Bacterial Morphology III
1/61
Earn XP
Description and Tags
Lec 4 - Exam 1
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
62 Terms
Gram negative bacteria have 2 cell membranes:
The outer membrane
The cytoplasmic membrane
between the 2 membranes lies the periplasm
The outer membrane of gram negative bacteria consists of:
An inner layer of phospholipids
An outer layer of LPS (lipopolysaccharide)
LPS is ________, so the hydrophilic lipid A portion of LPS is anchored in the _________ layer of the outer membrane.
amphipathic
phospholipid
The outer membrane of gram negative bacteria also contains cell surface receptors and _______, which form small, _____________ through the outer membrane.
porins
non-specific hydrophilic channels
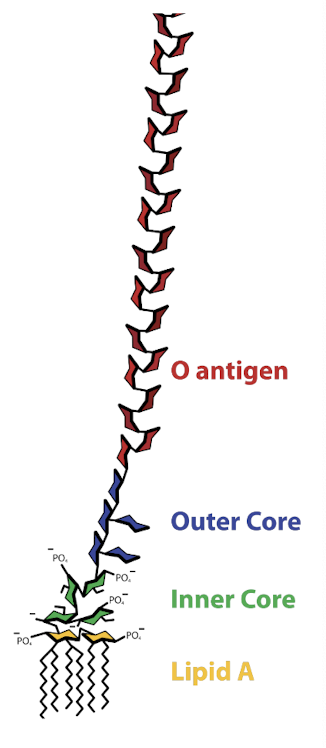
LPS consists of
lipid A + core + O-Antigen
The LPS is ______ charged with a ________ surface.
negatively
hydrophilic
The LPS acts as a barrier to ___________ like bile salts & _______ antibiotics.
hydrophoboic compounds (especially important for enteric bacteria)
catoinic
What are the big properties of lipid A
Hydrophobic (saturated fatty acids) → makes LPS rigid
Buried in the outer membrane
Acts of endotoxin
Lipid A is an _______, meaning that it is _________ by bacteria into the extracellular environment, but is released from _________ and can be released as blebs (outer membrane vesicles) from living bacteria.
endotoxin
NOT secreted
dying bacteria
Endotoxin (lipid A) causes _______.
sepsis (septic shock)
How does endotoxin (lipid A) cause septic shock?
binding to macrophage receptor triggers an inflammatory response, which cascades, resulting in a “cytokine storm”
Endotoxin (lipid A) causes what?
systemic vasodilation → drop in blood pressure, cardiac function, random clotting, & multiorgan system failure
*drop in BP causes organ failure*
The toxicity of endotoxin (lipid A) is due to activation of ________ and release of ________ that results in localized high concentration of complement & cytokines.
complement
cytokines
Lipid A causes macrophages to produce _______ which accumulates in the bloodstream.
tumor necrosis factor (TNF-α)
The increase in TNF-α causes a significant drop in ________ due to ________ of blood vessels (septic shock).
blood pressure
leakage
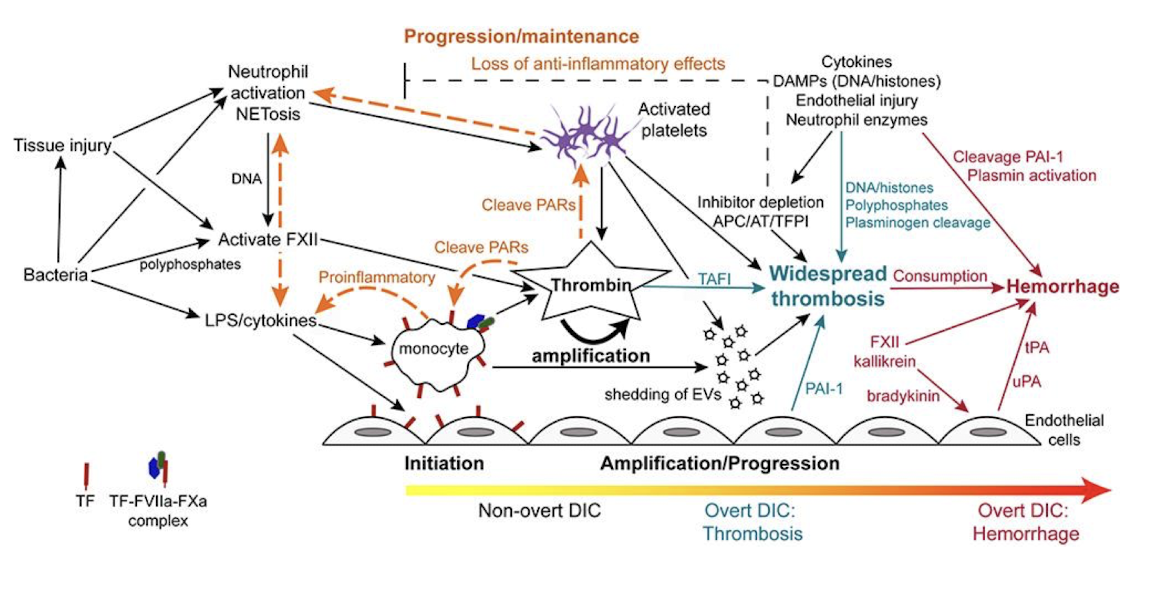
Sepsis-Related Disseminated Intravascular Coagulation (DIC)
Sepsis trigger (infection → PAMPs → immune activation)
Cytokine storm (TNF-α, IL-1, IL-6)
Endothelial activation & tissue factor expression
Activation of coagulation cascade (extrinsic pathway → thrombin → fibrin)
Inhibition of anticoagulants (↓ antithrombin, ↓ protein C, ↓ TFPI)
Suppression of fibrinolysis (↑ PAI-1 = ↓ tPA activity)
Widespread microvascular thrombosis (multi-organ ischemia)
Consumption of clotting factors & platelets
Bleeding phase (petechiae, mucosal bleeding, hemorrhage)
The core region of LPS is comprised of ________
inner & outer core
What is the function of the LPS core?
bridges lipid A to O antigen
T/F: The LPS core is relatively conserved.
TRUE
For enteric bacteria, the inner region of the LPS core is composed of
2-keto-3-deoxy-octonate (KDO), heptose, ethanolamine, & phosphates
For enteric bacteria, the outer region of the LPS core is composed of
hexoses
T/F: Core biosynthesis is well understood.
FALSE - poorly understood
The O-antigen of the LPS is comprised of
repeat oligosaccharide of 4-6 sugar residues
T/F: O-antigen is highly variable between and among bacterial species.
TRUE - one of the most diverse bacterial cell constituents
The O-antigen is instrumental for host ____________ and environmental ___________.
colonization
niche adaptation
O-antigen is highly _________ and targeted by ________ immune system and phage.
immunogenic
adaptive
T/F: O-antigen is used for serotyping.
TRUE
T/F: Bacteria have no adaptations to alter O-antigen structure to evade immune response.
FALSE - bacteria have many adaptations for this
What 3 things aid in specific serotyping using O-antigen?
The huge diversity of O-antigen
Knowledge of the specific type of O-Ag
Flagellar H antigens
What is a serogroup?
broad classification of bacteria based on shared antigenic structures, usually the O-Antigen of LPS in gram negative bacteria
Serogroup analogy
“family name” that groups related bacteria with similar surface sugar patterns
What is a serotype (serovar)?
a more specific classification within a serogroup based on antigenic markers (commonly both O-Ag & H-Ag (flagellar proteins), sometimes K-Ag (capsular polysaccharides))
Serotype analogy
If serogroup is the family name, serotype is the individual’s full name
T/F: Serotypes do not pose much importance.
FALSE - they can be a big deal! → there are 100s of different serotypes among different bacteria
ex: Salmonella enterica has >2600 serotypes
What are mollicutes?
bacteria that lack a cell wall
What are some examples of mollicutes?
Mycoplasma, Spiroplasma, etc.
Mollicutes have the ________ genome of any free-living prokaryotes.
smallest
The absence of a cell wall in mollicutes results in __________ to fluctuation in ___________.
hypersensitivity
salt concentrations
What do mollicutes have in place of a cell wall?
strong cell membrane made of sterols
What are sterols?
hydrophobic ringed structures that are normally found in eukaryotes → rigid
T/F: Mollicutes are not super harmful or hard to deal with.
FALSE - they are a major problem
Why are mollicutes a major problem?
Wide host range
Unique biology make them difficult to culture (slow growing/ non-culturable) & detect
Resistant to all β-lactam antibiotics
Chronic, persistent infections in carrier animals make eradication difficult
Major contributors to respiratory disease complex in poultry, swine, & cattle
Major contributors to abortion & infertility in sheep, goats, and cattle
Several diseases are internationally notifiable (OIE list)
result in culling, preventing animal movement, & impact international trade
The OIE maintains a list of animal diseases, infections, and infestations that member countries are ___________.
obligated to report
The OIE ensures early detection, rapid response, and international transparency for diseases that can:
Cause significant economic losses
Threaten public health (zoonotic bacteria)
Spread rapidly across borders
Affect biodiversity and trade
What species of Mycoplasma are OIE reportable.
M. mycoides
M. capricolum (subsp Capripneumoniae)
M. agalactiae
The cytoplasmic membrane is a ___________ present in ______ bacteria.
phospholipid bilayer
all
The cytoplasmic membrane is said to be a ___________ because of the extensive ___________ of many proteins and phospholipids.
fluid mosaic structure
lateral mobility
Proteins and lipids diffuse _______.
laterally
Certain protein aggregates (complex solute transporters & e- transport aggregates) remain as aggregates where the proteins __________.
interact to catalyze sequential reactions
T/F: The cytoplasmic membrane is the most functionally complex of the cell structures.
TRUE
Multiple antibacterial agents affect the cytoplasmic membrane including:
Detergents
Polymixins
Ionophore compounds
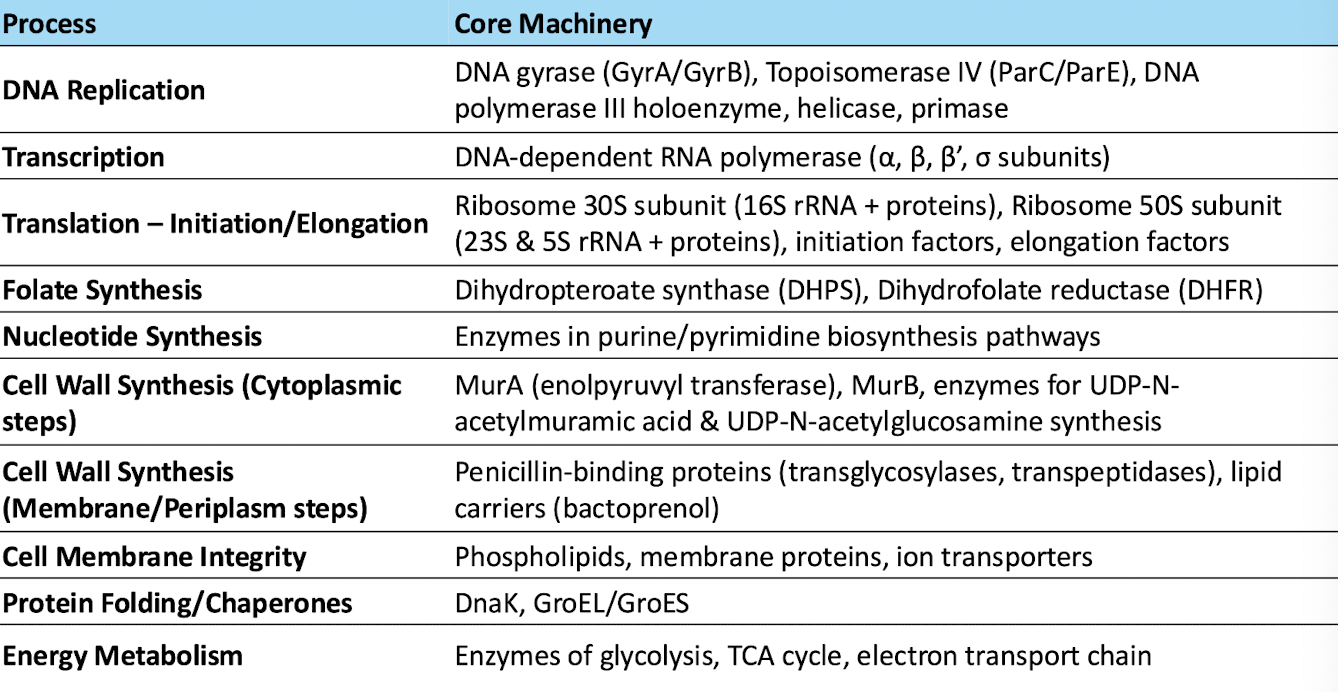
T/F: Only a few processes occur in bacterial cytoplasm.
FALSE - there a lot going on in there
What are endospores?
highly resistant, dormant structures formed inside gram positive bacterial cells when conditions become unfavorable (nutrient depletion, desiccation, extreme temps)
What do endospores contain?
bacterium’s chromosome, a minimal amount of cytoplasm, and multiple protective layers
What purpose do the multiple protective layers of endospores serve?
it makes them extremely resistant to heat, UV light, chemical, and desiccation
What is sporulation?
temporally-regulated cell differentiation
How is sporulation regulated?
complex cascade of gene expression ensures that not all bacteria sporulate at once, & spores only germinate when conditions are optimal
T/F: Many genera of both Gram + and Gram - bacteria produce true endospores.
FALSE - only certain Gram + genera
What are the most notable Gram + species that produce endospores?
Bacillus spp. → aerobic/ facultative anaerobes (B. anthracis)
Clostridium spp. → strict anaerobes (C. botulinum, C. tetani)
How are spores significant virulence factors?
Persistence → can survive decades in soil, bedding, or feed
Disease transmission → many cause serious vet & zoonotic dieases (tetnus, anthrax, botulism)
Disinfection challenges → resistence makes them hard to kill
Epidemiology → persistence = outbreaks recurring years after last known case
T/F: Endospores can be used in biowarfare.
TRUE - exceptional durability, ease of dissemination, high lethality in certain pathogens, delayed detection, difficult to decontaminate
Which spore spp is one of the most cited examples in bioterrorism history?
Anthrax spores → stable, deadly, & hard to neutralize once released