Microbes-L14-Adaptive Immunity 2: Anti TB Immunity
1/18
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
19 Terms
what are some downsides of immune system?
if uncontrolled can attack our own tissues
- usually have a tolerance for antigens
what are the innate and adaptive cells?
innate- neutrophils, NK cells, macrophages(have PRR’s) and secrete cytokines, dendritic cells
adaptive- T cells(T cell receptors), and B cells(have antibodies)
what do the cells in the innate do? what do the cells in the adaptive do?
presentation- macrophages and dendritic cells
phagocytosis- neutrophils and macrophages- also make cytokines
T cells have T cell receptors- make cytokines- CD4 and CD8
B cells- make antibodies
receptors of the innate system? what do these innate cells do specifically?
macrophages have pathogen recognition receptors- not very specific for any one single antigens
they take up bacteria and present them to T cells- their PRR’s bind to the pathogen associated molecular pattern PAMP- ie LPS
dendritic cells activate naive T cells
discuss macrophages- receptors types, roles
innate immunity
macrophages in the bone marrow- go to various tissues- liver(kupffer cells)
have non specific receptors- PRRs, Fc and complement receptors
have Fc and complement receptors- macrophages recognise and engulf pathogens when they’re “tagged”- with Fc receptors and compliment receptors- which helps target the antibody
phagocytose and kill microbes
and present the antigen to T cells
explain dendritic cells- what do they activate, how they go from immature to mature
only cell that can activate naive T cells in lymph nodes
once activated by a dendritic cell- T cell can become an effector T cell(fight infection) and memory T cell
dendritic cells- (immature)reside in lung, gut etc- encounters pathogen by PRRs and detect PAMPs- takes it up and activates dendritic cell and migrate to lymphatic tissue(mature)- activate naive T cells
discuss neutrophils- how long do they live, when are they mobilised?
they are short lived- last 2/3 days at most
first cells mobilised to phagoctyose
important against pyogenic pus forming bacteria- kill bacteria and then die
non dividing cell
polymorphic leucocyte- has distinct shape
3 defining features of the adaptive immunity
antigen recognition- discriminates self from non self T cell receptor and antibodies
specificity- each lymphocyte recognises 1 antigen
diversity- large no. of lymphocyte specificty- infinite capacity to responds
memory- can recall interaction with an antigen. when antigen is recognised by T cell- some become memory cells
produces highly regulated cytokines: cause inflammation- has regulatory cells, cytokines and immune checkpoints to turn this response off
what are adaptive immune responses?
B cells
bone marrow- make A- antibody producing plasma cells
receptor- Ig
antibody recognises unmodified naive antigen
mediate humoral imunity- promote phagocytosis, activate compliment system, neutralise pathogen
T cells
bone marrow/thymus
has CD4(helper) and Cd8 T cells(cytotoxic)
T cell receptor- unique to particular antigen
recognise processed antigen on APC(Antigen presenting cell) in association with MHC molecules- MHC I-CD8, MHCII-CD4
mediate cellular immunity-interacting with infected or abnormal cells or regulating others
difference between humoral immunity and cellular immunity
Humoral immunity involves B cells producing antibodies that recognize and neutralize pathogens, while cellular immunity involves T cells directly attacking infected or abnormal cells and regulating immune responses.
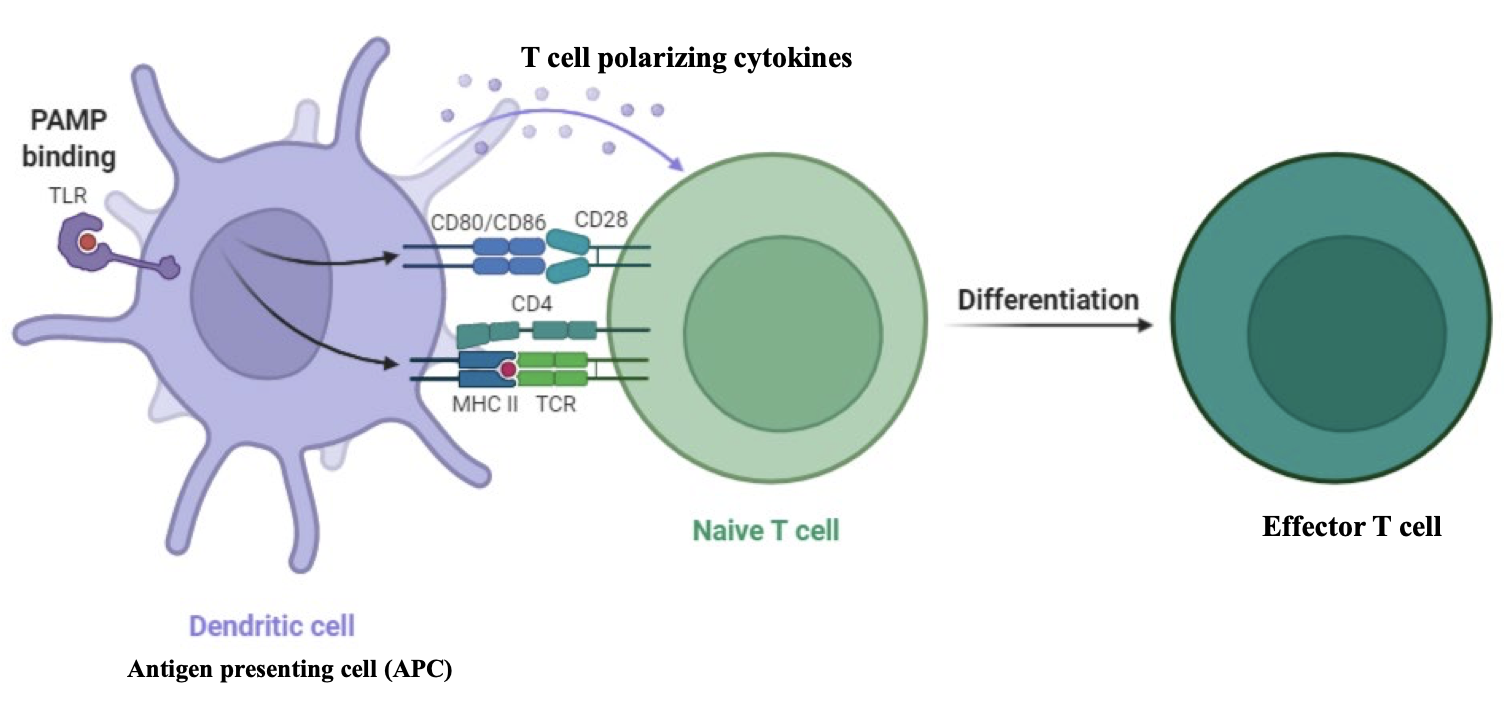
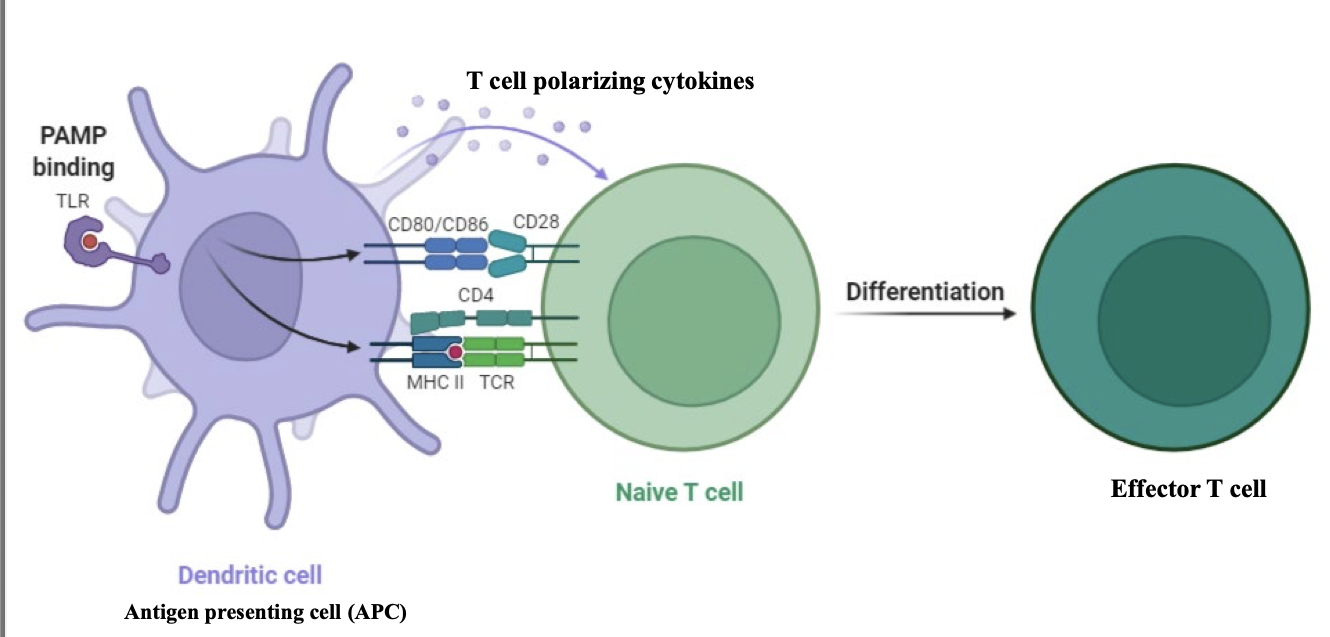
3 signals for T cell activation
T cell receptor recognises and binds to peptide presented on MHC molecule on the surface of an antigen presenting cell(dendritic etc)
MHC I presents to CD8 cytotoxic cells
MHC II presenting to CD4 helper cells
costimulatory signals are needed- CD80/CD86(dendritic) interaction with CD28(naive T cell)- 2nd signal
polarising cytokines that come from dendritic cells and other innate ones
difference between CD8 and CD4 T cells?
CD8- presented by MHC I- cytotoxic cells
CD4- presented by MHC II- helper cells
explain antibody molecules and explain T cell receptors.
have a contant region- same for all antibodies of a specific clas
has a variable region- specific to each antibody and binds to a specific antibody
TCR- T cell receptors
have a singular arm structure- still has constant and variable region
variable region- diversity- recognise a specific epitope displayed by MHC on the surface of antigen presenting cells
what are epitopes? how do they bind? 4 steps
Epitopes are specific regions on antigens that are recognized and bound by antibodies or T cell receptors. They are crucial for the specificity of immune responses.
antibodies bind to epitopes
epitopes recognised by T cells are buried- must be broken into fragments
epitope binds to a self MHC molecule(APC)
T cell then binds to the MHC complex(on antigen presenting cell)
explain the MHC structure- where are they found? what do they bind to? how do they bind?
MHC found on antigen presenting cells such as dendritic cells and bind to the epitope
MHC- 2 alpha helices with a cleft and beta sheets
peptide epitope is held by IONIC interactactions- peptide is pos and MHC neg- held in place
T cell binds on top
difference between CD8 and CD4
class 1 MHC-CD8- usually virus infected- becomes effector cytotoxic T cell-kills infected cell
virus needs host cell to replicate/bacteria need nurtients
viral DNA translated to proteins through ER and golgi- get processed as MHC I peptides as a viral class I MHC peptide
CLASS 1:PRESENT PEPTIDES FROM INTRACELLULAR ANTIGENS!!! IE VIRAL PROTEINS TO CD8!!
class 2 MHC-CD4- becomes activated T helper cells- which help B cells become secreting plasma cells by mediating cell responses
process the cell by ENDOCYTIC route
antigen taken up by antigen presenting cell
goes into the endosome and fuses with the lysosome- proteases inside with low pH which denatures the protein
CLASS 2: PRESENT PEPTIDES FROM EXTRACELLULAR THE CELL! TO CD4!!
CD4 MHC II- what do they secrete?
Th1- IFN- gamma- autoimmunity- intracellular- macrophages
th2- IL-4- extracellular pathogens- allergies- antibodies
Treg cell- IL-10- immune regulation- stops maturation of dendritic cells etc
Th17 cell-IL-17- immunity to infection/inflammation- autoimmunity-recruits neutrophils
immune response to a pathogen- 6 steps
recognition- detect pathogen using PRRs and PAMPS, APC present this to MHC molecules T cells recognise this
clonal expression- T and B cell activated- rapid division
differentiation of responder cells- ie T cells- CD8 cytotoxic or CD4 helper, memory cells, plasma cells
recruitment and activation of effectors- macrophages, neutrophils, NK cells, more T and B
effector function- eliminate using antibodies, cytotoxic T cells, macrophages, compliment
down regulation- regulatory T cells like Treg stop
how do antibodies work?
CD4 activate B cells to make plasma cells- for making antibodies- specific to antigen
neuralisation- bind directly to pathogen and block ability to bind to host cell receptors
opsonisation- coating of antigen with antibodies- make it easier to recognise and engulf it- Fc constant to Fc receptor- promotes phagocytosis
complement activation- in the blood can be activated by antibodies- enhances opsonisation and lyses some bacteria