exam 3
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
42 Terms
What is the most problematic effect of opiods
respiritory depression and sedation,
others: orthostatic hypotension nasuea vomitting, urinary retention constipation
what is the priority with opioid use related to abc and should be monitored?
respiritory depression affecting pts breathing, hypoxia
pulse oximetry
difference between objective and subjective findings related to opiod use
objective: nurse observed: respiratory rate, sedation, consciousness, pulse
subjective: pt reports: dizziness nausea, vomitting constipation
How should a pt store narcotics?
Opioids, in particular, must be locked away and should be stored in their original packaging.
What are non-verbal pain cues?
objective data: what we observe because pt cannot speak
Non verbal pain scale (NVPC): rates pain on a scale of 1-5 of different levels
facial expressions: clenching jaw, eye movemnets
pt physical actvitity:bodylanguage touching painful body part, rubbing, clucthing body part
guarding(voluntary contraction or stiffness of the body when in pain)
Vitals signs
Respiritory rate
sounds: crying moaning
territoroality, personal space: can make pt percieve a threat
Subjective findings for pain
pain scale score, along with quantity and quality of pain
Objective findings for pain
grimacing, guarding, crying
What is chronic pain?
Lasting 6+months and recurs, not protective
Physilogical: do not alter vitals
psychsocial: leads to disability
relief: long acting/controlled release opioids analegesics
what is acute pain
temporary pain, direct, protective, pain resolves w/tissue healing
physiological: tachycardia. hypertension, anxiety, diaphoresis(sweating) , muscle tension
behavior responses: grimacing, moaning, guarding, flenching
relief: treatment of acute pain problem
what is nociceptive pain
pain arising from damage or inflammation of tissue
characteristics: throbbing, aching, localized
relief: responds to opioids and non opioids
types:
-somatic: bones joints muscle skinn connective tissue
-visceral: organs stomach intestine
-cutaneous: skin or subq tissue
what is neuropathic pain
abdominal or damaged pain in nerves
ex: phantom limb pain(in amputee) pain below level of spinal cord injury and diabetic neuropathy
characteristics: intense shooting burning pain (pins and needles)
relief: adjuvnat meds, antidepressants, antispasmodic agents, skeletal muscle relaxants
what does PQRST stand for and what are you assessing with each letter?
Precipitating cause: What were you doing when the pain started?
Quality:Describe what your pain feels like.”
Region:Show me the location where you are experiencing pain.”
Serverity: On a scale of 1 to 10, how would you rate your pain?
Timing: “When did your pain first begin? Have you experienced this pain before?”
what are symtoms of fight or flight related to stress
elevated: BP, HR, mental alertness, increased secretion of epinephrine and norepinephrine, increased blood flow to muscles
what are teachings for stress
regular excercise
healthy diet
time management
personal resilance
rest relaxation methods:yoga
alternatives: journaling massage meditation
how can stress affect the body
impairs and weakens the immue system
hypertension
depression
autoimmune disorders
what can happen to a pt in a stressful state for long periods of time?
exhaustion stage: client cannot adapt to stress resulting in recovery or death
prolonged exposure to stress may result in illness or disease
physiological type of stress vs psychological stress
physiological: Physiological stressors are generally associated with injury or illness, such as exposure to extreme temperatures, trauma, injury, illness, or pain. The body’s reaction to acute physiological stress is immediate and necessary for survival. Chronic physiological stress can result in debilitating conditions.
psychological: psychological stressor is an event, situation, comment, condition, or interaction that an individual interprets as negative or threatening. Common psychological stressors include work or academic pressures, financial difficulties, change in marital status, or being a victim of a natural catastrophe.
four interventions the nurse can take to assist the client in coping with stress
be empathetic
identify strengths and aibilities
encoruage pt to use previous coping methods
identify availabe resources
examples of chronic stress and acute stress
chronic:often stems from serious life problems such as poverty, racism, illness, disease, or living in a dysfunctional family system.
Acute:being involved in a motor vehicle accident, experiencing the loss of a loved one, or being a victim of a crime.
what is “GAS:
general adaptive syndrome
body's attempt to maintain equilibrium and homeostasis. Consists of three stages: alarm, resistance, and exhaustion.
alarm: fight or flight epinephrine, norepinephrine, cortisone are released, elevated BP, HR, RR ,menatl alertness
resistance: body functions normalize while responding to stressor stabalizing vitals
exhaustion: body functions no longer able to maintain response to the stressor leading to recovery or death
first stage of sleep
NREM : light sleep, 1-5 mins long, 5% of sleep cycle muscle relaxation, loss of awareness, vitals begin to decrease, awaken easily, drowsy relaxed
second stage of sleep
NREM 2: deeper sleep,
2-25 min long,
vitals & metablolisim continue to slow,
more stimulation to waken,
reduced sympathetic activity 50% of sleep cycle
third stage of sleep cycle
NREM 3: slow wave sleep, or delta sleep
High amplitude electrical brainwaves in the frequency range of 1.0 to 4 hertz.
30-60 mins of mental cloudiness
more difficult to wake
psychological rest and restoration
reduced symphathetic activity
stage 4 of sleep cycle
REM: vivid dreaming
beta waves
90 min after falling alseep reucrring every 90 min
longer with sleep cycle
20 min long
varrying vital signs
difficult to awaken
loss of skeletal tone
cognitive restoration
what is a nurse teachinngs to a pt for promoting sleep routine
Avoid stimulants, such as caffeine, alcohol, and nicotine, at least 4 to 6 hours before bedtime.
Remove any unnecessary light and noise; substitute calming white noise if necessary.
Establish a bedtime routine, such as taking a warm shower or bath before bedtime.
Keep the room dark, quiet, and at a comfortable, cold temperature.
Only go to bed when tired. If the client feels restless while attempting to sleep, they should go to another room and do a simple activity like reading or listening to preferred music.
Keep a consistent sleep–wake cycle by going to bed and waking at the same time, which allows the body to fall into a biologic rhythm.
Keep naps short, less than 30 minutes.
Engage in a regular exercise routine, along with healthy eating; complete exercising at least 3 hours before going to bed.
Remove all work items and televisions from the bedroom when possible. The bedroom should be associated with sleep and sexual activity only.
When would you not want to massage a pt?
Contraindications to massage include clients with burns, wounds, and on medications to thin their blood (warfarin).
what is theapuetic communication for a terminal ill pt
intiate an open conversation
When giving information about medical conditions how should you give that info to pt’s?
clear, free from slang, medical terminology
what would a client look like with anxiety attack
A client with mild anxiety may exhibit minimal or no physiological manifestations of anxiety, whereas a client with moderate anxiety may appear animated and have slightly elevated vital signs. Clients with severe anxiety will likely exhibit elevated vital signs, diaphoresis, heart palpitations, and muscle tension.
how should you communicate with pts with hearing loss
visual aids
sit and face the client
avoid covering mouth while talking
speak slow and clearly
do not shout
use simple sentences
sign language interpeter if necessary
minimize background noises
what to do if langauge barrier
get medical interpeter
what would you include with therapuetic communication teaching?
open ended questions
give feedback
express empathy
active listening
clarifying the message
giving factual info
when discharing a pt with hearing loss what would you inform them of for health promotion?
do not place objects in ear
have otologist remove any logged items in ear
wear ear protection to high intense noises
blow nose with both nostrils obsutrcted
keeo volume low with headphones
barriers to therapuetic communications
Language differences,
cultural diversities,
speech or hearing impairments,
developmental or cognitive disorders,
medication effects,
effects of recreational drugs,
emotional distress,
environmental factors can all be communication barriers
if pt is a fall risk, how would you assess your pt
When caring for a client who has a mild to moderate vision impairment, the nurse should confirm the client has access to all required corrective lenses, such as prescription eyeglasses or contacts, and reading glasses. Be sure these are in working order and that the client wears them when needed. The nurse should ensure there is adequate lighting in the client’s environment and provide large-print reading materials if necessary. Some clients benefit from the use of a magnifying glass when reading. Face the client when speaking while making eye contact.
For a hospitalized client who has a moderate to severe impairment, or is blind, the nurse should announce their presence and ask permission to enter the client’s room. Instruct the client on the location of items in the room, including the call light. Encourage the client to request assistance with getting out of bed and ambulating. A client may use assistive devices, such as a cane or walking stick, a walker, or a service animal when ambulating. Keep the environment free from clutter to decrease the risk of falls.
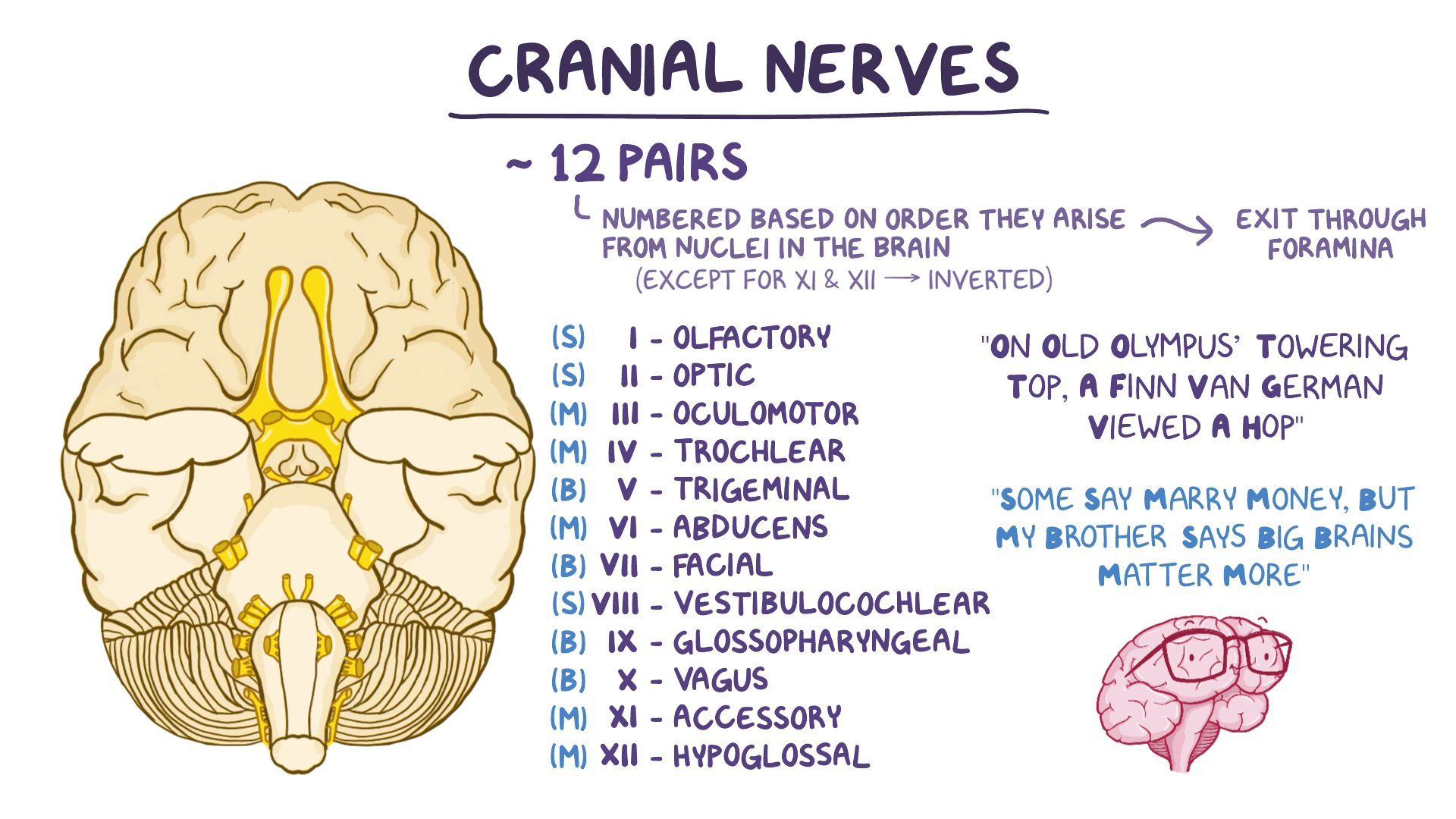
what are the 12 cranial nerves, and how would you assess them
“on old olympus towering top a fin van german viewed a mom”
Olfactory I
Sensory to nose for smell
Ask client to identify specific smells, such as coffee or peppermint, testing each nostril separately.
Optic
II Sensory to eye for vision
Test visual acuity using Snellen chart or by having client read printed material.
OculomotorIII
Motor to eye
Check extraocular movements by assessing the 6 directions of gaze.
Check pupillary reaction to light and accommodation.
TrochlearIV
Motor to eye
Assess the 6 directions of gaze.
Trigeminal
V
Sensory to face
Motor to muscles of jaw
Assess corneal reflex.
Palpate the masseter muscles at the temple while client clenches jaw.
Check sensation by lightly touching over the face with a cotton ball.
AbducensVI
Motor to eye
Assess the 6 directions of gaze.
FacialVII
Sensory to tongue for taste
Motor to face for expression
Monitor for symmetry of the face when the client smiles and raises/lowers eyebrows.
Check perception of sweet and salty tastes on the front of the tongue.
Vestibulocochlear (Auditory)VIII
Sensory to ear for hearing and balance
Whisper a word 2 to 3 cm away from one ear while client occludes the other ear. Check both ears.
Observe the client’s balance as they walk.
Glossopharyngeal IX
Sensory to tongue for taste
Motor to pharynx (throat)
Check perception of sweet and sour tastes on the back of the tongue.
Use a tongue blade to check the gag reflex.
Assess the ability to swallow.
Vagus X
Sensory to pharynx
Motor to vocal cords
Parasympathetic innervation to heart lungs, abdominal organs
Have client say “ah” and observe palate and pharynx for movement.
Listen for hoarseness of voice.
Assess pulse, bowel sounds.
Accessory XI
Motor to muscles of neck
Observe ability to turn head side to side.
Monitor client’s ability to shrug shoulders against resistance from examiner’s hands.
HypoglossalXII
Motor to tongue
Ask client to stick tongue out, observe if midline;
Assess ability to move tongue side to side.
how would comminicate w/ pt with impaired speech
allow time for pt to respond
check for comprehension
one person speaks at a time
speak clearly and slowly
tell pt when you do not understand them
picture charts
gestures body language
teaching for diabetic patients related to their feet
such as clients who have diabetic neuropathy. These clients should inspect their feet each day for cuts, blisters, areas of erythema or warmth, and report these to their provider. The client must be cautious when ambulating to avoid injuring the feet or toes.
The nurse should instruct the client to wear closed-toe shoes and avoid walking barefoot. A client who has diabetic neuropathy should follow dietary instructions and take all medications in order to manage blood glucose levels. Doing so can slow the progression of the neuropathy.
how to administer rinnes and webb hearing test
rinnes: A hearing test that is performed with a tuning fork that is vibrated and placed against the mastoid bone and the client is asked to identify when they are unable to hear the sound. The tuning fork is then moved 1 to 2 cm away from the ear and the client indicates if they can still hear the sound.
weber test: turning fork on the middle of head
audiometer: A hearing test whereby a client wears earphones and various sounds at different decibel levels are played in each ear. The client identifies when they can hear each sound
What are the benefits of excersise and what you would emphasize in teaching
excersise everyday 30min to promote sleep but 3 hours before bed
What are the stress disorders
stress-related disorders Stress-related disorders include
acute stress disorder (ASD): An intense and dysfunctional reaction to a traumatic event that lasts less than a month
posttraumatic stress disorder (PTSD):A prolonged and heightened stress reaction to a traumatic event that lasts more than a month.
irritable bowel syndrome (IBS):A gastrointestinal condition characterized by abdominal pain and changes to bowel elimination patterns that can include diarrhea and/or constipation.
what are strategies to enhance communication between nurse and pts
The nurse should ensure that the information is understood by using communication enhancers such as reflecting or summarizing.