7 Bacteremia/Infective Endocarditis
1/89
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
90 Terms
How are blood cultures packaged and why?
One set of 2 bottles:
-1 bottle anaerobic
-1 bottle aerobic
2 sets should be obtained (2 different sites) to make sure we actually have an infection and not that a culture was contaminated
which pathogens are frequent GI culture contaminants (ie/ often if they show up in culture they aren't the source of infection but rather just contaminating the culture)?
-CoNS (staph epidermidis)
-corynebacterium
-bacillus spp (other than anthracis)
-micrococcus spp
-cutibacterium acnes
which pathogens can be contaminants OR true pathogens in GI cultures?
-enterococci
-viridians strep
-clostridium spp
which pathogens are rarely contaminants and are true pathogens?
-staph aureus
-strep pneumo
-beta-hemolytic strep (GAS)
-listeria
-enterobacterales
-pseudomonas aeuriginosa
-neisseria meningitidis
-H. flu
-anaerobic GNRs
-candida
Don't overthink it. These are those that we have seen commonly implicated in infections so far in this course
why is bacteremia a concerning condition
-7% in the ICU have it
-High mortality (40-60%; 3X the risk of hospital death)
-↑ stay
-↑ cost
how are empiric and definitive therapy determined for bacteremia / candidemia?
empiric:
-gram stain and local antibiogram
definitive:
-pt. factors (allergies, renal, etc) and isolated organism
duration of treatment for each of the common pathogens in bacteremia/candida (at least those that were mentioned in this lecture for duration of treatment)
Duration of treatment begins once we have a negative blood culture
-Staph aureus = 14d
-GNR = 10-14d
-Candida = 14d
how often do we want to obtain blood cultures for a patient with bacteremia?
q 24-48 hours until negative
what is endocarditis, and what parts of the heart are most commonly affected?
-infection of endocardium
most common locations in order from most to least:
-mitral valve
-aortic valve
-tricuspid and pulmonic
-can also occur in septal defect or mural endocardium
most common cause of infective endocarditis
bacteria, but can also be caused by fungi or virus
most common predisposing factor for endocarditis in developed and developing countries
developed:
-mitral valve prolapse
developing:
-rheumatic heart disease
what patient populations are most likely to develop infective endocarditis?
-those w/ predisposing cardiac abnormality or risk factor (MOST common)
-elderly (> 50% cases in USA are > 60 yo)
-IV drug users
pathophysiology of infective endocarditis
1) turbulent flow damages vessel
2) sterile vegetation formation in damaged vessel (fibrin, platelets)
3) sterile vegetation is infected via trauma to skin, mucosal surfaces, or d/t peridontal disease
which IV drug is particularly associated w/ increased risk of endocarditis?
cocaine (repetitive bombardment of particulate matter and ischemia d/t vasospasm from drug)
which pathogen can directly invade the endocardium?
staph aureus
risk factors for endocarditis (including the previous ones)
-cardiac abnormality
-hx endocarditis
-intracardiac device
-elderly
-IVDU
-Male (2:1)
-dialysis
-diabetes
-HIV
-prosthetic valve
-cyanotic congenital heart disease
-chronic rheumatic heart disease
-age related degenerative valvular lesion
Essentially old men, cardiac problems or devices, drugs, dialysis, diabetes, and HIV
Is endocarditis easy or difficult to diagnose?
difficult
Explain how delayed therapy for endocarditis affects outcomes
-poorer outcomes
-increased mortality
-embolic events
complications of endocarditis
-mortality
-embolization (20-50%, highest in first 2 weeks of abx therapy)
-CHF
-valvular abscesses and pericarditis
-heart block / arrhythmias
why can infective endocarditis cause CHF?
-distortion or perforation of valvular leaflets
-rupture of chordae tendineae or papillary muscles
-perforation of cardiac chambers
what does evaluation of patient presentation in the setting of endocarditis always need to include?
-valve status
-comorbidities (including renal function)
presentation of endocarditis
-Non specific s/sx (fever, chills, N/V, fatigue) 2 wks after infection
-heart murmur (85% of cases)
-skin manifestations (Osler's nodules, splinter hemorrhages, petechiae, janeway lesions)
why is heart murmur detection important?
-85% of cases, but may be difficult to detect in ED
-< 50% of cases have murmurs detected on admission
why is fever an important sign in infective endocarditis?
-90% of cases present febrile; 98% in IVDU
-may be absent in elderly, recent abx use, HF, immunosuppression, renal failure
when is infective endocarditis treated outpatient
it isn't. Suspicion requires hospitalization
Who should infective endocarditis be considered in
-unexplained fever and known risk factors
-febrile IVDU or prosthetic valve
-murmur w/ evidence of vasculitis or embolism
How is infective endocarditis diagnosed
Blood cultures and echocardiography
How should blood cultures be obtained for IE?
3 sets from different sites
-1 hour between first and last set
-q24-48h until negative
which organisms are most commonly implicated in IE, and which one is the most commonly reported?
-staph aurues (most common)
-streptococcus spp
-enterococcus spp
why might someone have culture-negative endocarditis?
Fastidious Gram Negative Bacilli (HACEK organisms):
-Haemophilus
-Aggregatibacter
-Cardiobacterium hominis
-Eikenella corrodens
-Kingella kingae
what would we use to treat culture-negative infective endocarditis?
Ceftriaxone for any of the HACEK organisms
nuances of IE treatment
-native vs prosthetic valve
-inoculum effect
-duration
-treatment (drug penetration, static vs cidal drugs)
what is the inoculum effect?
Bacterial counts are too high and less reproduction is occurring, so cell wall active agents are less effective (i.e. beta-lactams and glycopeptides) and MIC increases
which type of endocarditis may have less dense vegetations
right sided
what type of drug might we choose in IE and why?
bactericidal drugs may sterilize vegetations w/ high bacterial densities and are preferred over static if possible
overall goals of IE treatment?
Patient specific goals of IE treatment?
Overall:
-eradicate causative organism
-reduce morbidity and mortality (Cardiac and embolic)
Patient treatment goals:
-resolve s/sx
-reduce/avoid toxicities and AEs
-reduce readmission
-increase compliance / tx success
how often is surgery needed for infective endocarditis?
50%
what type of cultures are taken for infective endocarditis and how often are they taken?
blood cultures q 24-48 hours until clear, then not needed unless clinical status worsens
what may indicate subtherapeutic drug levels in infective endocarditis?
-persistently positive blood cultures (ie/ bacteremia)
-fever
-elevated white count
When does treatment in infective endocarditis officially begin?
How long do we treat for?
after the 1st negative blood culture
KNOW. THIS.
eg/ if we take a culture on Sept 1st and we get the results that they are negative on Sept 5th, we treat for 2 weeks from THE DAY THE CULTURE WAS TAKEN, including that day (ie/ treat until Sept. 14th)
BUT remember, native valve and susceptible pathogens is 2 wks; prosthetic and resistant is ≥ 6 wks
If appropriate source control and antimicrobial treatment is conducted, when should symptoms resolve in patients with infective endocarditis?
Within the first week of treatment
-WITHIN THE FIRST WEEK AFTER THE FIRST NEGATIVE BLOOD CULTURE
why do we do repeat blood cultures in infective endocarditis?
We need to know when the clock starts for treatment so we can evaluate efficacy of treatment
-once there is no evidence of bacteremia (ie/ negative blood cultures) treatment officially begins and we expect symptom resolution within 1 week
explain how empiric therapy is used in infective endocarditis
-not recommended per guidelines unless patient condition worsens (ie/ patient is crashing or we expect sepsis or septic shock)
-if empiric therapy is warranted, target the most likely organism
per sanford guide, what empiric therapy options exist for infective endocarditis?
native valve:
-vanco + either gentamicin or ceftriaxone
prosthetic valve:
-vanco + gent + rifampin
REMEMBER empiric therapy is not recommended though
why is vanco included in empiric therapy for IE?
coverage of:
-MRSA
-ampicillin resistant enterococcus
-streptococcus
these are the most common organisms implicated in IE
what is recommended for MSSA definitive therapy in IE?
beta lactam
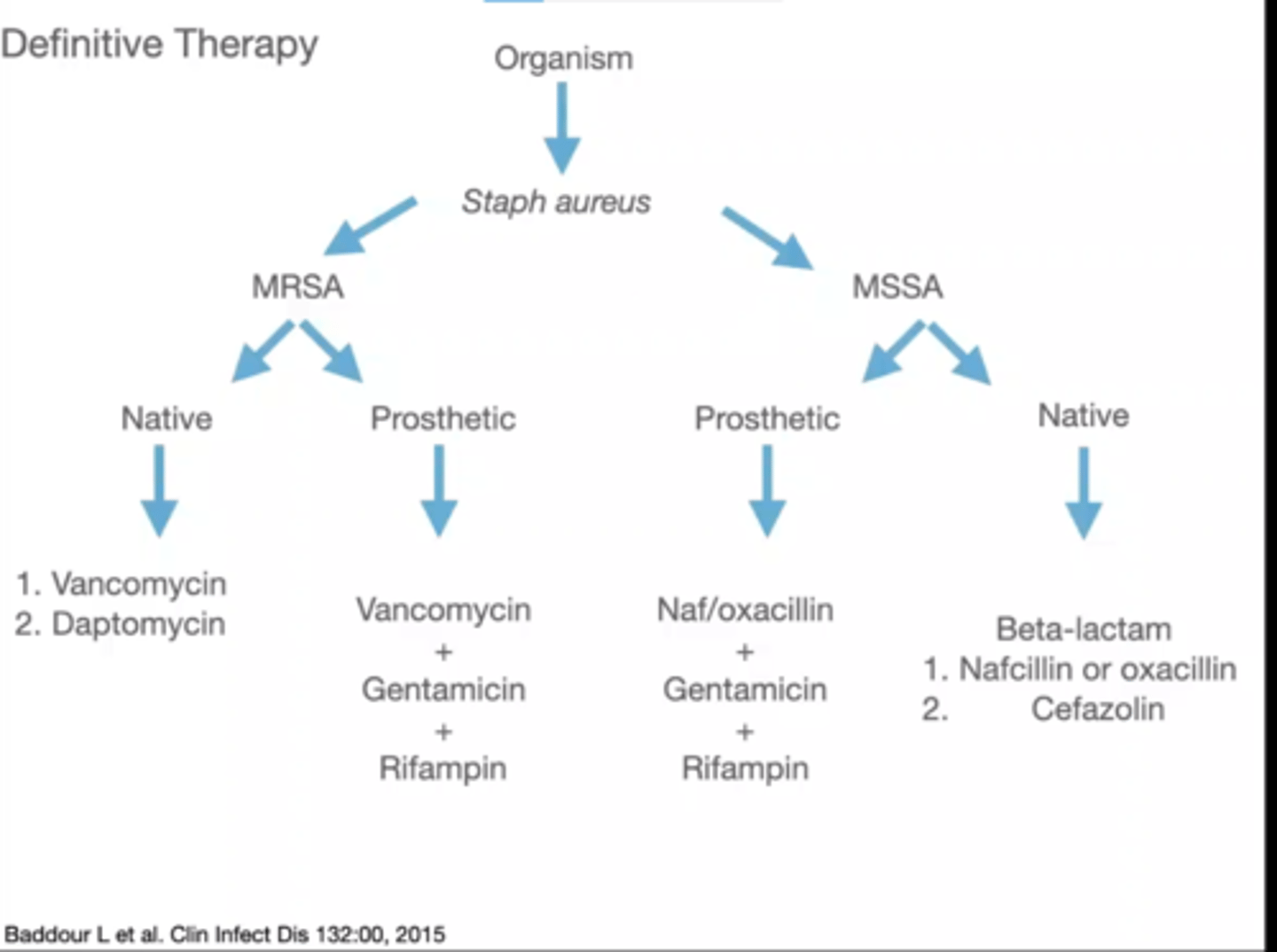
explain the flow chart for definitive therapy in endocarditis if the organism isolated is staph aureus
MRSA:
-native valve = vanco or dapto
-prosthetic valve = vanco + gent + rifampin (same as empiric therapy for prosthetic valve)
MSSA:
-native valve = BL (nafcillin, oxacillin, or cefazolin)
-prosthetic valve = Naf-/oxacillin + gent + rifampin
explain staph aureus definitive therapy for IE in simple terms
-MRSA native = vanco or dapto
-MRSA prosthetic = vanco + gent + rifampin
-MSSA native = BL (naf-, oxacillin, or cefazolin)
-MSSA prosthetic = add gent and rifampin
Easy. Vanco covers MRSA, add gent and rifampin for prosthetic.
Anti-staph PCNs cover MSSA. Add gent and rifampin for prosthetic
photo of definitive therapy for IE if staph aureus is isolated
which strep species are involved in the definitive therapy flow chart for infective endocarditis?
-viridians
-gallolyticus
definitive therapy for infective endocarditis if streptococcus is isolated
-if strep viridians or gallolyticus, and if highly PCN susceptible (MIC ≤ 0.12 mcg/mL)
native and prosthetic valve have the same tx:
1) PCN +/- gent
OR
2) ceftriaxone +/- gent
OR
3) vanco
photo of strep definitive therapy in IE
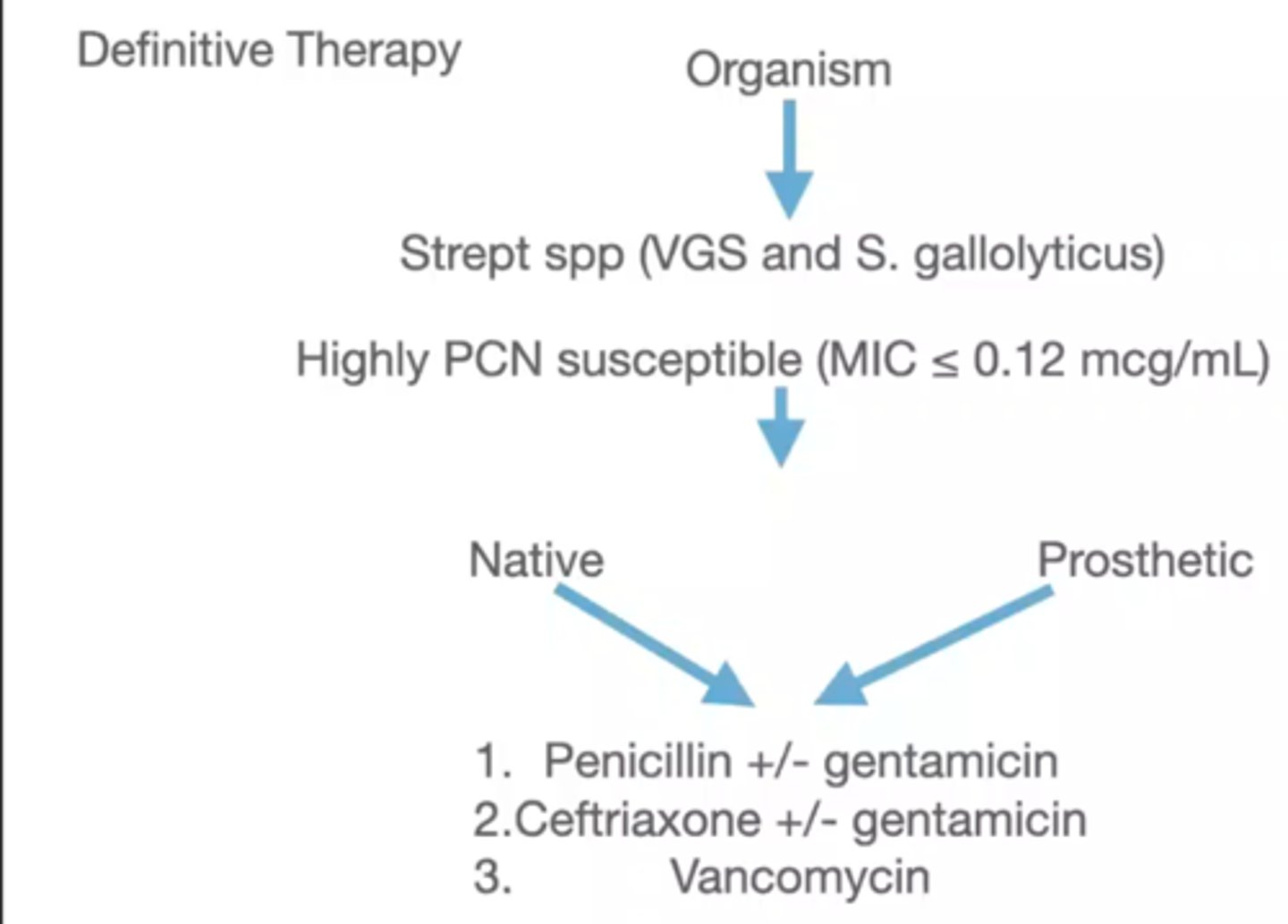
difference in duration of therapy for streptococcus IE
duration is longer for prosthetic valve compared to native valve
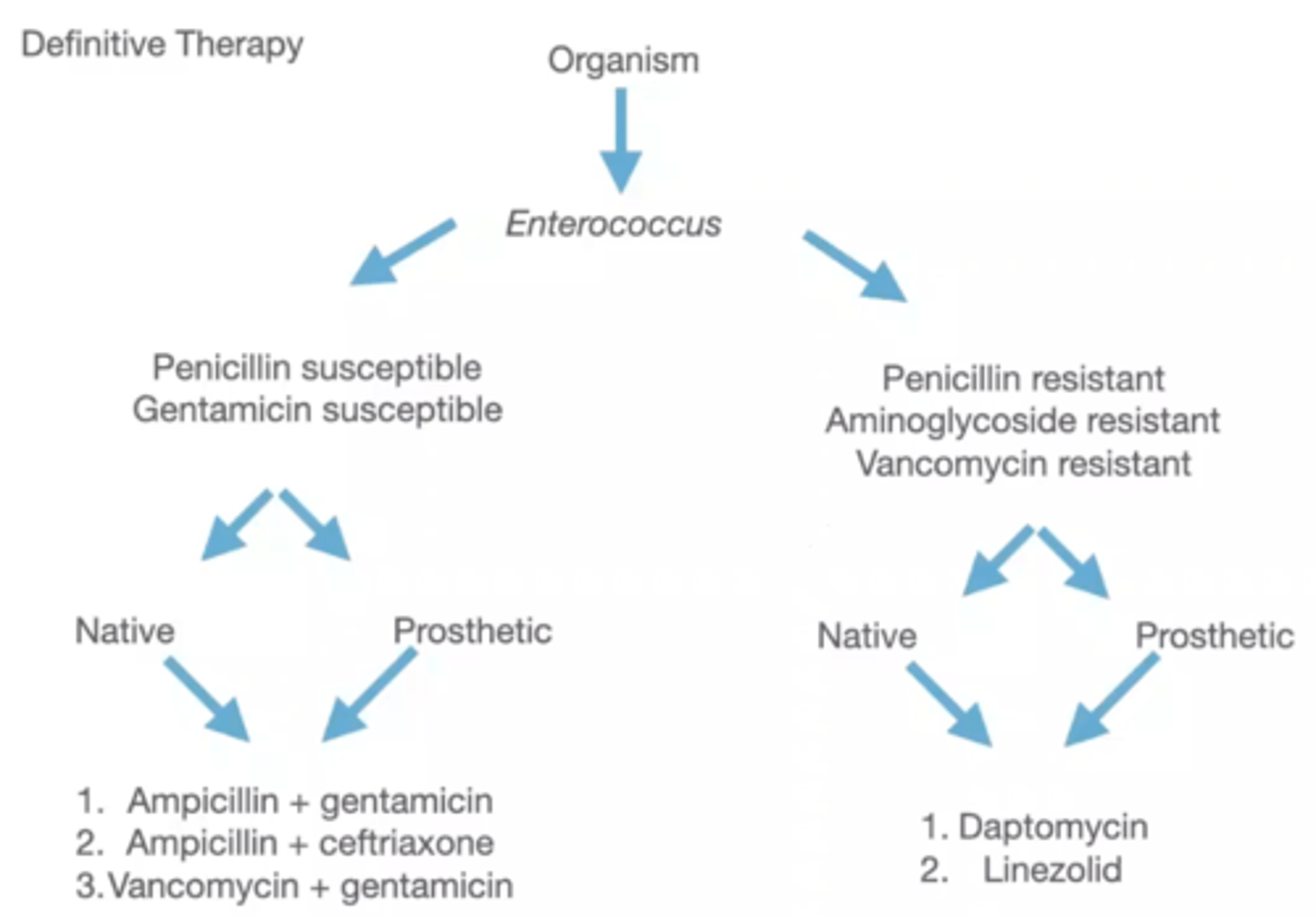
enterococcus IE definitive therapy tx algorithm step 1
PCN susceptible vs resistant
Gent susceptible vs resistant
Vanco resistance
after determining resistance, what is the next step in enterococcus IE tx algorithm?
type of valve does not matter -- tx is the same!
what are the treatment options for PCN and Gent susceptible enterococcus IE?
1) amp + gent
2) amp + ceftriaxone
3) vanco + gent
Go through the entire side of the enterococcus tx algorithm for PCN and Gentamycin susceptible side
1) PCN and Gent susceptible
2) valve doesn't matter
3) (amp + gent) OR (amp + ceftriaxone) OR (vanco + gent)
consider enterococcus in IE that is resistant. What agents would it be resistant to that helps determine the treatment algorithm?
-PCN resistant
-AGS resistant
-vanco resistant
once you determine that enterococcus is resistant, what is the next step?
Valve doesn't matter! tx is the same
tx options for resistant enterococcus in IE
1) dapto
OR
2) linezolid
go through the entire flow chart for the resistant enterococcus IE algorithm
1) organism isolated is enterococcus
2) resistant to PCN, AGS, or vanco
3) valve doesn't matter
4) give dapto or linezolid
Ask if a strain is vanco resistant but susceptible to AGS and PCN if we can still give the "susceptible" treatment
photo of enterococcus tx algorithm in IE
which agent is often used in synergy dosing?
gentamycin
dosing for gentamycin in synergy dosing
1mg/kg q8h (adjusted based on renal function)
This is LOW DOSE gent
when is once daily dosing for gentamycin supported in the literature?
What is the regimen?
only in streptococcal IE (3mg/kg/day)
Note this is just the 1mg/kg/8hr dosing as a single daily dose
-no longer recommended in Staph aureus
what does duration of therapy in IE depend on?
valve type and infectious organism
what are the general durations of therapy in IE and what are the criteria for these durations?
susceptible organisms in native valves:
-shorter courses (2 weeks)
prosthetic valves and/or more resistant organisms:
-longer courses (≥ 6 weeks)
Monitoring for the medications used to treat IE
-vanco = AUC (2015 guidelines recommend troughs)
-gentamycin = troughs for G(-) and safety; Peaks for efficacy (esp. in G(+)) double check this one
-dapto = CPK
-beta lactams = delayed hypersensitivities, drug fever (7-10 days), C. diff
-Nafcillin/oxa = AIN
-Linezolid = serotonin syndrome, myelosuppression, thrombocytopenia (esp after 2 wks)
criteria to consider for outpatient antimicrobial therapy for IE
-ability to travel
-cognition
-insurance
-IVDU hx
-stability of drug
-# of daily doses of abx
IE is more likely to occur with ____1____ rather than ___2____
1) activities of daily living
2) a single medical or dental procedure
what activities of daily living tend to be a potential cause of IE
brushing teeth and chewing food b/c we can become transiently bacteremic
what needs to be considered when determining if prophy for bacterial endocarditis is worth the costs?
-resistance
-AEs
-etc
how often do benefits outweigh costs of using IE prophy?
Usually benefits do NOT outweigh costs
best way for patients to avoid bacterial endocarditis
consistently good oral hygiene
what patient groups are most likely to be candidates for IE prophy?
-prosthetic cardiac valves
-prosthetic material used for valve repair (annuloplasty rings and chords)
-previous IE
-unrepaired congential heart disesase
-repaired congenital heart disease w/ residual shunts or regurgitation
-cardiac transplant w/ valve regurg. d/t abnormal valve (Note cardiac transplant by itself is NOT reason for prophy--must have structural abnormality as well)
when do we give patients IE prophy if they are a candidate?
prior to THESE dental procedures:
-manipulation of gingival tissue
-manipulation of periapical region of teeth
-perforation of oral mucosa
which dental procedures are NOT procedures for which we would provide IE prophy?
-routine anesthesia injections through non-infected tissue
-dental radiograph
-placement or adjustment of orthodontic device
-trauma to teeth or lips
what pathogen is targeted in IE prophy and why?
most common pathogen to cause IE from a dental procedure is viridians group strep
medications used for IE prophy
-amoxicillin PO
-ampicillin (IV/IM)
-cefazolin (IV/IM)
-ceftriaxone (IV/IM)
Remember ONLY FOR procedures that manipulate gingiva, periapical region of teeth, or perforation of oral mucosa
when is prophy for IE given for those who receive it?
BEFORE dental procedure
Pt with aortic valve infective endocarditis has blood cultures that are positive for GPC in clusters. Which of the following organism is most likely causing this infection? (furthermore, what would all of these look like on a gram stain)?
a) Enterococcus faecium
b) staphylococcus aureus
c) pseudomonas aeuriginosa
d) streptococcus gallolyticus
A) E. faecium is GPC in chains or pairs
B) staph aureus is GPC in clusters
C) pseudomonas is GNR
d) strep gallolyticus is GPC in pairs or chains
Pt. presents to ED w/ 2 wk hx of faigue and SOB. they are 35 yo w/ PMH of current IVDU (heroin). There is a new systolic murmur noted on exam and patient is sent for TTE that shows aortic valve vegetation. Dx is infective endocarditis. What is the most appropriate classification for this patient's infection?
a) native valve IE
b) prosthetic valve IE
A) native valve b/c this patient does not have a prosthetic valve
Pt is Dx w/ prosthetic valve IE. They are not stable, so the team wants to start empiric therapy while waiting for blood culture results. Pt has NKDA and good renal function. Which of the following is most appropriate empiric therapy for this patient?
a) vanco
b) vanco + gent
c) vanco + gent + rifampin
d) vanco + gent + ceftriaxone
C) Vanco + Gent + rifampin
B would be correct if the patient had native valve endocarditis:
-vanco + either ceftriaxone or gentamicin
a patient w/ prosthetic valve IE culture report comes back with E. faecalis growth and the following broth dilution information:
-Amp susceptible, MIC ≤ 8
-Dapto susceptible, MIC ≤ 2
-getn susceptible, MIC < 500
-Linezolid susceptible, MIC ≤ 2
-vanco susceptible, MIC ≤ 4
Which of the following would be the most appropriate definitive therapy?
a) linezolid
b) amp + gent
c) dapto
d) vanco
B) amp + gent
Recall that prosthetic valve endocarditis w/ enterococcus flow chart is as follows:
1) determine susceptibility to PCN, gent, and vanco
2) tx is same for each valve type
3) if susceptible, use amp + gent, amp+ ceftriaxone, or vanco + gent
4) if resistant, use dapto or linezolid
This patient has susceptible enterococcus, so we have 3 options to choose from, and B is the only one that works. Also note that this is not MRSA or VRE, so we don't need to use something as broad as vanco, dapto, or linezolid
which of the following should be monitored for linezolid?
a) alkaline phosphatase
b) CBC
c) linezolid peak concentration
d) CPK
B) d/t myelosuppression. It is usually thrombocytopenia, but can suppress any blood line, so we want a CBC usually.
Which of the following patients is prophylaxis for IE prior to dental procedures that manipulate the gingival tissue recommended? SELECT ALL that apply.
a) 65 yo F w/ PMH of IE 20 years ago
b) 54 yo on chronic prednisone for RA
c) 70 yo status post cardiac repair w/ prosthetic annuloplasty ring
d) 25 yo cardiac transplant pt w/o any cardiac complications or abnormalities
A and C
Remember criteria are:
-PMH of IE REGARDLESS of age or timeframe
-prosthteic valves or material used in repair
-unrepaired congential heart disease OR repaired but w/ residual shunt or regurgitation
-cardiac transplant w/ residual valve abnormality (eg/ regurgitation)
Immunosuppression does not require prophy, and neither does cardiac transplant w/o abnormalities
Pt dx w/ native valve IE. They are not clinically stable and want to start empiric therapy while waiting on cultures. Which of the following is most appropriate:
a) vanco
b) vanco + gent
c) vanco + gent + rifampin
d) vanco + ceftriaxone + gent
vanco + gent
Remember for native valves, empiric therapy is either:
-vanco + gent
OR
-vanco + ceftriaxone
Prosthetic valve empiric therapy would be C
consider these patients who each had 2 sets of aerobic and anaerobic blood samples drawn. Which of these would suggest a true infection and therefore requires treatment? (First two are one set, the second two are the 2nd set)
a) NG, NG, NG, G
b) NG, NG, G, G
c) NG, G, NG, G
d) Ng, G, G, G
e) G, G, G, G
You can't know without more information:
1) patient sick or not sick?
2) bacteria (frequent contaminant or true pathogen)
3) Which bottles are positive
For test:
a) sick patient w/ true pathogen = treat
b) not sick patient w/ frequent contaminant = no tx
Just as a note, if penicillin susceptibility is reported as S on a C+S but carbapenem sensitivities are not reported, you can assume that the organism is susceptible to carbapenems
which valve is most likely to be affected in IVDUs who contract endocarditis, and what pathogen is most likely to cause IE in these people?
Staph aureus on the tricuspid valve