PSYCH 101 Chap 16: Therapy
1/40
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
41 Terms
Psychotherapy
treatment of psychological problems through psychological techniques
over 500 types
placebo effect
nonspecific improvement as a result of a person’s expectations of change
double-blind technique
the researcher doesn’t know which group has the placebo
demand characteristics
characteristics in environment that may cue a participant to what’s going on
Hans Eysenck
claimed that psychotherapy produced no greater change in maladjustment than natural life experiences
but he took findings across all disorders (systematic research) → problem because some therapies not effective for some disorders
ex. psychoanalysis not appropriate for schizophrenia
eclectic approach
integrating diverse theories and techniques, taking pieces that are evidence based
ex. exercise is good + cognitive therapy with intervention, these come together, but also have own good factors
Client Common Factors
expect positive outcome
exceptions: people with schizophrenia may not because they think those people are against them (no insight so delusions of persecution), teenagers with personal fable, forced into it
receive attention, which helps maintain positive attitude
must be willing to make a change
Therapist Common Factors
(CCRMM)
communicate interest, understanding, respect, tact, maturity, ability to help
competency in the area
respect client’s ability to cope
make suggestions, offer encouragement, provide alternate interpretations and salient examples
must not engage in other relationships with the client
Rapport - interact well with you via all these things
must respect multiculturalism and recognize that culture is a powerful influencer of behaviour
Brief Therapy
planned short-term (1-2 sessions)
operational diagnosis: “why is the client here today?”
establish precise goals for the therapy
Psychodynamic Therapy
Freud = insight therapy
2 basic assumptions:
becoming aware of one’s motivation helps to change
the causes of maladjustment are unresolved unconscious conflicts
Psychoanalysis
Neo-Freudian based therapies
Psychoanalysis
developed by Freud, lengthy insight therapy that aims at uncovering unconscious conflicts and using techniques like free association and dream analysis
Goals: address unresolved conflicts then change of behaviour persists
**Primary Components: (F DIRT)
Free Association - talk about whatever comes to mind, not directed in any way, unconscious things might then come out, ex. Rorschach inkblot test
Dream Analysis - express any dreams, talk about in detail, not with a lot of interpretation at this point, unresolved unconscious things may come out
Interpretation - therapist + client provide context, explanation, meaning of some of these things coming out in preconscious
Resistance - may resist providing explanation/interpretation, client not working to do this
Transference - transfer feelings of love + safety onto therapist, client may think they’re developing real feelings, but really just safe place to share those feelings
Working Through - cycle of interpretation, resistance, and transference occurs repeatedly
Neo-Freudian based therapies
use techniques derived from Freud, reject or modify parts of his theory
concerned with conscious aspects of client’s functioning, more optimistic towards functioning, emphasize needs for power, love, status (not just sex + aggression)
Criticisms of Psychoanalysis
unscientific, imprecise, subjective
hard to evaluate
research based on women
expensive in time + cost (about $200/h, but multiple times a week for years)
not effective for CBT (Cognitive-Behavioural Treatment)
have to have certain level of intellectual functioning
Humanistic Therapy
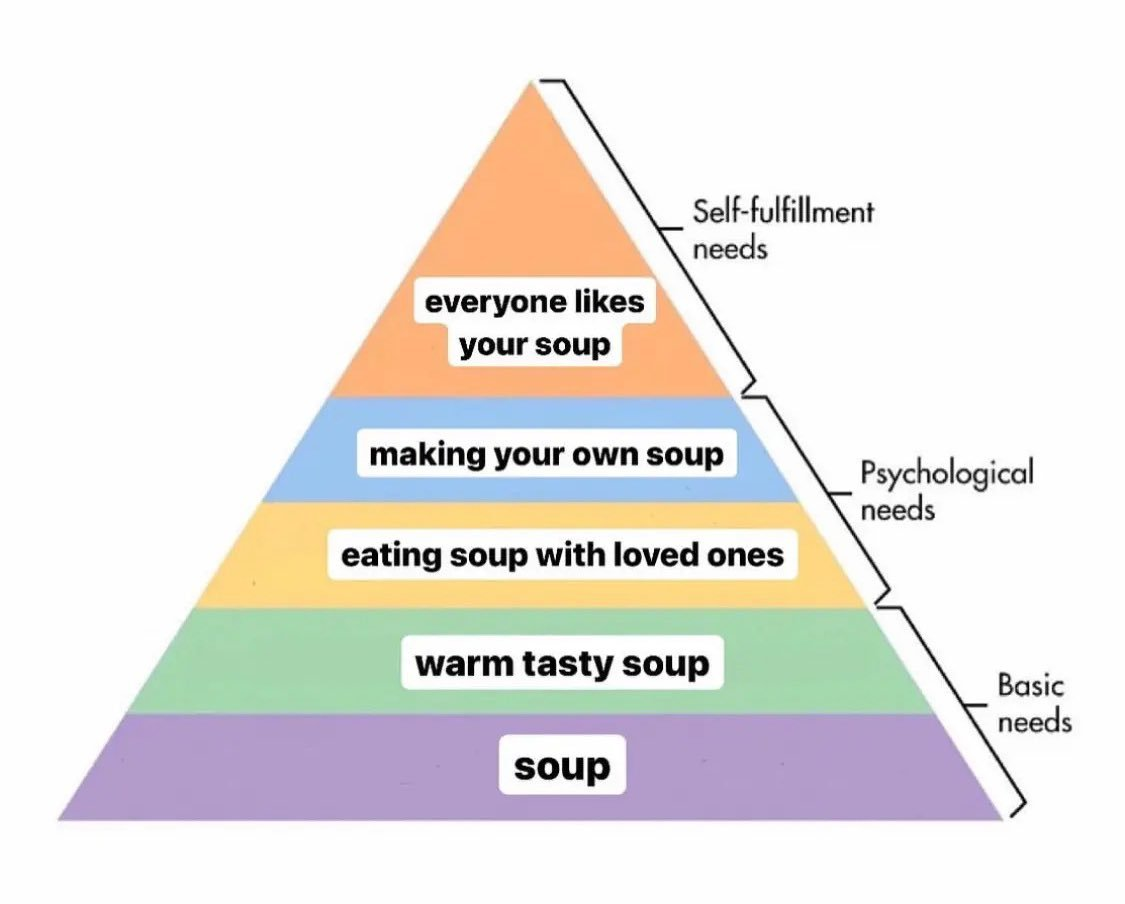
Carl Rogers, Abraham Maslow (hierarchy of needs)
emphasizes development of human potential (people want to be the best they can be), belief that human nature is basically positive, importance of assuming responsibility and living in the present (not blame unconscious, think about the role we play)
not typically for mental health issues, ex. schizophrenia, acute mental health issues
Client/Person-Centred Therapy
(Humanistic)
developed by Carl Rogers
insight therapy that helps people evaluate/gain insight to the world and themselves from their own perspective, when can’t reach full potential, can lead to mental health issues
therapist guides, discover ideal selves, ask lots of questions
therapist must show: (CUE)
unconditional positive regard - accepting of who the client is right now, shows positive interaction even if they don’t agree
congruence - therapist themselves must be aware of things that might bias them towards their clients, should be neutral
empathetic listening - show client that they understand that the client is feeling that way, even if they haven’t felt that way themselves, often paraphrasing what the client tells them
tries to increase awareness and heightened self acceptance, hopes to: (RAT)
think more realistically - ex. feel less guilt
become more tolerant of others
engage in more adaptive behaviours - ex. more productive behaviours
Pos/Neg of Client/Person-Centred Therapy
positives:
- focus on therapeutic relationship
negatives:
- core concepts are difficult to falsity
- not enough to bring about change
- more effective than no treatment, but mixed results compared to other therapies
Behaviour Therapy
quick, relatively unexpensive, effective for problem behaviour
focus on what person is doing right now, help replace maladaptive behaviours with effective ones
operant conditioning to establish a new behaviour often depends on a reinforcer, an event or circumstance that increases the probability a response will occur, ex. want to clean room, allowance, positive reinforcement
token economies, extinction, punishment, time out
Token Economies
(Behaviour Therapy)
reward adaptive behaviour: people who display appropriate behaviours receive “tokens”, use tokens to buy or trade in for items
often seen in classrooms, want behaviour to continue, similar to allowance
Extinction
(Behaviour Therapy)
if you don’t reinforce behvaiour or don’t pay attention to it, eventually the behaviour will go away/into extinction
ex. babies cry and their parents come, so as they get older, pull back time going into room and they’ll learn to sleep (sleep training)
Punishment
(Behaviour Therapy)
does not replace with positive behaviour, just aversive stimulus
ex. not put hand up, X on board, but not told how to get rid of it → suppress behaviour, but not increase likelihood of a positive behaviour
punishment is imitated and can bring about generalized aggression → ex. bobo doll, modelling
Time Out
(Behaviour Therapy)
removal of a person from sources of reinforcement to decrease behaviour, takes persistance
ex. kid moved to other area to not get laughs from lots of kids
should only do 1 minute per year of age, good to be in a place nearby, not have ongoing conversations with them
Exposure Therapy
in counterconditioning (reinforces feared situation won’t happen), a person is taught a new, more adaptive response to a stimulus
Systematic Desensitization
Aversive Conditioning
Systematic Desensitization
(Exposure Therapy)
developed by Joseph Wolpe
based on reciprocal inhibition (can’t be anxious and relaxed at same time)
taught relaxation first (2 types):
progressive muscle relaxation - tightening + relaxing muscle groups (taught then do at home)
manual relaxation - picture soothing image in head and think about sensory experiences about that environment, imagining they are there
hierarchy of fears to then gain mastery of these fears, progressing with each level until anxiety is 0
Dismantling research (look at full procedure) showed that no single component was essential → flooding is without teaching relaxation and the ladder, takes commitment but very effective
Aversive Conditioning
(Exposure Therapy)
a noxious stimulus is paired with a stimulus that elicits an undesireable behaviour, often used to combat addictions
ex. take nausea inducing drug, so if drink or smoke, feel nauseous, then associate drinking/smoking with unpleasant feeling/nausea
Modelling
(Exposure Therapy)
developed by Bandura
used effectively for teaching new behaviour, helping eliminate fears, and enhancing already existing behaviours
ex. kid afraid of dogs, adult pets and talks to dog, show everything is good
Cognitive Behaviour Therapy (CBT)
change client behaviour by changing the person’s thought or perceptions
3 basic assumptions: (IFI)
Cognitions are identifiable and measurable (tackle thoughts)
Cognitions are key in both healthy and unhealthy psychological functioning
Irrational beliefs or thinking can be replaced by more rational and adaptive cognitions (if have unhelpful thought → identify → then change)
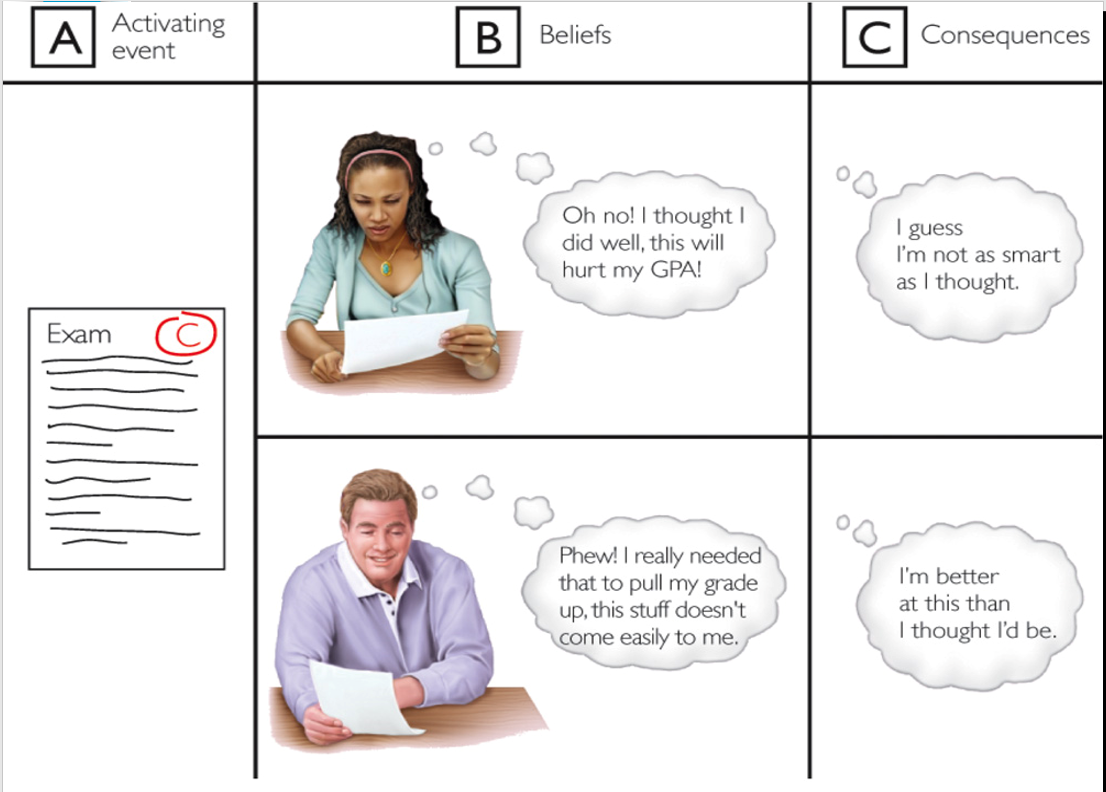
Rational Emotive Therapy
emphasizes the importance of logical, rational, thought processes
Albert Ellies, very much in-your-face/directive, same event won’t effect everyone the same
assumed abnormal behaviour is caused by faulty and irrational thinking patterns
how we feel about the consequences of an event is determined by our beliefs or opinions
A. Activing event (ex. C on exam)
B. Belief (ex. see as good or bad)
C. Consequences (ex. positive or negative thoughts about self)
Irrational beliefs: product of people’s needs to be liked, to be competent, to be loved, and to feel secure
exaggerated value on needs = abnormal behaviour
Aaron Beck’s Approach
(Cognitive Behaviour Therapy/CBT)
depression is caused by people’s distorted thoughts about reality, lead to negative views of the world, self, and future →
identify this as unhelpful, then can do something to change it, more directive
Shown effective with depression, and also bipolar disorders and schizophrenia
Waves of CBT
First: Behavioural
Second: Cognitive
Third: Acceptance and Commitment Therapy and Dialectical Behaviour Therapy
highly eclectic, remains to be seen if more effective
Internet Delivered CBT
Dr. Heather H. (Dr. Thomas H’s wife)
message or phone to help guide through therapy, transdiagnostic, designed to treat anxiety + depression together
50% reduction of symptoms
Group Therapy
3-20 clients meeting on a regular basis with therapist, group members selected on the basis of what they can gain and offer to the group, group members encouraged to role play new behaviours
led by a therapist, there is an agenda
social anxiety disorder would be good for this → garner skill set just exposed to the group, focused on anxiety disorder, already exposed because showed up
Family Therapy
two or more people who are committed to each other’s well-being are treated together, therapists attempt to change the family systems (what is going on), the dynamic social system of the marriage or family (focus on interactions)
ex. not just focusing on the anxious child, but also behvaiours of the other family members maybe inciting or maintaining that anxiety
Biologically Based Therapies
include medication, hospitalization, physicians
often used in combination with traditional forms of psychotherapy
Drugs
(Biologically Based Therapies)
- will not permanently cure (garner skillset, symptoms reduce, then look to get off them)
- start on low dosage typically then move up
- side effects may deter people
- began with development of Thorazine (antipsychotic) in 1954
- 15% of population on antidepressants
Anti-Anxiety Drugs
(Biologically Based Therapies)
reduce physiological symptoms of stress, calms them so able to think more rationally about thigns
Benzodiazephines - modulate GABA, modifies these inhibitory receptors so serotonin can move more freely
used for seizures in a hospital
abusable, not prescribed long term
may be given a few if have bad panic attacks
colonoxopy to help sleep
fast affects
Selective Serotonin Reuptake Inhibitors (SSRIs) - modulates serotonin
able to be prescribed long term
take longer to exhibit change
Anti-Depressant Drugs
(Biologically Based Therapies)
work by altering levels of brain chemicals
3 major categories:
Tricyclics - oldest types
insomnia, chronic headaches
blocks reuptake of multiple neurochemicals, not as specific → serotonin, norepinephrine
because of that, more side effects, allows for more of these neurochemicals to be available in that synapse
Monoamine Oxidase (MAO) Inhibitors
works by breaking down monoamine oxidase (enzyme that destroys neurotransmitters), then allows for more neurochemicals to be available which results in change of mood
not prescribed often, food restrictions
SSRIs
Mood Stabilizing Drugs
(Biologically Based Therapies)
often used for bipolar disorder, careful monitoring required, too much will produce noxious side effects, too little will have no effect
lithium carbonate - harsh on system, can impact immune system, very effective but hard on body
anticonvulsant agents - more likely for stabilization in younger patients, sometimes used for epilepsy
Anti-Psychotic Drugs
(Biologically Based Therapies)
antipsychotics are a group of drugs commonly but not exclusively used to treat psychosis and schizophrenia
Chlorpromazine (Thorazine) was the first antipsychotic, 1st gen
only affected dopamine (D-2) receptors, blocking them
effect was primarly seen on positive symptoms (hallucinations + delusions)
Atypical antipsychotic (newer/2nd gen)
Clozapine, Olanzapine, Risperidone
affected both dopamine + serotonin, so both positive + negative symptoms
major side effect is tardive dyskinesia:
central nervous system disorder
involuntary, spasmodic movements of upper body, leg jiggling, tongue protrusions, facial tics and involuntary movement of mouth + shoulder
more risk with older types of anti-psychotics
because dopamine is so restricted, mimics Parkinson’s disease
Psychosurgery
brain surgery, common type in 1940s-50s was prefrontal lobotomy:
removal of parts of brain frontal lobes thought to alleviate mental disorder symptoms
made some people unnaturally calm and completely unemotional
used today as absolute last resort with conditions like severe OCD, depression, bipolar disorders, done very small and precisely
Electroconvulsive Therapy (ECT)
electric current is briefly applied to the head to produce a generalized seizure (convulsion), affecting negative mood symptoms
sparingly now, once widely used for depression, was used willy-nilly in psych hospitals
now used for treatment resistant depression (late measure), all that shows is a toe moving, under control of physicians with anesthesia/pain meds
50% relapse within six months, clouded memory
Deinstitutionalization
transitioning of treatment for mental health problems from inpatient facilities to outpatient or community-based facilities, while in would be engaged in work, activities, and therapies
benefits must be weighted against number of untreated individuals and homeless with mental illness
problem: transitioned out, but there was no community support for them when let out, many homeless or into the criminal justice system