PSYC327: Clinical Neuropsychology
1/138
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
139 Terms
Clinical Neuropsychology
Clinical Neuropsychology is a specialty field within Clinical Psychology, dedicated to understanding the relationships between brain and behaviour, particularly as these relationships can be applied to the diagnosis of brain disorder, assessment of cognitive and behavioural functioning and the design of effective treatment.
Neuropsychological Manifestations
- Cognition
- Emotions
- Behaviour/Personality
- Social Skills
Neuropsychological Manifestations: Cognitive Impairment
- Impaired alertness/arousal
- Slowed cognitive processing
- Attentional impairment
- Learning and memory impairment
- Executive functioning impairment
- Aphasia
- Social functioning impairment
Traumatic Brain Injury & Cognition
- Mechanism of injury: how did the brain injury occur
- Injury severity: how significant is the brain injury
- Pathophysiology: what happens in the brain as a result of the injury
Mechanism of Injury: Closed Head Injury
- Direct Impact Injury
- Acceleration - Declaration
- Blast injury
Direct Impact Injury:
external force colliding with your head directly Results in blood throughout the brain and impairs function Do not need direct contact to head to experience impairments
Acceleration - Declaration:
forces of body movement have been back and forth has impacted the physiology of the brain e.g., motor accident
Blast Injury
significant blast forces that permeate through the brain and impact brain function See a lot in veterans
Mechanism of Injury: Penetrating Injury
- Occurs when an external object has penetrated through the skull and entered the cerebral cortex
- Penetrating injury is less severe (typically) than direct injury because the area of localisation being less generalised compared to direct injury which may spread across the brain
- Variable in its intensity/significant due to where it hits
- Less common
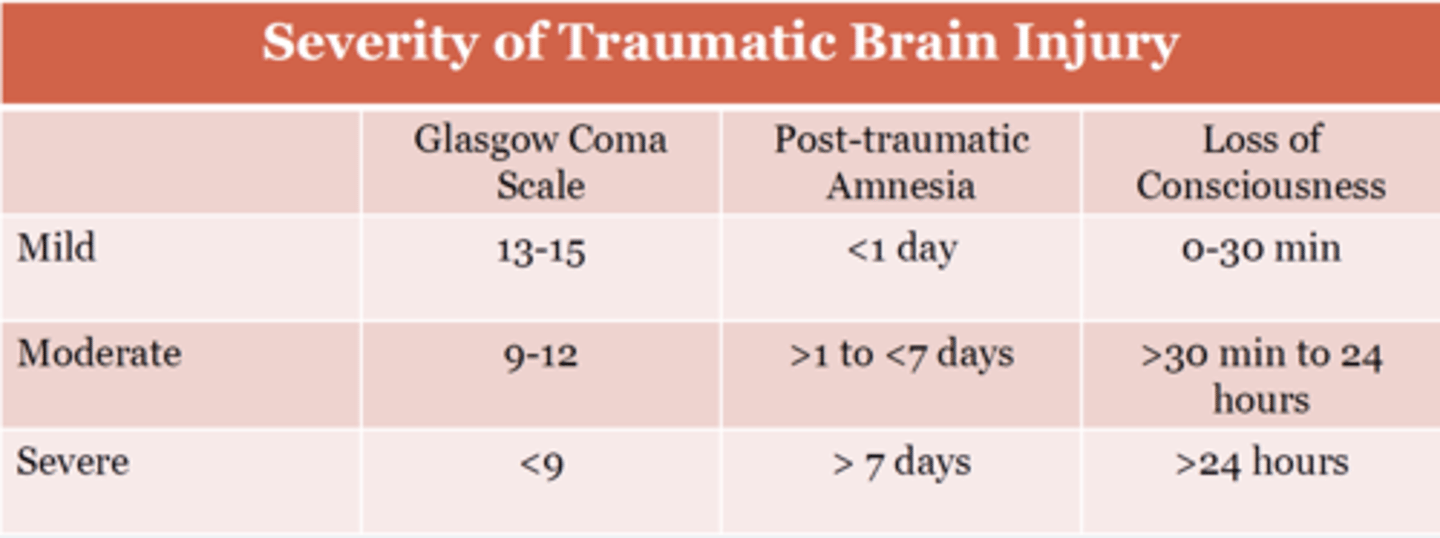
Injury Severity: Rating Severity of TBI
- Duration of loss of consciousness
- Glasgow Coma Scale (GCS)
- Post Traumatic Amnesia
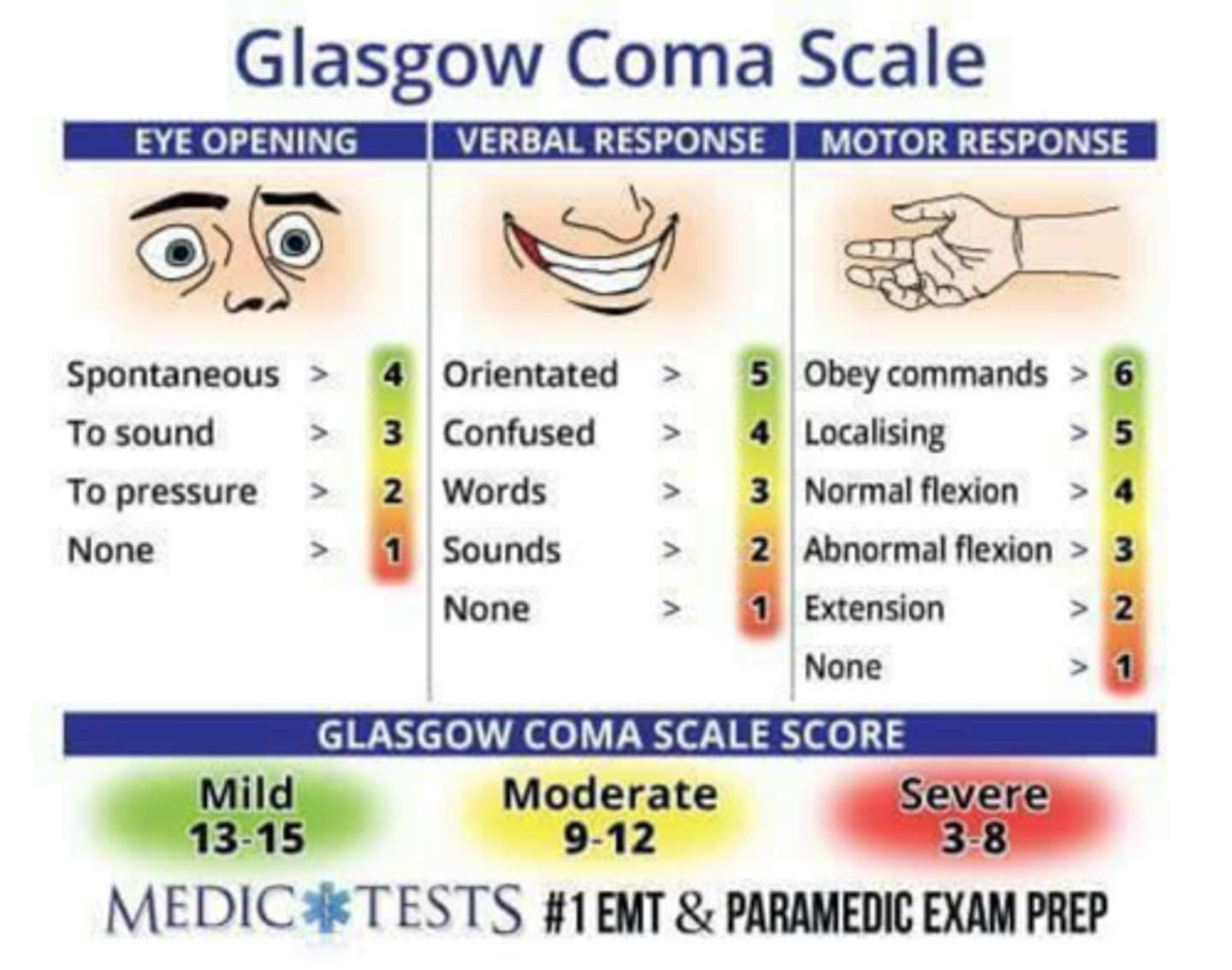
Glasgow Coma Scale (GCS)
rates verbal responses, eye opening behaviour and motor responses on a 3 (coma-state) to 15 (alert) point scale
Post Traumatic Amnesia
anterograde memory loss for events occurring immediately following the injury and retrograde loss for events immediately prior to the injury
- Test: Clinician show pp 3 objects then the following day, ask them what 3 objects you showed them yesterday. If they can't, their brain is still very vulnerable and more evidence that the BTI is serve
TBI Severity Classification
If one column trumps another, always go for the most severe option
Mild TBI (Concussion)
American Congress of Rehabilitation Medicine (MTBIC-ACRM) states that only of the following is needed to indicate the presence of TBI:
1. Any period of LOC (no less than 30 mins) flawed as 90% of concussions do not result in no consciousness
2. Any loss of memory for events immediately before or after the accident (PTA less than 24 hours)
3. Any alteration in mental state at the time of the accident such as feeling, dazed, confused or disoriented 4. Focal neurological deficit which may or may not be transient
Pathophysiology
- Soft squishy brain hitting hard skull
- Axons in grey matter can be torn during a severe BTI
- Injury to blood vessels = release of red blood cells into the surrounding tissue and
Pathophysiology: Focal
- These are common in more moderate/severe BTI
- Contusion (bruise)
- Countrecoup Contusions
- Intracranial Bleeding (Hematoma)
Contusion (Bruise)
- Can be external: more in direct impact injuries
- Can also be internally: cerebrospinal fluid means that brain moves but is contained within the skull, thus the brain may hit the top or front of the cranium which may also result in the contusion
Areas Vulnerable to Contusion
- Cranium has rigids, thus when the brain moves, it can hit the groves which makes it more vulnerable to contusions and bleeding
- Areas most vulnerable to contusion: Prefrontal cortex & Anterior and inferior temporal lobe
- Less common: Superior parietal region Cerebellum
Contusion to Prefrontal Cortex:
- Cognitive control/executive function
- Resource allocation
- Emotional control/decision making
Contusion to Temporal Lobe
- Episodic memory
- Semantic memory
- Autobiographical memory
Countrecoup Contusions
when the brain move sand hits the back of the skull
Intracranial Bleeding (Hematoma)
rupture of blood vessels within the brain leading to bleeding within or around the brain
- Need significant brain damage
Pathophysiology: Diffuse
- More likely to see because it occurs it occurs at as micro level
- Diffuse axonal injury -> shearing of neuronal axons
- Tearing of bridging veins resulting in intracranial bleeding throughout brain
- rotation movements more likely to caused tearing, thus mechanism of injury is crucial to uncover to understand the severity of the pathophysiology
Diffuse Injury and Cognition
- Occurring at the micro level
- Cognitive domains that involve large network of brain regions: Attention, Processing speed, Memory, Executive function/cognitive control
- Because BTI has more diffuse, it is different to other brain injuries such as strokes
Case of TK
- Has a brain injury following a car crash: Direct injury TBI & Acceleration - Declaration
- Based on markers of TBI severity, TK has severe In intensive care for 6 weeks, thus likely to be in a high medical needs situation Period of loss of conscious greater than < 24
TK Cognitive Observations
- Slowed processing - communication
- Effort to sustain attention
- Affect regulation
- Short term memory difficulties
- Executive function: Overriding well-learned associations & Monitoring and Correcting behaviour
- Emotional control: Difficulties in "hot" context & Poor social awareness
- Explained by diffuse pathology and focal pathology in PFC
Recovery Pathway
Dosage dependent = more severe the BTI, the more cognitive difficulties are more likely to be severe, higher persistence, and permit
Stroke (CVA)
Defined as a sudden onset of impairment in neurological functioning due to severe decrease of blood supply to the brain.
Brain Tissue & Blood Supply
- Brain tissue needs glucose (energy)/nutrients/food to stay alive. It does this via the blood supply
- Blood supply brain needs to stay alive/function has been obstructed/impacted
- Blood contains oxygen, glucose, and important nutrients for proper functioning. If brain cells do not get enough of this supply, they die.
Ischemic
starved brain tissue
Ischemic Stroke
Most common in adults and produces neuronal damage from decreased cerebral blood flow due to obstruction (e.g., plaque, blood clot),
- The damage or infarct is caused by inadequate blood supply to a particular part of the brain
- The anterior circulation (anterior cerebral, middle cerebral or anterior choroidal arteries) is affected most frequently, in about 80% of cases
- Where the blood clot occurs in the brain has huge impacts of how the brain tissue is impacted
Causes of Ischemic Stroke
- Embolic stroke
- Thrombotic stroke
- Vasospasm
Embolic stroke
a blood clot forms elsewhere in the body breaks loose and travels to the brain via the blood stream.
Thrombotic stroke
a blood clot develops in the blood vessel inside the brain
Vasospasm
is the narrowing of intracranial arteries, which can lead to hypoperfusion (a reduction in the amount of blood flow)
Hemorrhage Stroke
Less common and caused by a weakened vessel that ruptures and bleeds into the surrounding brain rather than death of blood tissue (ischemic)
- Associated with higher mortality (especially for subarachnoid hemorrhage)
- Causes a change in pressure in the brain as you have more fluid, compresses brain tissue
Intracerebral Hemorrhage
bleeding within the brain tissue itself
Subarachnoid Hemorrhage
bleeding within the subarachnoid space
Transient Ischemic Attack (TIAs)
- TIA's are brief episodes (most commonly <1 hour but up to 24 hours in duration) of neurologic dysfunction resulting from focal cerebral ischemia
- Obstruction is brief, temporary, and no permanent damage
- Considered to be a warning sign that a future stroke may occur and an underlying problem needs to be addressed
Risk Factors for Strokes
- Age
- Hypertension - increased blood pressure
- Atrial fibrillation - irregular heart rhythm
- Family history
- Substance addiction
- Diabetes
- Smoking
- Sleep apnea
- Obesity
Acute Clinical Symptoms
- Weakness of the face, arm and/or leg on one side of the body
- Numbness/tingling of the face, arm and/or leg on one side of the body
- Confusion, trouble speaking or understanding speech
- Trouble with vision in one or both eyes
- Difficulty walking, loss of balance, discoordination, or vertigo
- Severe headache with no known cause
Stroke and Cognition
- Cognitive deficits are common following stroke
- Neuropsychological deficits vary widely, may encompass any cognitive domain
- Vulnerable cognitive domains: Attention, executive function, perception, language
- Function of the size and localisation of the stroke directly map onto the neuropsychological impairments (stroke syndromes)
Two Main Pairs of Arteries that Provide Blood to the Brain:
- Internal carotid arteries -> supply the anterior and middle brain
- Vertebral arteries -> supply the brainstem and posterior brain
Anterior and posterior cerebral circulations interconnected via bilateral posterior communicating arteries
Form part of the Circle of Willis
Anterior Cerebral Circulation
- Internal carotid artery
- Anterior cerebral artery
- Anterior communicating artery
- Middle cerebral artery
Posterior Cerebral Circulation
- Vertebral artery
- Posterior Communicating artery
- Basilar artery
- Posterior cerebral artery
Middle Cerebral Artery
- About two thirds of all ischemic strokes occur in the middle cerebral artery territory
- MCA stroke can involve frontal, temporal, and parietal lobe
- MCA stroke can also involve the basal ganglia
- MCA Covers a Large Portion of the Hemisphere
MCA Stroke Syndromes: Left Hemisphere
- Right hemiparesis - weakness (motor deficit) to the lower face and arm
Left inferior gyrus - motor control
- Right sided sensory loss similar pattern to that of the motor deficit
Left posterior gyrus - sensation
Changes in the ability to speak, write and understand language
MCA Stroke Syndromes: Right Hemisphere
- Left hemiparesis - similar pattern to right
- Left sided sensory loss
- Neglect of the left side of the environment
- Difficulties navigating (visuospatial processing)
- Flat affect
Anterior Cerebral Artery
Covers the medial portion of the brain
ACA Stroke Syndrome
- Motor deficits - commonly in the lower extremities
- Difficulties in drive and motivation ACC
- Agitation
- Memory and speech impairments (this involves many brain regions, thus even damage to non-critical areas, it facilitates and supports other areas and can result in deficit)
- Emotional lability
- Incontinence
Posterior Cerebral Artery: Stroke Syndromes
- Thalamus: Sensory and motor deficits
- Occipital lobe: Visual field deficits (i.e. hemianopia), Visual agnosia, Alexia
- Medial temporal lobe: Deficits in long-term and short-term memory & behavioural alteration (agitation, anger, paranoia)
Cognitive Impairment and Stroke Recovery
- Approx. two-thirds of stroke patients experience cognitive impairment or cognitive decline; about one-third go on to develop dementia.
- There is a huge variability in recovery, often indicative of severity and quickness to response
- Most improvement occurs in the first 3 months, although recovery may continue for up to a year
Seizure
A transient occurrence of signs and/or symptoms due to abnormal excessive or synchronous neuronal activity in the brain
Large number of brain cells are activated abnormally at the same time
Seizure disrupts neurons synchrony within our brain, thus the synchrony we require for normal functioning is impacted
Seizure Characteristics
There are different characteristics of seizure, these are critical to determine what seizure is occurring and identify where it is in the brain.
Clinicians analyse behaviour occurring during the seizure to as a clinical marker to identify the characteristics of a seizure
Behaviours exhibited during a seizure (referred to as "ictal semiology") varies considerably depending on the underlying cause of the seizure
Causes of Seizures
- Fever (especially in young children)
- Electrolyte imbalance
- Acquired injury to the brain: TBI, stroke, infection
- Drugs and other chemicals
- Serious Infections
- Low blood glucose levels
The Semiology of a Seizures
The behavioural features associated with a seizure:
- Pre-ictal period
- Ictus or ictal period
- Post-ictal period
seizure semiology varies depending on the localisation of seizure onset, duration, and propagation pathways of discharging neurons
Pre-ictal period
immediately before the seizure Feeling an aura
Ictus or ictal period
during a seizure
Type of motor sensations or are there non-motor features
Post-ictal period
immediately following a seizure How long does it take the pp to regain consciousness
Seizure Classification
- Where the seizures begin in the brain
- Level of awareness during a seizures
- Other features of seizures: Non-motor? Cognitive seizure? Emotion seizure?
Two Types of Seizure Classifications
- Focal
- Generalised
Focal Onset
- Localised to a specific region
- Need to figure out whether Aware or Impaired Awareness
- Need to figure out whether Motor Onset or Nonmotor Onset
Focal Seizures - Motor Onset: Automatisms
Non-purposeful, stereotyped, and repetitive behaviours e.g., closing your eyes
- Person is aware
Focal Seizures - Motor Onset: Atonic
A sudden loss muscle tone and strength
- Person is aware
Focal Seizures - Motor Onset: Tonic/Clonic Seizure
- Tonic: A sudden stiffness or tension in the muscles of the arms, legs or trunk
- Clonic: A fast stiffening and relaxing of a muscle that happens repeatedly
- Person is aware
- Localised to one area
Focal Seizures - Motor Onset: Myoclonic
A quick, involuntary muscle jerk
Focal Seizure with Impaired Awareness
- Focal but because it is impacts awareness, it impacts a bigger part of one hemisphere
- Consciousness is affected: blank look/day dreaming
- Stereotypic movements: Open and close lips, Pick at clothes, or wander around
Focal Seizures - Non-Motor: Autonomic
A 'rising' feeling in the stomach
Focal Seizures - Non-Motor: Cognitive
déjà vu, slowed thinking, memory difficulties, problems talking and understanding
- déjà vu - in temporal lobe, hippocampus
Focal Seizures - Non-Motor: Emotional
sudden fear, dread, anxiety or even pleasure Intense feelings and sudden
Focal Seizures - Non-Motor: Sensory
changes in hearing, vision, taste, "auras" or feelings of numbness, tingling, or pain (sensory)
Generalised Onset
- Awareness is always impaired
- Need to figure out whether Motor Onset or Nonmotor Onset (e.g., absence)
Generalised Onset - Non-Motor Onset: Absence Seizures
Non motor - brief episodes of impaired awareness with no warning and short duration (typically less than 20s)
- Blankness, frequent, and brief
- Children with absence seizures is likely to impact with attention cognition
Generalised Onset - Motor Onset: Generalised Tonic-Clonic Seizure
Present as:
1. Tonic extension of the extremities for about 20s followed by
- Tonic phase = the muscles will stiffen, the person will fall to the floor if standing
2. Clonic synchronous rhythmic muscle movements generally lasting about 45s
- Clonic phase = the muscles will jerk randomly
Associated with a period of post-ictal confusion
Classifying Seizure
- Seizures are usually classified by symptoms and signs
- Ictal period is crucial, thus clinicians try to provoke a seizure to observe it and determine a classification
- Supportive information may be helpful, when available: Videos brought in by family, EEG patterns, Lesions detected by neuroimaging, and Laboratory results such as detection of anti-neuronal antibodies
Epileptic Malformations
cite in cerebral cortex that the seizure is begging
Epilepsy
abnormal epileptic malformations that result in abnormal electrical activity originating in the brain, causing seizures
Epilepsy is diagnosed if an individual has:
1. At least two unprovoked seizures >24 hr apart
2. There is no other underlying cause of the seizures, such as substances or an infection
Cognitive Deficits and Epilepsy
- highly variable given the different types of seizures
- May include abnormalities in: Language, visuo-perception, attention, memory, language, executive function
- Due to epileptic dysfunction or developmental/acquired structural abnormalities (decreased brain tissue volume)
There is a correlation between the area of the brain
- Cognitive deficits can be characteristics of a particular epilepsy syndromes
Temporal Lobe Epilepsy (TLE)
- Most common type of seizure (25% of children and 50% of adults)
- Focal seizures arise from temporal lobe
Temporal Lobe Epilepsy (TLE): Pathology
70% of TLE patients have evidenced of hippocampal sclerosis (abnormality of brain tissues within hippocampal structure in temporal lobe)
Potential theory for this is that hippocampus is highly active in forming new memories, thus the likelihood of abnormality occurring here is higher
Temporal Lobe Epilepsy (TLE): Risk Factor
Febrile seizure (fever induced seizure) in childhood
- Induces abnormalities in temporal lobe and hippocampus, thus creates a risk factor for TLE later in life
Temporal Lobe Epilepsy (TLE): Focal Aware Seizure
- Déjà vu, a memory or jamais vu
- Emotion based-seizures: A sudden sense of fear, panic or anxiety; anger, sadness or joy.
- A rising sick feeling in your stomach
- Altered sense of hearing, sight, smell, taste or touch (somatosensory functioning in located in PFC & Anterior aspects of Temporal lobe)
Temporal Lobe Epilepsy (TLE): Focal Impaired Awareness Seizure
- Staring into space
- Repetitive behaviours and movements
- Confusion
- Unusual speech (Broca's area/Dorsal processing stream)
- Brief loss of ability to speak, read or comprehend speech
Temporal Lobe Epilepsy (TLE) and General Cognition Clusters
- Cluster 1: minimally impaired (47%)
- Cluster 2: predominately memory impaired (27%)
- Cluster 3: Generalized impairment (29%)
The differences in general cognition with different Temporal Lobe Epilepsy (TLE) pp because of differences in speed to treatment
Cluster 3
- Earlier onset of seizures
- Longer duration of seizures
- Great seizure frequency
Factor Associated with Poorer Cognitive Functioning (Cluster Three):
- Brain tissue volume
- Age at seizure onset
- Longer duration of seizures
- Greater seizure frequency
- Greater lifetime total generalized seizures
Normal Aging - Declined Cognition
- Declines in certain aspects of cognition are typical with ageing but quite variable
- Sensory and motor loss are common, thus need to rule out
- Changes in sleep pattern
Normal Aging - Cognitive Abilities Typically Resistant to Aging
- vocabulary and verbal skills (reading ability)
- Simple attention and concentration
- Basic arithmetic problem solving
- Recognition memory and recall of the gist of stories
- Remote memory (recall from many years ago)
Normal Aging - Examples of Common Cognitive Changes with Aging
- Decreased sustained and divided attention
- Less efficient and slower rates of learning new information
- Reduced recall of detailed information presented recently
- Reduced cognitive flexibility
- Sensory and motor loss are common, thus need to rule out
- Changes in sleep pattern
Life Span Models of Aging: The Processing Speed Theory
- With increasing age, the capacity and mental energy, or cognitive processes, required to perform information processing routines and information from the environment becomes limited
- This imposes constraints on many types of processing and hence a range of cognitive domains are impacted
- As we age, there is a decrease in white brain tracts (critical for efficient processing speed) and tissue. This means processing abilities and processing is limited. The efficiency of the cognitive system reduces, having implications on higher order cognition (Cognitive flexibility impacted)
Mild Cognitive Impairment (MCI)
MCI is a clinical diagnosis that requires memory or other cognitive complaints from the patient and psychometric evidence of impairment
Consists of relatively isolated cognitive impairment beyond that seen in normal ageing
Impact of MCI
Cognitive impairments in MCI do not dramatically interfere with an individual's everyday functioning
- If it does, it is indicative of dementia/neurodegenerative disorders
First Impairment in MCI
Verbal episodic memory is usually impaired first with intact general cognitive functioning
Prevalence Rates of MCI
- increase with age
- Roughly 6%-15% of MCI cases per year develop or "convert" to dementia
Diagnosing of MCI
- often requires comprehensive neuropsychological assessment due to the limited sensitivity of clinical interview or brief cognitive screening
- By diagnosing MCI it allows for earlier treatment to see if these cognitions are truly declining
- What's helpful for diagnosing MCI: looking at general factors in the brain that could support the individual: mental health, sleep, diet and identify vulnerability and reduce the decline is important
Alzheimer's Disease
A progressive, degenerative brain disorder that results in generalised brain dysfunction and dementia
Alzheimer's Disease: Memory
Typically characterised by anterograde amnesia that is eventually accompanied by deficits in other cognitive domains
Alzheimer's Disease: Neuropathology
- synaptic and neuronal loss associated with progressive deposition of amyloid (brain waste) in the form of neuritic plaques, along with the accumulation of tau in the form of neurofibrillary tangles and neurophil threads
- Neurons begin to die and brain dip tissue begins to atrophy
Alzheimer's Disease: Where i Occurs
occurs in hippocampus and Medial Temporal Memory System, followed by frontal, and parietal areas (and other cognitive abilities)
Primary motor, visual, auditory and somatosensory cortices, as well as aspects of subcortical structures, tend to be relatively unaffected until quite late in the disease process
Alzheimer's Disease: Diagnosis
- The presence of AD pathology can only be ascertained by neuropathological examination of brain tissue
- Clinical diagnosis is 85-90% accurate
- Requires the integration of information from a variety of sources but is often characterised by the history and nature of presenting symptoms
- neuropsychological deficits must reflect a significant decline from premorbid functioning