Therapeutics II Exam 4 - Medical Management of Type 1 Diabetes
1/55
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
56 Terms
Which insulins have the lowest risk of causing hypoglycemia?
Ultra long acting insulin
-U300 glargine
-insulin degludec
Which insulins have the highest risk of causing hypoglycemia?
Ultra rapid insulin
-aspart (Fiasp)
-human insulin inhalation
Rapid insulin
-lispro
-aspart
-glulisine
Basal insulin options
-detemir (Levemir)
-glargine U100 (Basaglar, Lantus)
-glargine U300 (Toujeo)
-degludec U100 or degludec U200 (Tresiba)
-NPH (not frequently used as other options)
Basal insulin - NPH
-least desirable in terms of matching human physiology due to distinct peak and duration much less than 24 hours
-usually dosed BID
-not used as much anyone due to availability of other options
Basal insulin - detemir
-has a peak
-often lasts less than 24 hours
-not ideal, but better than NPH
Basal insulin - glargine U100
-peakless
-usually can be given once daily
Basal insulin - glargine U300
-peakless
-longest duration of action of glargine options
-can give once daily
-less glucose variability , lowest risk of hypoglycemia
-more costly
Basal insulin - degludec
-peakless
-longest duration of action
-can give once daily
-less glucose variability , lowest risk of hypoglycemia
-more costly
Bolus insulin options
Rapid acting insulin
-aspart
-lispro
-glulisine
Ultra rapid insulin
-Afrezza
-Fiasp
Short acting regular insulin (not commonly used)
U500 Insulin
-reserved for use in patients with extreme insulin resistance and significant daily insulin needs (more than 200 units daily)
-given 2 to 3 times daily
-to avoid errors, use pens instead of vials
-if using a vial, use U500 syringes
True/false - U500 insulin can be used in an insulin pump
false
Insulin dose adjustment in renal impairment
-15% to 20% of insulin metabolism is renal
-ESRD have lower dosage requirements
-longer duration of action of insulin
-always adjust insulin based on blood glucose readings
Insulin adverse effects
[] hypoglycemia
[] weight gain
[] injection site reactions
[] lipohypertrophy or lipoatrophy
Insulin adverse effects - hypoglycemia
more common in type 1 diabetes due to sensitivity to insulin and more intensive therapy
Insulin adverse effects - weight gain
-dose dependent
-mostly truncal fat
Insulin adverse effects - injection site reactions
-pain
-itching
-redness
-edema
-inflammation
Insulin adverse effects - lipohypertrophy or lipoatrophy
-from long term use
-counsel patients to rotate injection site
-if lipodystrophy occurs, avoid that injection site
Inhaled insulin
-can still cause hypoglycemia and weight gain
-also can cause cough and URI
-associated with small decline in pulmonary function
Inhaled insulin - contraindications
-COPD
-asthma
(due to bronchospasm risk)
Inhaled insulin - management of decline in pulmonary function
-have spirometry test at baseline, 6 months, and annually thereafter
-if ≥ 20% reduction of FEV1 is observed, inhaled insulin should be discontinued
Principles for insulin dosing
-regimen should mimic the body's normal insulin secretion as closely as possible
-should include basal insulin replacement, bolus/prandial or mealtime dosing, correction/supplemental dosing
-there is no one perfect insulin regimen for either type 1 or type 2 diabetes
-a patient's response to insulin cannot be predicted
-basal requirements may vary at different points in the day
Typical starting dose of insulin in T1DM
0.3 to 0.7 units/kg/day (calculation for total daily insulin amount)
Insulin regimens
1. Basal bolus insulin regimen
2. Split/Mix regimen
3. 70/30 or 75/25 regimen
Basal bolus insulin regimen
-one time daily basal dose at same time each day (does not matter what time)
-bolus doses throughout the day
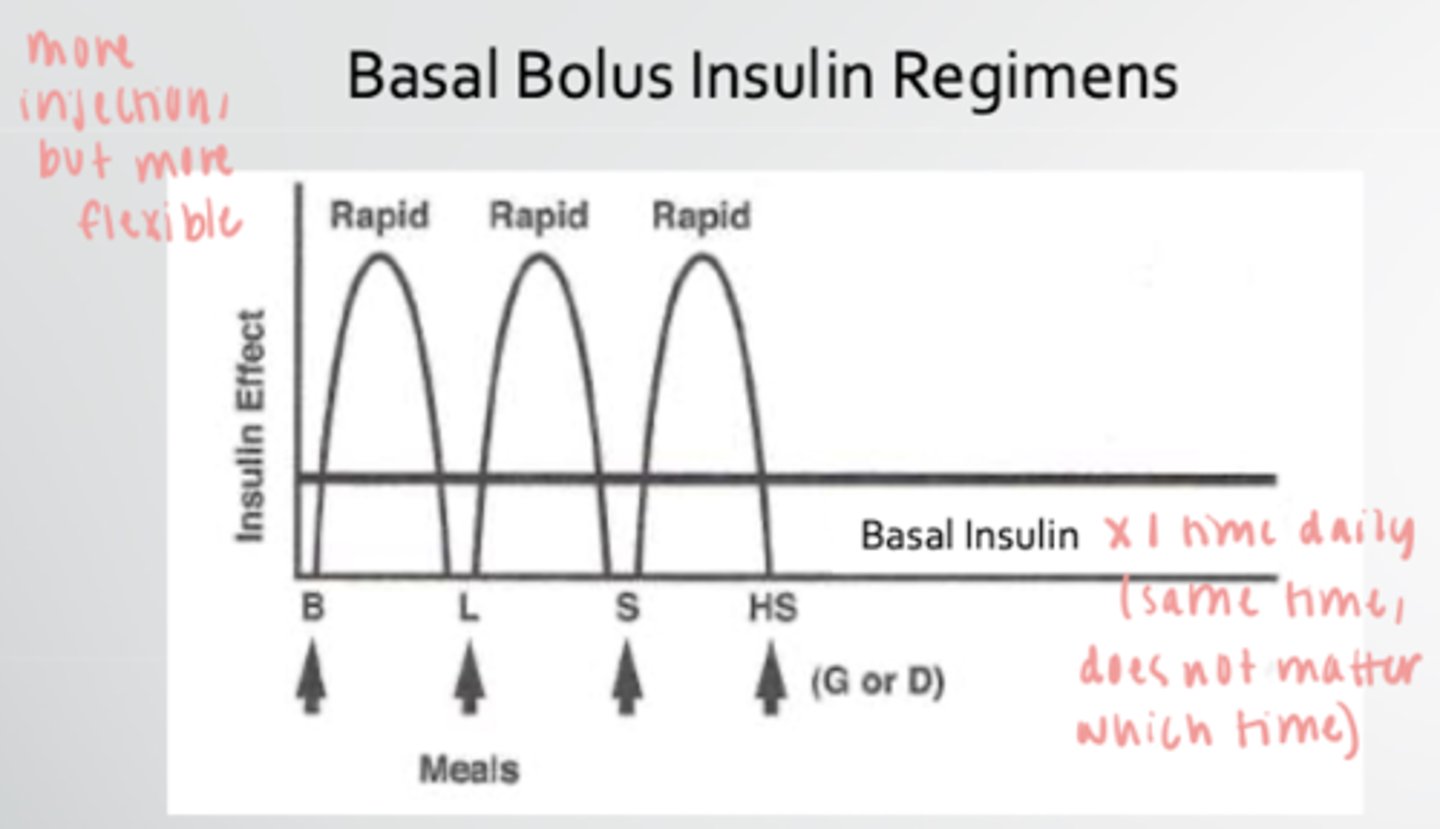
Advantages and disadvantages of basal bolus insulin regimen
advantage - flexibility
disadvantage - more injections
Calculation for basal bolus insulin regimen
1. Calculate total daily units with 0.5 units/kg/day
2. Divide the total dose in half
3. 1/2 of total daily dose is basal insulin dose
4. Divide other half by 3 to calculate rapid acting meal coverage
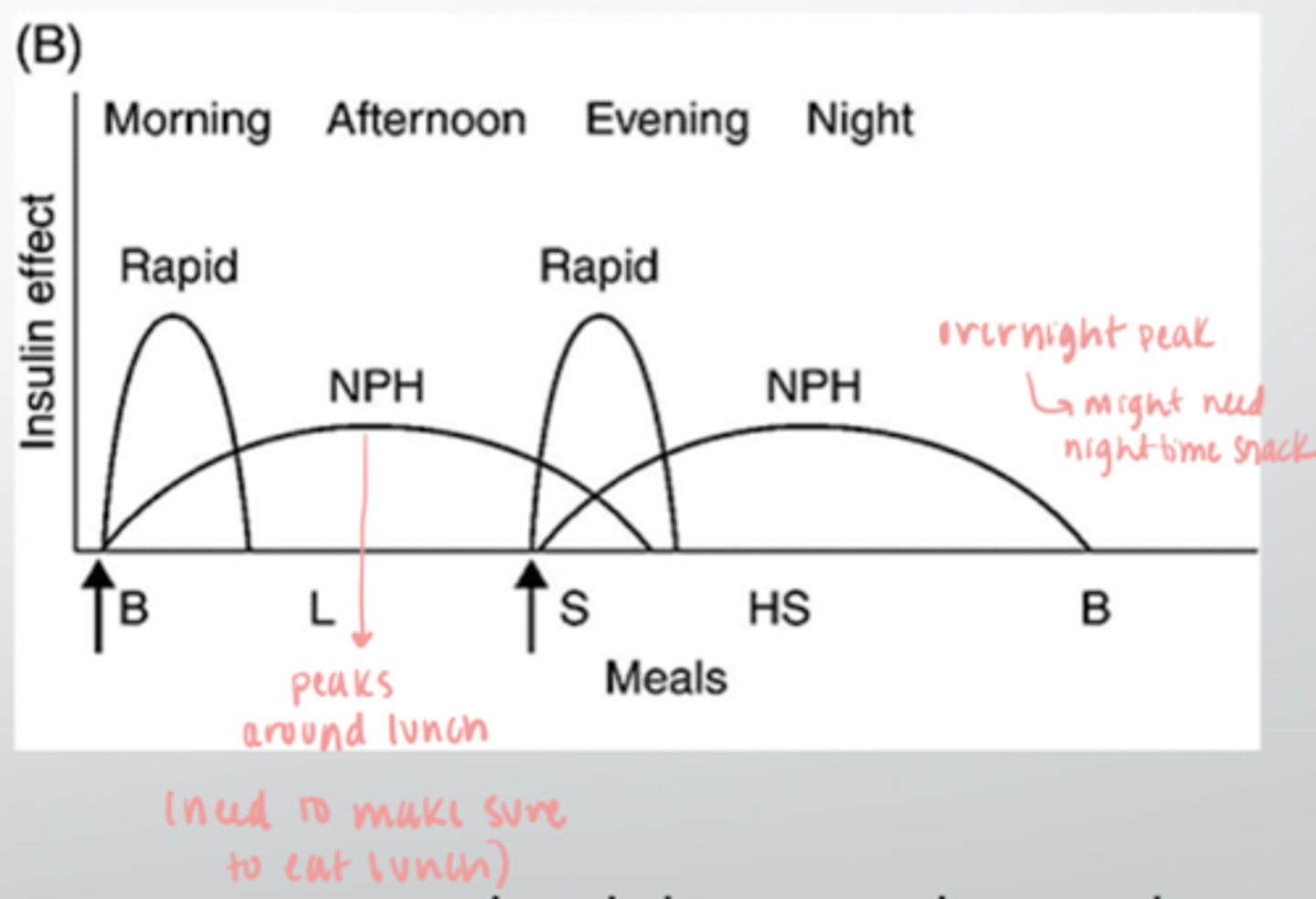
Split/Mix regimen
-2 injections daily (breakfast and dinner)
-peaks around lunch and overnight
-may need to eat nighttime snack due to overnight peak
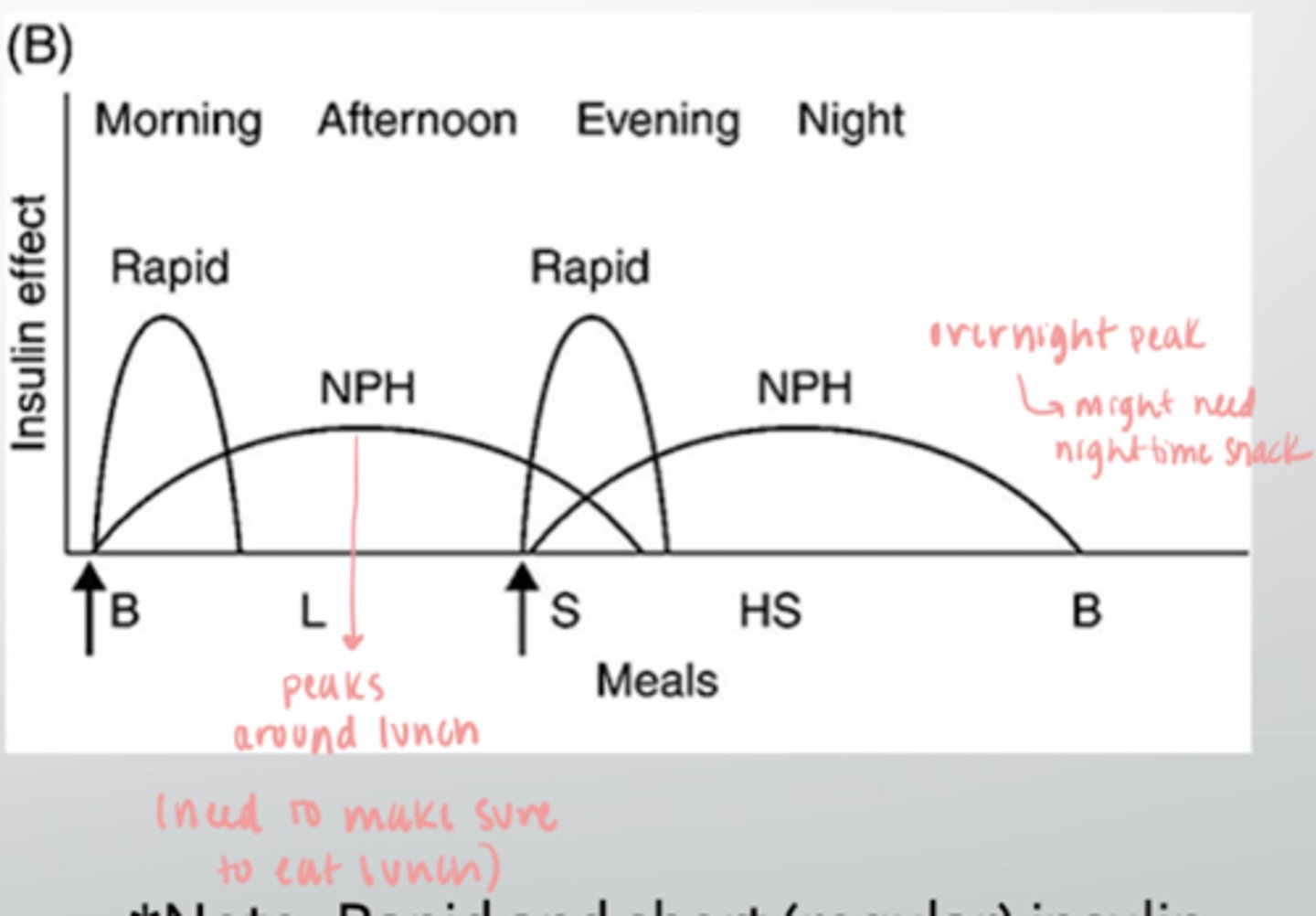
Calculation for split mix regimen
1. Calculate total daily units with 0.5 units/kg/day
2. 2/3 of total daily dose divided by 2 is long acting NPH dose (2 doses per day)
3. 1/3 of total daily dose divided by 2 is the rapid insulin dose (2 doses per day)
(NPH and rapid insulin are separate pens/vials)
Advantages and disadvantages of split mix regimen
advantage - only 2 doses per day
disadvantage - must time meals to align with insulin peaks
70/30 or 75/25 regimen
-2 injections daily (breakfast and dinner)
-peaks around lunch and overnight
-may need to eat nighttime snack due to overnight peak
Calculation for 70/30 and 75/25 regimen
1. Calculate total daily units with 0.5 units/kg/day
2. Divide total daily dose by 2 for individual dose amount (2 doses per day)
If the pre-breakfast (fasting) glucose is out of range, what meal would affect this?
dinner/bedtime
If the pre-breakfast (fasting) glucose is out of range, what insulin dose would affect this?
evening basal insulin dose or
evening NPH dose
If the pre-lunch glucose is out of range, what meal would affect this?
breakfast
If the pre-lunch glucose is out of range, what insulin dose would affect this?
breakfast dose
If the pre-dinner glucose is out of range, what meal would affect this?
lunch
If the pre-dinner glucose is out of range, what insulin dose would affect this?
lunch dose or
morning NPH dose
If the bedtime glucose is out of range, what meal would affect this?
dinner
If the bedtime glucose is out of range, what insulin dose would affect this?
dinner dose
Dawn phenomenon
-normal rise in blood sugar as the body wakes up
-caused by increase in cortisol, growth hormone, and catecholamines
Somogyi effect
-blood sugar drops too low in the early morning hours
-cortisol, growth hormone, and catecholamines are released to correct it
-leads to a rebound high morning blood glucose
If the patient's blood sugar is normal or high at 2 am to 3 am, and then high when waking up, this is the ___________ phenomenon
dawn
If the patient's blood sugar is low at 2 am to 3 am, and then high when waking up, this is the ___________ phenomenon
Somogyi
Sick day management
-continue basal insulin at normal dose
-hydrate with water or electrolyte solution at a rate of 8 to 12 oz per hour
-adjust bolus dosing if not eating
-check urine ketones every 4 hours when BG is over 250 mg/ml
-call physician if vomiting and BG > 500
-call physician if moderate to large ketones and BG > 250 mg/dl
Sick day management - not eating
-stop bolus/mealtime insulin
-cover hyperglycemia with fast acting insulin every 4 to 6 hours using correction factor
-keep blood glucose under 250 mg/dl
What is considered when refining insulin doses?
[] insulin to carbohydrate ratio
[] correction insulin
Insulin to carbohydrate ratio
-amount of rapid acting insulin to cover carbohydrates in meals and snacks
-patients may have different insulin to carbohydrate ratios for different meals
-for rapid acting insulin: rule of 500
Rule of 500
-divide 500 by the patient's total daily insulin dose
-method of calculating starting point of insulin to carbohydrate ratio
-most accurate in type 1 diabetes
-limitations in type 2 diabetes due to insulin resistance, slowing of gastric emptying from GLP1 agonists, gastroparesis
If you perform a rule of 500 calculation and get an answer of 20, what does this mean?
ratio is 1:20
1 unit of insulin should be injected for every 20 grams of carbohydrates
If the insulin to carb ratio is correct, post prandial glucose measurements should be within target range ________ hours after a meal
2
Adjustments after initial rule 500 calculation
Frequent lows
-too much insulin
-decrease the insulin to carb ratio
Post prandial levels too high
-not enough insulin
-increase the insulin to carb ratio
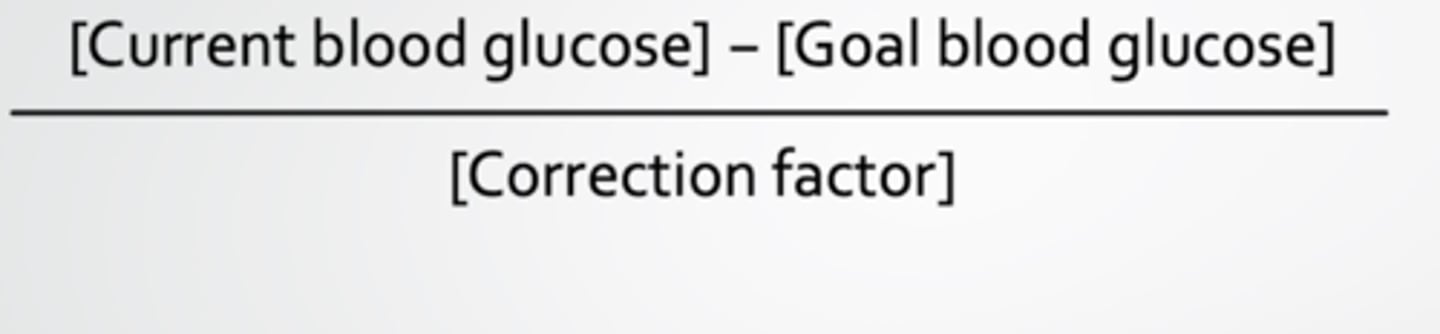
Correction factor
-insulin sensitivity factor
-amount of rapid acting insulin needed to return an elevated blood glucose to target level
-quantifies the degree of change in blood glucose expected with injection of 1 unit of insulin
1800 rule
-divide 1800 by total daily dose of insulin
-quick method of calculating correction factor in T1DM
If a Rule 1800 calculation and get an answer of 50, what does this mean?
1 unit of insulin should lower blood glucose by approximately 50 mg/dL
Correction dose
calculates how much insulin should be injected to correct blood glucose back to goal
Five questions patients should answer before meals
1. What is my target blood glucose range?
2. What is my current (pre meal) reading?
3. How many carbohydrates am I planning to eat?
4. What is my insulin to carbohydrate ratio?
5. What is my correction factor?
Also consider:
-level of activity (exercising, etc.)
-any changes in lifestyle or routine (sickness, medications, etc.)