lecture 7/8: regulation of calcium and phosphate balance
1/85
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
86 Terms
hydroxyapatite; contains calcium and phosphorus
what is the main crystalline salt of bone?
-form a crystal precipitate!
-we don't want that, so there are mechanisms of exchange
in a physiologic fluid, calcium and phosphtae
increases the number of sodium fast channels, hence easier depolarization
how does low calcium increase excitability of cells?
8.5-10.5
normal calcium range:
intestinal calcium absorption is less than calcium excretion, and the deficit comes from the maternal bones
how is there a negative calcium balance in pregnant women?
intestinal calcium absorption exceeds urinary excretion, and the excess is deposited in the growing bones
explain the positive calcium balance in growing children:
1,25-dihydroxycholecalcirerol
active form of vitamin D
ionized
-rest is bound to albumin (40%) or complexed with anions (10%)
the most abundant form of calcium:
-only calcium bound to albumin cannot be filtered
-only ionized calcium is biologically active
is calcium filtered? is calcium active?
-pH
-albumin: increased H+ binds to albumin, raising amount of ionized calcium
factors modifying ionized calcium
-decreases protein bound calcium
-no change in free ionized calcium
-decreased total calcium
how does hypoalbuminemia (cirrhosis, critical illness) impact calcium levels
-increased protein bound calcium, no change in free ionized
-increased total calcium
how does hyperalbuminemia (hypovolemia, high protein intake) impact calcium levels?
-increased pprotein bound, decreased free, normal total
how does alkalosis alter plasma calcium levels?
-increased protein bound calcium, normal free ionized calcium, increased total calcium
how does pregnancy alter plasma calcium levels?
phosphate
-major intracellular acid-base buffer
-uptake from gut is linear with diet levels
-regulation via urinary excretion
leads to increased binding of free calcium, therefore there is decreased free calcium
how does hyperphosphatemia affect calcium?
Insulin; contributes to refeeding syndrome
____ promotes phosphorus uptake into peripheral cells
FGF23
peptide produced by osteocytes
-negative regulator or serum phosphate via ability to inhibit Pi reabsorption in the kidney
2.5-4.5
normal serum phosphate level
-Ricketts, osteomalacia
hypophosphatemic disorders associated with excess production of FGF23
-AD: mutation in FG23
-X linked: excess FGF23 secondary to PHEX mutation
inheritance types of hypophosphatemic rickets
FGF23
_______ sometimes ectopically produced by slow-growing occult mesenchymal tumors, causing a hypophosphatemic paraneoplastic syndrome.
hyperphosphatemia and 1,25 dihydroxyvitamin Dd
production of FGF23 is increased by
FGF23
-inhibits 1,25-dihydroxyvitamin D, resulting in decreased phosphate absorption intestinally and renally
there is a calcium sensing receptor on the plasma membrane of chief cells
how do chief cells monitor calcium levels?
decreases transcription of prepro PTH as well as post translational processing
how does chronic hypercalcemia impact PTH production?
C terminal fragment
PTH derived fragment that is most represented in serum, has a longer half life
within seconds!
how fast does PTH respond to calcium levels?
magnesium
_______ has parallel, but less important effects on PTH secretion compared to calcium
DIRECTLY on bone and kidney
INDIRECTLY on intestine
what does PTH work on?
-increase 1-OHase, making more active vitamin D
-increase calcium reabsorption in the distal tubule
-decrease PO4 reabsorption in the proximal tubule
effects of PTH on the kidney
-indirectly: the increased vitamin D from the kidneys increase calcium and phosphate uptake
effects of PTH on the intestines
-increase reabsorption of mineralized bone, with increases serum calcium
-Phosphate will increase initially
effects of PTH on the bone
Bind to osteoblasts, which respond by activating osteoclasts to resorb bone-
how does PTH increase bone resorptionn?
hydroxyproline (collagen fragments) excretion
increased bone resorption is reflected by what excretion?
effects in the kidney!
what effect of PTH happens the quickest?
increased urinary cAMP, low phosphate
PTHs effect on the proximal tubule results in what finding?
NO!
-PTH increases intestinal Calcium absorption indirectly by stimulating 1,25 dihyddroxycholecalciferol in the kidney
are there PTH receptors in the intestine?
-PTH and vitamin D bind osteoblasts
-osteoblasts release M-CSF and RANK-L promoting osteoclastogenesis and osteoclast activity
-mineralization occurs over weeks once calcium becomes available from the exposed bone
how does PTH increase bone resorption?
androgens, estrogens
-thyroid hormone, GH, IGF, calcitonin, vitamin D
hormones promoting bone formation
PTH, cortisol, HIGH thyroid hormone, inflammatory cytokines
hormones favoring bone resorption
androgens, estrogens, calcitonin
hormones inhibiting bone resorption
increases calcium release
bone resorption's effect on calcium levels
NERF proteins
-urinary cAMP indicates PTH action
cAMP activation on _____ proteins in the proximal tubule results in decreased reabsorption of phosphate in response to PTH
PTH action
urinary cAMP indiicates
1 alpha hydroxylase
enzyme that converts 25, Vitamin D to its active form
-upregulated by PKA in the distal tubule in response to PTH, increasing calcium reabsorption
short term: increases bone resorption
long term: enhances mineralization
long term and short term effects of vitamin D on bone
-nucleus of osteoblasts (binding activates osteoclasts)
-GI tract
where are vitamin D receptors located
increase plasma calcium and PO4- so it can be used to promote bone mineralizaiton
what is the goal of Vit D?
vitamin D
a group of related secosteroids either derived from the diet or from metabolism of cholesterol
Ergocalciferol (Vitamin D2)
precursor of vitamin photochemically synthesized in plants
Cholecalciferol (Vitamin D3)
-form of vitamin D synthesized in skin in ressponse to sunlight
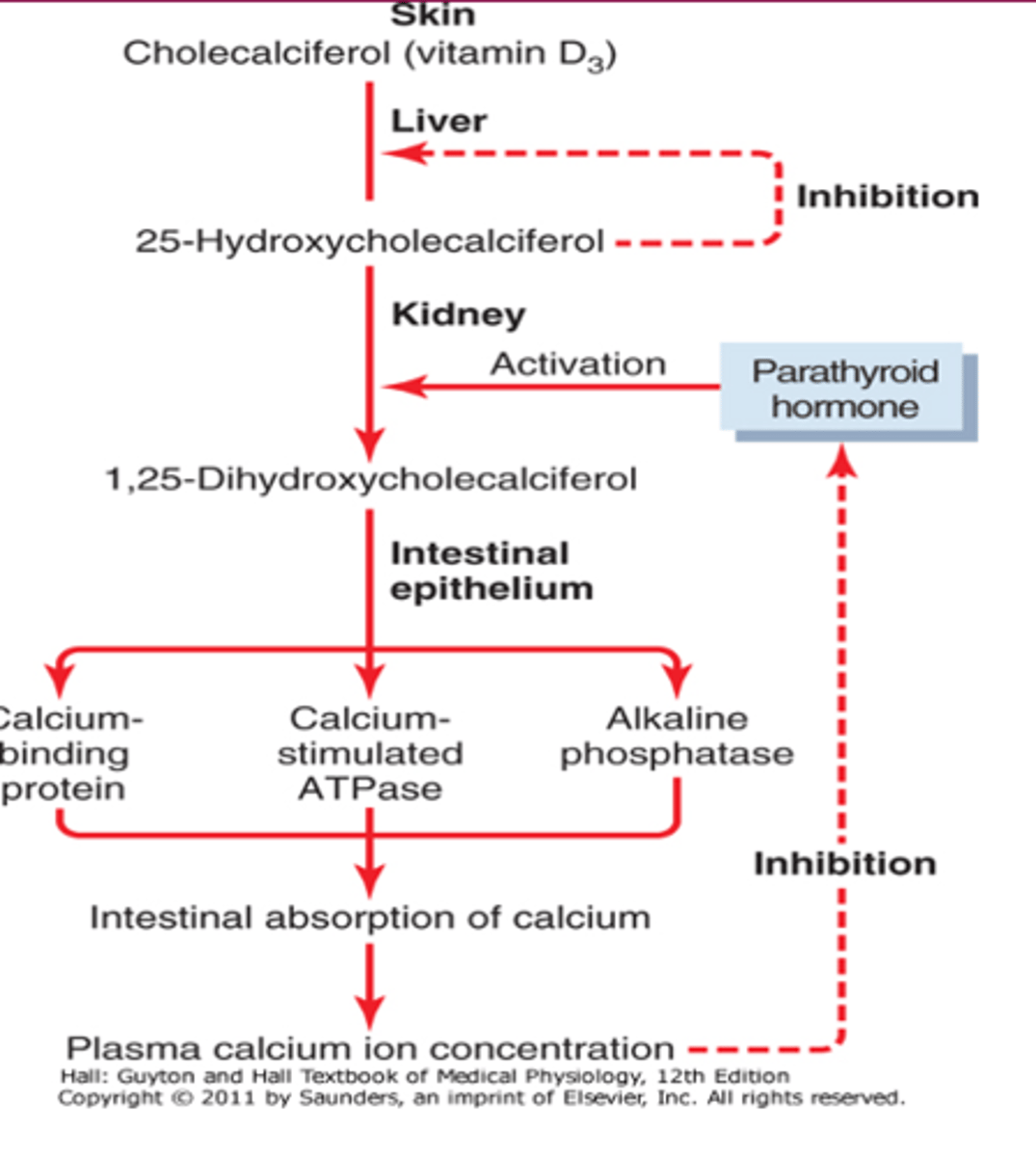
25-OH vitamin D made in the liver by 25-hydroxylase
when we measure vitamin D levels, this is what we measure
1,25-(OH)2 D synthesized by 1-alpha hydroxylase in the kidney
the active form of vitamin D
7-dehydrocholesterol; converted to D3 by UV light
precursor to Vitamain D3 (cholecalciferol)
conversion of calcidiol to calcitriol in the kidney by 1-alpha hydroxylase
primary regulatory step of vitamin D formation
-25-hydroxycholecalciferol on the liver
-1,25 hydroxycholcalciferol
negative feedback of vitamin D produciton
25-hydroxycholecalciferol stays relatively constant, regardless of D3 intake; represents negative feedback
why do we measure 25, Vit D to assess vitamin D status?
-decreased calcium
-increased PTH
-decreased phosphate
1 alpha hydroxylase activity is increased by
-increased 1,25 Vit D activates 24-OHase, which converts vit D to an inactive form
negative feedback regulator of 1,25 Vit D
FGF-23
_____________ represses 1a-hydroxylase activity to reduce phosphate absorption
-freely enters cells and binds to DNA receptor
signaling of Vit D
-stimulate calcium and phosphate absorption through intestinal brush border
-increases sodium-phosphate transporters in enterocytes
-increases epithelial calcium transporters
-increases calbindins
effect of vitamin D on the intestiinie
calbindins
Protein that transports Ca across osteoblasts to mineralizing (osteoid) side.
slightly increases reabsorption of calcium and phosphate
affect of Vit D on kidney
-interacts with osteoblast Vit. D receptors, causing increase in RANKL and M-CSF and hence resorption in the short-term. BUT, increases availability of both Ca++ and Phosphate, so lots of substrate for mineralization during bone formation
affect of Vit D on Bone
calcitonin
-works to lower plasma calcium, beginning only at calcium levels of 9.5 or higher
osteoclast
-bind up osteoclasts to decrease bone resorption to decrease serum calcium
what is the target cells of calcitonin
vitamin D
increases serum calcium and phosphate
-cause loss of calcium at the kidney
-reduces calcium absorption in the intestine
affect of cortisol on calcium:
decrease bone formation during remodeling-
-leads to OSTEOPOROSIS
long term effects of cortisol on bone
increased bone turnover
increased alkaline phosphatase is a sign of
yes! due to the increased filtered load of calcium
does PTH increase calcium excretion?
-decreased production of 1,25-dihyddroxycholecalciferol decreases calcium gut absorption
-kidney failure decreases calcium reabsorption
-causes increased PTH---> bone loss (osteomalacia)
-increased serum phosphate complexes free calcium, decreasing calcium
affect of chronic renal failure on calcium and bones
Secondary hyperparathyroidism
high PTHH, low calcium, high phosphate, VERY low vitamin D
tertiary hyperparathyroidism due to sustained secondary hyperparathyroidism
ESRD may also be called
primary hypoparathyroidism
-low PTH, low calcium and tetany , high serum phosphate, low urinary phosphate
Pseudohypoparathyroidism
Defective Gs protein in kidney and bone, which causes end-organ resistance to PTH.
Heterozygous inactivating mutation in the GNAS1 gene that codes for α-subunit of the stimulatory G protein
Pseudohypoparathyroidism type 1A (Albright hereditary osteodystrophy)
•Hypocalcemia and hyperphosphatemia occur (as in hypoparathyroidism), which are not correctable by the administration of exogenous PTH
-Circulating PTH levels are elevated
•Round face, short stature with a stocky habitus, brachydactyly, subcutaneous ossification, and dental anomalies, Developmental delay, obesity (early-onset), and relative macrocephaly
presentation of pts with pseudohypoparathyroidism
PTH-related peptide (PTHrP)
some malignant tumors secrete _________ resulting in hypercalcemia, hypophosphatemia, increased urinary pohsphate, decreased serum PTH
familial hypocalciuria hypercalcemia
AD mutation in calcium sensing receptor or downstream regulators
-increase the parathyroids setpoinnt for calcium, making parathyroids less sensitive to calcium
-decreased ionized calcium and increased PTH; secondary hyperparathyroidism
result of rickets and osteomalacia
calcipenic rickets
-vit D deficiency due to decreased 25-OH causing rickets
phosphotenic rickets
phoshapte transport defects, excessive FGF23 causing rickets
Secondary hypoparathyroidism
rare but seen in sarcoidosis