Module 5 NURS 2112: Bacteria vs. Viruses and Antivirals
1/47
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
48 Terms
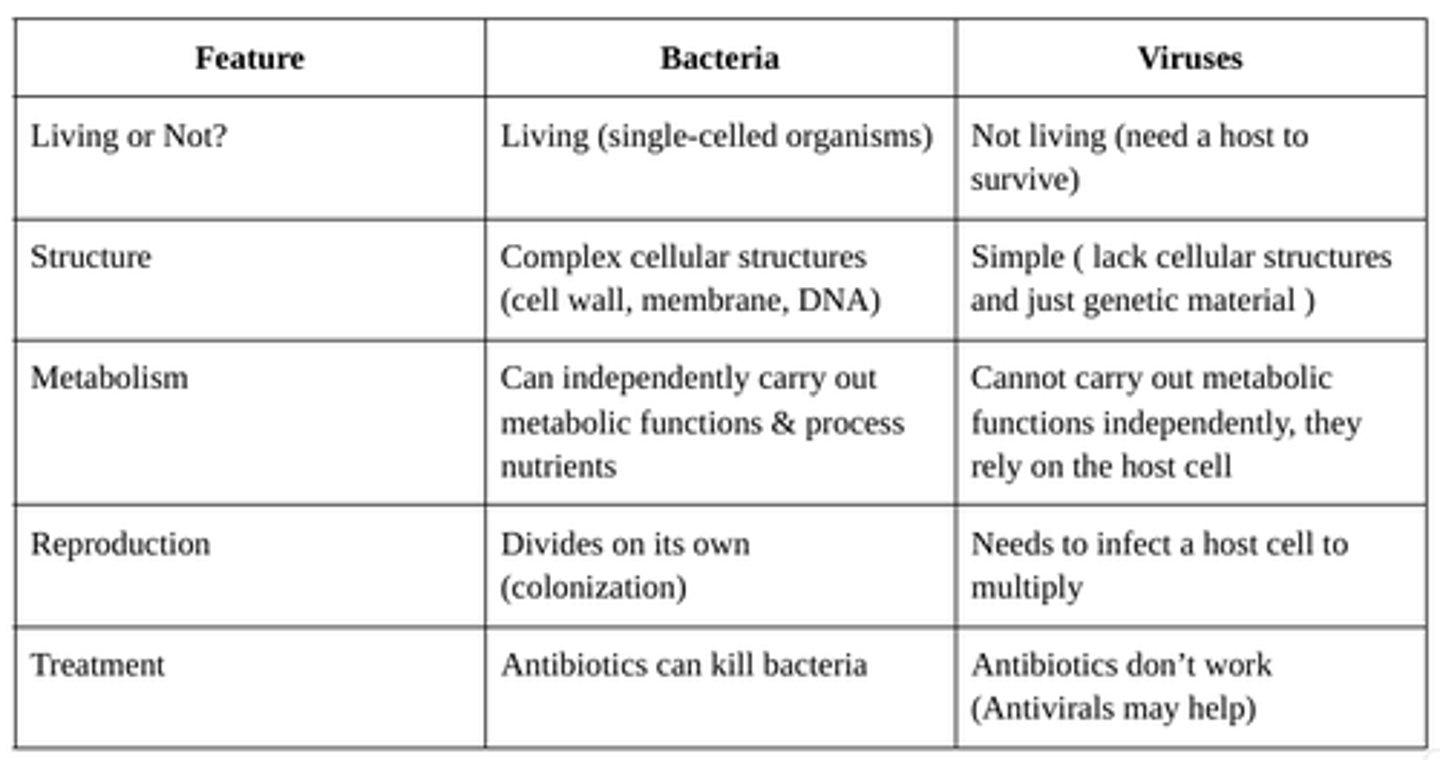
What is the difference between viruses and bacteria?
Bacteria are single-celled organisms that can live and reproduce on their own, with some being beneficial and others causing infections treatable with antibiotics.
Viruses, on the other hand, are much smaller, cannot survive or reproduce without a host, and require vaccines or antiviral medications for prevention and treatment.
virus
Viruses are tiny particles made of DNA or RNA surrounded by a protein coat, in some cases may be surrounded by a lipid envelope. Viruses are acellular (not living) because they have no cellular structure and cannot carry out metabolic processes on their own. I n order to reproduce, a Viruses must infect a host cell
How do viruses infect cells
1️⃣ Attach → The virus binds to a host cell using specific receptors.
2️⃣ Enter → It gets inside the cell by direct penetration, membrane fusion, or endocytosis.
3️⃣ Hijack → The virus takes over the cell to make more viral proteins
4️⃣ Release → New viruses are made and released, often killing the host cell.
5️⃣ Spread → The new viruses go on to infect other cells.
Why Are Viruses Hard to Kill
They live inside cells, so attacking them may also harm healthy cells. Antibiotics do not work on viruses (antivirals or vaccines are needed).
Retrovirus
A retrovirus is a type of virus that uses RNA instead of DNA. It has a special enzyme called reverse transcriptase that converts its RNA into DNA. The RNA is converted into DNA so the virus can insert itself into the host's DNA and hijack it for reproduction.
How do retrovirus work?
1️⃣ Infects a host cell.
2️⃣ Uses reverse transcriptase to turn its RNA into DNA.
3️⃣ Inserts viral DNA into the host’s DNA.
4️⃣ Uses the host cell to make more viruses.
For Example: HIV
HIVs genetic information is carried as RNA, and converted to DNA to attack the host's DNA.
How does our body fight viral infections
through a competent immune system that is healthy, strong against viral infections, as well as thorugh a well functioning immune system that will eliminate or effectively destroy virus replication.
Whta populations are at risk for not having a competent immune system against viruses?
Cancer patients: (especially those with leukemia or lymphoma)
Weakened immunity due to the disease or chemotherapy.
Transplant patients: They take medications to stop their immune system from attacking the new transplanted organ. These medicines weaken the immune system, making it harder to fight off viruses.
AIDS patients:
AIDs attacks the immune system, making it hard to fight infections.
what are antivirals
Antivirals are medicines that fight viruses by stopping them from growing or spreading in the body. Unlike antibiotics (which kill bacteria), antivirals do NOT kill viruses—they just slow them down so the immune system can fight them better.
How Do Antivirals Work?
1️⃣ Stop the Virus from Attaching (Inhibit Viral Attachment
Viruses need to attach to a host cell to infect it.
Antivirals block this attachment, preventing the virus from entering the cell.
2️⃣ Stop the Virus from Making Copies (Prevent Genetic Copying)
Viruses use the host cell to copy their genetic material (DNA or RNA).
Antivirals block this process, which stops the virus from multiplying.
3️⃣ Stop the Virus from Producing Proteins
Viruses need proteins to build new virus particles.
Antivirals block protein production, so the virus cannot spread
what do nurses do before giving antivirals
1) Check medical history, allergies, and current conditions.
2) Take vital signs and check nutritional status.
3) Look for drug interactions or contraindications
what patient education do you do with antivirals?
1) Do not mix with other medications without doctor approval.
2) Maintain good hygiene to prevent reinfection.
3) Antivirals do not cure infections but help manage symptoms.
4) Take the full course of medication as prescribed for best results.
Amantadine and Rimantadine
Therapeutic Classification: Antiviral (used for influenza A)
Pharmacological
Classification: Viral M2 Channel Inhibitor
How it Works: Blocks the M2 ion channel of the influenza A virus, preventing the virus from releasing its genetic material into the host cell.
Side Effects: dry mouth, sweating, bradycardia, insomnia, nausea, loss of appetite, lightheadedness
Foscarnet, Gancoclovir and Acyclovir
Therapeutic Classification: Antiviral (used for Cytomegalovirus)
Pharmacological Classification: Viral DNA Polymerase Inhibitor
How it Works: Blocks viral DNA polymerase, this enzyme is needed for the virus to copy its DNA. Therefore it prevents viral replication because without DNA replication, the virus cannot multiply.
Side Effects of Foscarnet: acute renal failure, seizures, nausea, vomiting, diarrhea, headache
Side Effects of Acyclovir: burning (when applied to skin), nausea, diarrhea, headache
Oseltamivir and Zanamivir
Therapeutic Classification: antiviral (used for influenza A and B)
Pharmacological Classification: Neuraminidase Inhibitor
How it Works: Blocks neuraminidase, an enzyme the flu virus needs to spread. Therefore, it slows the spread of the virus in the body, helping reduce symptoms and duration of illness.
Side Effects: nausea, vomiting, headache, diarrhea, dizziness
Acquired Immunodeficiency Syndrome (AIDs)
-IDS is the most advanced stage of HIV infection, where the immune system becomes severely weakened.
-It happens when HIV (Human Immunodeficiency Virus) destroys too many immune cells (CD4-T cells), making the body unable to fight infections and diseases.
How does AIDS Develop?
1️⃣ HIV Infection - The virus enters the body and slowly attacks CD4 T-cell (decreases helper T cells)
2️⃣HIV Progression - Over time, the immune system weakens if untreated.
3️⃣ AIDS Stage - CD4 T-cell count drops below 200 cells/mm³, and the body is vulnerable to severe infections and certain cancer
Human Immunodeficiency Virus (HIV)
HIV spreads through blood and body fluids (semen, vaginal fluids, breast milk).
It is mainly transmitted by:
1) Unprotected sex (vaginal, anal, or oral)
2) Sharing needles (drug use, accidental needle sticks in healthcare)
3) HIV infected mother transmits HIV to baby during birth or breastfeeding
how do you reduce HIV transmission
1) Using condoms lowers the risk of sexual transmission.
2) Needle exchange programs help prevent spread among drug users.
3) Medications for pregnant HIV infected women can prevent passing HIV to babies.
How do you kill HIV on surfaces
Heat (60°C for 10 minutes), disinfectants (bleach, alcohol, hydrogen peroxide) can kill HIV. Washing dishes and clothes normally also eliminates the virus.
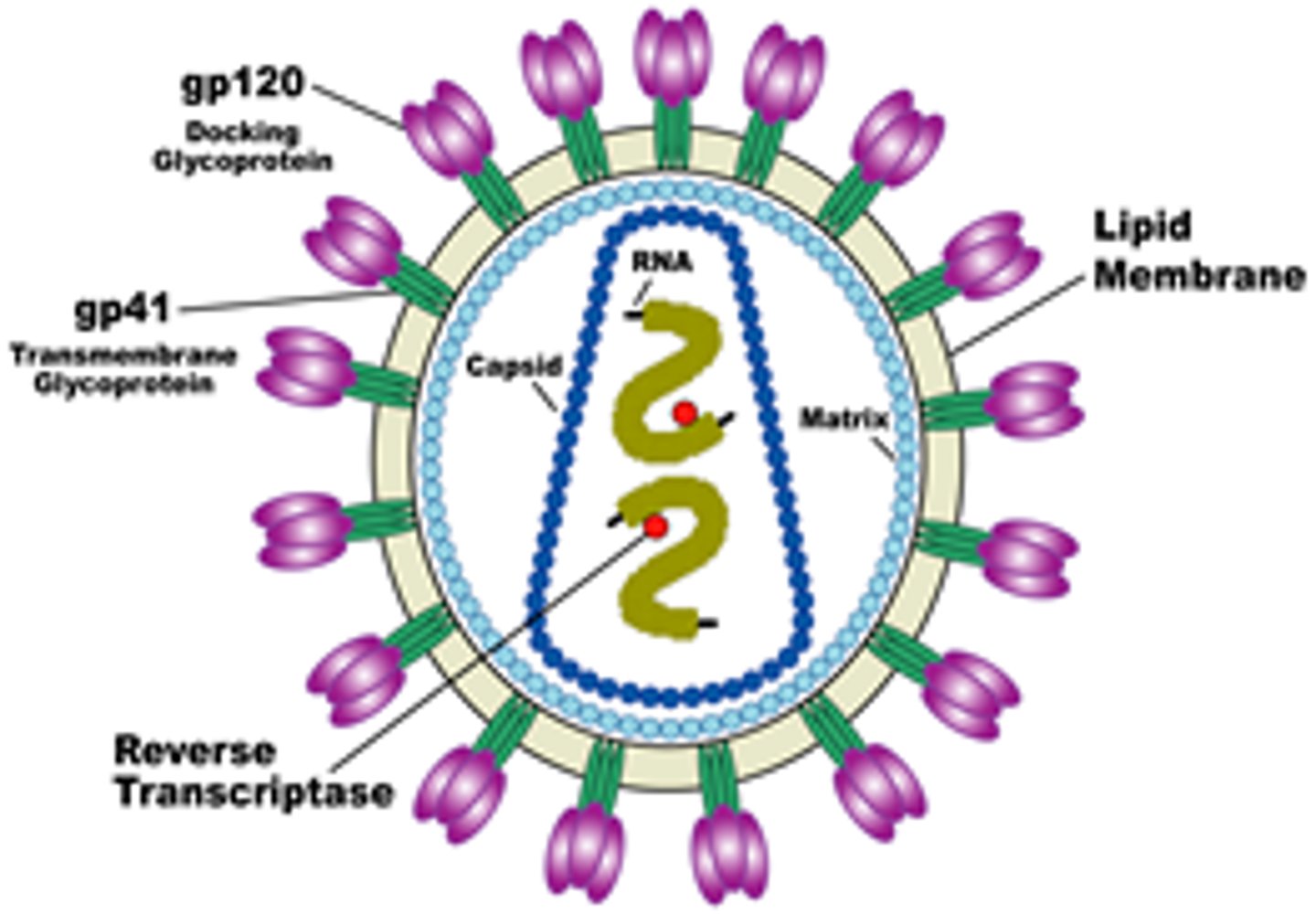
explain the structure of HIV
1) RNA (two strands) – The virus’s genetic material.
2) Enzymes (Reverse Transcriptase, Integrase, Protease) – Help the virus replicate.
3) Capsid (Protein Coat) – Protects the virus.
4) Membrane Envelope with Glycoproteins – Helps the virus attach to host cells.
how does HIV infect cells?
HIV cannot reproduce outside a host cell. Once inside, it uses the host’s machinery to make more viruses.
Steps of Infection:
1️⃣ HIV attaches to a host cell using its glycoproteins.
2️⃣ The virus enters the cell through a process called endocytosis.
3️⃣ Reverse Transcriptase converts viral RNA into DNA.
4️⃣ Integrase inserts viral DNA into the host’s DNA, allowing it to be copied when the cell divides.
5️⃣ The host cell produces new HIV particles, using Protease to form virus structures.
6️⃣ New HIV viruses leave the host cell and infect other cells.
Antiretroviral Drugs
Antiretroviral drugs (ARVs) are used to control HIV / AIDS and prevent it from multiplying in the body
ONLY USED FOR HIV/AIDS
They do not cure HIV but help control it, allowing people to live longer and healthier.
what are the classes of antiviral drugs
1) Nucleoside Reverse Transcriptase Inhibitors (NRTIs)
2) Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs)
3) Protease Inhibitors (PIs)
4) Fusion Inhibitor
5) Integrase Inhibitors
Nucleoside Reverse Transcriptase Inhibitors (NRTIs)
Block reverse transcriptase, preventing HIV from making DNA, which slows progression of the disease
Note: Monitor liver function and CBC values
Ex: Zidovudine (AZT)
Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs)
Directly inhibit reverse transcriptase, stopping virus replication
Note: can disrupt the actions of other drugs
Monitor liver function and CBC values
Example: Nevirapine
Protease Inhibitors (PIs)
Block the enzyme protease, which prevents virus from making proteins, therefore stopping the virus from maturing, infecting and spreading
Note: Expensive, Must be used with other retroviral to prevent resistance. Monitor liver and CBC values
Ex: Lopinavir
Fusion Inhibitor
Block the fusion between the viral and target cell membranes
(Blocks HIV from entering cells)
Note: Used in combination with protease inhibitors which potentiates the
effect of the protease inhibitor
Integrase Inhibitors
Target and inhibit integrase which is a viral gene that
inserts viral DNA in the DNA of the host
(Prevent HIV from inserting its DNA into the host's DNA)
Acute Viral Hepatitis
Hepatitis is liver inflammation, usually caused by viruses
Hepatitis A, B, C, D, E
Other viruses like Herpes (Cytomegalovirus, Epstein-Barr, Varicella-Zoster) can also cause hepatitis.
Extent of inflammation and necrosis depends on the person's immune response.
Phases of Acute Viral Hepatitis
-incubation period
-prodromal phase
-icteric phase
-convalescent phase
incubation period
No symptoms, varies by virus (2-7 weeks or 2-6 months).
Prodromal Phase (Before jaundice appears)
Flu-like symptoms: Tiredness, muscle & joint pain, loss of appetite and easily fatigued
Digestive issues: Nausea, vomiting, diarrhea, constipation.
Mild right-side abdominal pain.
Icterus Phase
-Jaundice appears (5-10 days after prodromal phase)
-Severe itching (pruritus).
-Liver tenderness.
-Jaundice (except in many Hepatitis C cases).
Convalescent Phase
recovery period
-Increased sense of well being
-Appetite returns.
-Jaundice disappears.
Hepatitis A
inflammation of the liver caused by the hepatitis A virus (HAV), usually transmitted orally through fecal contamination of food(raw shelfish) or water
Note: Many people have no symptoms and don’t realize they are infected.
Incubation period: 15-30 days
Treatment & prevention of Hepatitis A
1) No specific treatment – The body fights it off naturally.
2) Avoid alcohol & fatty foods to protect the liver.
3) Rest and eat healthy to recover faster.
4) Wash hands after using the toilet and before handling food to prevent spreading.
5) Most people recover fully in a few months.
Hepatitis B
inflammation of the liver caused by the hepatitis B virus (HBV), which is transmitted sexually or by exposure to contaminated blood or body fluids. It doesnt spread as easily as hepatitis A.
Incubation period: 2 to 6 months and poses more serious health risks than type A
How do you protect yourself from hepatitis B
vaccine
1) 3 doses (initial, 1 month later, and 6 months later).
2) Provides lifelong protection, no booster needed.
3) Available alone or combined with the Hepatitis A vaccine (Twinrix).
Hepatitis b long term effects
Most people recover from HBV and become immune for life.
Some become chronic carriers and can infect others.
The younger you are when you become infected, the more likely you are to become infected for life.
Carriers are at high risk of cirrhosis , liver failure, liver cancer and Some carriers may need a liver transplant in severe cases
treatment for chronic hepatitis B
No cure, but antiviral medications help control the virus and
Patients should avoid alcohol, rest, and eat a healthy diet.
Hepatitis c
inflammation of the liver caused by the hepatitis C virus (HCV), which is transmitted by exposure to infected blood; this strain is rarely contracted sexually. people wit alcoholic liver disease often have hepatitis C, but some healthy individuals can be chronic carriers
Long term effect of hepatitis c
HCV is the most common cause of chronic hepatitis, cirrhosis, and liver cancer.
Can lead to liver fibrosis leading to cirrhosis, end-stage liver disease and hepatocellular cancer
Treatment combines the antiviral drugs interferon and ribavirin.
hepatitis d
Delta Hepatitis. Secondary infection caused by a mutated hepatitis virus. Only develops in patients with Hepatitis B. Protect yourself by getting the hepatitis b vaccine because there is no specific cure or vaccine for this type!
d for drug attacks being at the highest risk
Hepatitis E
A virus spread via fecal-oral transmission (contaminated water) especially in developing countries. Pregnant women are most at risk for sever illness and there is no specific treatment for this kind.
chronic viral hepatitis
Caused by HBV, HCV, and HDV
Principal cause of chronic liver disease, cirrhosis, and hepatocellular cancer in the world
Chief reason for liver transplantation in adults
Symptoms of chronic hepatitis
1) Mild fever, loss of appetite, and fatigue.
2) Malaise (feeling of uneasiness or discomfort but unable to identify the exact cause)
2) Jaundice (yellow skin and eyes).
3) Nausea, vomiting → Dehydration → tachycardia, dry mouth, and skin changes.
4) Enlarged, tender liver.
treatment for chronic hepatitis
Interferons (Peginterferon): Help the immune system attack the virus.
Liver transplant: For severe cases where liver damage is irreversible.