accomplished by osteoblast
Calcium ( and others) taken from blood stream → deposited into bone
Bone deposit occur when the bone is injured or requires more strength
Bone resorption
Accomplished by osteoclast
Lysosomal enzymes digest organic matrix ( hydrogen pumps and chloride ions)
Hydrochloric acid coverts calcium into a soluble form
Calcium enter bloodstream
Parathyroid hormones
Produced in the parathyroid gland
Responds to low blood calcium levels
Stimulate osteoclast and inhibits osteoblast
Increase renal absorption of calcium from urine
encourages the body to keep calcium in blood instead of eliminating it as waste
Calcitonin
Produced in thyroid gland
Responds to high blood calcium levels
Stimulates osteoblast and inhibits osteoclast
Is calcium homeostasis a negative or positive feedback loop
Negative feedback loop
Falling calcium levels in bloodstream
Rising calcium levels in bloodstream
Wolff’s Law
Bone grows ( via remodeling) in response to the mechanical stresses placed on it
More stress = more bone/ high response
Less stress = less bone / low response
Vigorous exercise =
increased mechanical stress = thicker stronger bones
This is important for handedness and strength training
Fetus/ bed bound patients → less mechanical stress = resorption = dramatically weaker bones
Example : bone spurs in response of continuous stress
Bones disorders
Imbalances between deposit and bone resorption underlie nearly every disease that affects the human skeleton
Osteomalacia
Osteoporosis
Paget’s disease
Osteomalacia
Bone is poorly mineralized ( calcium salts inadequately deposited )
Problem : soft, weak bones
Cause: vitamin d deficiency or lack dietary calcium
Rickets
Osteoporosis
resorption exceeds deposit
Matrix is normal, but bone mass declines
Common result in veterbral and hip fractures
Risk factors : post menopausal women ( estrogen levels decline)
Treatment : vitamin d supplements, calcium and weight bearing exercise
Paget’s disease
Excessive, haphazard bone deposition and resorption
Problem : high ratio of spongy bone to compact bone ; reduced mineralization
Cause: unknown, maybe viral
Treatment : calcitonin and biphosphonates
Fractures
Are breaks
During youth , most fracture result from trauma
In old age, most result from weakness of bone due to bone thinning
hematoma formation
Bleeding at site of fracture leads to formation of hematoma
Bone cells deprived of nutrients die
Area swells, inflames and becomes painful
Fibrocartilaginous callus formation
Capillaries invade hematoma followed by fibroblast and osteoblast
Phagocytic cells clear debris
Fibroblast differentiate into chondroblast and form cartilage matrix
Bone callus formation
Within a week the FC callus begins to be converted into bone
Trabeculae appears
FC callus converted into bone callus of spongy bone
Goes on for about 8 weeks