US QUIZ
1/40
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
41 Terms
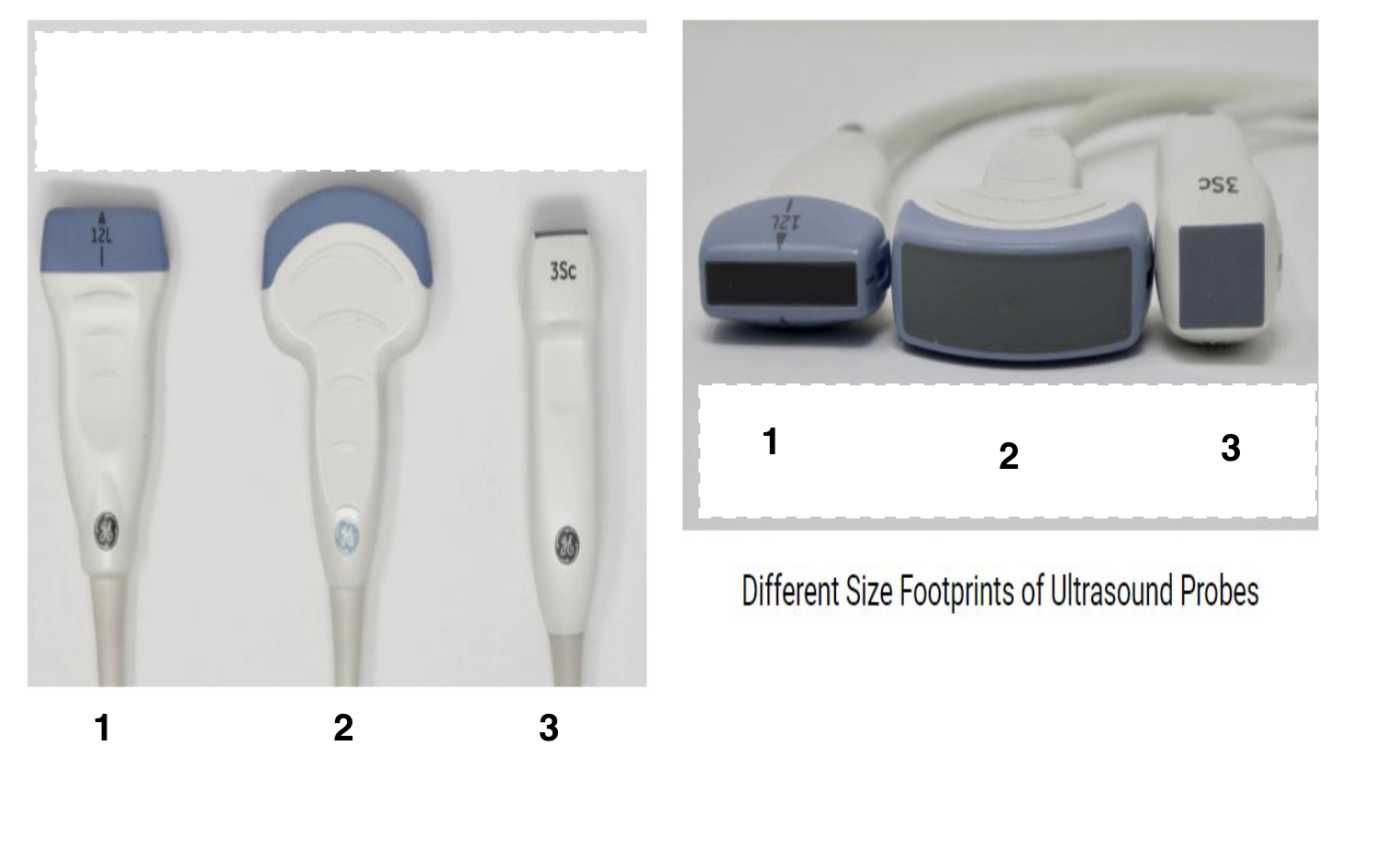
1- linear
2- curvilinear
3- phased array
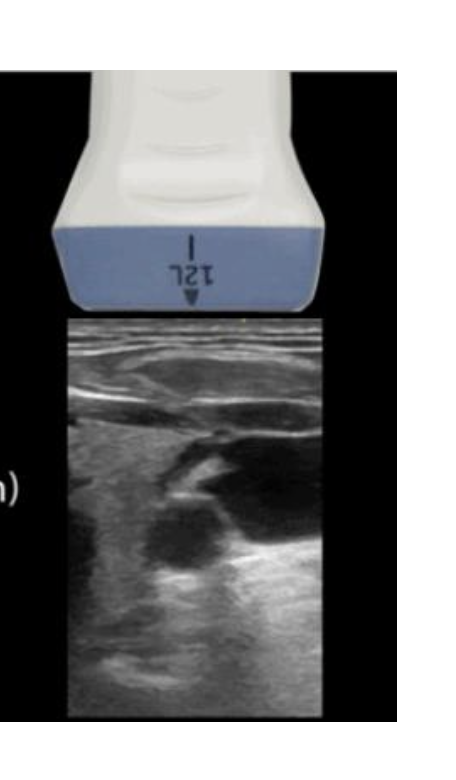
LINEAR PROBE
high frequency
linear footprint
shallow structures
GOOD FOR BREAST AND CHEST IMAGING
• Frequency affects penetration.
Frequency also impacts velocity scales (Nyquist limit & Doppler equation in Colour Doppler).
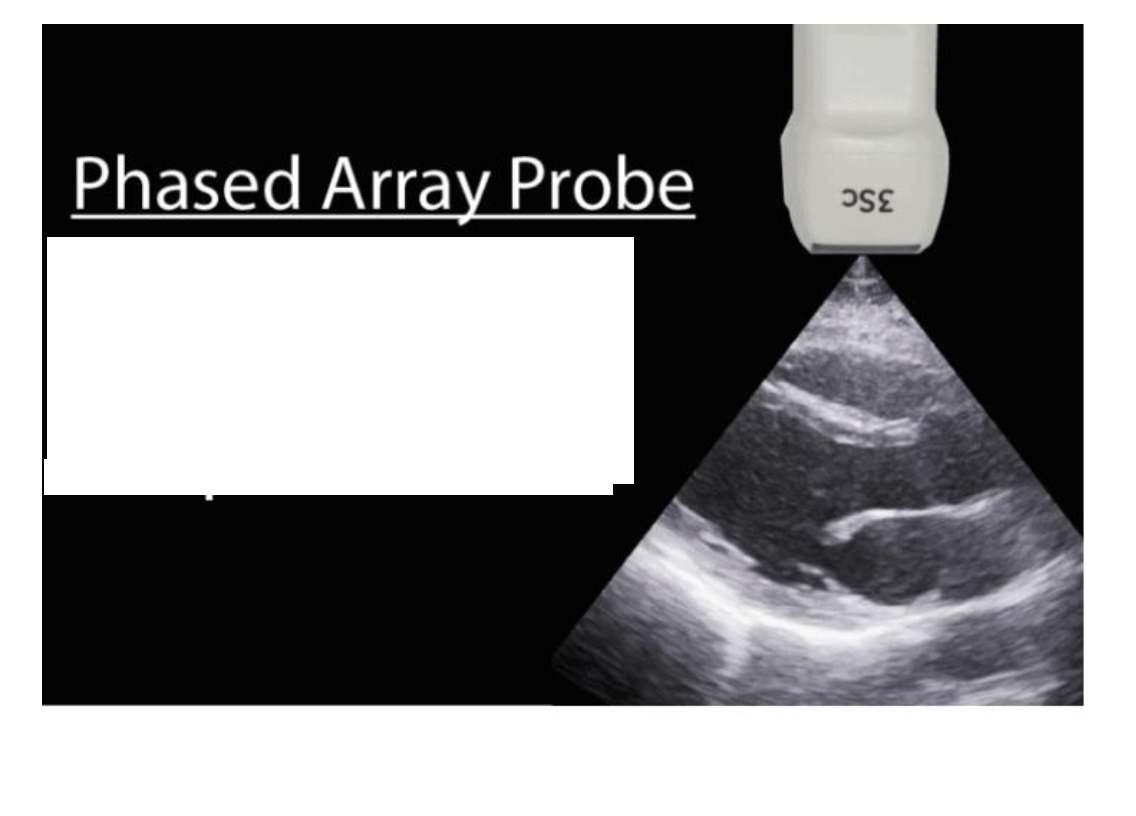
The Phased/ Sector array transducer
Low frequency
Narrow footprint
Deep structures
FOR BREAST AND CHEST US
Larger body habitus → need greater penetration, lower frequency.
Phased array useful, incl. for biopsies.
The curvilinear ultrasound transducer
low frequency
wide footprint
deep structures
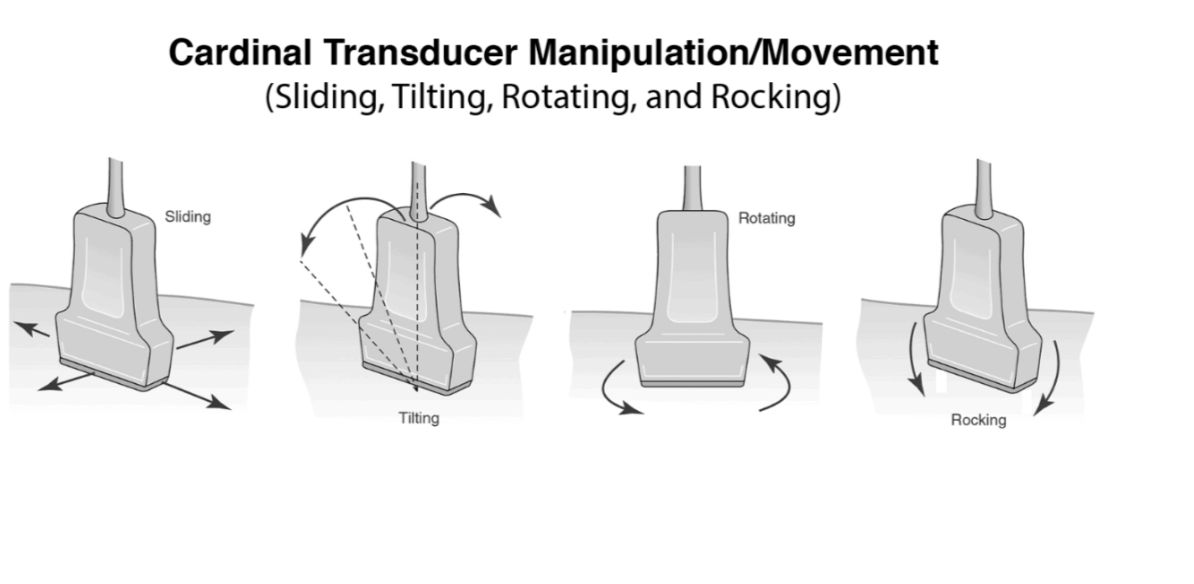
Ultrasound probe movements and manipulation
GAIN VS TGC
Overall Gain – adjusts the brightness of the entire image by amplifying returning echoes uniformly, affecting the whole field of view.
Time Gain Compensation (TGC) – selectively amplifies echoes at different depths, compensating for attenuation so that deeper structures appear with similar brightness to superficial ones.
Function – optimises image quality and contrast without altering the actual transmitted ultrasound beam or patient exposure.
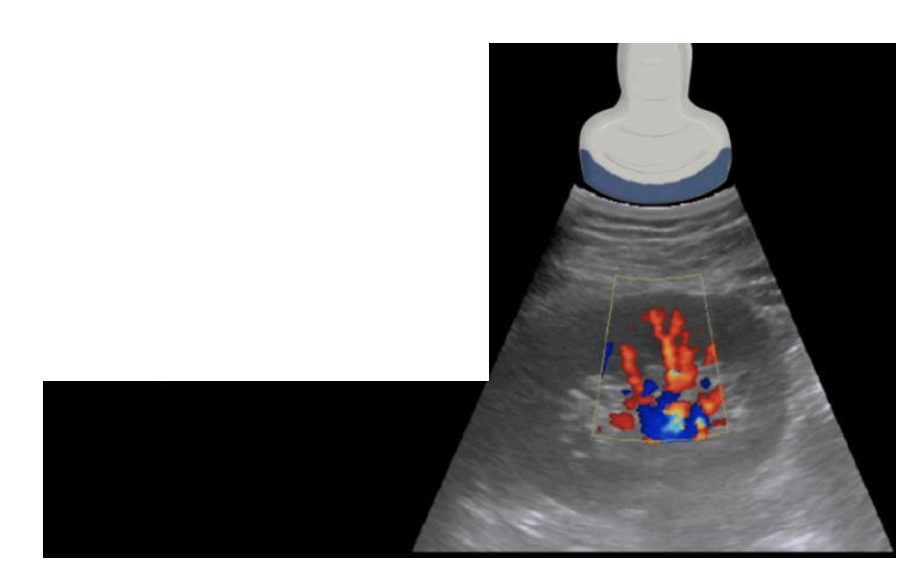
Power Doppler Mode
-PD is more sensitive than color Doppler and is used to detect low flow states such as venous flow in the thyroid or testicles
Displays the amplitude (strength) of blood flow signals rather than velocity or direction.
More sensitive to low-velocity or small vessel flow than colour Doppler.
Does not provide directionality of flow, but reduces angle dependency and is less affected by aliasing.
7. Modifications and Limitations of the
abdomen ultrasound
Exam components may require flexibility in order and patient positioning.
Recognition of anatomy, orientation, respiration effects, gas, and fluid pockets in real-time.
Recognise when modifications are needed.
Advantages of Breast and Chest
ultrasound
Rapid *contralateral & dynamic** assessment
* Non-invasive, portable, inexpensive
* No claustrophobia, safe with pacemakers/metal
* Guides procedures, repeatable for monitoring
* Real-time imaging
Limitations of Breast and Chest ultrasound
• Deeper structure are still difficult to visualize
• Error of Sonographer with ultrasound machine interobserver variability
• Operator dependent
• Competition of medical advancements and technology with interventional
procedures and other modalities such as CT and MRI
• Interventional procedures and invasive surgical examinations superiority
Selection of transducers and image
parameters for Breast and chest ultrasound
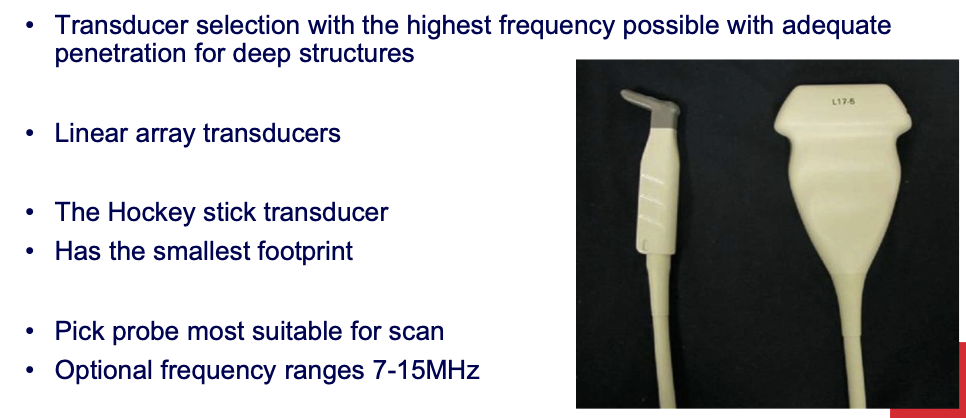
hockey stick transducer
High frequency greater resolution
• Small footprint
• Superficial structures and vessels
• Chest or Breast lump
Breast ultrasound pitfalls and problems
with solutions
Lesion not visualised → poor resolution (freq/shape/focus), poor positioning, isoechoic to tissue.
Correlation issue → cannot match with mammo/MRI/CT/clinical finding.
Indeterminate mass (solid vs cystic).
Techniques → harmonics, colour, adjust settings, patient reposition.
Pitfalls → small posterior cysts (↓ enhancement), reverberation mimicking debris, Cooper’s ligament shadowing, accessory axillary tissue (matches glandular echo).
History important → lactation may show milk-filled ducts (not tumour).
Cooper’s ligaments: are connective tissue in the breast that help maintain
structural integrity, can be seen as thin white curvilinear lines and cause
artificial shadowing and this artefact can be reduced with compression
• Tissue Harmonic imaging can provide images of higher quality
• Harmonic signals are generated differently and lead to higher contrast resolution
• Harmonics can increase real echoes and can reduce artefactual echoes
Awareness of Grading, Staging and Survival rate of
breast cancer and types of non-invasive breast cancer
Grading → histological features
Staging → size & spread (Stage 1–4)
Survival rate → % reaching survival period
Non-invasive BC types:
Intraductal carcinoma
Comedo carcinoma
Intraductal & LCIS
Papillary carcinoma
LCIS
Breast biopsy and some interventional
procedures
Hook-wire → pre-op, ultrasound-guided lesion localisation for surgery
FNA Fine Needle Aspiration→ sample tissue from solid lesion or aspirate cystic fluid
Core biopsy → gun needle (variable throw) or vacuum-suction probe
Breast ultrasound implants and the male breast
Augmented breast:
Reasons for US: routine follow-up, palpable mass, implant concerns (rupture, thickening, capsular fibrosis)
Examine breast tissue over implant + implant
Implant appears smooth, echogenic balloon with anterior reverberation artefacts
Male breast:
Usually exclude malignancy (rare, prognosis like females, more chest wall invasion)
Gynecomastia → common pathology, breast enlargement
Chest ultrasound
Biopsy of chest wall, mediastinal and peripheral lung masses
• Diagnostic and therapeutic drainage of pleural fluid collections and
• Assessment of soft tissue masses of the chest
aid in the detection
of lymphomas, retrosternal thyroids, dermoid cysts or aortic aneurysms with
this ultrasound chest approach
CHEST US INTERVENTION
• Diagnostic and therapeutic drainage of pleural fluid collections
• Moveable strands, fibrinous strings and septations are typical of
inflammatory effusions.
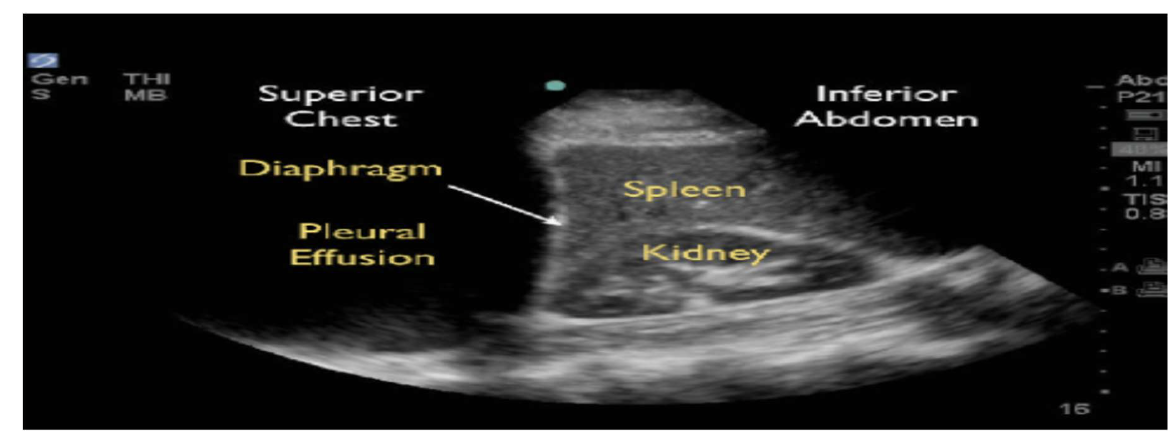
• Ultrasound can detect nodular metastases not seen in radiographs
Transabdominal US
A transabdominal ultrasound is conducted with a full bladder, using a 3.5-7MHz curvilinear probe over the abdomen
The patient is in a supine position
The bladder filling allows for the complete penetration of sound waves to the posterior pelvic organs while simultaneously
displacing the bowel laterally
A transabdominal ultrasound is a complete scan when transvaginal contraindications are present. They include:
Paedatric age group
Patients with no history of vaginal intercourse
Vaginismus
Significant vaginal atrophy
Vaginal obstruction
Recent vaginal surgery
When a patient denies consent
In obstetrics: premature rupture of membranes, due to risk of introducing infection and bleeding associated with known placenta
previa
Transvaginal US
A transvaginal ultrasound is conducted with a 5-12 MHz, narrow
transvaginal probe
It is inserted into the vagina and then carefully moved by the
sonographer to obtain the images
The patient can be lying in the supine position with a bolster under the
pelvis to allow for free movement of the probe
Empty bladder
Generally, when there are no contraindications both a transabdominal
then transvaginal scan is completed, in the same visit
Translabial
ultrasound
A translabial ultrasound is completed with either a curvilinear or linear array
transducer which is placed over the perineum and not inserted into the vagina
This allows for high resolution imaging of superficial structures with a wide field of view
Empty bladder
Recent advances in imaging for prolapse show translabial ultrasound as way to dynamically assess for the movement of the uterus, bladder, bowel in relation to
each other and the rectum using dynamic real time assessment
We can use transvaginal ultrasound to manually assess ovarian and uterine mobility and
differentiate between the origin of a mass
We can ask the patient to cough, to bring up the ovary if its obscured by bowel or gas
We can provide comfort to the patient
There is no ionizing radiation exposure associated with ultrasound imaging
Limitations of Breast, Chest and Reproductive
ultrasound
•
Deeper structure are still difficult to visualize
• Error of Sonographer with ultrasound machine interobserver variability
• Operator dependent
• Competition of medical advancements and technology with interventional
procedures and other modalities such as CT and MRI
• Interventional procedures and invasive surgical examinations superiority
The Endocavitary probe
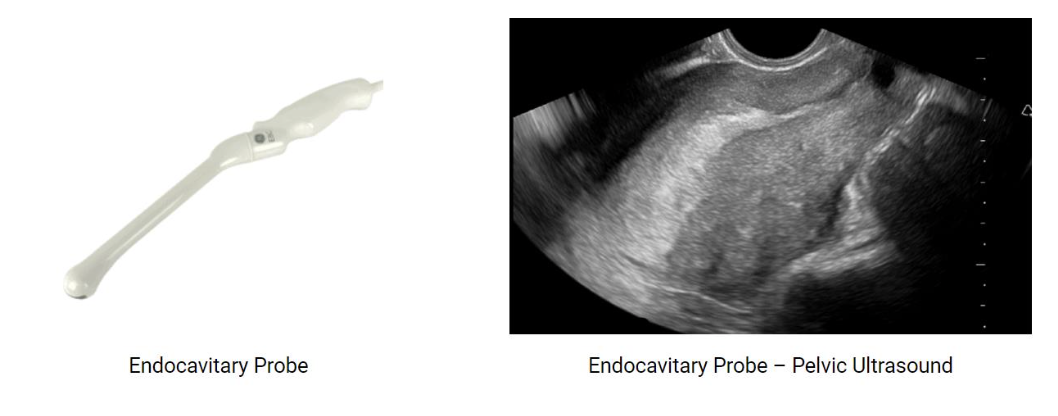
Designed for internal imaging (e.g., transvaginal, transrectal).
Higher frequency → better resolution, shallower penetration.
Provides close proximity to organs for detailed assessment.
linear probe chest n breast imaging mghz selection
Minimal glandular breast tissue15-7MHz or
• Enlarged breast glandular tissue 10-7MHz
Advantages of MSK ultrasound
• Real time assessment (joint crepitus)
• Dynamic examination (specific motion induced pain, discomfort)
• Higher spatial resolution images of superficial soft tissue anatomy than MRI
• Allows for rapid contralateral examination (limb comparison)
• Non invasive
• Portable (availability)
• Relatively inexpensive compared to other modalities (MRI, CT)
• No claustrophobia
• Practical and rapid method of obtaining images
• Safe in patients with pacemakers and metal artefacts
• Guide procedures (Injections, aspirations, biopsy)
The high frequency linear array transducer
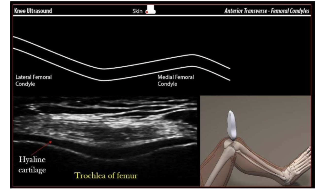
• High frequency 17-5MHz
• Greater resolution
• Superficial structures
• Linear array transducer
Power Doppler (PD) Mode in MSK
ultrasound
• PD is more sensitive than color Doppler and is used to detect blood flow or
vascularity in tendons
• Increased PD signals are associated with inflammatory conditions.
• Doppler signals are easily obliterated with probe pressure or when the
tendon is stretched
MSK ultrasound techniques to aid in
artefact prevention including anisotropy
• Thick gel or stand off pad (not contaminated)
• Spatial compounding
• Beam steering
• Panoramic imaging
Spatial compounding in MSK ultrasound
Greater beam _______
Greater beam reduces the frame rate
Beam steering in MSK ultrasound and Anisotropy
manual beam steering. This technique involves tilting the probe over the area of
interest to make the ultrasound beams approach being perpendicular to the needle
and increasing signal as seen above.
• A false hypoechogenicity of a structure due to obliquity of ultrasound beam
• One of the most common artifacts especially in MSK ultrasound.
• To minimize the artifact, the MSK structure should be scanned
perpendicular to the ultrasound beam (parallel to the transducer face).
• This can be achieved by “heel-toeing” the transducer.
MSK ultrasound artifacts and pitfalls
Shadowing
• Enhanced through-transmission
• Comet-tail artifact
• Refraction
• Speed or sound artifact
• Beam width artifact
• Motion artifact
• Ensure comparison with contralateral side
• Don’t compress and obliterate small fluid collection or tears and
• Examine dynamically and at all angles
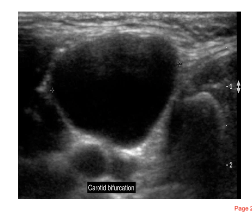
Ultrasound characteristics of a true cyst in neck and
associated structures sonography
• Anechoic (isoechoic)
• Posterior enhancement
• Posterior wall definition
• Side wall definition
• No internal echoes
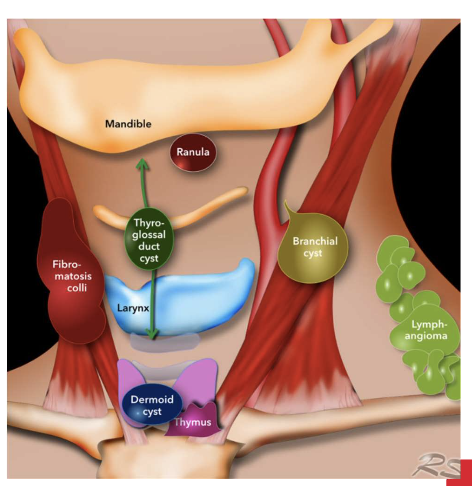
Neck ultrasound: common cystic locations and other
regions of patholog
Thyroglossal duct cysts- most commn
• Brachial cleft cyst
• Miscellaneous cystic masses and
Other common pathology regions:
• non-cystic masses
• Lymphatic nodes
• Salivary glands
Ultrasound features in assessing Thyroid nodule –a
set of different case studies
Co-existing multilnodularity
• Echogenicity compared with normal thyroid tissue
• Peripheral anechoic halo
• Internal consistency
• Surrounding structures
• Margination
• Calcification
• Vascularity
Ultrasound features that favour a benign lesion in the
neck region
Co-existing multilnodularity
• Echogenicity compared with normal thyroid tissue
• Peripheral anechoic halo
• Internal consistency
• Surrounding structures
• Margination
• Calcification
• Vascularity
Ultrasound features that favour a malignant lesion in
the neck region
Co-existing multilnodularity
• Echogenicity compared with normal thyroid tissue
• Peripheral anechoic halo
• Internal consistency
• Surrounding structures
• Margination
• Calcification
• Vascularity
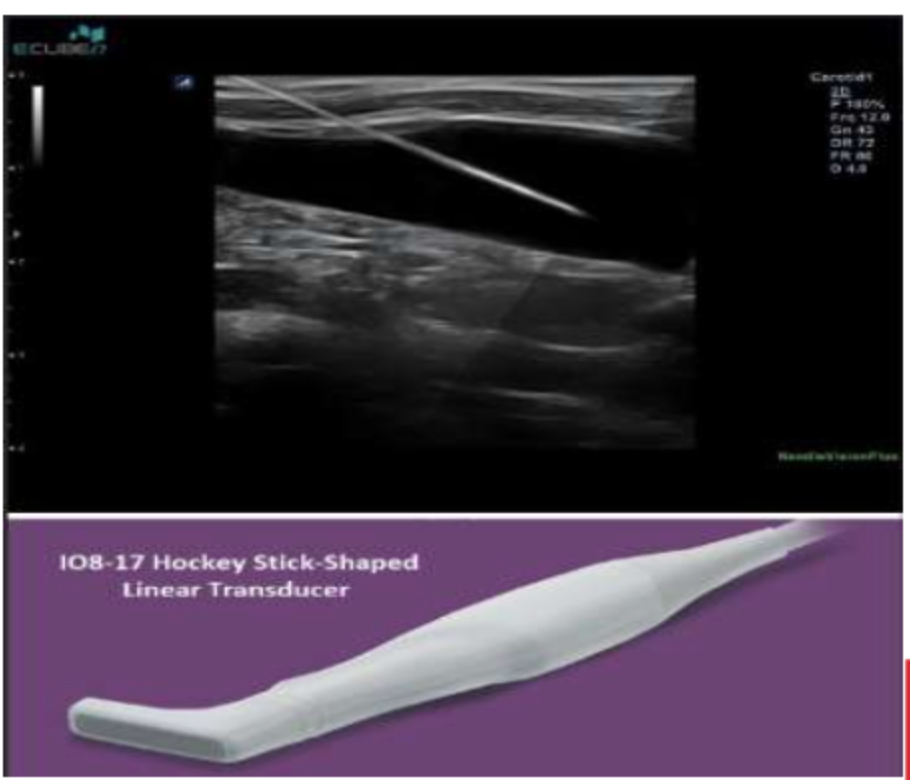
The high frequency linear array
transducer for Vascular ultrasound
• Transducer frequency is dependent on patient body habitus for example a
carotid examination:
• Thin neck 5-7MHz or
• Thick larger neck 10-7MHz
The Doppler shift using the velocity of
blood
Best Doppler angle = parallel (0°) to us probe→ accurate measurement
>25–30° → underestimation
90° (perpendicular) → cos90=0 → no flow detected
Pulse Wave (PW) Doppler in
Vascular ultrasound
PW Doppler → measures velocity at a single point
Sample gate specifies location (marked by 2 horizontal lines)
Limitation → aliasing artefact
PW Doppler limit = Nyquist limit → beyond this → aliasing
Not suitable for speeds >200 cm/s
Continuous Wave (CW) Doppler
• CW Doppler is very similar to PW Doppler except it does not alias
• And can detect very high velocities (greater than 1000cm/second).
• Optimal choice for measuring high-velocity applications such as valvular
stenosis and regurgitation.
• CW Doppler does not rely on a sample gate to measure a single point
• Therefore what you will see will be the maximum velocity of flow detected
along the cursor line. This is a pro and a con.
• It is a pro because you don’t have aliasing and can detect high velocities
• It is a con because you don’t know exactly where that velocity is coming
from on the cursor.
Wall filter → removes low-velocity signals / ↓ artefacts
Steer → adjust colour box to improve angle
Angle correction → for PW, corrects sample gate angle
Vascular ultrasound techniques to aid in artefact prevention
including aliasing
Aliasing:
Most common Doppler artefact → occurs when signal undersampled
Solution → ↑ pule repetition freq PRF
Limited by Nyquist limit
Other optimisation:
Compound imaging → multiple sightlines → better plaque definition, ↑ contrast, improved imaging through calcific plaques