PHAR 232-Fluid Balance/Cardiology
1/114
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
115 Terms
total body fluids are found:
• Intracellular (ICF) about 2/3 of total body water (TBW)
• Extracellular (ECF) about 1/3 of total body water (TBW)
-Plasma
-Interstitial
Can water easily move between ICF and ECF?
yes
can solutes such as Na+ easily move between ICF and ECF?
no
the body has to maintain a certain amount of circulating fluid in the ___ to maintain ___ and ____.
The body has to maintain a certain amount of
circulating fluid in the vasculature (plasma) to maintain
blood pressure and perfusion of organs and tissues.
what regulates sodium concentration and affected by what four factors?
Sodium concentration is regulated by physiological processes of WATER balance
• Intake of water and thirst
• ADH (Vasopressin)
• Kidneys holding on to or releasing H2O
• osmoreceptors
What regulates Fluid status and the four factors?
Fluid status is regulated by Sodium balance
• FLUID is your VOLUME (fluid= SODIUM + WATER)
• Water always follows sodium --so retention or excretion of sodium by the kidneys causes FLUID loss or gain
RAAS (Renin, Aldosterone, Angiotensin II)
ANF – atrial natriuretic factor (or peptide)
Kidneys retaining or releasing sodium
Baroreceptors
Hyponatremia is having too much water that can’t be
excreted
Hypernatremia is having too little water that can’t be
replaced
Hypovolemia is the
loss of SODIUM AND WATER
Hypervolemia is the
gain of SODIUM AND WATER
You can have hypernatremia with hypo- or hypervolemia and vice versa however …
H***VOLEMIA AND H***NATREMIA ARE TWO SEPARATE ASSESSMENTS
Hypovolemia—any condition where the ECF volume ___ due to
is reduced
• Dehydration
• Major bleeding
• ETC
Euvolemia is
normal fluid levels
Hypervolemia- any condition where the ECF volume
is increased
• Edema
• Inappropriate IV fluid replacement
Hypovolemia: Volume depletion results from loss of sodium and water
from the following 4 anatomic sites:
Gastrointestinal losses, including vomiting, diarrhea, bleeding, and
external drainage
Renal losses, including the effects of diuretics, osmotic diuresis,
salt-wasting nephropathies, and hypoaldosteronism
Skin losses, including sweat, burns, and other dermatological
conditions
Third-space sequestration, including intestinal obstruction, crush
injury, fracture, internal bleeding, and acute pancreatitis
What are the signs and symptoms of hypovolemia?
• Postural dizziness– aka orthostatic hypotension
• Low blood pressure and increased heart rate (HR)
• Reduced jugular venous pressure (JVP)
• Fatigue
• Thirst
• Low urine output
• Delayed capillary refill –demonstrate
• Cool extremities
• Weight loss
• Extreme levels of hypovolemia lead to shock and hemodynamic collapse
What is dehydration?
Is when the ICF has lost significant amount of fluid
What rises as body loses water in dehydration?
As body loses water, osmolality and Na+ concentration rises
Water movement when dehydration occurs and fluid is not replaced?
Water moves from ICF to ECF along osmotic gradient if fluid is not replaced
What happens to ECF during dehydratio?
ECF usually maintains sufficient volume until ICF is
significantly depleted
Signs and symptoms of dehydration:
• Dry skin and mucus membranes
• Poor skin turgor and sunken eyes
• Low blood pressure
• Impaired mental status
• Extreme thirst
• Decreased urine output/Dark concentrated urine
What are causes of hypervolemia?
Excessive sodium or fluid intake
• Inappropriate IV hydration therapy
• Ingesting excessive amounts of sodium
Sodium or fluid retention
• Heart failure
• Nephrotic syndrome
• Cirrhosis
• Corticosteroid therapy
signs and symptoms of hypervolemia:
• Rapid and “bounding” pulses
• Increased blood pressure
• In heart failure a S3 heart sound (gallup)
• Distended veins
• Weight gain: 500 ml of fluid retained increases weight by about 0.5 Kg
• In prolonged sodium or fluid retention EDEMA will develop
Why does edema occur?
EDEMA occurs when a patient retains fluid (Na and H2O) and then the excess fluid moves out of the vasculature and into the interstitial space
Where does fluid accumulate in edema?
fluid can accumulate in the lower limbs, lungs, and/or heart or other tissues or organs
Where does standing patients vs bed bound pt have edema?
Standing patients will have edema in the feet whereas bed bound patients will have sacral edema
How is pitting edema?
• Can be assessed by pushing a finger into the edematous skin
• Measured as +1, +2, +3, +4
• + 1 is a mild imprint and + 4 is a deep imprint which is slow to reform
How is pulmonary edema asessed?
• Fluid builds up in lung tissue
• Associated with heart failure
• Auscultation of lungs will find “crackles”
• Shortness of breath
• Pink frothy sputum
What are common cardiac conditions?
CAD (aka CHD) - Coronary artery disease
Angina
Acute MI- A “Heart Attack”
arrhythmia
heart failure
What is CAD?
Usually asymptomatic until patient develops angina or has an MI.
What is angina?
• Chest pain, pressure, heaviness in chest.
what is unstable angina?
increasing in severity, longer in duration, or occurs at rest.
What is acute MI?
Intense and unremitting chest pain/pressure for 30-60 minutes
describe the three points of MI
• Retrosternal and often radiates up to the neck, shoulder, and jaw and down to the ulnar aspect of the left arm
• Usually described as a sub-sternal pressure sensation that also may be characterized as squeezing, aching, burning, or even sharp
• Some patients have a feeling of indigestion, fullness and/or gas
What is arrhythmia?
• Alteration of the heart rhythm affecting ability to pump blood
• Presents with palpitations, dizziness, fast or slow heart rate
• Fainting
What is heart failure?
• Inability of the heart to pump enough blood to meet the needs of the body.
• Shortness of breath at rest or exertion, lower extremity swelling, pulmonary edema.
• Sodium and fluid retention.
What are 6 modifiable factors of cardiac assessment?
• Smoking
• HTN
• Cholesterol
• DM
• Physical inactivity
• Diet
What are 4 non-modifiable factors for cardiac assessment?
• Age
• Race
• Sex
• Family history: Premature cardiovascular disease in 1st degree family member (men<55yo,
women <65yo)
What are 4 subjective measurements of cardiac assessment?
• Chest pain
• Dyspnea and/or Orthopnea (when self reported!)
• Syncope
• Palpitations
What are 9 objective measurements of cardiac assessment?
• Blood pressure –covered in vitals
• Pulse – covered in vitals
• RR- covered in vitals
• JVP
• Heart sounds
• Bruits
• Lung sounds– crackles
• Laboratory blood tests
• ECG
How is pulse taken?
Pulse– found by palpating the radial artery with index and middle fingers
Normal resting pulse rates in adults?
60 to 100 beats per minute (bpm)
What is bradycardia?
A rate of <60 bpm
Is bradycardia physiologically normal for some patients?
yes
what causes bradycardia?
• Can be the effect of drugs such as beta blockers
• Can be the effect of comorbidities such as hypothyroidism or heart block
What is tachycardia?
A rate of >100 bpm
what are causes of tachycardia?
• Can be the effect of drugs such as amphetamines, epi, etc.
• Can be the effect of comorbidities such as hyperthyroidism, pheochromocytoma, etc.
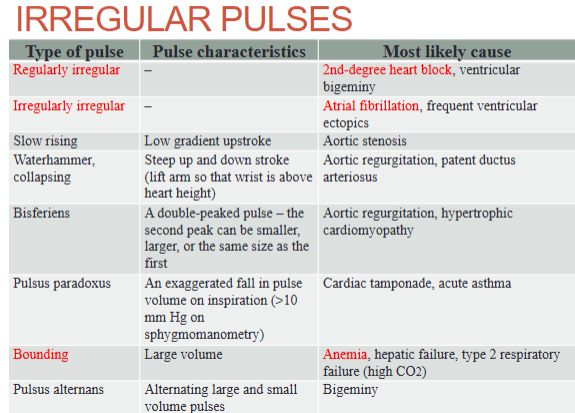
Irregular pulses
image
What is JVP?
JVP-The jugular venous pressure (JVP) is an estimate of the central venous or right atrial (RA) pressure
→The internal jugular vein connects to the RA without any valves in-between, acting as a column of blood to directly measure pressure
What is normal range for JVP?
JVP is 6 to 8 cm above the right atrium
What is abnormal/elevated range for JVP?
JVP is > 9 cm above the right atrium (> 4 cm above the sternal angle)
What happens to JVP in hypovolemia?
it falls
JVP rises with:
• Pulmonary hypertension
• Heart failure
Describe normal heart sound in S1
S1 – The first heart sound, S1, is produced by the closure of the mitral and tricuspid valves. This sound occurs at the beginning of systole and is best heard at
the left lower sternal border
Describe normal heart sound in S2
S2 – The second heart sound, S2, is produced by the closure of the aortic and pulmonic valves. This sound indicates the beginning of diastole and is best heard at the second left intercostal space.
Describe abnormal heart sound in S3
S3 – The S3 heart sound or “ventricular gallop” is produced when blood strikes a compliant ventricle during passive filling. This sound is best heard at the apex and occurs in the mid-third of diastole. The presence of an S3 is a sign of HF, as it occurs when the right or left ventricle is dilated and filling at high pressures.
Describe abnormal heart sound in S4
S4 – The S4 heart sound or “atrial gallop” occurs at the end of diastole, shortly before S1, and is produced when the atria contract and blood strikes a noncompliant left ventricle. This sound may be heard in those with left ventricular hypertrophy secondary to hypertension, aortic stenosis, or hypertrophic cardiomyopathy.
What are murmurs?
Murmurs –the sound of blood as it passes through a heart valve
Why do some murmurs occur?
Some murmurs occur as the result of high flow across the valve or
insignificant cardiac defects that are not pathologic in nature.
Called innocent or flow murmurs, these sounds are usually soft and
short in duration and have a “blowing” quality that may mimic the
sound of ocean waves
What else produces murmurs?
Murmurs may also be produced by turbulent blood flow through
a heart valve, and can indicate the presence and severity of
valvular abnormalities
how are murmurs defined?
Murmurs are defined according to their
timing within the cardiac cycle. Systolic murmurs are heard after
the S1 heart sound and before S2, whereas diastolic murmurs are
heard after S2 but before S1. Continuous murmurs extend across
multiple phases of the cardiac cycle
What are BRUIT?
BRUIT- sound of turbulent blood through an artery
• Can be due to narrowing or stenosis
• Usually heard during systole
How are lung sounds like in cardiac assessment?
Crackles- Sounds like Velcro ripping apart
• Can be found in pulmonary edema secondary to heart failure (HF)
What are the lab blood tests?
1)Biomarkers of myocardial necrosis
• cTN- CARDIAC TROPONIN
• MI and stable/unstable angina
2) Markers of inflammation
• CRP, hsCRP
• Risk factors for CVD
3) Markers of hemodynamic stress
• BNP, NT-proBNP
• Heart failure
Myocardial cell death due to
lack of blood flow
___“leak” into the blood stream where they can be tested
Dead myocardial cells “leak” into the blood stream where they can be tested
Purpose of biomarkers of myocardial necrosis:
• Aid in the diagnosis (or exclusion) of myocardial infarction as the cause of chest pain
• Facilitate triage and risk stratification of patients with chest discomfort
• Identify patients who are appropriate candidates for specific therapeutic strategies or interventions
what are Cardiac Troponins (cTnI and cTnT)?
• cTnI and cTnT are contractile proteins found only in cardiac myocytes.
• Highly sensitive and specific for for MI.
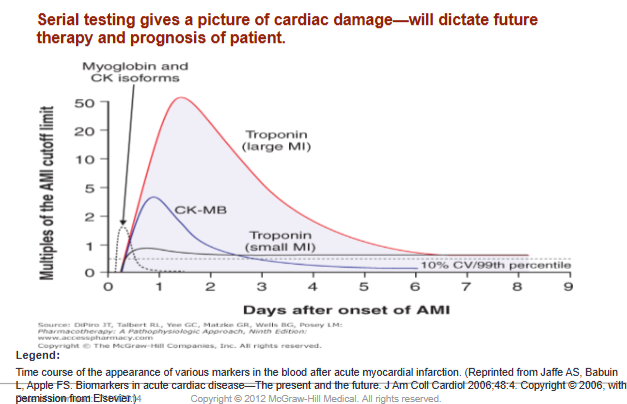
• Troponins are detectable in the blood 2 to 4 hours after the onset of symptoms and remain detectable for about 5 to 10 days.
What is the preferred marker for evaluating the patient suspected
of having a myocardial infarction?
cTn
In the patient with ischemic chest pain and electrocardiographic (e.g., ST segment) abnormalities, ____establishes the diagnosis of MI, and the absence of such an elevation excludes it
In the patient with ischemic chest pain and electrocardiographic (e.g., ST segment) abnormalities, an elevated serum cTn concentration establishes the diagnosis of MI, and the absence of such an elevation excludes it
The use of high-sensitive cTn assays improves
the early diagnosis of patients with suspected myocardial infarction, particularly the early exclusion of it.
What is cardiac troponins?
Cardiac Troponins- differences between the cTnI and cTnT
What are the differences between cTnI and cTnT?
1.cTnI
• Rise within 3-12 hours after MI
• Peaks in 24 hours
• Normalizes in 5-10 days
2.cTnT
• Rises within 3-12 hours after MI
• Peaks in 12 hours to 2 days
• Normalizes in 5-14 days
What are the markers of inflammation?
c-reactive protein
Hs-CRP
What are C-reactive protein?
an acute phase reactant produced by hepatocytes and induced by release of interleukin 1 and 6
What C-reactive protein indicative of?
Indicator of systemic inflammation in response to infection, injury, or chronic conditions
what is used in risk assessment for cardiovascular disease?
C-reactive protein
What can be raised by C-reactive protein?
Not Specific! Can be raised by DMII, HTN, Tumors, infections, and smoking
What is Hs-CRP and what does it effect?
Hs-CRP– high sensitivity C-reactive protein.
• Epidemiologic studies have shown that the relative
risk of future vascular events increases as the hs-
CRP concentration increases.
What is the value of Hs-CRP that is associated with CVD developing?
Values greater than 3 mg/L are associated with an increased risk for developing CVD
What Hs-CRP values are intermediate risk?
Between 1 and 3 mg/L are considered to be at intermediate risk
What Hs-CRP values are low risk?
Values less than 1 mg/L are associated with a low risk.
What are the markers of hemodynamic stress?
Natriuretic Peptide- NP
What is the precursor of BNP?
B-type natriuretic peptide (BNP) and its precursor, N-
terminal pro-brain natriuretic protein (NT-proBNP)
Where are BNP and its precursor are released?
from ventricular myocytes in response to pressure overload/stretch
What are the effects of NP?
Potent diuretic, natriuretic, and vascular smooth muscle relaxing effects
What is BNP levels correlated with?
BNP levels correlate with severity of HF and the degree of left ventricular dysfunction, as well as prognosis
What is used in screening and diagnosis of CHF?
Markers of hemodynamic stress-BNP and NT-proBNP
What is a symptom of CHF?
dyspnea
What are differential diagnosis of dyspnea?
• Readings >400 pg/ml indicate a 95% chance of CHF.
• Readings <100 pg/ml rule out CHF
Does BNP and NTproBNP have same values?
Use of BNP and NTproBNP are the same but have different values for normal/abnormal
What is BNP levels correlated with?
BNP levels correlate with NYHA classes and is prognostic in stages III and IV
What is ejection Fraction?
Ejection Fraction – Heart failure
Ejection Fraction- Amount of blood pumped out of the heart on systole
How is ejection fraction measured?
Measured as a %
What is the normal range of ejection fraction?
Normal is between 50-70%
What are the Various tests used to measure EF?
• Echocardiogram (Echo) - most widely used test
• MUGA scan
• CAT scan
• Cardiac catheterization
• Nuclear stress test
What is preserved ejection fraction (HFpEF)?
also referred to as diastolic heart failure. The heart muscle contracts
normally but the ventricles do not relax as they should during ventricular filling (or
when the ventricles relax)
What is reduced ejection fraction (HFrEF)?
also referred to as systolic heart failure. The heart muscle does not
contract effectively and less oxygen-rich blood is pumped out to the body
What can ECG detect?
• Arrhythmias
• Conduction disturbances
• Myocardial ischemia or infarction
• Metabolic disturbances that may result in lethal arrhythmias (e.g., hyperkalemia)
• Increased susceptibility to sudden cardiac death (e.g., prolonged QT interval).