Body Fluids Exam :)
1/176
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
177 Terms
CSF
CSF functions
-mechanical barrier to cushion brain and spinal cord for trauma
-supply nutrients to nervous system
-remove metablic waste
-provide lubrication of the CNS
CSF Menginges (layers)
-Dura Mater: outermost close to bone
-Arachnoid: middle
-Pia mater: innermost by neural tissue
*subarachnoid space is between arachnoid and pia matter where CSF is!!!!
CSF is produced by
choroid plexus cells and ependymal cells in the VENTRICLES
-reabsorbed by arachnoid cells
CSF amount
ADULTS: 140-170 mL and about 20mL is made per hour
NEONATES: 10-60mL
most common method to obtain CSF
-LUMBAR PUNCTURE
-collection needle between L3-L4 lumbar vertebrae (or 4-5)
-drips into collection tubes NEVER ASPIRATED
normal spinal fluid pressure
50-180 mmHg
-if normal about 20mL or less of CSF is taken
-but if pressure is high or low it is only safe to take 1-2mL
order of tube collection for CSF
1. chemistry/immunology (could have contamination or traumatic tap with more RBCs)
2. microbiology
3. hematology (cell count and diff)
4. if neeed, it's for serological studies
ALL TESTING IS STAT!!!!!!
indications for lumbar puncture
-infection like meningitis, encephalitis, syphilis
-CNS malignancies
-acute leukemia or lymphoma with CNS involvement
-demyelinating diseases like MS or Guillain-Barre syndrome
-subarachnoid hemorrhage
Normal CSF color
CLEAR!
Cloudy, hazy, turbid, or milky CSF
could be increased WBC, microorgansism, or increased protein
meaning meningitis if WBC or microorganism
increased protein means blood brain barrier disorder where proteins are allowed to enter CSF or CNS production of IgG
**turbidity only happens when >200 cells or RBCS >400
bright red CSF
fresh blood so hemorrhage from fractured skull or intracranial hemorrhage
bloody CSF
RBCs due to hemorrhage or traumatic tap
smoky CSF
RBCs due to hemorrhage before RBC lysis or traumatic tap
xanthochromic CSF (yellow)
Hgb: lysed RBCs from traumatic tap or an OLD hemmorhage
Bilirubin: RBC breakdown and elevated serum bilirubin
Carotene: increased dietary levels
Protein: blood-brain barrier or CNS production of IgG
Melanin: meningeal malignant melanoma
clot or pellicle CSF
-increased fibrinogen from traumatic tap, subarachnoid block, tuberculosis meningitis
-protein from bb barrier or CNS production of IgG
oily CSF
x-ray contrast dye
greenish CSF
myeloperoxidase meaning PURULENT FLUID
viscous CSF
-caspular polysaccharide meaning cryptococcus
-mucus from mucin-producing metastatic carcinoma
fatty CSF
fat from fat embolism
Xanthochromia
supernatant of CSF is
-YELLOW: conversion of oxyhemoglobin to unconjugated bilirubin
-PINK: very slight oxyhemoglobin
-ORANGE: heavy hemolysis
*a yellow tint is present in supernatant when a small amount of CSF is centrifuged
*SUGGESTS SUBARACHNOID or intercranial hemorrhage
-usually a breakdown of RBCs is the cause so color depends on quanitity and length of time they RBCs have been in CSF
-could also be caused by elevated serum bilirubin, carotene, increased protein, melanoma pigment, immature liver (infants)
blood CSF: traumatic or subarachnoid hemorrhage?
-hemorrhage will be throughout all tubes whereas traumatic will only be in the first tube and decreasing in the rest
-blood may only clot in traumatic tap
-xanthochromic with HEMORRHAGE, supernantant is clear in traumatic tap
-RBCs engulfed by macrophages is hemorrhage
-iron-laden macrophages (RBCS engulfed by macrophages break down to form dark purple/black pigment within macrophage) ONLY IN HEMMORHAGE
Cell Counts in CSF
-need to be testing within 1 hour of collection (because cells lyse and disintegrate after 60 minutes)
-acetic acid dilution lyses RBCs to better count WBCs
-methylene blue dilution stains WBCs for easier differentiation
# cells count total x dilution / # squres x volume of 1 square
NORMAL:
-WBC: 0-5 for adults; 0-30 for newborns
-no RBCs ever!
Cytocentrifugation of CSF
-differentiation of cells in body fluids
-allows for separation of cells from the medium to collect a representative sample with an uncrowded monolayer
-WRIGHT GIEMSA then used
1. cuvette
2. filter paper
3. slide
4. clip
5. centrifuge
-filter paper absorbs fluid while the cells are forced onto the slide
ALBUMIN CAN BE ADDED before the sample is run to the cuvette to help the cells stick to the slide (increased yield) and decrease distortion!!!!!
-cytocentrifuge body fluid slide can have accentuation of lobulation, peripheral localization of lobes, accentuation of nucleoli, irregular blebs or projections, vacuoles, or central concentration of granules
CSF differential
-main cells are lymphocytes and monocytes (mononuclear)
-technically any neutrophil is bad but a small # can technically be present bc of contamination usually
LYMPHS: 60 +/- 20% in adults; 20 +/-15% in neonates
MONO/MACRO: 30+/-15% adults; 70 +/20% neonates
NEUTROPHILS: 2+/-4% adults; 4+/-4% neonates
Neutrophilia in CSF
-Meningitis (bacterial, early viral, early tuberculous, amebic, aseptic)
-CNS trauma, cerebral infarct, brain tumor, spinal anesthesia, cerebral abcess, etc.
Lymphocytosis in CSF
-meningitis (viral, sometimes bacterial, tuberculous, sphylitic, leptospiral, fungal, parasitic)
-polyneuritis
-CLPDs!!!
-MS or Guillain-Barre Syndrome!!!
Monocytosis in CSF
-tuberculous, chronic, partially treated bacterial, viral or fungal meningoencephalitis, fungal, leptospiral, toxoplasma
-brain abscess, CNS hemorrhage, MS, CNS malignancy
Eosinophils in CSF
-never normal
-parasitic infections, fungal infections, shunts/meds
Basophils in CSF
-never normal
-inflammatory, parasitic, seizures, shunts, CML
Reactive Lymphs in CSF
-can be seen in viral infections or viral meningitis
plasma cells in CSF
-not normal but in MS, lyme disease, neurosyphilis, viral meningitis, herpes encephalitis
CSF lining cells in CSF
-ependymal cells and choroid plexus cells
-can look like maliingant cells!!
-sometimes can be normal
-rare in lumbar punctures, more common in ventricular or cisternal punctures
-can be found with traumatic brain injury, surgery, shunts, etc.
CSF macrophages with erythrophagocytosis
-monocytes can appear in the CSF 2-4 hours after RBCs
-common in HEMMORHAGE
-macrophages and monocytes are the same thing at mayo
CSF macrophages -hemosiderin
macrophages may have hemosiderin granules (dark purple/black granules)
-or hematoidin crystals
-from breakdown of RBCs
Nucleated RBCs and Immature Granulocytes
-sign of BM contamination
-caused by traumatic tap and specimen should be recollected
Bacteria in CSF
-not unusual especially when WBC or neutrophils are high
-bacteria vs stain precipitate is important
-can be intracellular or extracellular but always uniform in size
-stain precipitate is always extracellular and varies in shape and size
-REPORT AS INTRA OR EXTRACELLULAR
Yeast in CSF
-cryptococcus neoformans loves the CNS!!!
-encapsulated budding yeast or hyphae can be seen on slide
Malignant cells in CSF
-individually or in clusters
-can look like mesothelial or lining cells but mesothelial cells are NOT FOUND IN CSF
-ALL is the most common acute leukemia to go to CSF
-lymphomas could be seen and they happen without other organ involvvement and can look like large and small lymphs and tend to appear in clusters based on type of lymphoma. NUCLEI is cleaved and primennt nucleoli!
-metastatic carcinoma cells can be seen coming from lung, breast, etc, or a melanoma from the brain
primary CNS malignancies include
-high grade astrocytomas
-ependymomas
-medulloblastoma
-retinoblastoma
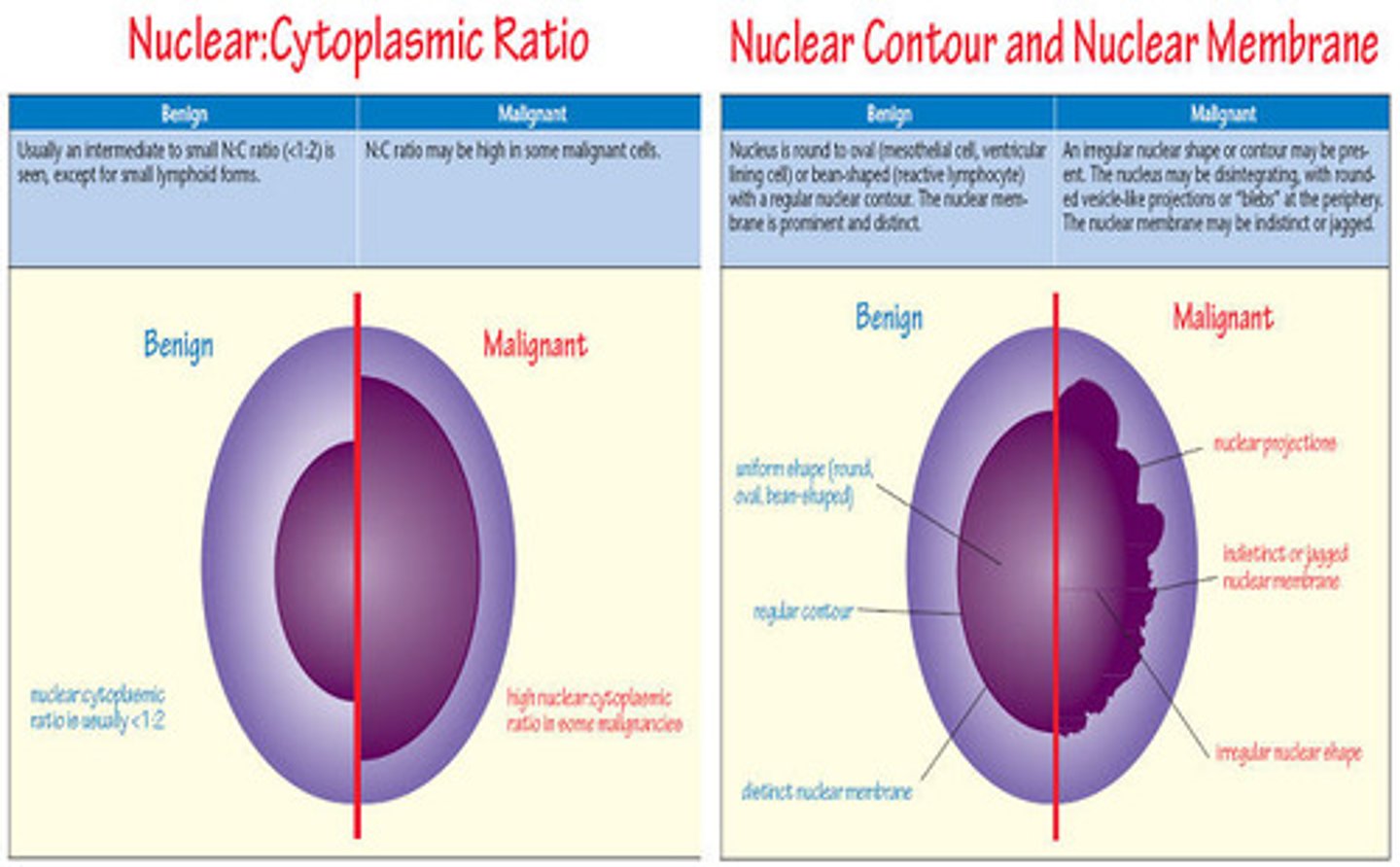
MALIGNANT CELLS LOOK LIKE:
-fused cell walls
-nuclear irregularities
-multinucleated cells
-occurs in clusters or singles
-bizarre appearance
Protein in CSF
-very little is normal and is mostly albumin (could be albumin, transferrin, or transthyretin), fever fibrinogen
-NORMAL: 15-45
-elevated causes
*meningitis, hemorrhage, traumatic tap, tumors, GB syndrome, CNS producing IgG, degeneration of neural tissue, CNS malignancy
((NEVER FLUID LEAKAGE!, this leads to lower i think)
-decreased causes
*leukemias, brain swelling, CSF leak or rapid production, hyperthyroidism
damage to blood brain barrier will result in
protein fractions similar to that in serum
*MM or other disease that stimulate immunocompetent cells in the CNS will have increased IgG
IgG assessed using serum and CSF levels
CSF/serum albumin index
-blood brain barrier integrity
-<9 INTACT
-9-14 minimal impairment
-15-100 severe impairment
->100 complete breakdown
IgG index
-evaluates IgG synthesis WITHIN CNS
-<0.77 means IgG production
electrophoresis in CSF
-used to detect oligoclonal bands
-extra bands in the GAMMA region that indicate IgG production resulting in inflammation of the CNS
-IN CSF but serum
-If oligoclonal bands in CSF not serum it means MS, encephalitis, neutrosyphilis or GB syndrome, can be present in some lymphoproliferative disorders IN BOTH THE SERUM AND CSF!!!
myelin basic protein
used to monitor MS patients because this demonstrates destruction of myelin sheath which protects neurons
Glucose in CSF
-glucose crossing BB barrier
-represents plasma glucose concentrations 30-90 minutes before collection
-NORMAL: 60-70% of plasma glucose levels so like 40-70
ELEVATED
-bloody tap, hyperglycemia (not a big deal)
LOW
-more diagnostic for meningitis (bacteria eating glucose) or hypoglycemia
-represent defective BB barrier and increased glycolysis
lactate in CSF
-diagnose meningitis
->35 means bacterial meningitis
->25 in fungal and tubercular meningitis
-<25 in viral meningitis (NORMAL!!!)
-good way to monitor effectiveness of tx since lactate levels stay high until meningitis is resolved
-other causes of increased could be in conditions that destroy tissue in CNS leading to less O2 or hypoxia
*increased intracranial pressure, trauma, seizures, intracranial hemorrhage, brain abscess
*usually high lactate leads to low glucose findings too
microbiology in CSF
-gram stain, culture, india ink prep, acid fast stain, latex agglutination for strep, e.coli, pneumiae, neoformans, etc.
serology in CSF
-neurosyphilis
-VDRL (venereal disease research laboratories) method
-+ confirmed using FTA-ABS test
LAB STUFF
Hemocytometer calculation
# cells x dilution / # squares x hxwxd
synovial fluid reference ranges
-TNCC: <150 microliters
-neutrophils <25%
-lymphocytes <75%
-monocytes <70%
pleural, pericardial, and peritoneal fluids
-TNCC <500 microliters
-neutrophils <25%
SEROUS FLUIDS LESSON
serous fluid is
pleural, peritoneal and pericardial (PPP)
pleural fluid
-fluid around the lungs
-pleural cavity (between chest wall and outside of lung) usually has some fluid
peritoneal fluid
-fluid around stomach or abdomen
-peritoneal cavity (inner abdominal wall and outer organ wall) usually has some fluid
pericardial fluid
-fluid around the heart
a single layer of mesothelial cells is what
lines these cavities!
two membranes
-parietal membranes: lines cavity wall
-visceral membranes: covers the organ
SEROUS FLUID: between parietal and visceral layers (production and absorption is usually equal)
serous fluids are formed as
ultrafiltrates of plasma and provide lubrication for organ movement
formation and absorption of serous fluids is controlled by
-hydrostatic and colloidal (osmotic) pressure
fluid formation is controlled by
-permeability of capillaries
-hydrostatic pressure in capillaries
-oncotic or colloidal pressure produced by plasma protein in capillaries
-absorption of fluid in lymphatic system
effusion
buildup of fluid due to a disruption in hydrostatic or colloidal pressures or in formation vs absorption
primary causes of effusions
-Increased hydrostatic pressure (CHF)
-Decreased oncotic/colloidal pressure (hypoproteinemia)
-Increased capillary permeability (inflammation&infection)
-Lymphatic obstruction (tumors)
physicians usually diagnose increased amounts of serous fluid based on physical exams or using
-radiographic imaging, ultrasound, echocardiograms
indications for needing a needle aspiration
-infection, malignancy, trauma, pulmonary embolism, collagen vascular diseases, GI diseases, cardiovascular diseases
collection of serous fluid
-sterile needle aspiration
PLEURAL FLUID: thoracentesis
PERITONEAL FLUID: paracentesis
PERCARDIAL FLUID: pericardiocentesis
sample amount
~50-100 mL
1. anticoagulated for hematology
2. sterile for microbiology
3. heparinized for chemistry
4. larger volume for cytology
STAT testing!
If the fluid is transudate
no further testing is needed usually
transudate vs. exudate
TRANSUDATE:
-effusion because of a systemic disorder that affects regulation of fluid filtration and reabsorption
-fluid that has been extruded through tissue like in CHF or NEPHROTIC SYNDROME
EXUDATE:
-effusion that is localized or directly involves membrane cavity
-fluid that deposits in or on surface of tissues because of INFECTION, MALIGNANCY, INFLAMMATION, SYSTEMIC LUPUS ERYTHEMATOSUS
lab testing transudate vs exudate
TRANS:
-pale yellow/clear
-no clotting
- <1000 WBCs
- <3g protein (<50% serum)
-fluid: serum protein ratio <0.5
-specific gravity <1.015 (hypoosmotic)
-fluid: serum lactate dehydrogenase ratio <0.6
EXUDATE:
-cloudy
-possible clotting
->1000 WBC cells (think infection so cloudy and lots of cells)
-protein >3g or >50% of serum
-fluid: serum protein ratio is >0.5
-specific gravity >1.015
-fluid: serum lactate dehydrogenase ratio >0.6
PLEURAL FLUID COLORS
-clear/straw colored: transudate, no further testing
-cloudy, purulent: infectiion, empyema (pus in body cavity)
-bloody: traumatic tap, trauma, infarction, malignancy
-greenish/turbid: rhuematoid arthritis
-milky, yellow-bloody: chylous effusion
-milky or green metallic sheen: pseudochylous effusion
-brown: rupture of amebic liver abscess
PERITONEAL FLUID
-clear, pale yellow: cirrhosis
-cloudy/turbid: bacterial peritonitis, pancreatitis, malignancy
-green/brown: biliary tract disease or ruptured bowl
-bloody: trauma, pancreatitis, intestinal infarction, malignancy
-milky: chylous or pseudochylous ascites
PERICARDIAL FLUID
-clear,pale yellow: normal transudate
-cloudy, turbid: infection, malignancy
-bloody: cardiac puncture, tumor, tuberculosis
-milky: lymphatic drainage
Lab testing of serous fluids
-gross exam, cell count and diff, gram stain, cytology
-pleural fluid you usually also do a fluid:serum protein ratio and a fluid: serum lactate dehydrogenase ratio and a cholesterol test
*specialized testing includes tumor markers, pH, enzyme studies, flow cytometry
normal counts for serous fluids
-TNCC: (total nucleated cell count) <500 cells/uL
-Neutrophils <25%
slide prep
cytocentrifuge to concentrate the sample and then stain with wright giemsa
neutrophils in serous fluid
-bacterial infection, pancreatitis, pulmonary infection
lymphocytes in serous fluid
-can be small, large or reactive
-tuberculous effusion, viral infection, LYMPHOMA, autoimmune disorder, CHF, nephrotic syndrome, chylous effusion, cirrhosis
monocytes/macrophages in serous fluid
-common in serous fluid
-macrophages are large, more irregular, have more cytoplasm and contain more vacuoles and phagocytosed material
signet ring cels
-phagocytic macrophages with a large vacuole that flattens the eccentric nucleus
-can be benign or malignant
mesothelial cells in serous fluid
-mesothelial is normal lining of serous fluid
-large cells 15-30 microns
-low N:C ratio
-abundant cytoplasm
-mononuclear or multinucleated
-nuclear membrane is SMOOTH and round/oval
-up to 3 small nuclei
-cytoplasm light gray to deep blue
-cytoplasmic vacuoles possible
*during inflammation, they become pleomorphic occuring singles, flat sheets, or in 3D clusters
microorganisms in serous fluid
-intracellular vs extracellular!!!!!
-yeast forms of fungi are most common to see
LE cells in serous fluid
-phagocytic cell (neutrophil or monocyte)
-has engulfed the nucleus of another neutrophil!!!!
-suspicous for SYSTEMIC LUPUS ERYTHEMATOSUS
-may be present in other autoimmune disorders though
malignant cells in serous fluid
-large to giant
-HIGH N:C ratio
-IRREGULAR nuclear borders
-prominent nucleoli
-irregularly clumped chromatin
ADENOCARCINOMA and small cell carcinoma cells are most common
lymphoma cells in serous fluid
-moderate to large
-irregular nuclear membrane with partially clumped chromatin
-small to prominent nucleoli
blasts in acute leukemias in serous fluids
-look like blasts in BM or PBS
-larger cells with high N:C ratio and fine nuclear chromatin
Pleural Fluid
- CHOLESTEROL >60 is exudate
- SERUM CHOLESTEROL RATIO: >0.3 is exudate
- serum total bilirubin ratio: >0.6 is exudate
-normally pale yellow to clear
-turbid: infection, TB, rheumatoid arthritis
-bloody: hemothorax, injury, membrane damage from malignancy (hemorrhagic exudate), traumatic aspiration
hemothorax vs hemorrhagic exudate
if hematocrit of the pleural fluid is >50% of the circulating blood hematocrit it is HEMOTHORAX meaning it is coming from an injury to the membrane = traumatic
if its <50%, its a chronic disease effusion that has some blood and increased pleural fluid *hemorrhagic*
Chylous vs pseudochylous effusions
CHYLOUS:
-thoracic duct leakage
-lots of TRIGS >100 mg/dL
-milk white
PSEUDOCHYLOUS:
-bc of chronic inflammation
-high CHOLESTEROL
-milky GREEN
-trigs <50!
pleural fluid other lab testing
-glucose should be similar to plasma levels (if low indicates RHEUMATOID or PURULENT infection)
-pH = 7.6 (<7.3 need chest-tube drainage and antibiotics; <6 means esophageal rupture)
-amylase: elevated means pancreatitis, esophageal rupture, malignancy
-NORMAL protein: 1-2 g/dL
-cell count <100 cells is normal
*few RBCs should be there
-antinuclear antibody (ANA) or rheumatoid factor (RF)
-cea = carcinoembryonic antigen (malignancy)
pericardial fluid more info
-normally pale yellow/clear
-turbid means malignant or infection
-blood usually caused by malignancy
-can be milky due to chylous or pseudochylous
pertioneal fluid more info
-accumulation of peritoneal fluid = ASCITES!!!!
-caused by hepatic cirrhosis, nephrotic syndrome, bacterial infection, ruptured appendix, malignancy
-COLOR: yellow and clear
-green if bile present (confirmed with bilirubin)
-ANC (absolute neutrophil count): >250-500 or 50% of total WBC count is peritonitis = INFECTION (cirrhosis can also have high white count but neutrophils are <50% i think)
peritoneal lavage
-saline introduce and then reaspirated
-elevated cell counts means intra-abdominal bleeding or trauma
malignancies of peritoneal fluid are most likely of
ovarian or GI origin
lab testing in peritoneal fluid
-serum to ascites albumin gradient: >1.1 means transudate of hepatic origin (<1.1 means exudate)
-CEA or CA125 = malignancy
-glucose is low in tubercular peritonitis and malignancy
-amylase increased in pacreatitis or GI perforations
-alkaline phosphatase: increased in intestinal perforations
SYNOVIAL FLUID LESSON!