VIVA IMAGING APPS
1/97
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
98 Terms
What is FLAIR and what is it used for?
Fluid attenuated inversion recovery
Fluid is suppressed
Thus high areas of signal indicate pathology
`
What MRI fields can cause harm to a patient and how?
Static: biological fields, Can move metal objects and affect implants.
Gradient: heating, acoustic noise, and nerve stimulation
RF (radiofrequency waves): heating, burns, interference with implants
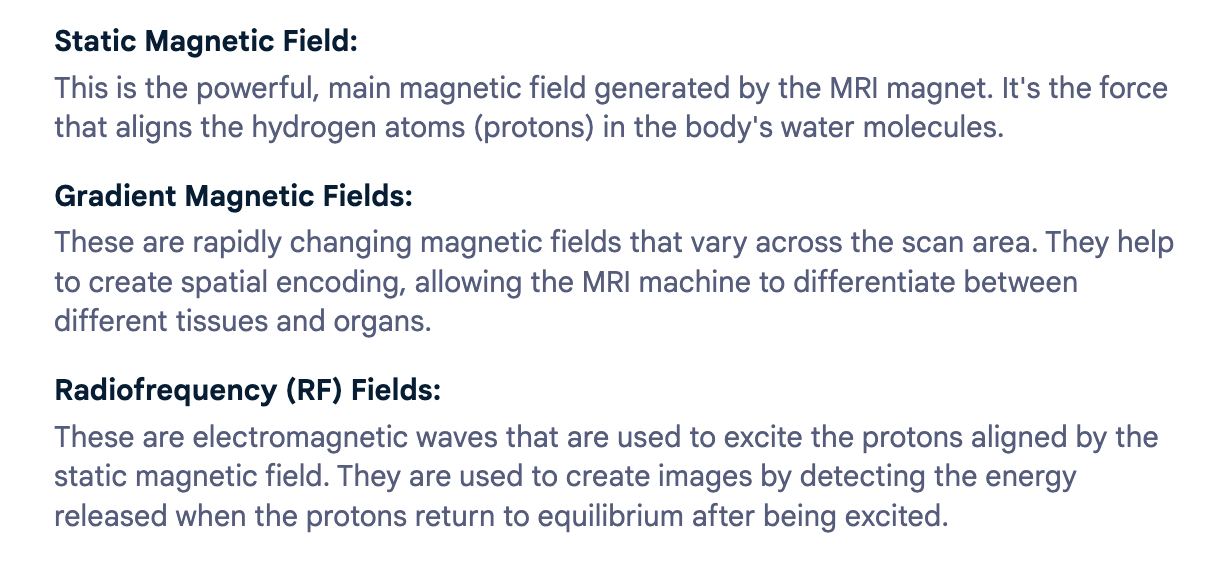
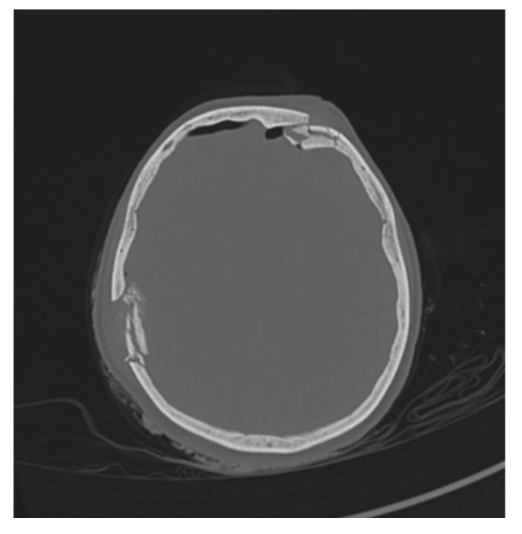
What is the pathology?
Skull fracture along lambdoid suture line.
Sits along the suture and the regular suture pattern is abnormal.
Best seen on non-contrast brain bone window.
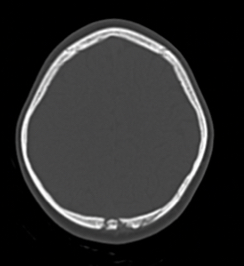
What is the pathology?
Saccular aneurysm: abnormal swelling of brain blood vessel
Rounded shape
Best seen on COW and carotid CT especially post contrast as vessel will enhance.
What is the planning protocol for C+ A/P
Pt position: supine, feet first, hands above head
Scan range: diaphragms to pubic symph
Phase: Post contrast
For viewing bowels oral contrast is given and opacification should be seen in bowels
For other abdominal related pathology IV contrast is given with and arterial and PV phases.
What are the abnormal effects of IV contrast?
Hot flush
Metallic taste in mouth
Feeling that they are wetting themselves
How does IV contrast effect allergies and how can you minimise this risk?
Increases the risk of hypersensitivity reaction if patient has other allergies.
Medications can be taken prior such as antihistamines
How does IV contrast affect beta blockers and how can you minimise this risk?
Taking beta blockers increases the risk of the patient having a moderate to severe reaction to IV contrast.
Intravenous glucagon can be used instead of iodinated contrast
How does IV contrast affect renal function and how can you minimise the risk?
IV contrast is nephrotoxic therefore can cause further renal damage to the already existing condition.
Consult radiologist and identify EGFR
IV hydration is recommended prior to CT scan.
How does IV contrast affect diabetic patients on metformin and how can you minimise the risk?
Consult radiologist on pt eGFR
lactic acidosis
eGFR>30 low risk of developing lactic acidosis therefore pt can take metformin as normal.
eGFR <30 cease taking metformin 48 hrs prior to CT scan.
How does IV contrast affect thyroid disease and how can you minimise the risk?
IV contrast can cause thyroxicosis
Need to outweigh risk v benefits
Pt needs to be monitored and an emergency crash kit needs to be located close by.
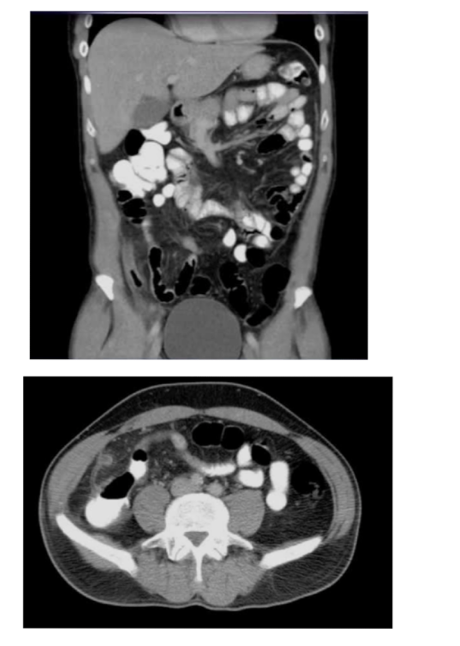
What is the pathology?

Diverticulosis: pockets of air
branching from the bowel
Thickening of the lumen wall
Leaking of gas into Abdo cavity
What are the sequences and what is the pathology?
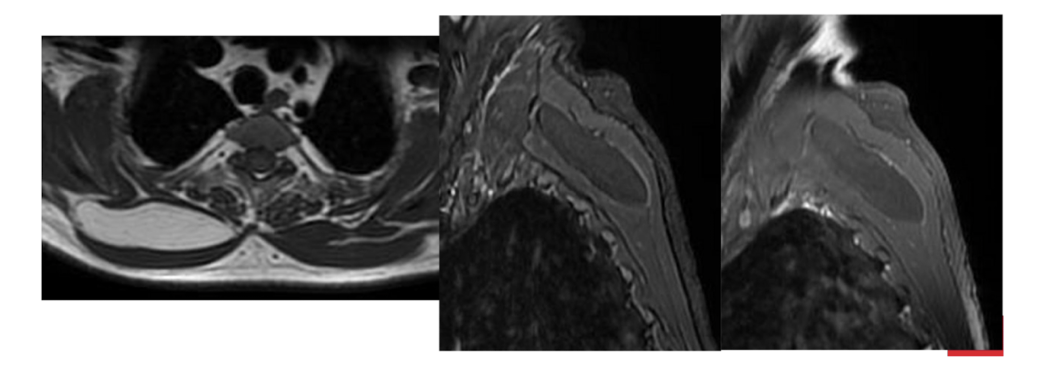
T1, STIR, T1FS C+
Tissue lipoma- benign tumour made of fat tissue
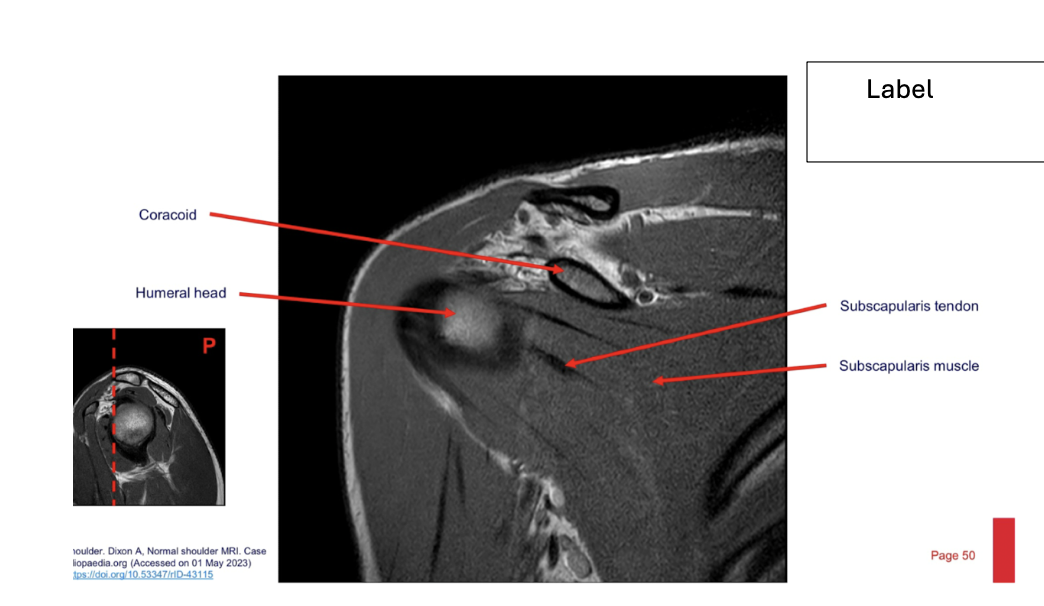
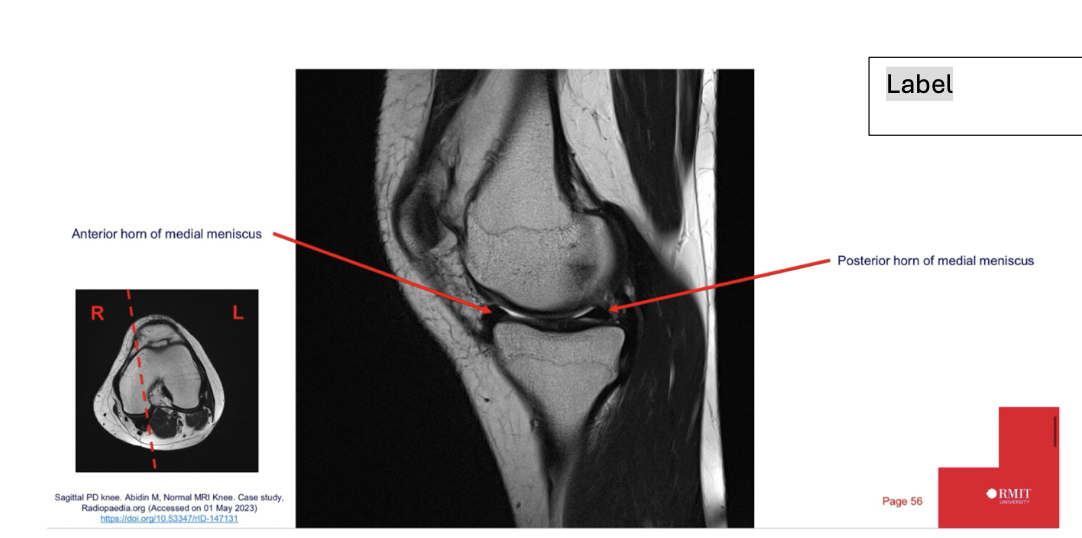
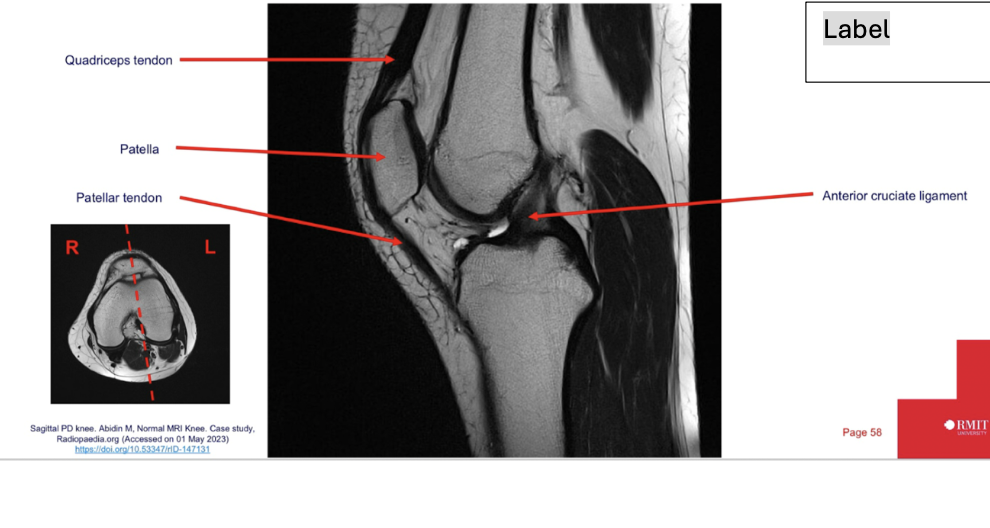
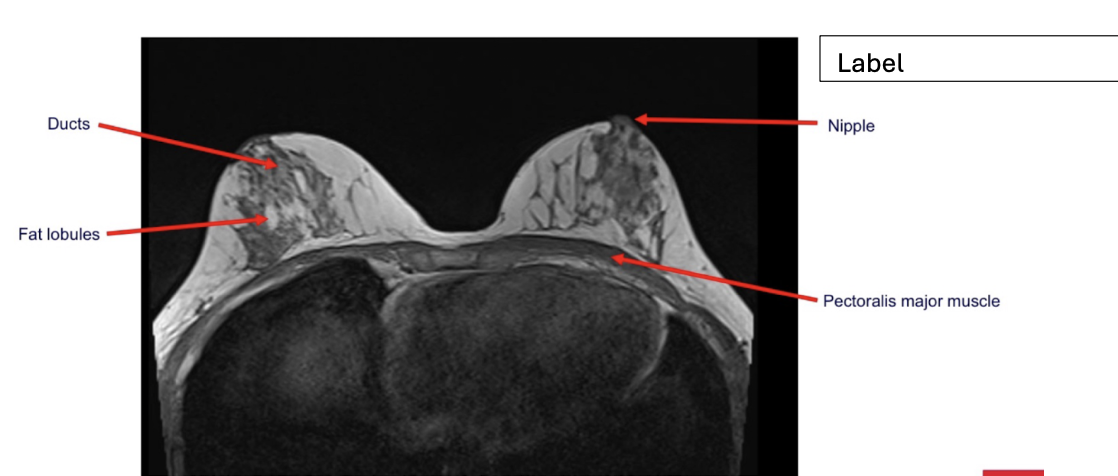
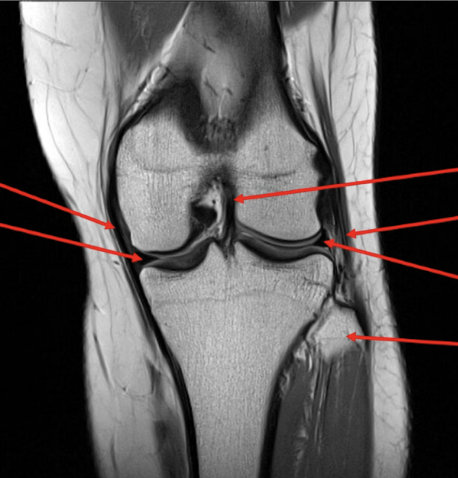
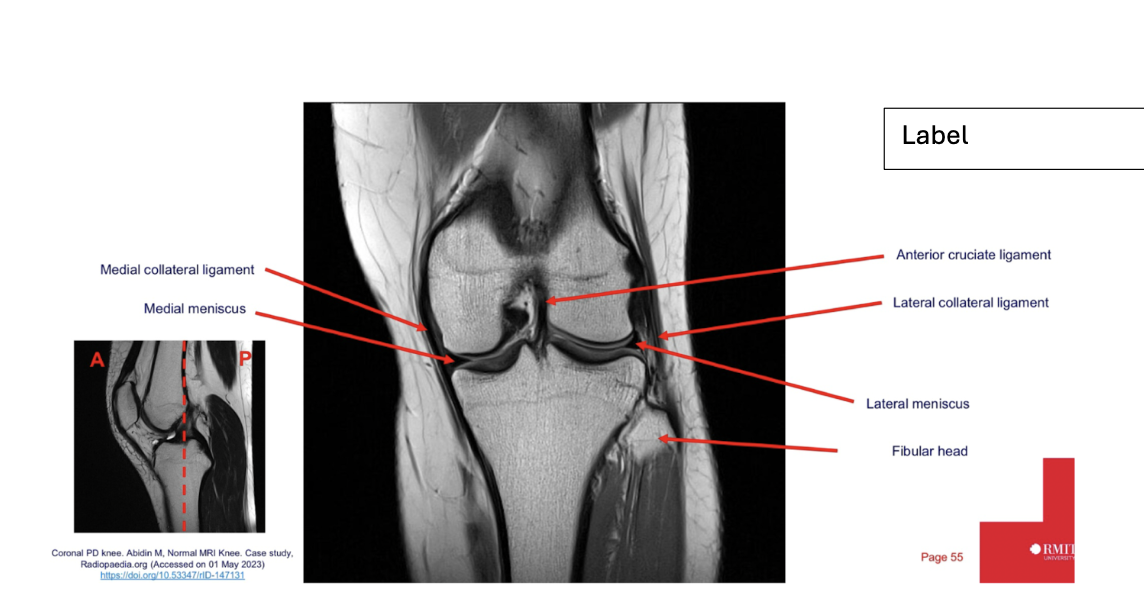
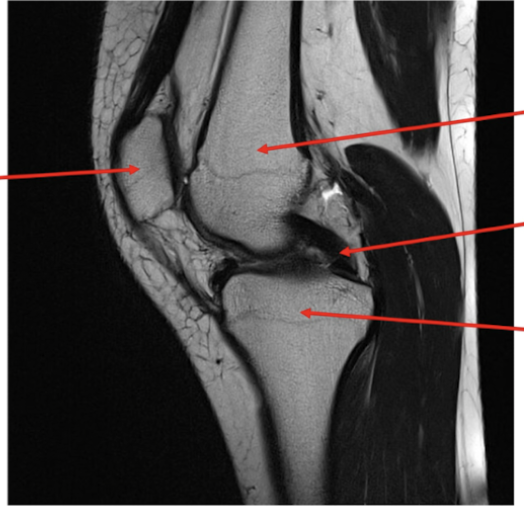
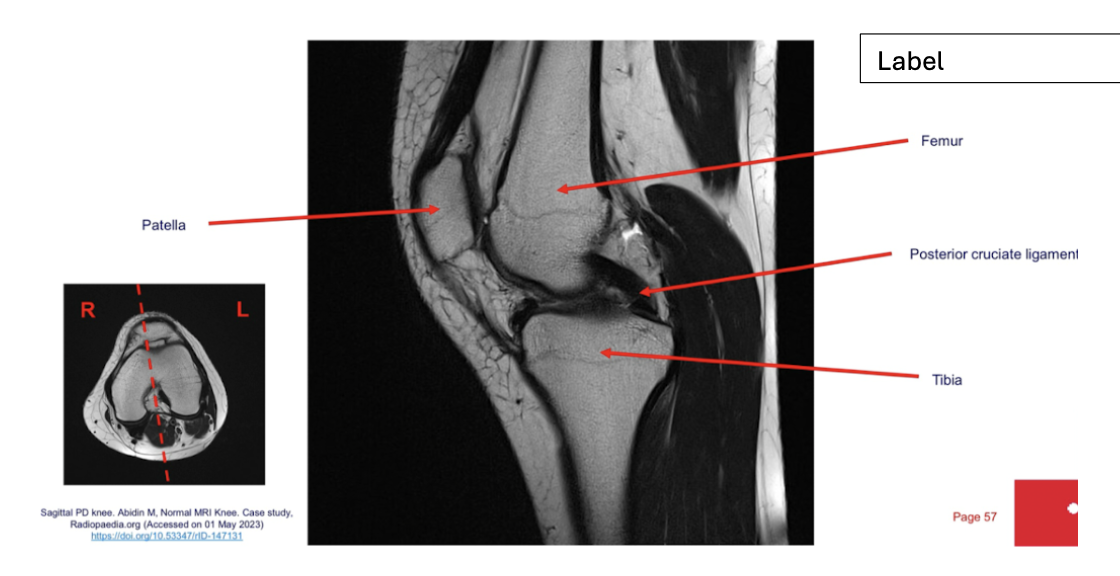
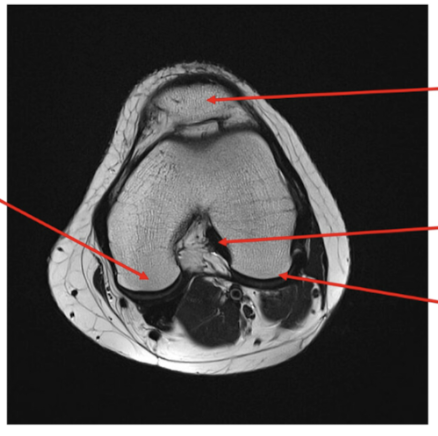
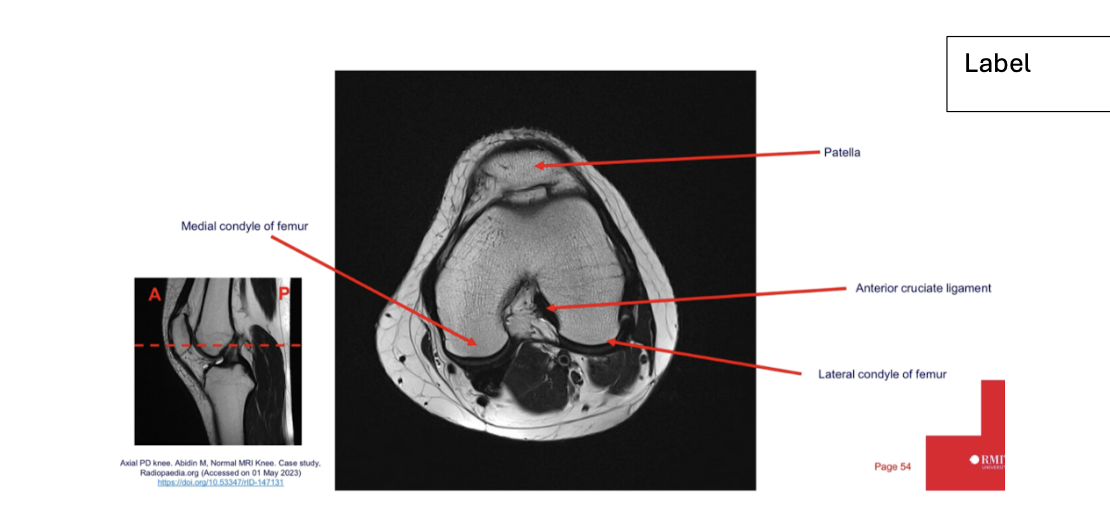
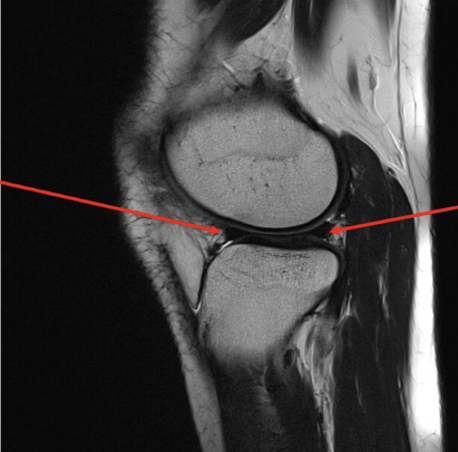
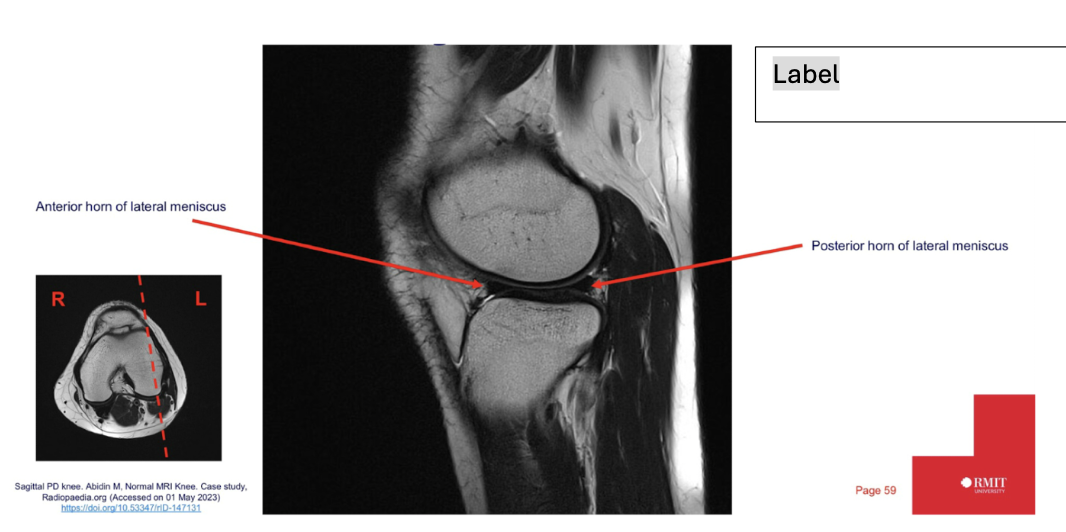
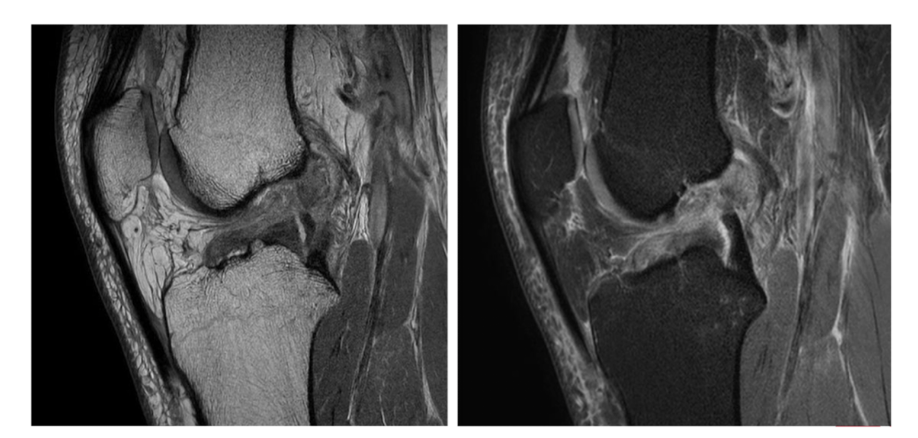
label each
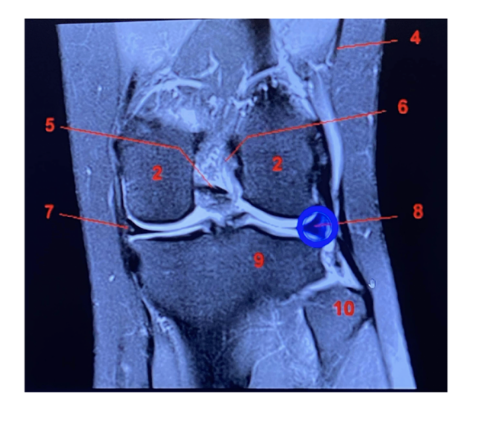
2- lateral and medial condyles of femur
4- vastus lateralis muscle
5-posterior cruciate ligament
6- anterior cruciate ligament
7- medial meniscus of knee
8- lateral meniscus of knee
9-tibia
10-fibula
What is the protocol planning for a CT thoracic angiogram?
Pt position: supine, feet 1st, arms above head
Scan range: skin margins above shoulder to iliac crests (aorta bifurcation)
Phases: non contrast and arterial phase – we will know we are in arterial phase when the aorta has maximum opacification
Recons: axial, sagittal and coronal in angio, soft tissue and lung windows
MIPs
Rotational VR
Why are the advantages of using MRI for MSK imaging?
Non-invasive
Non ionising
High level of soft tissue detail
3D imaging
Low cost compared to diagnostic surgery.
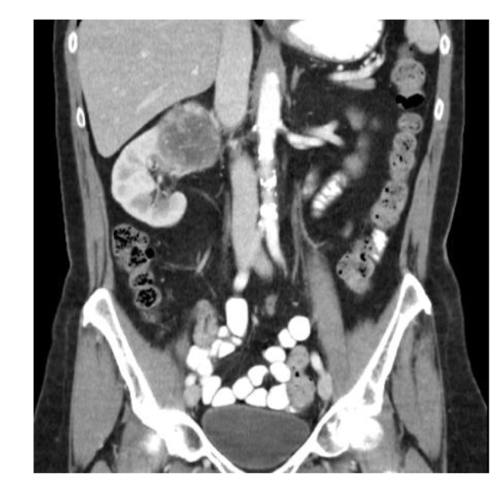
What is the pathology?
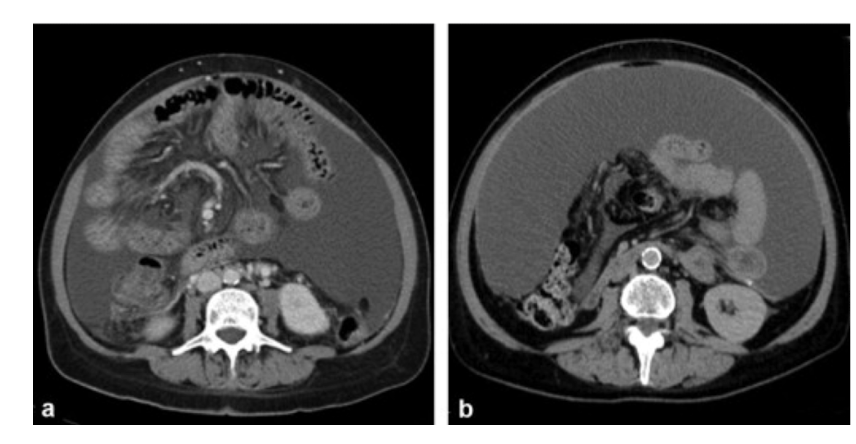
Ascites: abnormal
collection of
intraperitoneal fluid
Evidenced by the fluid within the recesses of
peritoneal cavity
What is T2 Fat Sat and what is it used for?
Shows T2 however, fat will now be supressed thus, appear dark.
It enhances contrast between pathological changes associated with fluid.
What MRI plane best shows carpal tunnel?
Axial plane
It can show flattening or oedema of muscles and nerves sitting within the carpal tunnel.
What is T2 weighting and what is it useful for?
T2 relies on long time to repetition and long time to echo.
Fat and fluid appear bright.
It is useful for identifying fluid related pathologies such as oedema.
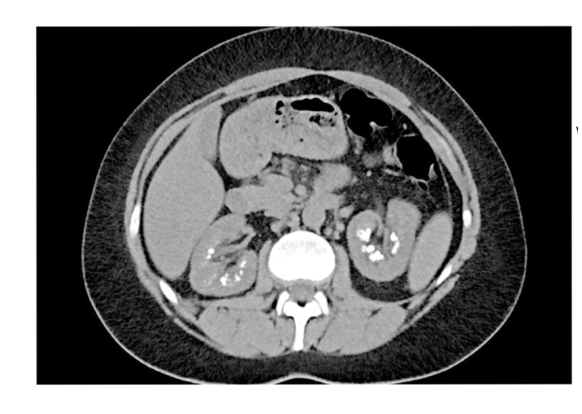
Phase + pathology?
In PVP as there is opacification of
the portal vein and the liver is also
opacified
Path = small bowel obstruction
Small bowel as its characterised by
the ridged lines
Bowels are dilated and we can’t see
any gas patterns distal to the obstruction.
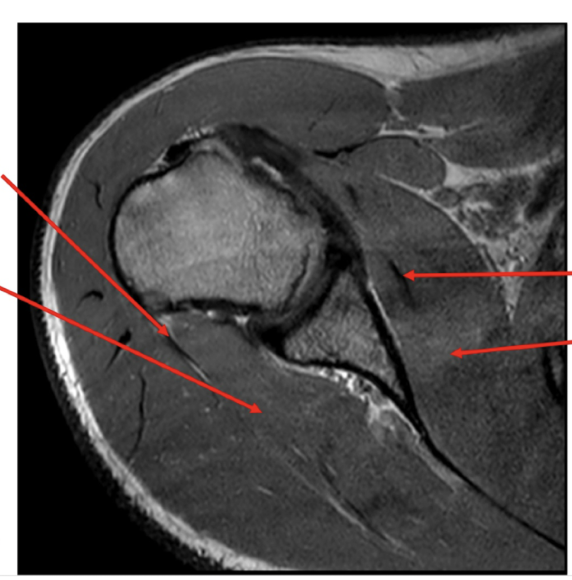
Label:
What is DWI and what is it used for?
Diffusion weighted imaging
Areas that have high signal intensity indicates there is restricted diffusion within that area and therefore, a pathological process.
Used in tumour characterisation and cerebral ischemia
What MRI imaging plane best demonstrates the glenoid labrum?
• Axial (expand? or)
What are the advantages of scanning brain in MRI?
No ionising radiation
3D imaging
High level of soft tissue contrast and detail
More sensitive and specific for abnormalities within the brain
Allows evaluation of structures that may be obscured by artefacts from bone in
CT images.
Gadolinium based contrast is less likely to cause adverse reactions than
iodinated contrast
What sequences are useful in identifying brain tumours and what does each identify?
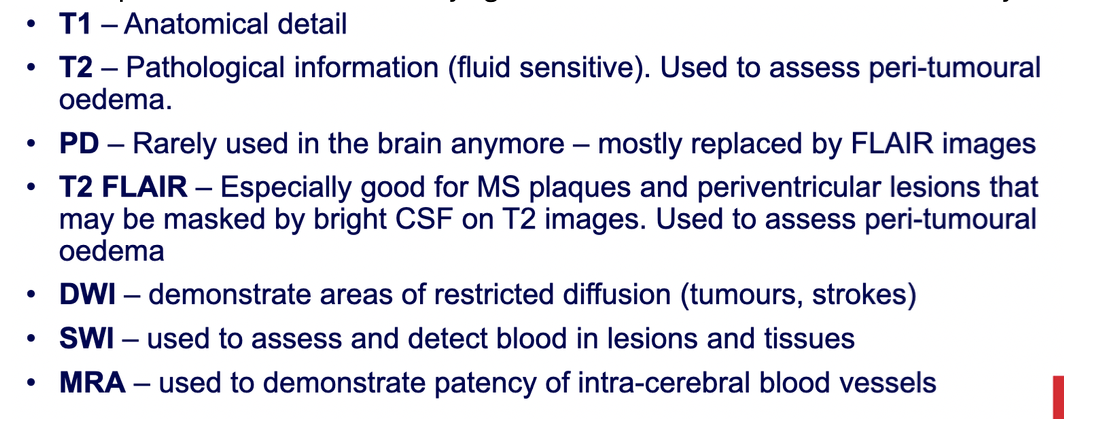
What is the phase and pathology?
Appendicitis: inflammation of
the appendix
Appendiceal wall thickening
This is a A/P C+ scan. Oral
contrast has been given as there is max opacification seen in the bowels.
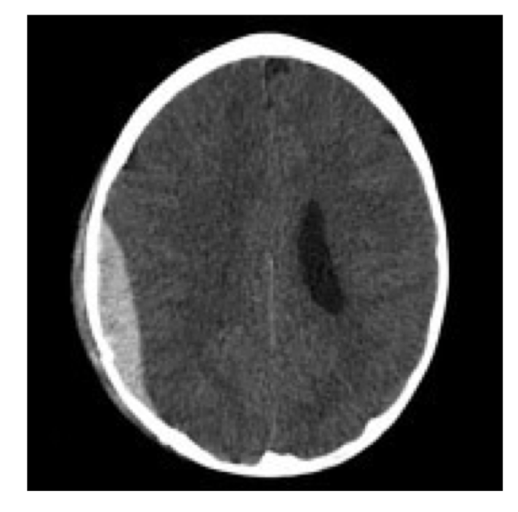
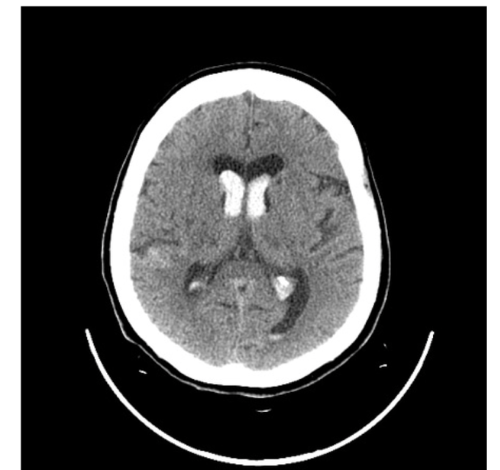
What is the pathology?
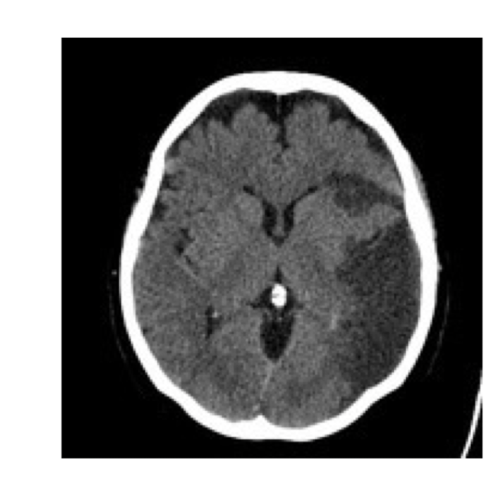
Ischaemic stroke: blood flow to
the brain has been blocked.
Hypodense areas = infarct (dead
brain tissue)
What is the sequence + pathology?
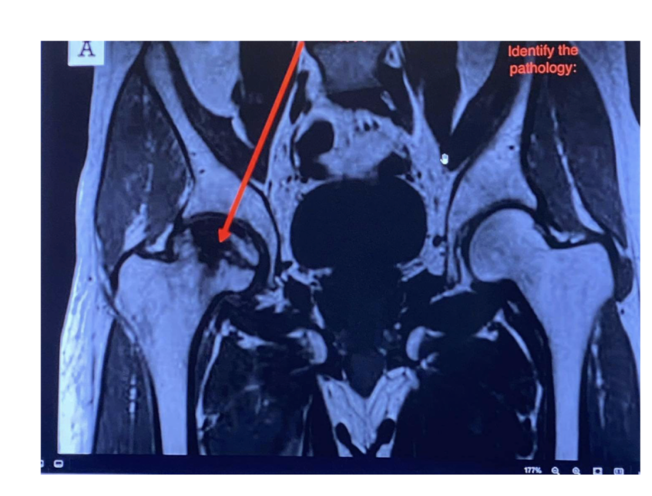
T1 – fat is bright fluid is dark
Path = avascular necrosis of the
femoral head
Lost blood supply to the femoral
head. = bone death
Decreased signal = oedema
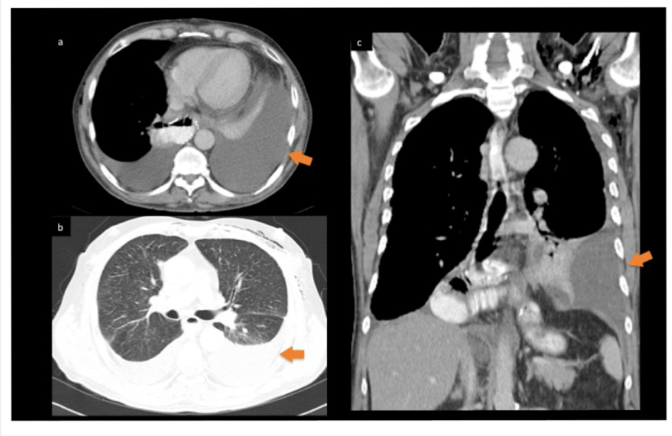
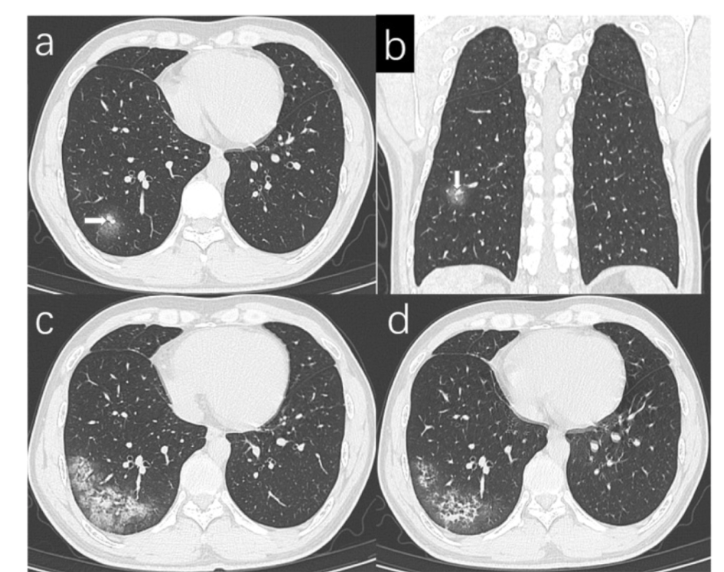
What is the protocol + pathology?
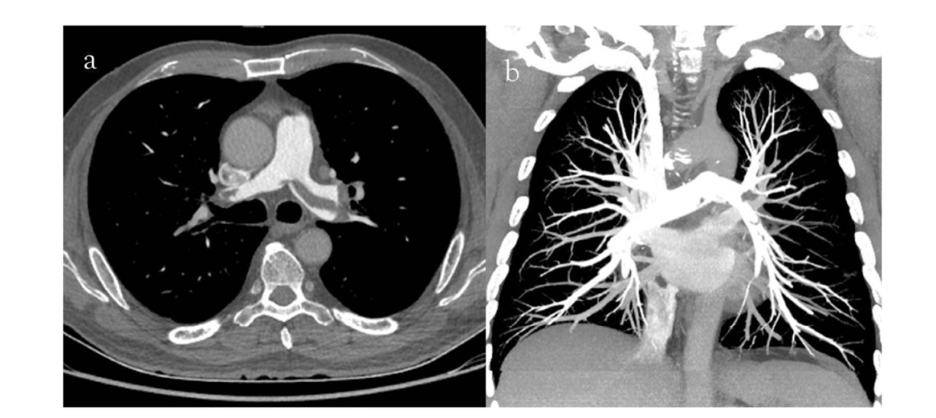
CTPA
There is max opacification within the pulmonary arteries therefore contrast was used and it’s in an EARLY arterial phase.
Path = pulmonary embolism with an occlusion in the left pulmonary artery
Filling defect characterised by hypodense streak within the left pulmonary artery.
Coronal MIP = highest attenuation values within the voxel selected
What is the protocol + pathology?

Non contrast A/P CT
Path = hypodense renal cyst
Well defined margins
Best seen on Quad Phase Renal
CT
No enhancement therefore,
composed of water
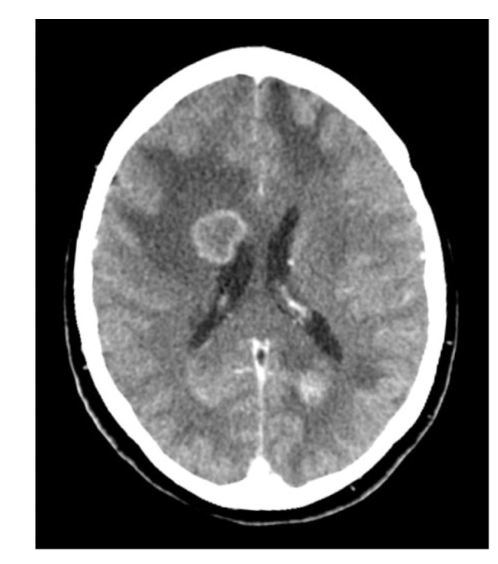
What is the protocol + pathology?

CT non con brain
Intraparenchymal
haemorrhage: brain bleed within the brain parenchyma
Hyperattenuating mass posteriorly in the occipital lobe
Midline shift
Adjacent oedema.
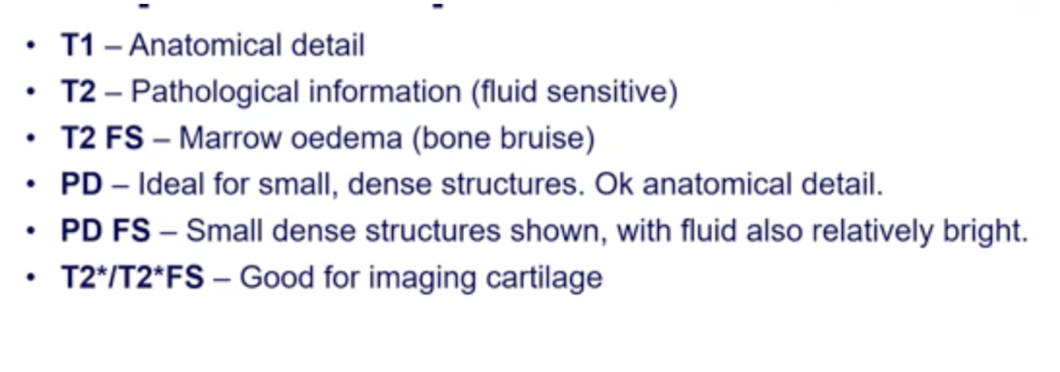
What are the sequences used in MRI MSK and what does each provide?
What is the CT + Pathology?
Abdomen CT C+
- In arterial phase as the abdominal
aorta has maximum opacification • Path = renal cell carcinoma
- Heterogenous mass on the kidney
with poorly defined margins
What is the planning for CT pulmonary angiography?
Pt position: supine, feet 1st hands, hands above head
Scan range: lung apices to base of lung
Phase: minimal scan delay to achieve max opacification in the pulmonary
arteries only
Recons – axial, coronal sag, MIPs in angio, soft tissue and lung windows.
Scan + pathology?
Non con CT
Path = primary brain tumour
Adjacent oedema
Double ring sign
Contrast phase should be
done to see if tumour is vascular
What is the protocol planning for a non con brain CT?
Pt position: supine, head 1st , chin tucked in (reduce dose to orbits)
Scan range: C2 lamina to skull vertex
Phase: non contrast therefore, no vessel enhancement should be seen.
Recons: axial, sagittal and coronal soft tissue and bone windows.

What is CT and pathology?
Abdomen C-
Path = pneumoperitoneum
Gas seen anteriorly
It has pushed the liver
posteriorly.
What is the post contrast brain planning protocol?
Pt position: supine, head 1st, chin tucked (reduce dose to orbits)
Scan range: C2 lamina to skull vertex.
• Phase: delayed phase involves a 5-minute scan delay post contrast injection
- Good opacification in cerebral vessel indicates enough time has passed for the
contrast to pass the blood brain barrier.
• Recons: axial, sagittal and coronal in bone and soft tissue window
What is the planning protocol for a Quad phase liver?
Pt position: supine, feet 1st, hands above head (reduce dose to arms and assist
with dose modulation)
Scan range: diaphragm to iliac crests
Phases:
- Non contrast: no vessel enhancement
- Arterial: 15-30s delay– arteries should be enhanced
- Portal venous: 50-70s delay – portal vein should be enhanced.
- Delayed: 2-5min delay – portal vein will still be enhanced but not at its maximum
opacification as in PVP
• Recons: axial, coronal and sagittal in soft tissue and lung windows.
CT + pathology?
KUB CT – image presents non-con
Path = renal calculi evidenced by the
hyperattenuating stones seen within the kidney
What appears dark on every MRI scan?
• Tendons and ligaments
On a T1 weighted image oedema appears dark because it has a ---- relaxation time?
Long relaxation time therefore,
protons in (fluid-rich) tissue take longer to realign with the magnetic field, resulting in low signal (dark appearance) on T1 images.
What is the CT + Pathology?
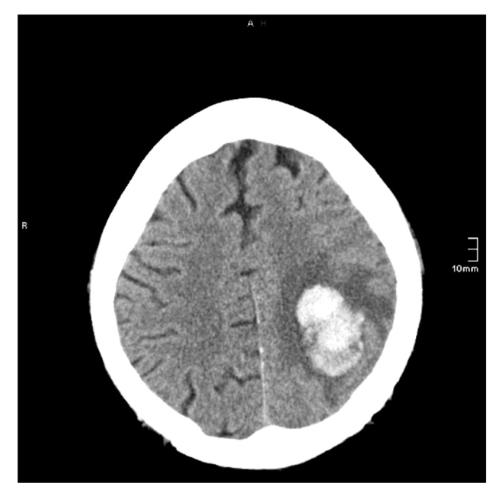
Brain CT C-
Path = haemorrhagic stroke
Hyperattenuating mass
Adjacent oedema to the bleed
What is the CT + Pathology?
Chest CT C-
Path = left sided pleural e`usion
Hazy areas of consolidation
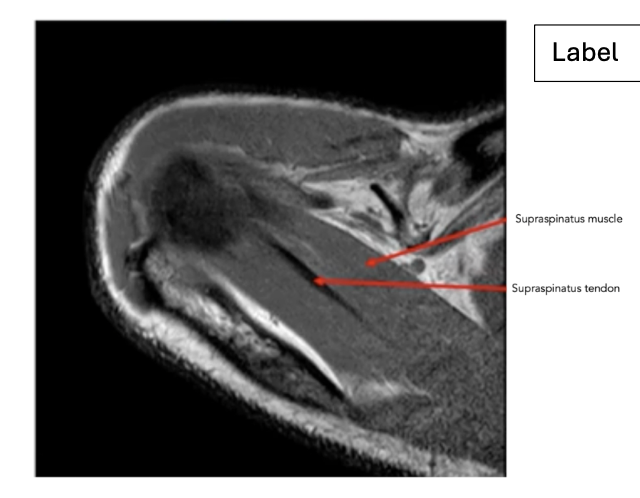
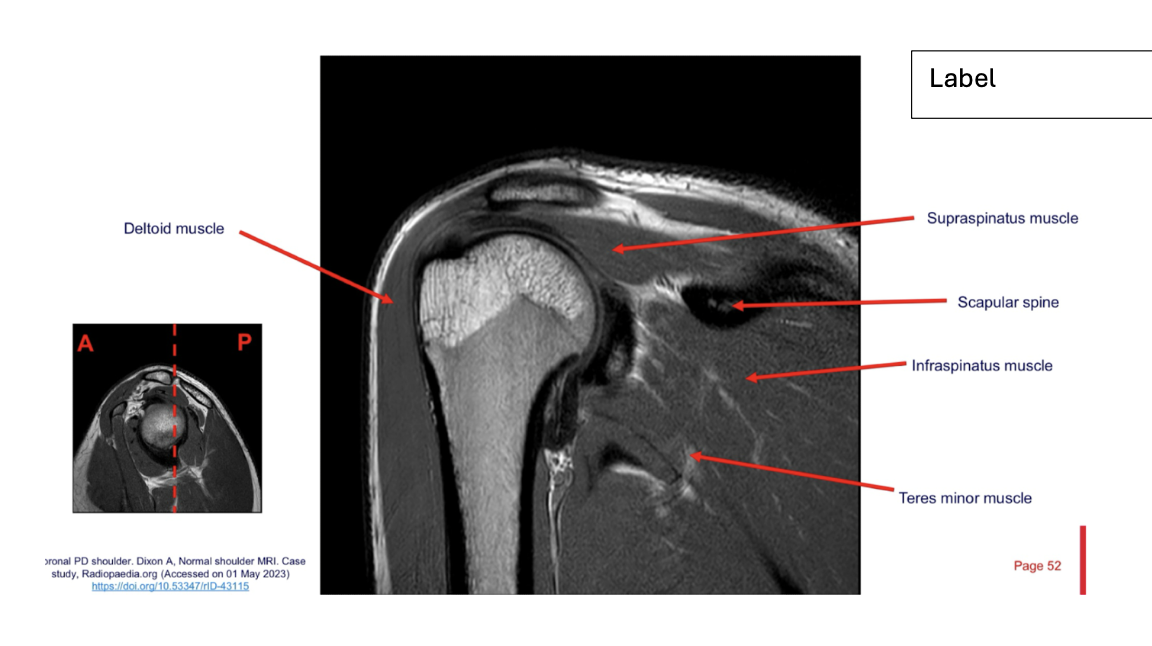
What is the most common rotator cuff tendon tear?
• Supraspinatus tendon
What is the CT + Pathology?
Brain CT C-
Path = subdural haemorrhage:
blood between the dura and
subarachnoid matter
Characterised by its convex shape.
Hyperattenuating spot seen
laterally and posteriorly.
What is the CT + Pathology?

HRCT
Path = bronchiectasis: dilation of the bronchial wall due to chronic inflammation
Ground glass appearance: hazy areas of increased attenuation through the lung.
Bronchial wall thickening
What is a T1 weighting and what is it most useful for?
T1 weighting has a short time to repetition and a short time to echo
This is characterised by the appearance of fat as bright on images and fluid as
dark
It is useful in highlighting anatomical detail and useful for pre and post contrast
studies
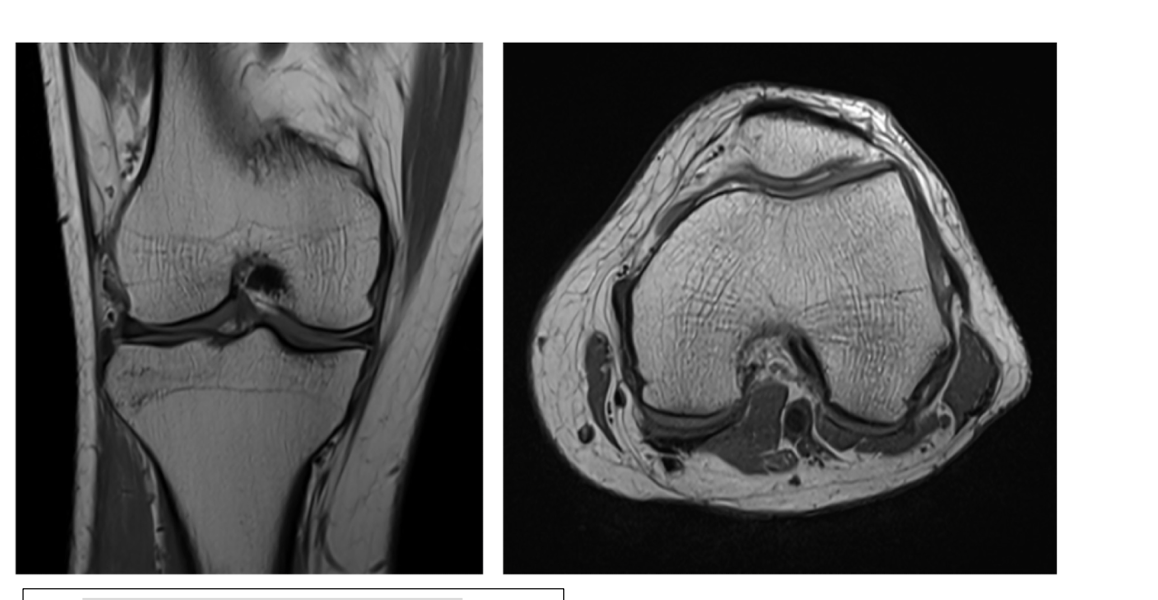
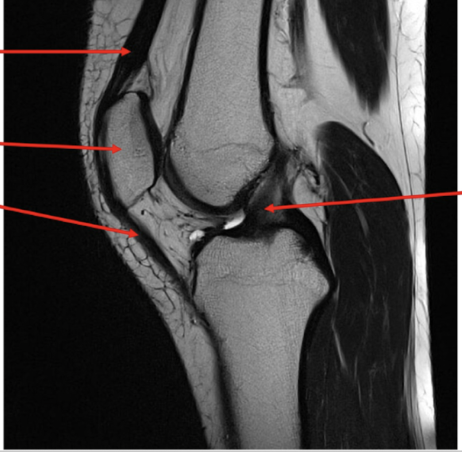
Pathology

Medial collateral ligament tear
High signal intensity within the
medial aspect of the knee indicative of fluid presence as a result of a pathological process in this case the tear.
CT protocol + Pathology?
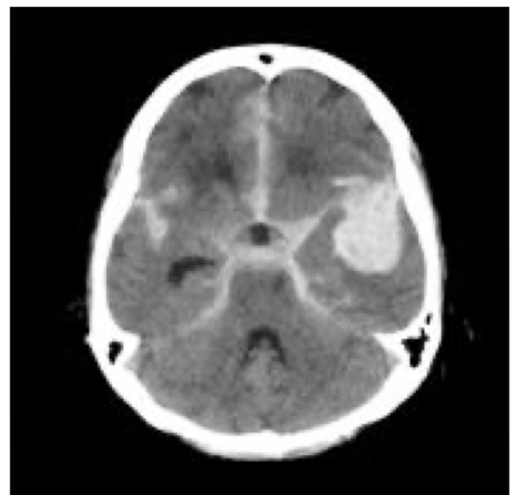
Brain C-
Subarachnoid haemorrhage: brain bleed within the subarachnoid space and pia mater
Hyper attenuation within the basal cistern
Located around the circle of Willis
CT protocol + Pathology?

Brain C-
Glioma: tumour that arises within the brain and spinal cord
Mass extends across the
CT protocol + Pathology?
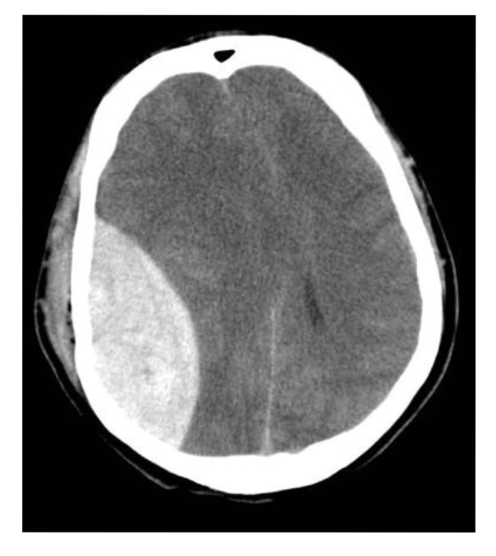
Brain C-
Extradural haemorrhage: bleed between the skull and the dura
Convex shape
Hyperattenuating
Midline shift
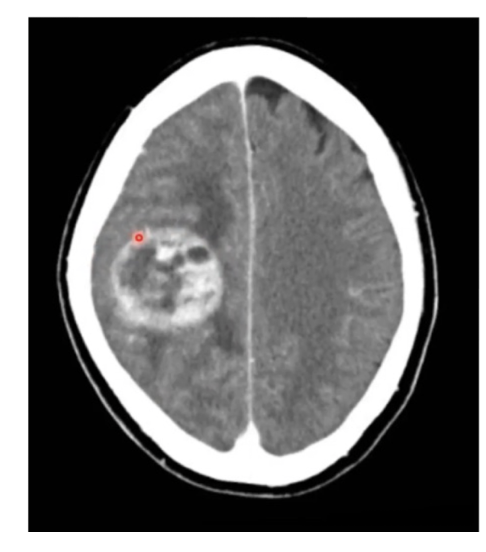
CT protocol + Pathology?
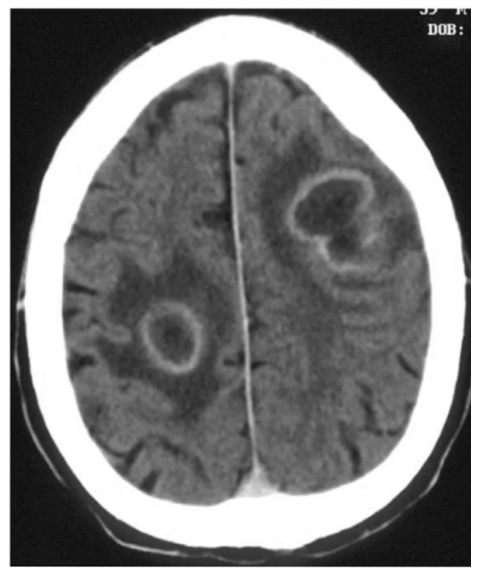
Brain C-
Abscess: fluid filled pockets of infection within the brain parenchyma
Ring like structure where the hypodense inner ring is pus and the hyperattenuating outer ring is other fluid.
Adjacent phasogenic oedema.
CT protocol + Pathology?
C- brain
Depressed skull fracture: parts of the skull have sunken into the cranium.
There is steps within the cortical margins of the frontal and temporal bones
label
What is the sequence and why?
• T1 – fluid is dark but fat is bright
Label

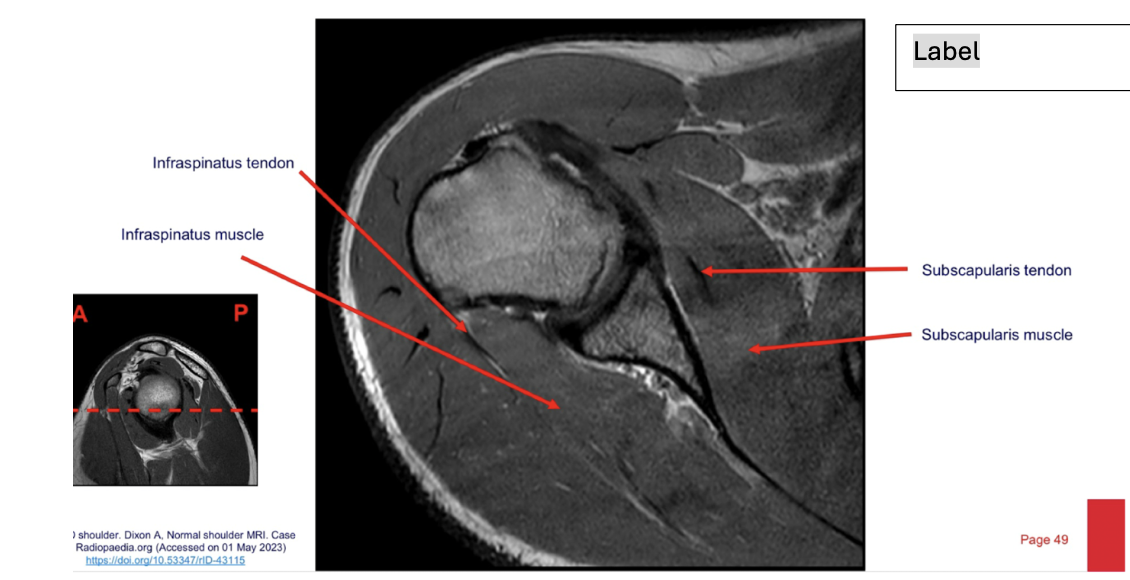
Sequence + Pathology?
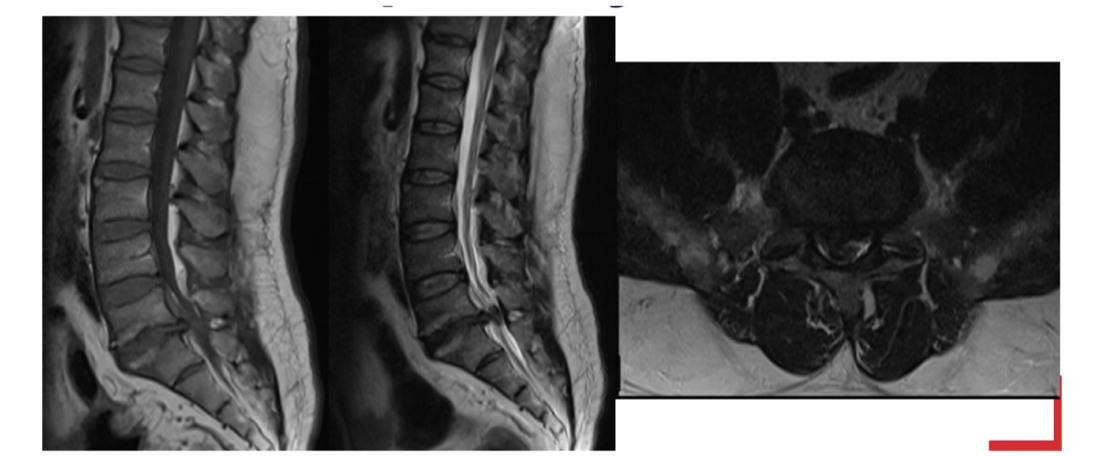
T1,T2
Cauda Equina syndrome
L5/S1 disk space herniation compressing the cauda equina.
Signal intensity is lost in T2 sag as you get to L5/S1 disk space.
Sequences + pathology?
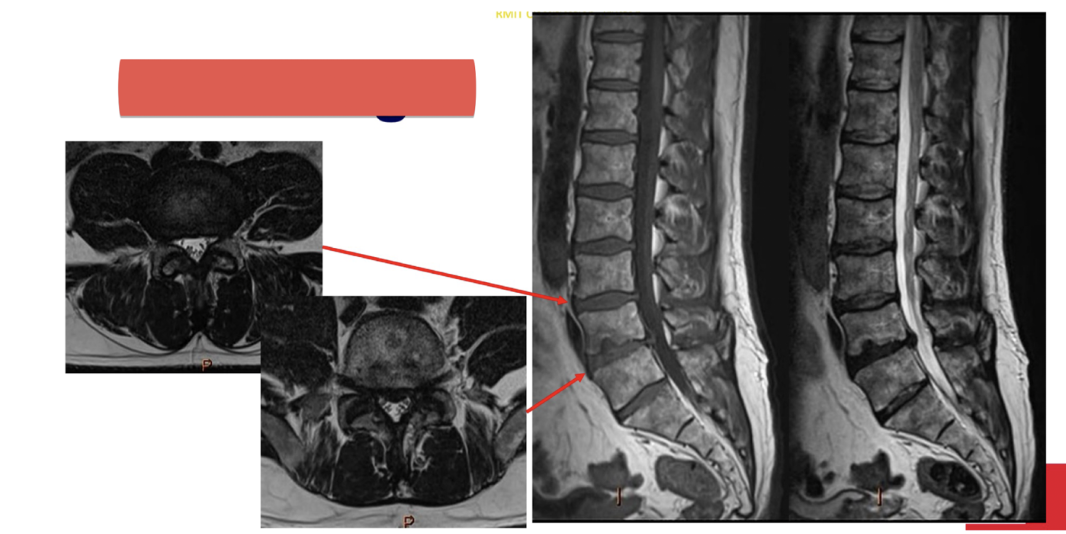
Axial=T2,1st sag=T1,2nd sag=T2
Anterior disk bulge of L3/4 and L4/5 disks
Anterior longitudinal ligament has lost its normal shape as it is being pushed
anteriorly by the disk bulges.
Label
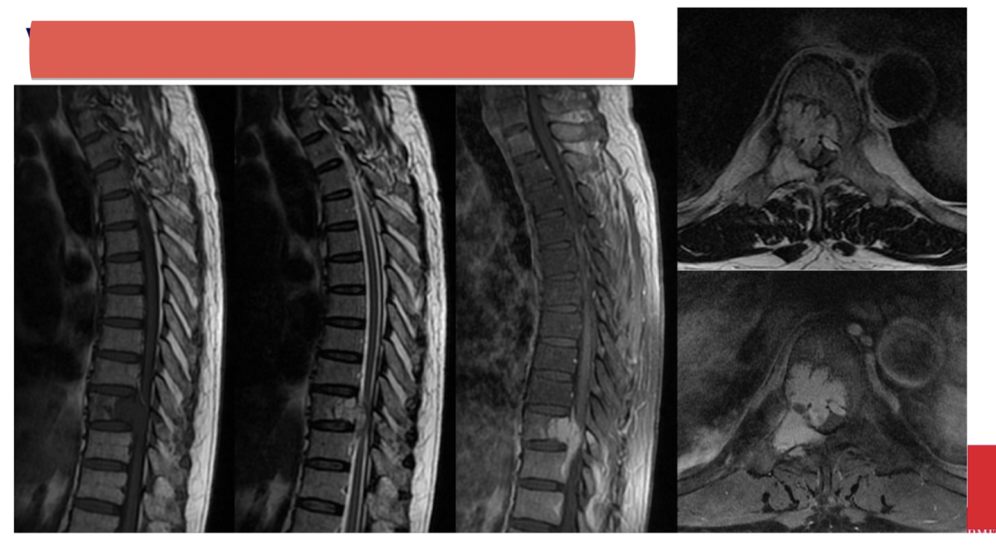
Sequences + pathology?
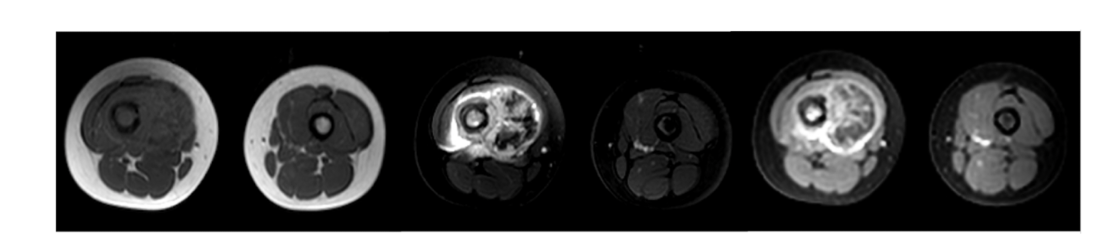
T1, STIR, T1FS C+
Sarcoma within the muscle of the right thigh
T1 – lacking symmetry between the left and right thigh
STIR – fluid sensitive scan that has picked up fluid involvement hence,
suggestive of a pathological process.
T1FS C+ - vascular involvement has there is high signal from contrast
situated inside the sarcoma.
Sequences + pathology?
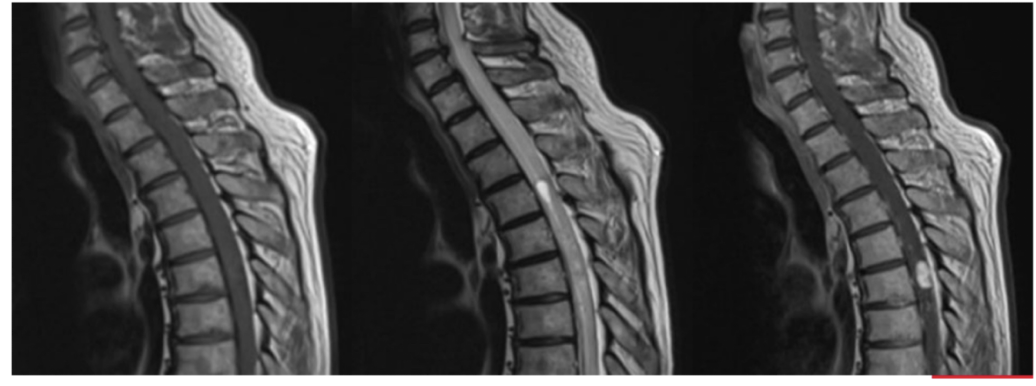
T1
• Syrinx: fluid filled cyst that sits within the spinal cord • Areas of increased signal present
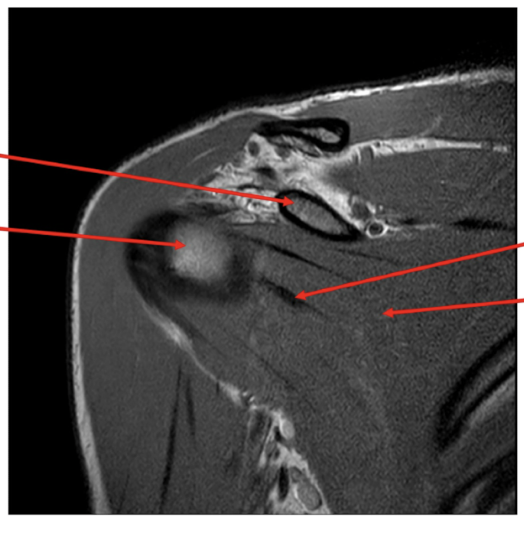
Sequences + why?
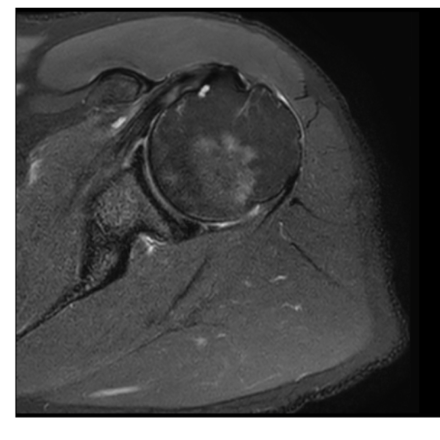
T2FS
• Spots of high signal fluid around the humeral head
• Fat is dark hence has been supressed.
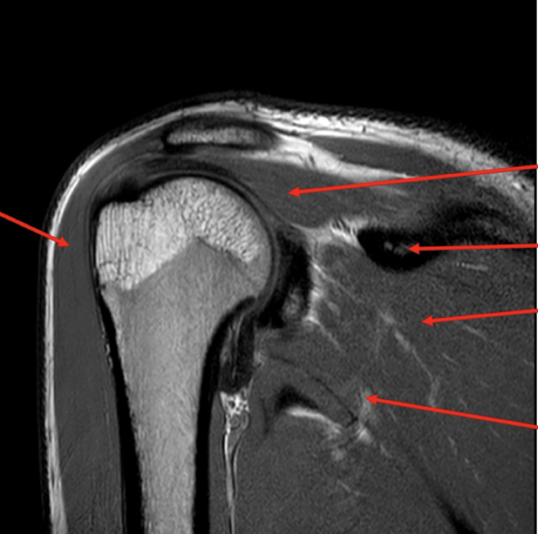
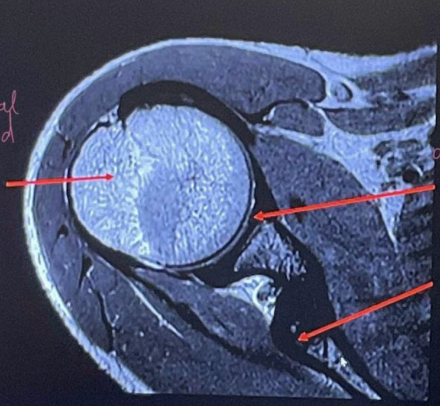
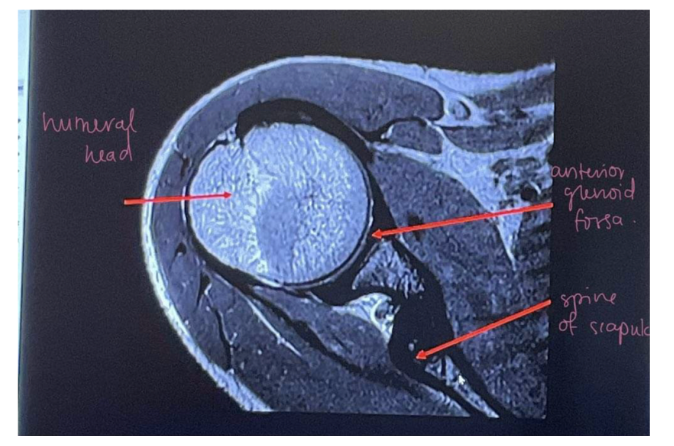
Label
Pathology?
• Vertebral tumour that has invaded the spinal cord
Sequence + Why?

T2 – fat is bright and fluid
is bright
Label
Label
Sequence + Why?
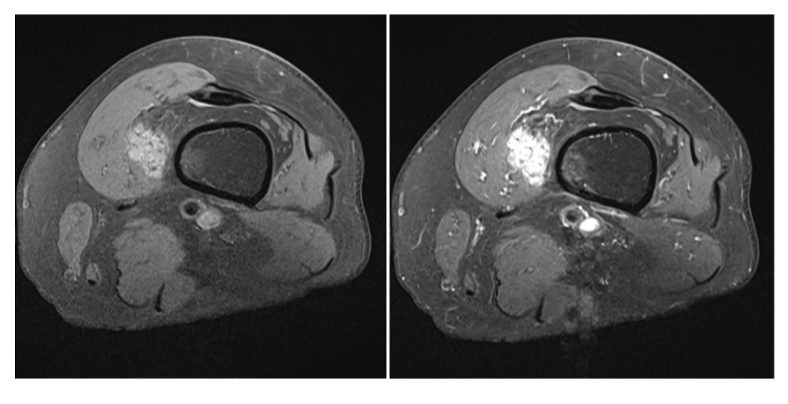
1st – T1FS: fluid is dark and
fat has been supressed
2nd T1FS C+: vessel
enhancement however T1 characteristics still remain
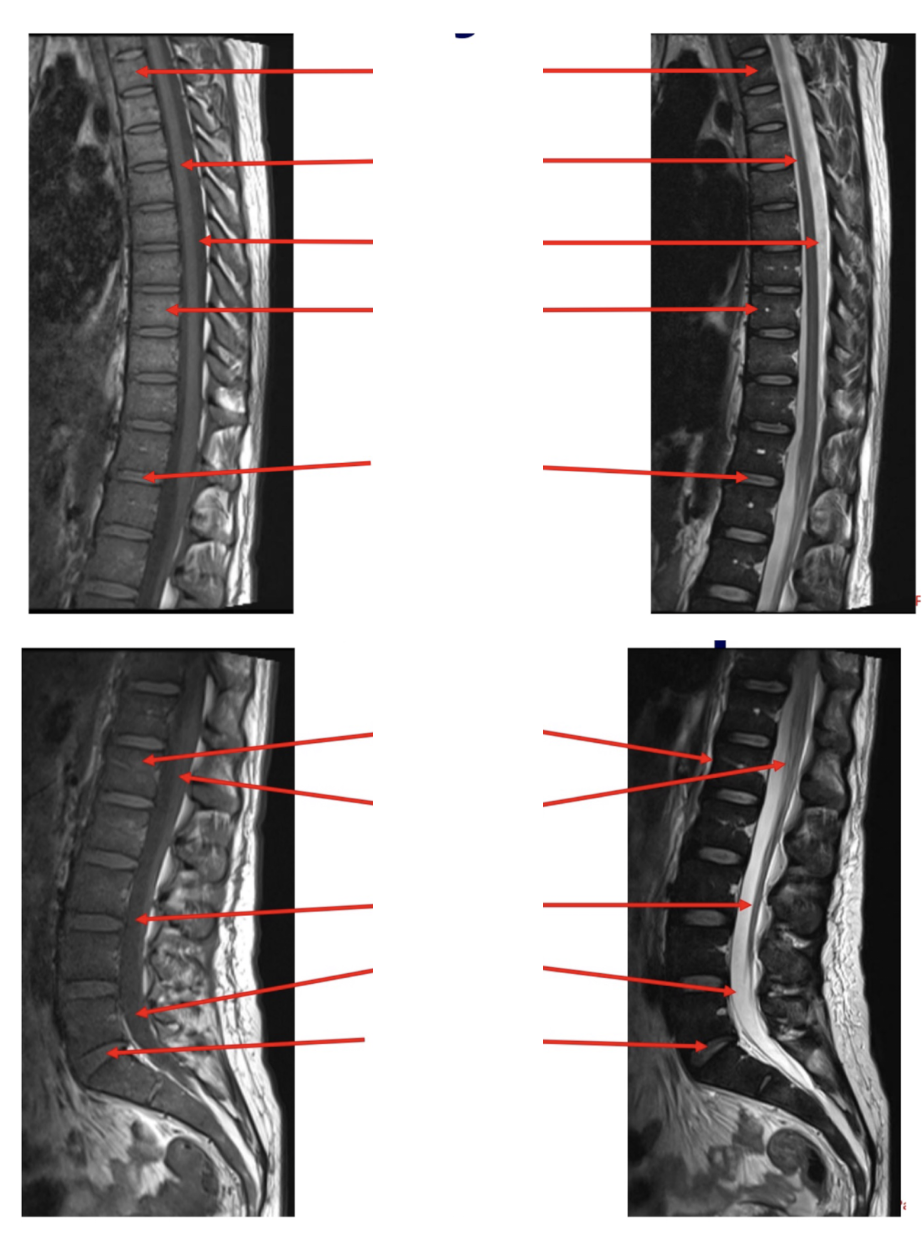
Label
\
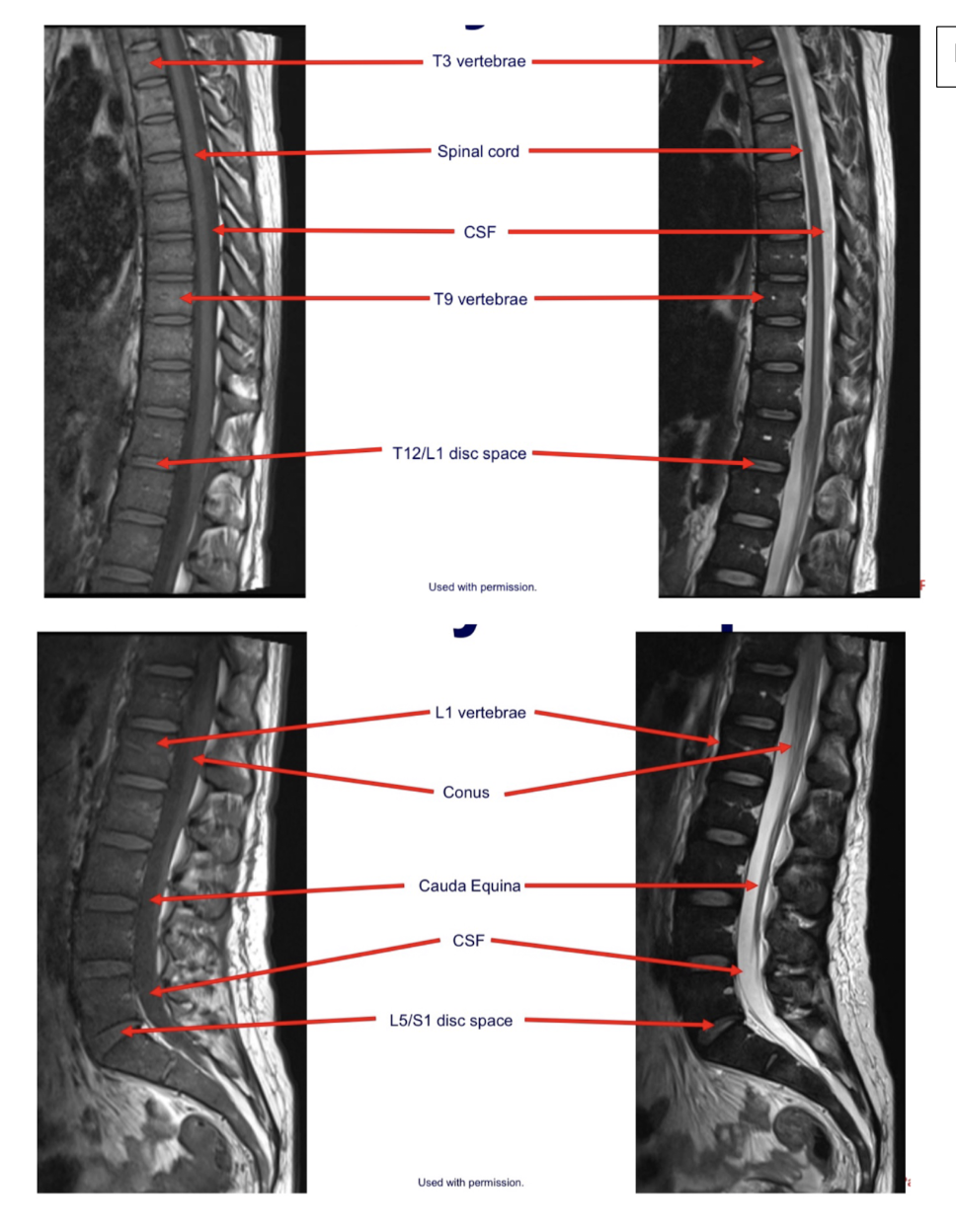
Label
Sequences + Pathology?
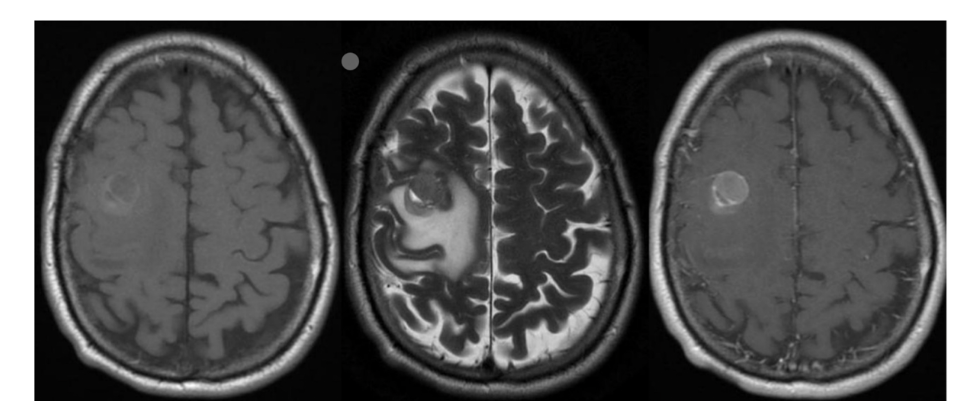
1st = T1: the white matter is brighter than the grey matter
2nd = T2: the white matter is darker than the grey matter
3rd = T1 C+: still has T1 characteristics but there is vascular involvement as there is
increased signal from the lesion
Path = intra-axial lesions
Sequence + Why?

PD- proton density
• Fat is bright, fluid is bright, intermediate signal from muscle.
What is the planning protocol for a post contrast CT Chest?
Pt position: supine, feet 1st, hands above head (reduce dose to arms and allows for
accurate dose modulation)
Scan range: skin margins above shoulder to diaphragm.
Phase: arterial phase (30s delay) should have max opacification in the thoracic aorta
and its branching vessels.
Recons: axial, coronal and sagittal in bone, lung and soft tissue windows.
Label
Sequences + Pathology
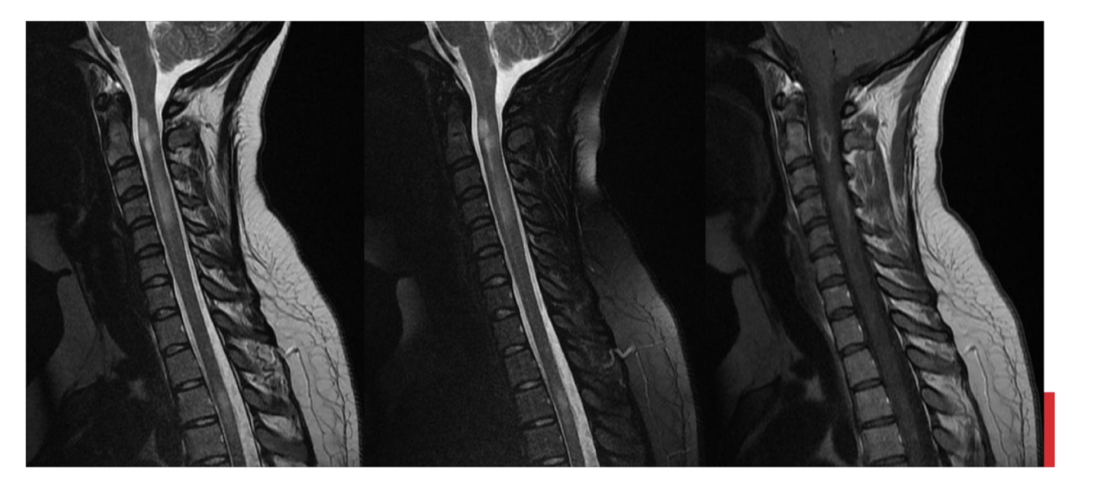
T2, T2FS, T1C+
Path = multiple sclerosis
Increased signal within the spinal cord confirming the presence of lesions
Label
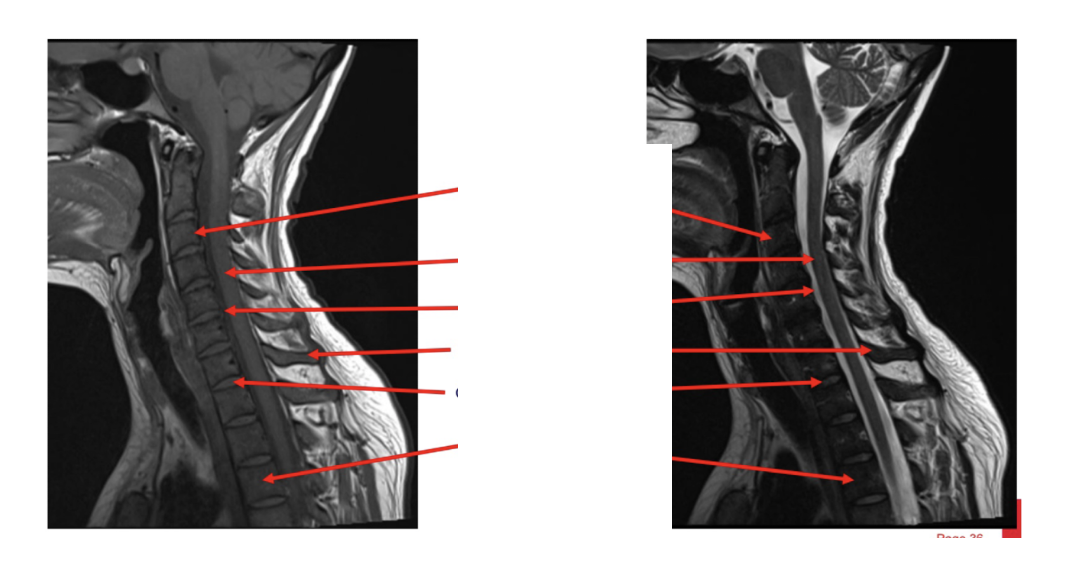
Label
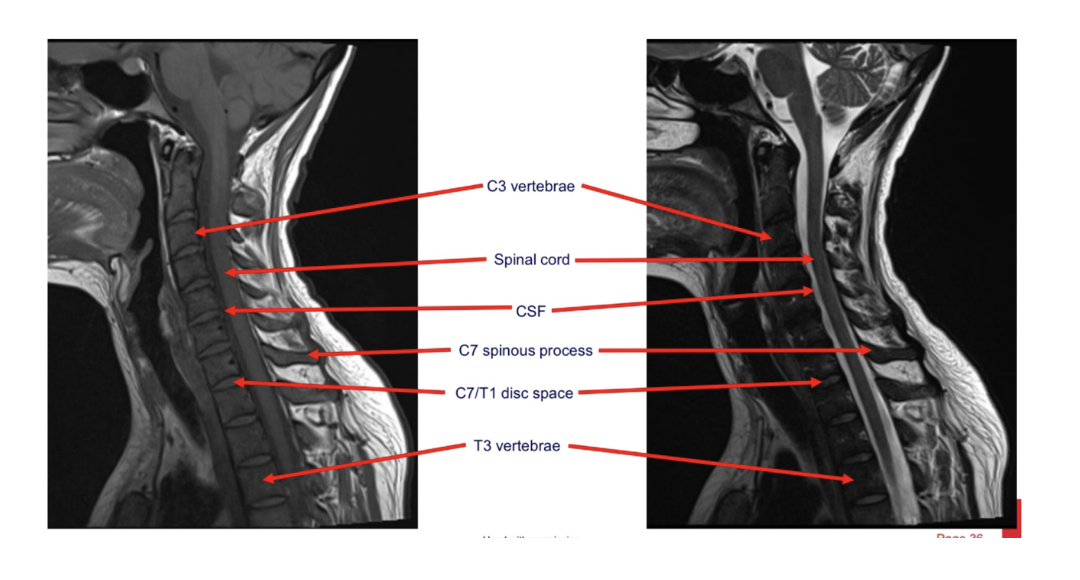
Label

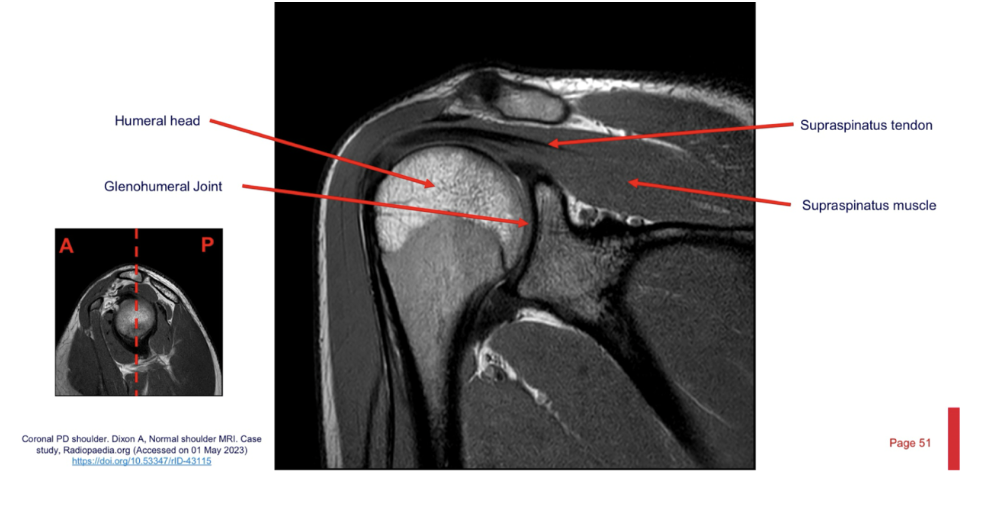
What is the proton density MRI sequence and what is it used for?
Receives signal from areas that have the highest proton density, and these appear
bright on an image.
Fat usually has the highest signal and appears bright.
Used for brain imaging as there is good grey and white matter contrast.
Also used for MSK imaging.
What is the T1 FS sequence and what is it used for?
Adipose tissue appears dark.
This allows for tissue characterisation and better visualisation of contrast material.
CT protocol + pathology?
Brain C-
Path = intraventricular haemorrhage
Abnormal hyper attenuation in lateral ventricles indicating the presence of blood.
CT protocol + pathology?
Brain C-
Path = metastases: spread of cancer from its primary site
Ring sign where there is a hyperattenuating capsule
CT protocol + pathology?
Chest C-
Path = pneumonia: infection of the lungs where pus sits within the alveoli
Hazy appearances in lung consistent with consolidation
Pulmonary consolidation
What is patient prep in CT?
Positive patient ID
Pregnancy status
Contrast safety risk.
- Previous allergic reaction to contrast and any known allergies?
- Thyroid issues?
- Kidney disease?
- Diabetes and taking metformin?
Removal of radiopaque objects in ROI
Practice Breathing instructions prior to the commencement of examination if required.
CT protocol + pathology?

CT thoracic angiogram – delayed arterial
phase.
Path = dissection of the ascending aorta:
there is a tear in the intima causing
blood to leak into the media
intimal flap
dilated ascending aorta.
density di`erences within the aorta
What is pathway of IV contrast from the right anti-cubital fossa?
Rt basilic v – Rt axillary v – Rt subclavian v – SVC – Rt atrium – Rt ventricle – Pulmonary a –
pulmonary V – Lt atrium – Lt ventricle – ascending aorta
Label
What are the disadvantages of using MRI for MSK imaging?
Poor bony detail compared to CT
Decreased availability
Decreased pt compliance – claustrophobia as well as pt movement due to long scan times
More expensive
Increased safety considerations
What are IV contrast side e`ects and what can be done to minimise these from occurring?
Side effects:
- Allergic reaction
- Nauseous
- Vomiting, coughing, choking.
• Preventative methods:
- Safety screening prior to giving contrast.
- Having an anaphylactic or emergency kit close by
Label
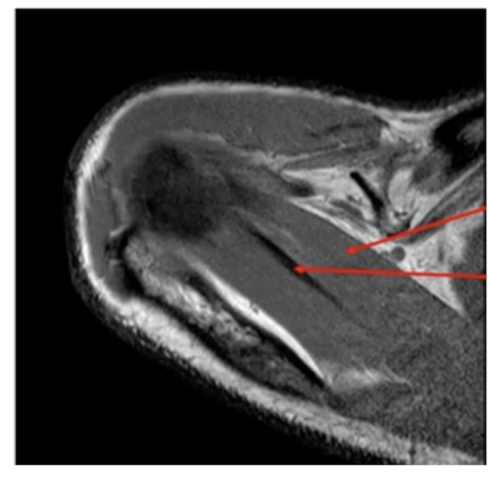
Sequence + pathology?
1st = PD: intermediate signal from muscle and fat is bright, image quality is much better
2nd = PD FS: fat has been supressed appearing much darker
Path = complete ACL tear: in a normal knee you would see a black band which is the acl sitting
across the anterior aspect of the tibia and extending to the posterior aspect on the femur. This is not present at all hence, a tear.
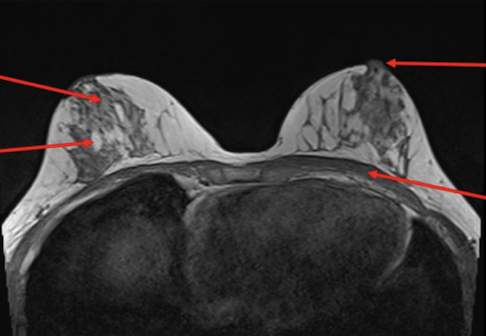
Sequence + pathology?
PD, PDFS
Path = supraspinatus tendon tear
- You can follow the tendon and see that it stops just above the humeral head rather than
attaching to the lateral aspect of the head.
- More prominent of the PDFS you can see high signal around the lateral aspect of the humerus
indicative of a pathological process occurring because of the tear.
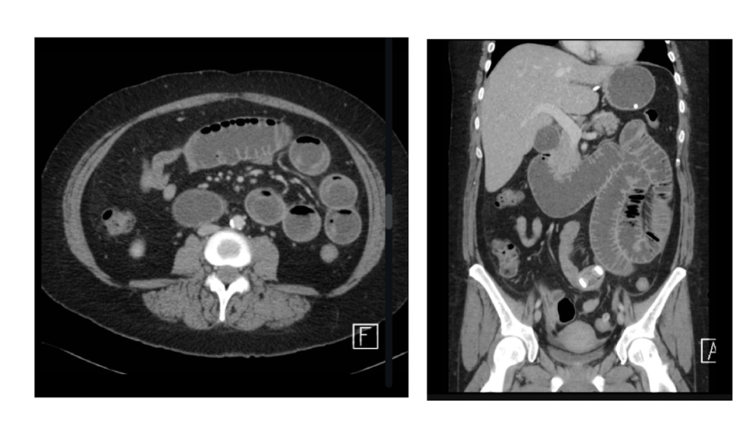
CT protocol + pathology

Quad Phase Renal CT
Path = hydronephrosis: swelling of the
kidney and ureters caused by a blockage
in the path of urine.
Significant dilation of kidneys
Hyperattenuating calculi causing the
occlusion of the path of urine from the kidney to bladder.
What is the planning protocol for a post contrast A/P CT?
Pt position: supine, feet 1st, hands above head (reduce dose to arms and allows for appropriate
dose modulation)
Scan range: diaphragms to pubic symphysis.
Phases: portal venous phase (50-70s post injection scan delay) – should see max opacification
in the portal vein
Recons: axial, sagittal and coronal in soft tissue and lung windows.
What is the planning protocol for a high-resolution CT (HRCT)
Pt position: supine, feet 1st, hands above head (reduce dose to arms and allows for appropriate dose modulation)
Scan range: skin edge above shoulders to diaphragms.
Phase: non contrast
Recons:
INSPIRATION – axial in mediastinal, bone and lung window
EXPIRATION – axial in lung window only.