Intrapartum
1/97
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
98 Terms
Theories of Labor
Uterine distention, increasing uterine pressure
Aging of placenta
Increased sensitivity to Oxytocin (normal hormone that produces breast milk & induces labor)
Changes in barometric pressure --> more L&D's
Changes in hormonal concentration:
Estrogen increase
Progesterone decreases
What are early signs and symptoms of impending labor?
1. Lightening: (baby dropping) fetus descends into the pelvic inlet (engagement).
Pressure is then moved from the pressing up against the diaphragm to the lower abdominal area causing:
leg cramps, increased pelvic pressure, venous stasis, urinary frequency, increased vaginal secretions.
2. Braxton-Hicks Contractions: irregular intermittent contractions; may become uncomfortable ((False contractions/labor)).
3. Cervical changes: softening (ripening)
4. Bloody show: cervical secretions mixed with some blood from ruptured capillaries; mucus plug is expelled.
5. Ruptured Membranes: occurs in 8-10% of women prior to labor; 80% will go into labor within 24-48 hours.
6. Sudden burst of energy
7. Others: weight loss, back ache, indigestion, diarrhea.
What are the components of true labor?
Presence of Bloody Show:
pink mucus
Contractions:
regular pattern
interval shortens
intensity increases
duration increases
starts from back to front
intensified by walking
Cervix:
change in dilation and effacement
***WHAT DETERMINES TRUE LABOR IS DILATION OF THE CERVIX AND REGULAR CONTRACTIONS!!!
What are the components of false labor?
No Bloody Show:
brown mucus (old blood)
Contractions:
irregular pattern
no change in intervals
no change in intensity
stays in the front
not changed by walking
Cervix:
no change
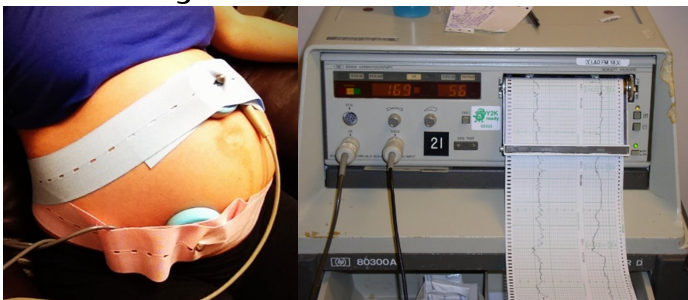
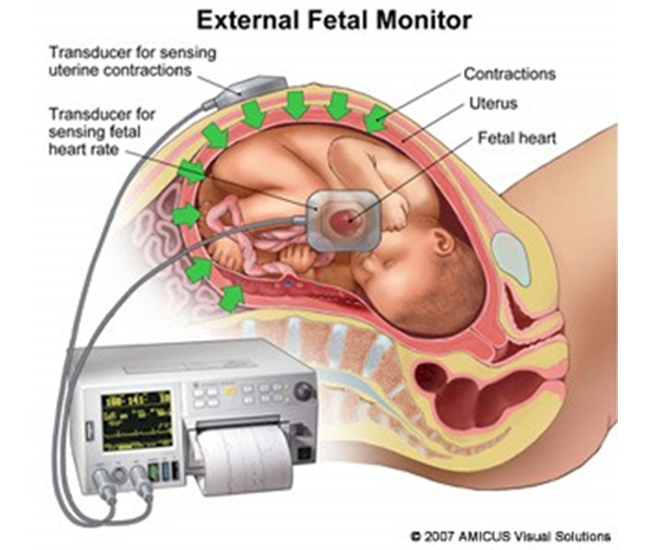
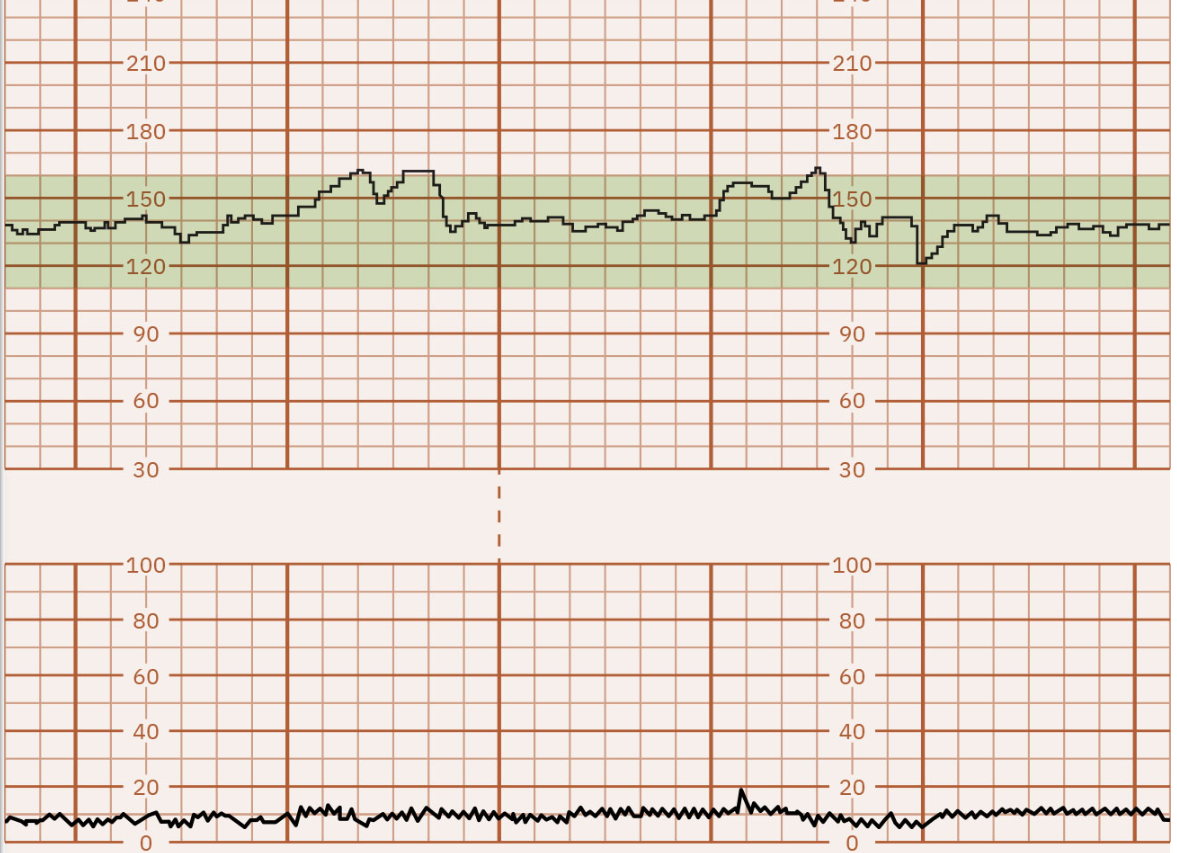
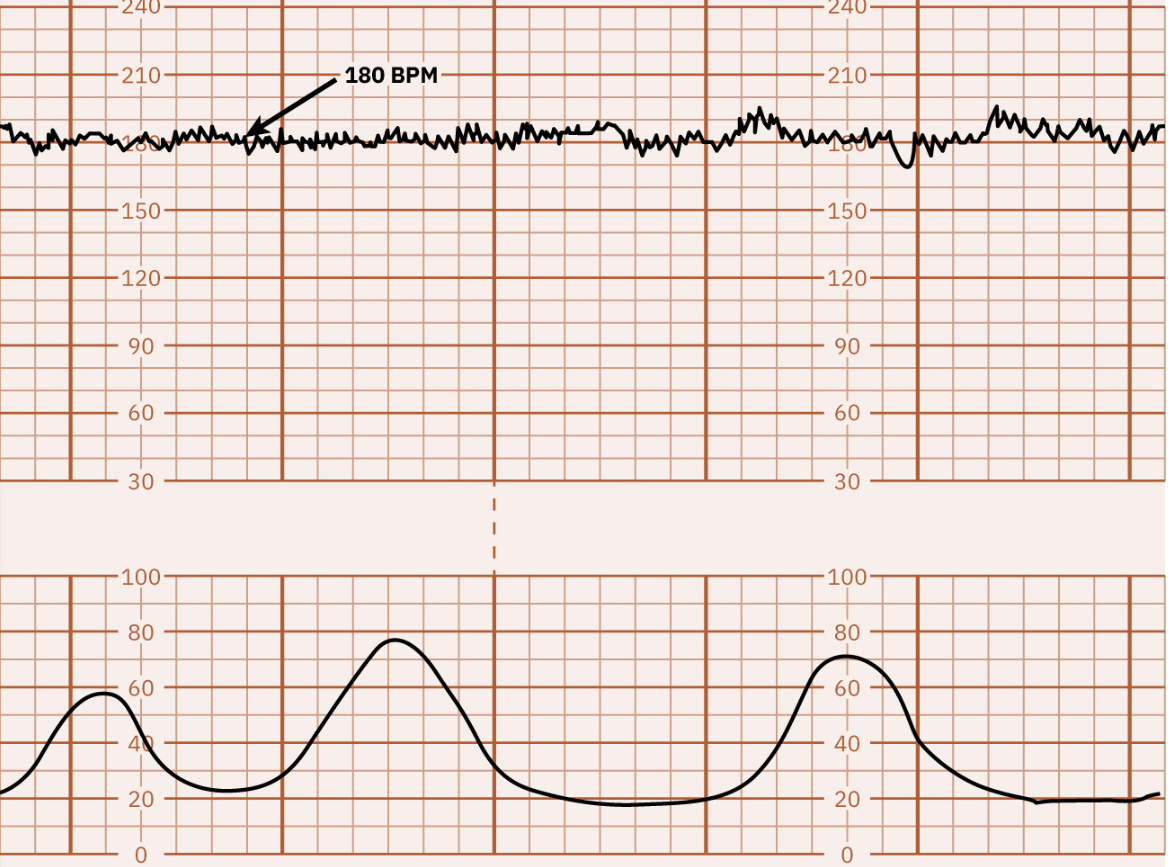
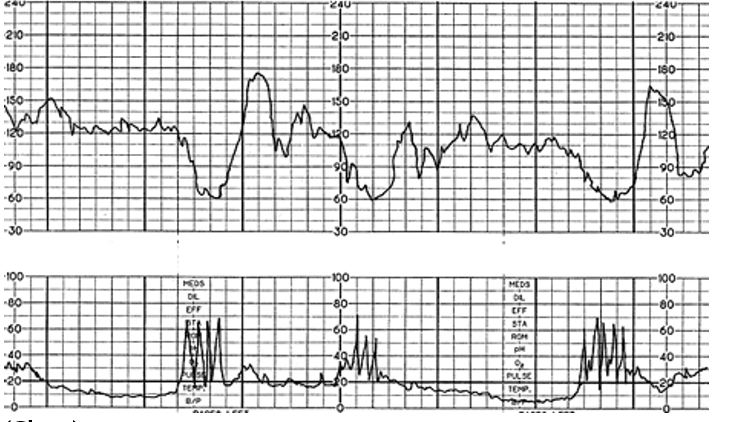
Electrical Fetal Heart Monitoring is…
Commonly used for tracking how well the baby is doing within the contracting uterus and for detecting signs of fetal distress.
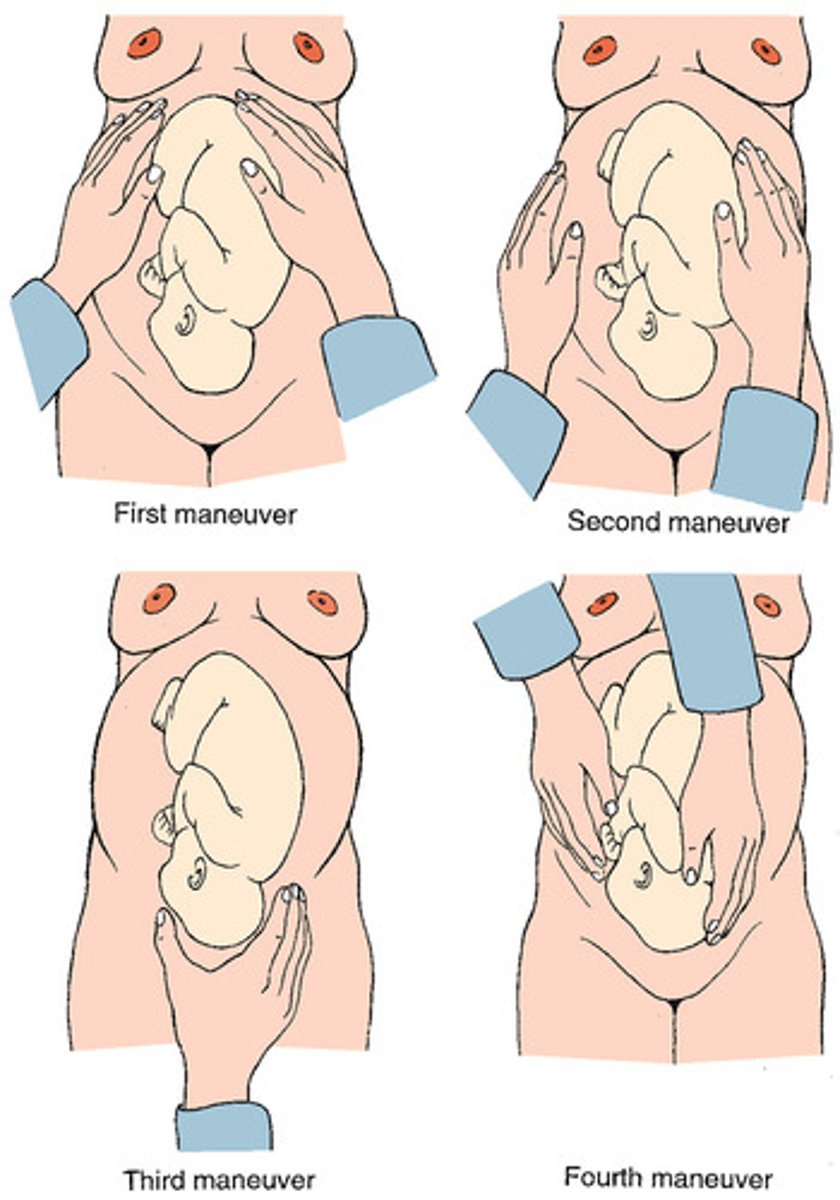
Leopold's Maneuver
What does the external fetal monitoring strip tell us?
Identifies baseline of fetal HR.
Determines whether there are accelerations or decelerations from the baseline.
Identifies patterns of uterine contractions.
Correlate accelerations & decelerations with uterine contractions.
With this, we can determine if the recording is reassuring/reactive, non reassuring/nonreactive, or ominous!
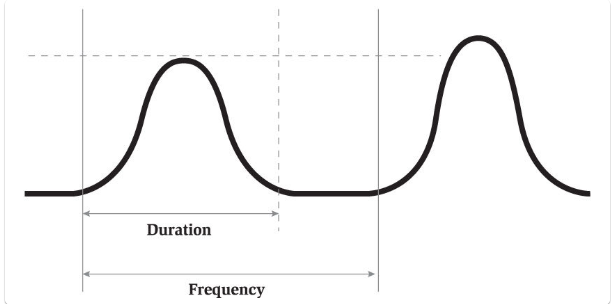
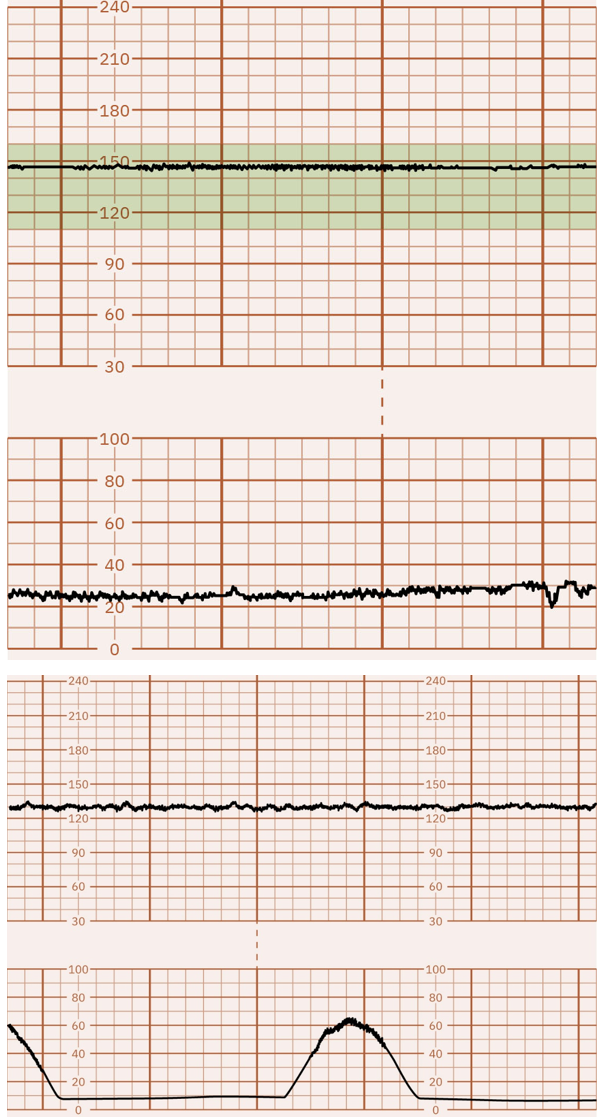
Segments of Contractions
Frequency: how often contractions come in minutes (from start of contraction to start of another); a range; increases if progressing.
Duration: length of contraction; a range (from the start of the contraction to the end of that contraction)
Intensity: how hard/strong contraction is (not accurate on external monitor--usually just ask momma—pain scale; feeling the fundus)
If there is minimal/absesnt variability on the strip, the baby could be sleeping, so you will give momma some…
SUGAR
Normal Fetal HR Range
110-160 bpm
Determine Baseline of Baby's HR
1. Average Fetal HR that occurs during a 10 min segment.
2. Excluding periodic rate changes.
3. Excluding time during a contraction.
What is variability?
Small up & down fluctuations.
Want in a healthy baby.
Moderate Variability means a…
Well developed, well oxygenated fetus, and a good sign for fetal well being.
Absent or Minimal Variability is caused by…
Fetal Academia Secondary to Placental Insufficiency
Cord Compression
Preterm Fetus
Maternal Hypotension
mom is not well hydrated (Ex: bottoming out after an epidural)
Uterine Hyperstimulation
uterus is contracting too often → not enough oxygen going to baby.
Placental Abruption
placenta is pulling off the uterus.
Fetal Dysrhythmia
Marked Variability
More than 25 beats of fluctuation in the FHR baseline.
Usually caused by:
Cord Prolapse or Compression
Maternal Hypotension (mom is not well hydrated.)
Uterine Hyperstimulation/Tetonic—hard & stays hard (too many contractions, too close & uterus needs a break)
Placental Abruption—(placenta pulls away from uterus - no blood or O2)
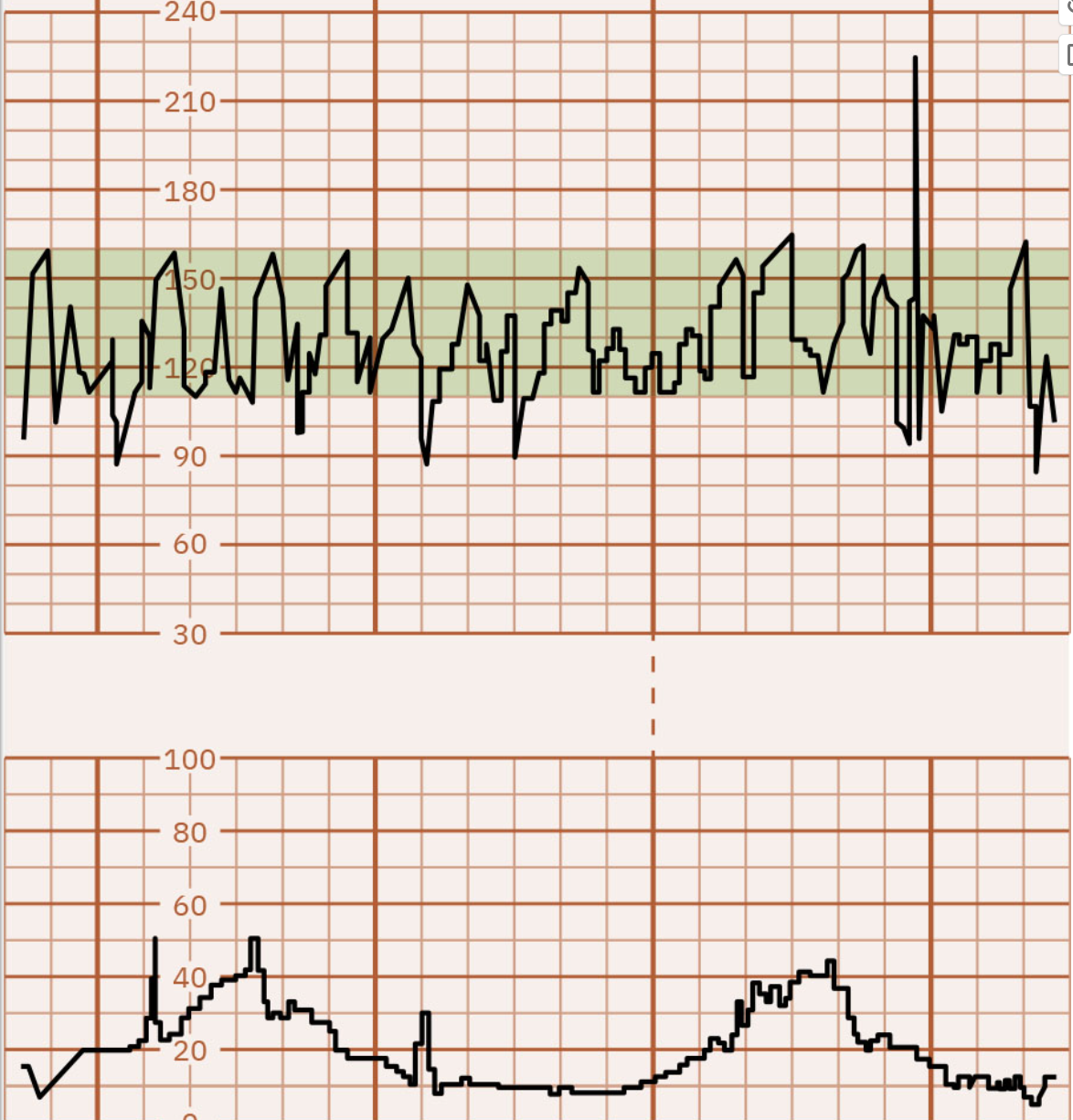
Interventions for Absent, Minimal, and Marked Variability
These are standing orders!
Lateral positioning of mother (left side is optimal; NO back)
Baby is laying on the cord!
Stop the Pitocin (oxcytocin) if infusion running
Increase IV fluid rate
decreased amniotic fluid, etc.
Administer Oxygen 8-10 mL/min by mask
mom needs oxygen
Consider internal fetal monitoring
Notify MD
One of the last things to do.
***If no change after these interventions, may need to prepare for C-section!***
Tachycardia
Fetal HR > 160 bpm that lasts 10 min or longer.
Can be an early compensatory response to asphyxia, maternal fever, etc.
Other causes may be:
Maternal fever
Maternal dehydration
Amnionitis
Drugs (cocaine, amphetamines, nicotine)
Maternal hyperthyroidism
Maternal anxiety
Fetal anemia
Prematurity
Fetal infection
Congenital anomalies
Fetal heart failure
Fetal arrhythmias
***Considered ominous sign if it's accompanied by a decrease in variability and late decelerations.***
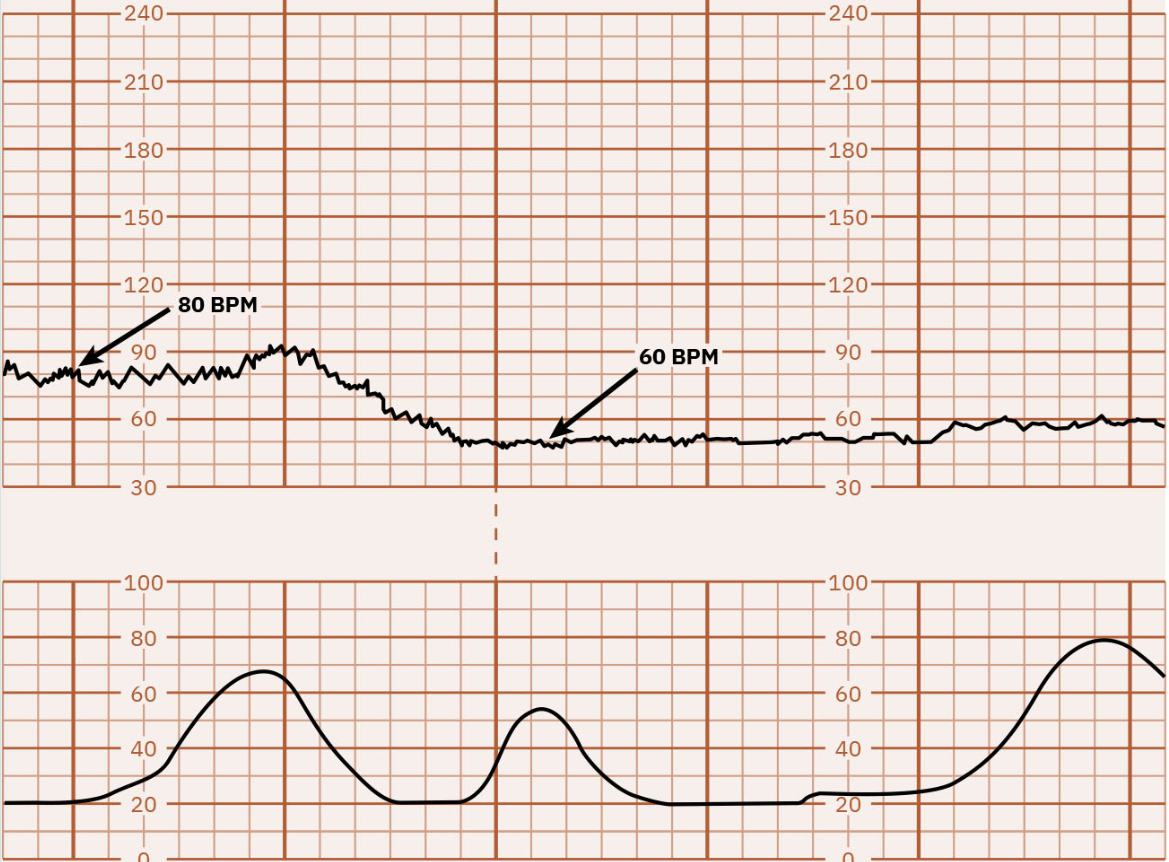
Bradycardia
Fetal HR is below 110 bpm & lasts 10 min or longer.
May indicate asphyxia, maternal hypoglycemia, hypothermia, etc.
Other causes may include:
Prolonged maternal hypoglycemia
Fetal acidosis
Administration of analgesic drugs to the mother
Hypothermia
Anesthetic agents (epidural)
Maternal hypotension
Fetal hypothermia
Prolonged umbilical cord compression
Fetal congenital heart block
***Ominous sign when accompanied by decrease in variability & late decelerations***
Accelerations
Abrupt increases in FHR above baseline.
Associated w/ sympathetic nervous stimulation.
Considered reassuring & require no interventions.
--Must have elevation of more than 15 bpm above baseline & duration must last at least 15 sec but no more than 2 min--
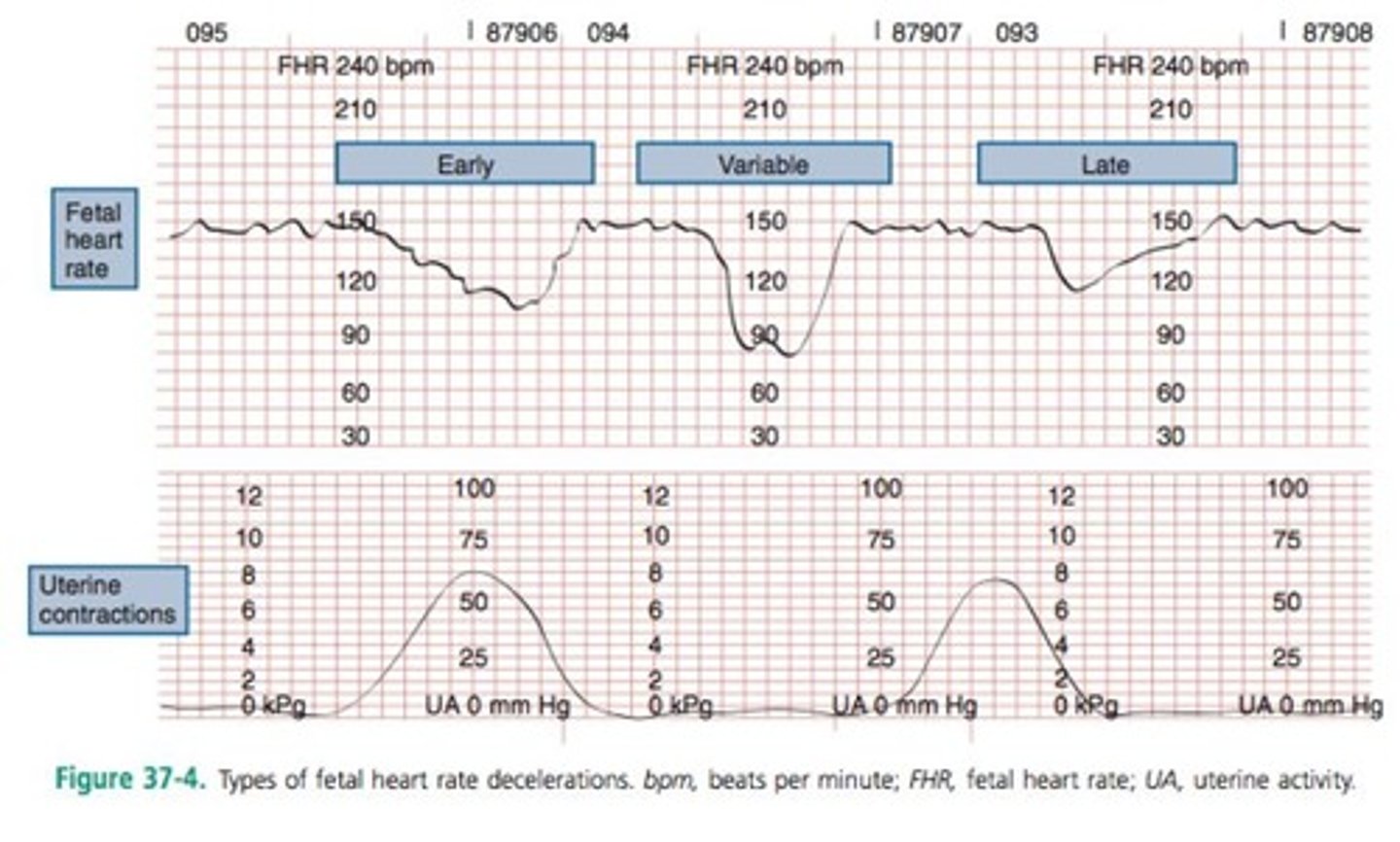
Decelerations
Fall in FHR caused by stimulation of parasympathetic nervous system.
Falls w/ the uterine contractions.
Classified as Early, Late, or Variable only.
What does a Reactive strip contain?
At least 2 accelerations in 15-20 min.
Non-Stress Test (NST)
Indirect measure of uteroplacental function.
Patient marks fetal movements during a 20 min period of fetal monitoring.
Reactive/Reassuring: 2 FHR accelerations from baseline of at least 15 bpm of at least 15 sec within 20 min period.
Non-Reactive/Non-Reassuring: Absence of 2 FHR accelerations using 15 by 15 criteria in 20 min.
Amnio-chorionic Membranes & Fluid
Amnio: inner layer
Chorion: outer later
Amniotic fluid: 1-2 L; bathes & cushions fetus & placenta within uterus.
Clear or straw colored & odorless (if odor, then an infection present).
Abnormal color indicates maternal problem or fetal distress.

Spontaneous Rupture of Membranes (SROM)
Prior to or during labor.
If preterm: antibiotics given, no intercourse, bed rest until delivery.
If at term: 24 hr window until delivery.
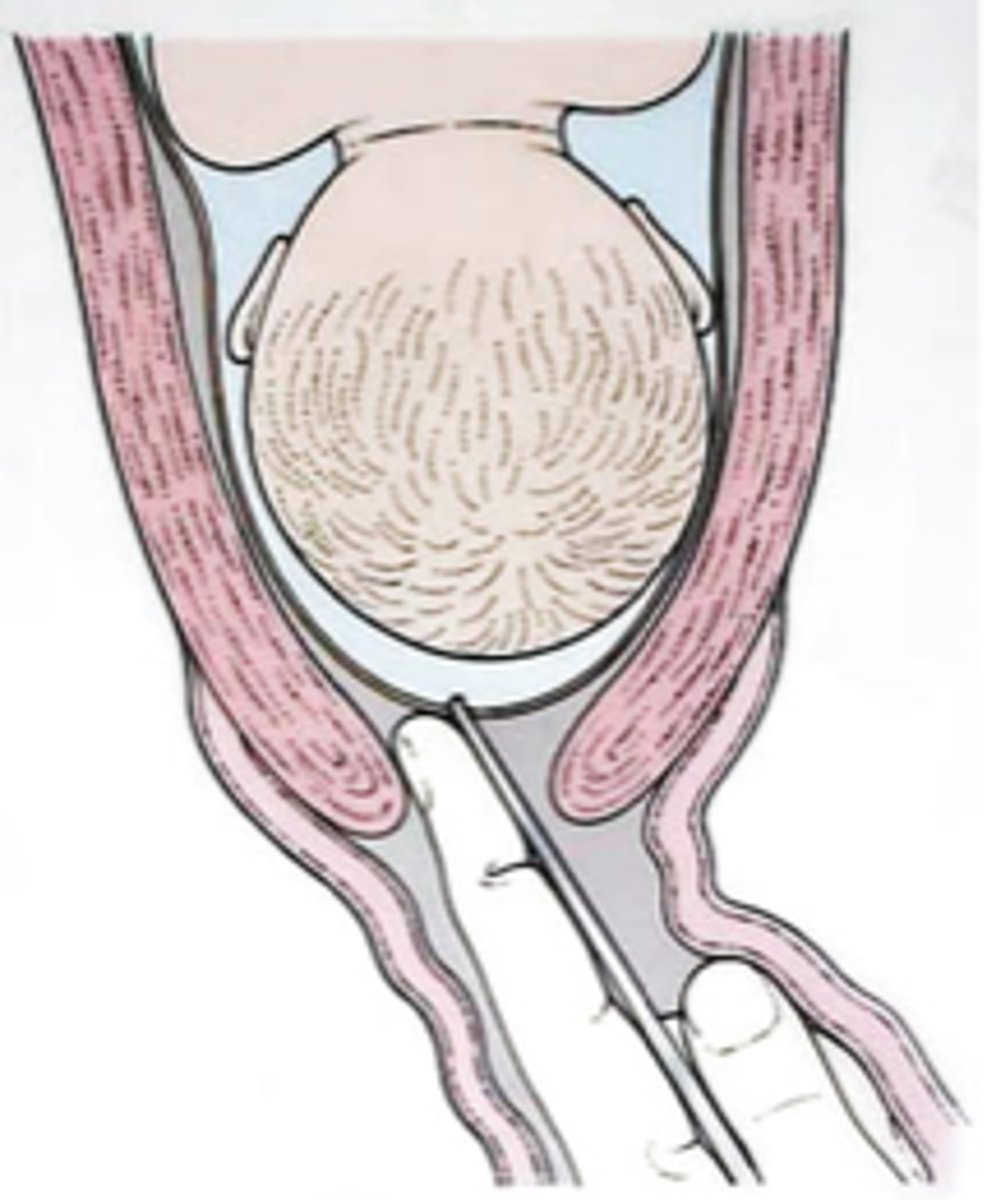
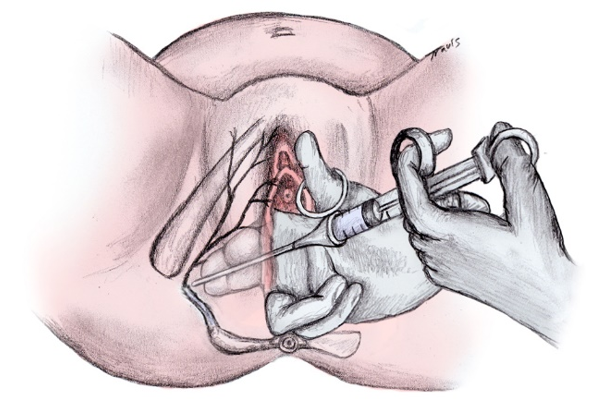
Artificial Rupture of Membranes (AROM)
While in labor.
Prior to delivery using an Amnio Hook (painless) by a midwife or physician.
If cervix is closed, can't get amniotic hook in (needs to be dilated around 2 cm).
baby’s head needs to be well engaged in pelvis (and not ballotable), so no cord prolapse occurs or breech.
What are the 3 tests to know a rupture has occured?
Fern Test:
A sample of vaginal fluid is applied to a slide and examined under a microscope.
A fern pattern on the slide indicates presences of amniotic fluid.
Nitrazine Paper:
Blue = Positive
Yellow = Negative
AmniSure Vaginal Swab:
Vaginal Swap is placed in a vial.
Then test strip detects placental cells.

Nursing Interventions for Ruptured Membranes
Monitor fetal heart rate.
Check for possible cord prolapse.
Document:
Time
Color
Odor
Clarity
Estimated amount
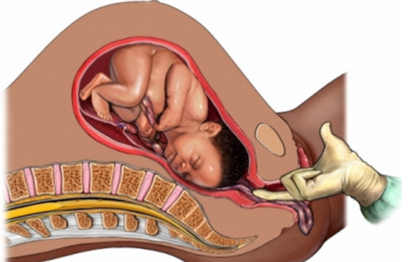
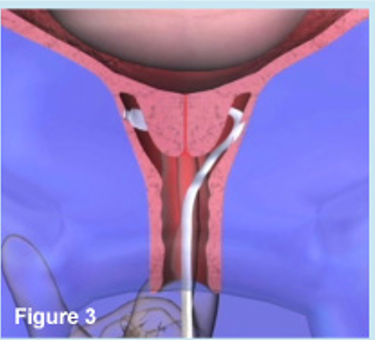
**If mom has a cord prolapse, you have to keep pressure off cord so baby doesn't die, so have to hold up the body part on the bottom (head). (as shown in picture)
**Remember santa claus story**
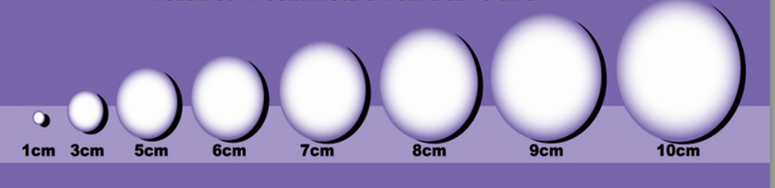
Dilation
The opening of cervix during labor.
Subjective measurement.
Expressed in cm between 1-10.
10 cm is completely dilated.
**Must occur completely & effaced to deliver baby**
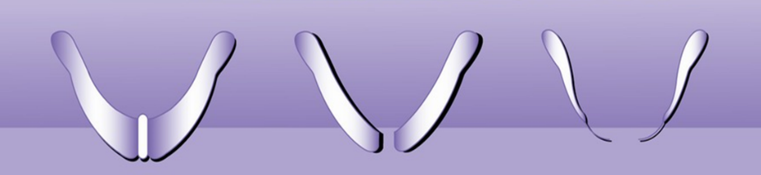
Effacement
Cervix thins (effaces) (Ex: the difference between cardstock and a piece of paper)
Measured as a percentage 0-100%.
100% is complete.
**Must be 100% & dilated to 10 cm to deliver baby**
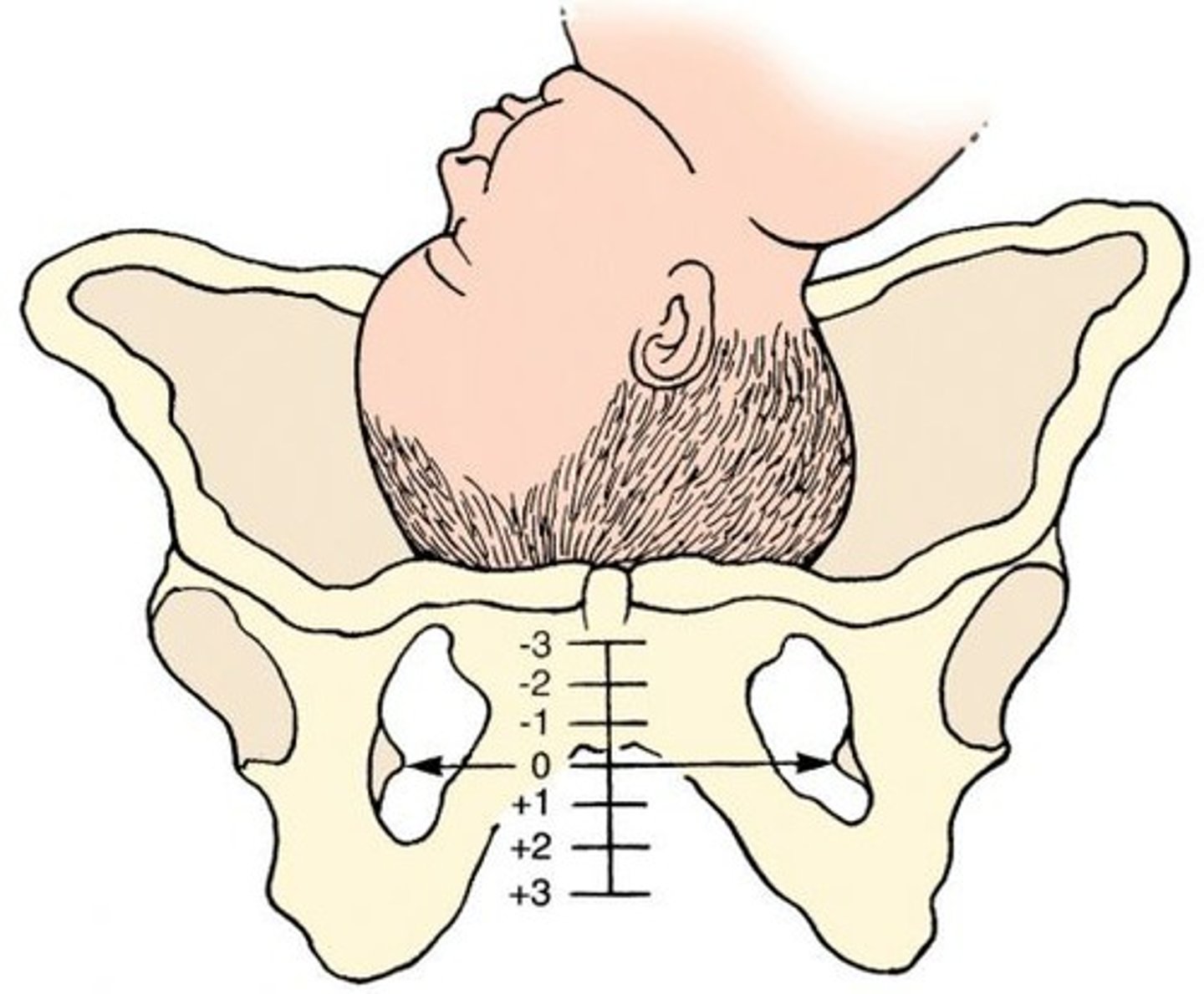
Station
Relationship of presenting part to the level of maternal pelvic ischial spines.
Plus or minus depending on its location above or below ischial spine.
Ischial spines = 0
Higher then ischial spine = -
Lower than ischial spine = +
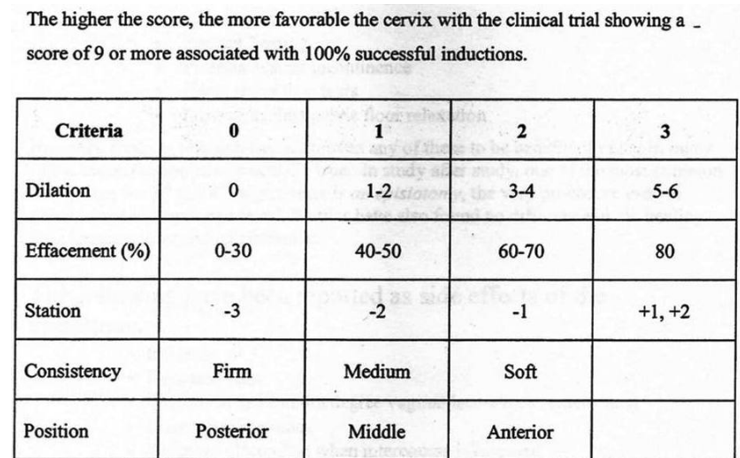
Cervical Exam Score
Dilation / Effacement / Station
Ex: 5 cm / 60% / -1
Bishop Score
Identifies women who would be most likely to achieve a successful induction.
Higher the score, the more favorable.
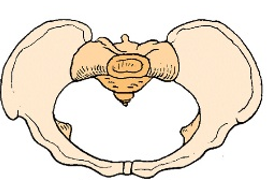
The Pelvis
False (greater) pelvis: the upper flared parts of the two ilium bones, where there is ample room.
True pelvis: bony passageway through which the fetus must travel; contains important narrow dimensions where the fetus must pass.
Key areas of the pelvis:
Inlet
Pelvic cavity
Outlet-AP diameter = 9.5-11.5 cm
Transverse diameter = 11 cm
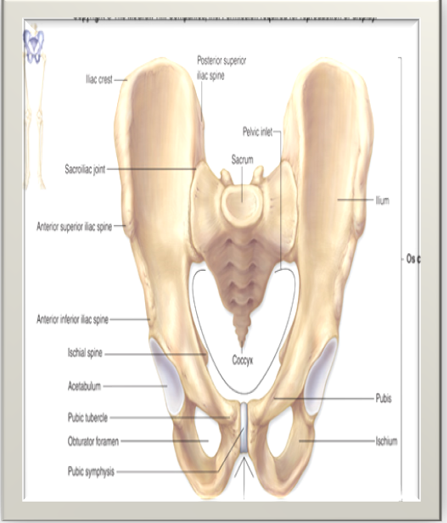
What is the main concern of the pelvis?
The adequacy in size & shape for labor & vaginal delivery.
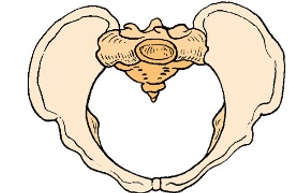
Gynecoid pelvic shape
AP and lateral diameters are equal, ideal shape, found in 40% of women.
(looks like a circle)
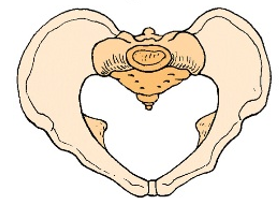
Android pelvic shape
Typical male pevis, narrow dimensions, 20% of women, forceps often needed for delivery, sometimes arrests labor.
(transverse diameter is more narrow) (kind of looks like a heart)
Anthropoid pelvic shape
Apelike pelvis, adequate for labor and birth, 25% of women.
(oval laying upright)

Platypelloid pelvic shape
Pelvis-not good for labor, frequent delays in descent 3% of women.
(longer and narrow side to side) (oval laying on its side)
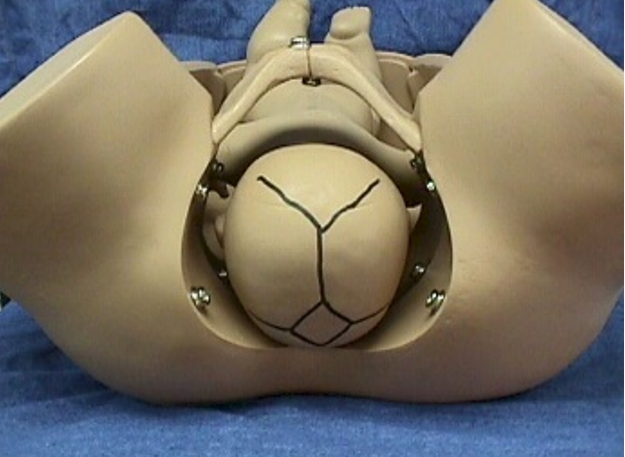
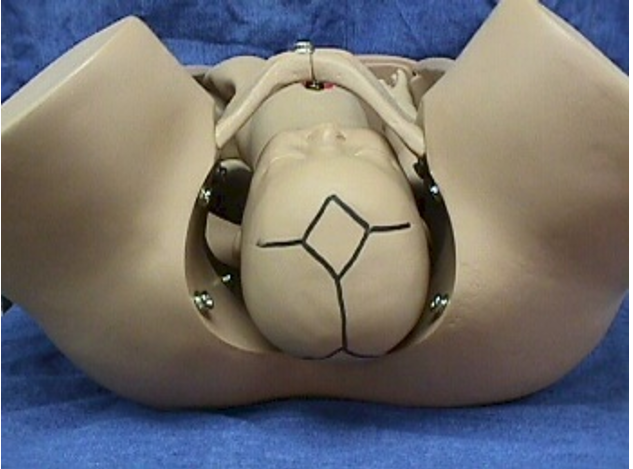
Fetal Head
1/4 of body surface area.
Sutures: the gaps between the plates of bone.
they are important b/c they allow the bones to overlap during the passageway through the pelvis.
Fontanelles: the intersection (middle) between the sutures.
Molding: the change of shape of fetal skull during labor.
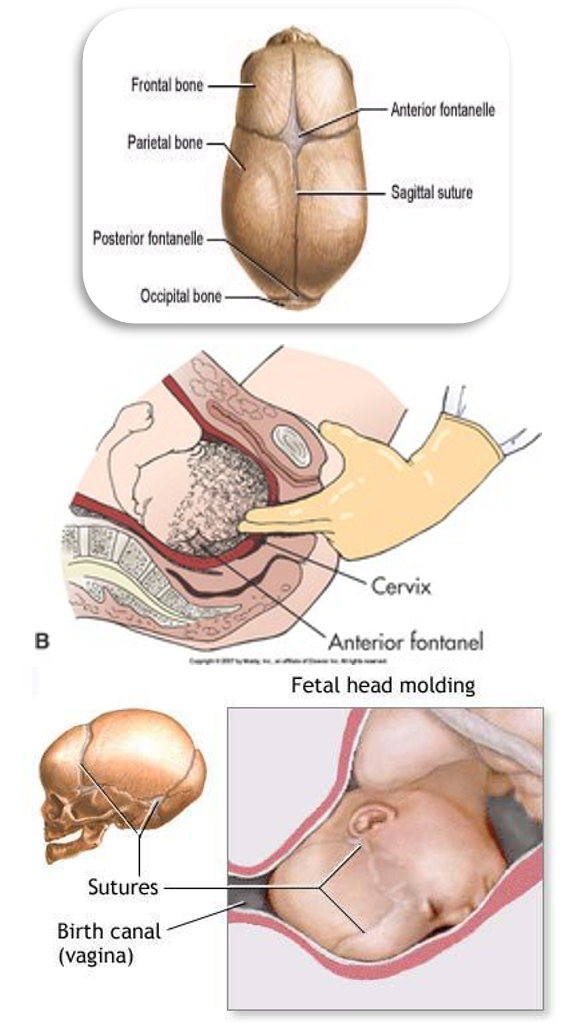
Fontanelles allows us to….
Identify position of baby during vaginal exam.
Anterior Fontanelle
"Soft spot"; diamond shaped; 1 to 4 cm; remains open for 12 to 18 months after birth; helpful in evaluating the newborn’s status.
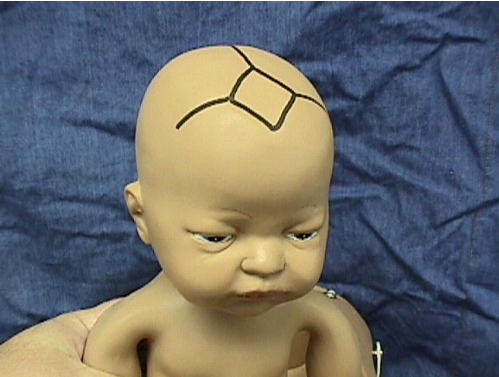
Posterior Fontanelle
Triangular shaped “Y”; 1 to 2 cm; located on the back of the fetal head; closes within 8 to 12 weeks after birth.

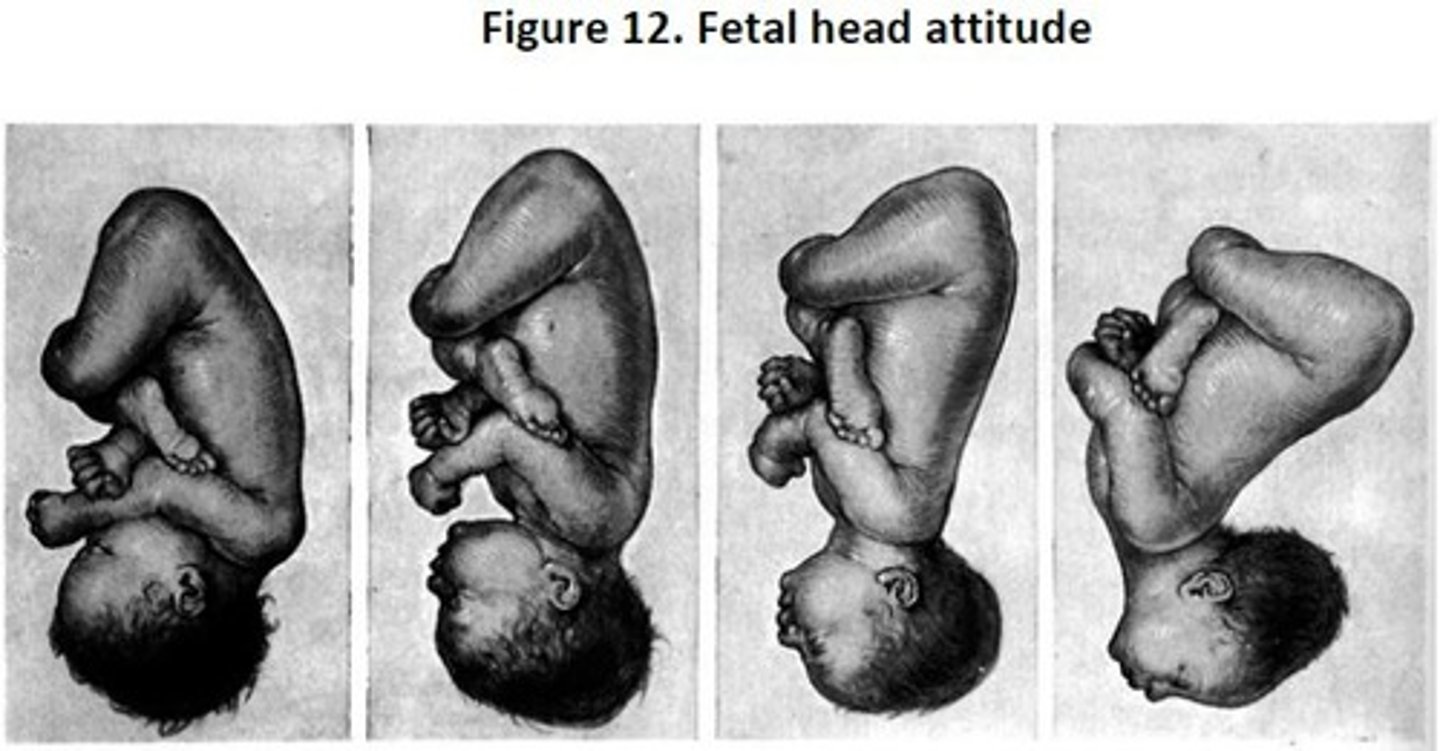
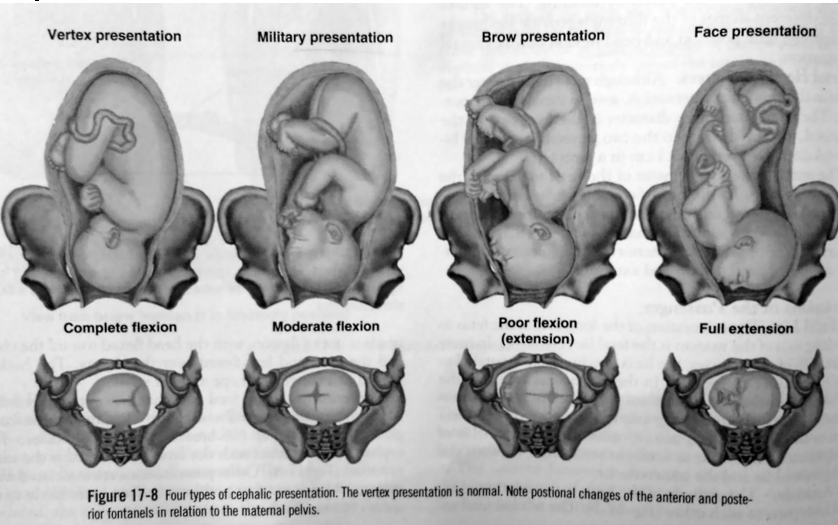
Fetal Attitude
Posturing: Flexion or Extension of the joints and the relationship of the fetal parts to one another.
Most common and most favorable for a vaginal delivery:
All joints flexed—the fetal back is rounded, the chin is to the chest, the thighs are flexed on the abdomen, and the legs are flexed at the knees.
**We want the baby’s fetal attitude in the fetal position w/ everything flexed!**
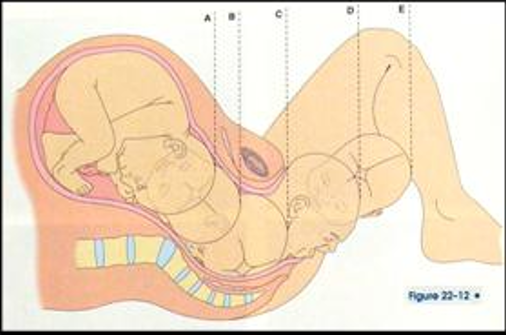
Fetal Lie
The relationship of the spine of fetus to the spine of the mother.
Longitudinal: The long axis of the fetus is parallel to that of the mother.
Transverse: The long axis of the fetus is perpendicular to the long axis of the mother (the baby cannot be delivered vaginally).
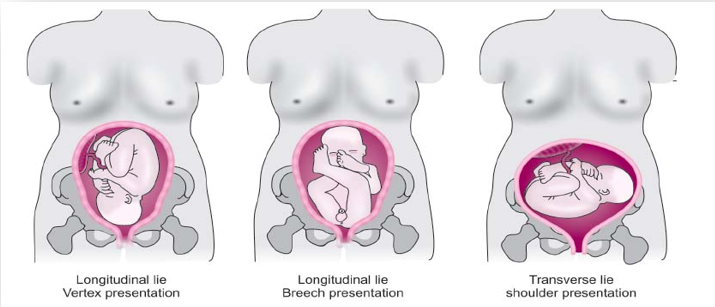
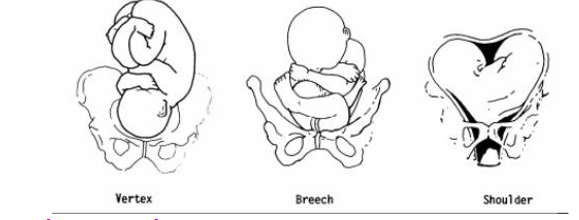
Fetal Presentation: 3 Presentations
Body part of fetus that enters pelvic inlet first "presenting part".
3 Main presentations:
Cephalic/Vertex/Occiput - head first (95%)
Breech - pelvis first (3%)
Shoulder - Scapula first (2%)
Cephalic Presentation
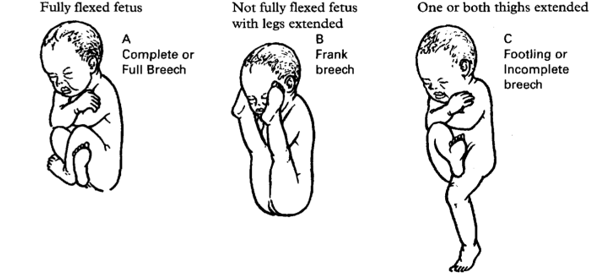
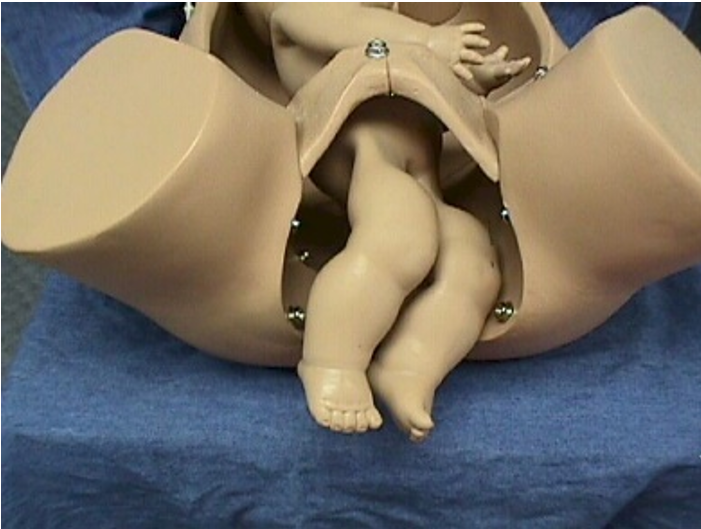
What are the 3 types of Breech Presentations?
Complete: buttocks first, fetal knees flexed.
Frank: buttocks first, legs extended.
Footling: foot or feet first; single or double footing breech.
Only a double footling can deliver vaginally (one leg can be brought down, or pushed up)
Breech deliveries can be vaginal deliveries but are somewhat higher risk b/c the head (largest diameter) is delivered last and respiratory resuscitation is last.
Fetal Position
Describes the relationship on the presenting part of the fetus to a designated point of the maternal pelvis.
Fetal Position: Landmarks
Relationship of a given point on presenting part of fetus to a designated point of maternal pelvis.
Landmark Presenting Part:
O = Occipital Bone/Vertex
M = Chin or Mentum/Face
S = Sacrum/Butt/Foot/etc.
A = Scapula/Acromion process
Fetal Position: Maternal Pelvis
Right Anterior
Left Anterior
Right Posterior
Left Posterior
What are the steps in determining fetal Position?
Identify presenting part.
Identify maternal quadrant the presenting part is facing.
Fetal Position: Abbreviations
1st Letter: L or R (presenting part is tilted towards left or right side of mom's pelvis)
2nd Letter: O, S, M, or A (represents particular presenting part of fetus)
3rd Letter: A, P, or T (location of presenting part in relation to maternal pelvis)
OA
LOA

ROA

LOT

ROT

OP
LOP

ROP

S
Pain Management Considerations During Labor
Risk to mother
Risk to fetus
Effects on contractions
Medical status of mother
Progress in labor (may slow it down unless it relaxes, then will speed it up)
Maternal Considerations for Analgesics
Discussion with mom: what are her wishes?
Assessment of mom's vitals (low BP, need fluids)
Contraindications (allergic to lidocaine, etc.)
Fetal Considerations for Analgesics
FHR & NST
Weeks of gestation
Presence of meconium (poop) in amniotic fluid
Fetal monitor / fetal status
Analgesics for Laboring Woman
Examples of Analgesics:
Stadol
Nubain
Demerol
Morphine
Phenergan
Visteral
Benadryl
Antagonist:
Narcan (for baby @ bedside)
Labor Considerations:
Contraction pattern
Engagement and descent
Effacement and dilation
Side Effects in Newborn:
Respiratory depression
Decreased alertness
Inhibited sucking
Delay of effective feeding
Before an epidural, mom needs ___ mL to ____ mL bag of IV fluid pumped rapidly into her before the procedure so her blood pressure does not bottom out. Afterwards, mom needs to ___.
800; 1000; pee
Epidural Anesthesia
1. Injection of local anesthetic agent (lidocaine or bupivacaine).
2. Injection of opioid analgesic agent (morphine or fentanyl) into lumbar epidural space.
3. Small catheter is then passed through the epidural needle to provide continuous access to the epidural space for maintenance of analgesia.
4. Tubing is hooked to pump for continuous infusion during labor & delivery.
**If medicine goes up instead of down, then respiratory depression occurs → death*
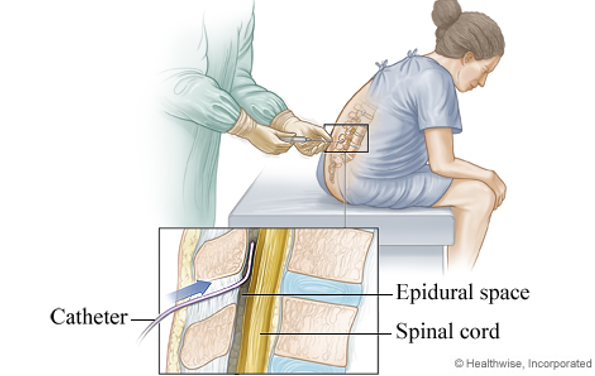
Complications of Epidurals
Increases duration of the second stage of labor.
May increase the rate of instrument assisted vaginal deliveries.
May increase need for oxytocin administration.
Nausea and Vomiting
Hypotension (Avoid supine position to minimize)
Fever
Allergic Reaction
Respiratory Depression
Fetal Complications: Fetal distress due to maternal hypotension.
Give fluids! Give mom her fluids before the procedure (800 to 1000 mL).
(Ensure the patient avoids supine position after an epidural to help minimize hypotension!)
Local Anesthetics for Labor
Pudendal Nerve Block: injection of local agent into pudendal nerves near each ischial spine (used before episiotomy).
Marcaine
Xilocaine
Lidocaine
Carbocaine
Neither maternal or fetal complications common.
Stage 1 of Labor
A. Early Phase (Latent): avg. 7-8 hrs; 0-3 cm; 30-40 sec contractions; 5-20 min contraction interval.
B. Active Phase: avg. 3-5 hrs; 4-7 cm; 50-60 sec contractions; 2-3 min intervals; beginning of discomfort.
C. Transition Phase: avg. 30 min-1.5 hrs; 8-10 cm; 60-90 sec contractions; 2-3 min intervals.
Stage 2 of Labor
Expulsion:
begins w/ complete cervical dialation & ends w/ delivery of infant.
Stage 3 of Labor
Placental:
begins after delivery of infant & ends w/ emulsion of placenta --- CAN'T PULL IT, CAUSES HEMORRHAGE!
Stage 4 of Labor
Recovery (physiological readjustment):
1-4 hrs after birth.
Monitor: fundal firmness, vital signs, bonding, hemorrhage, food, fluids, output.
Cardinal Movements of Labor
Labor begins & fetus starts to go through many position changes as it travels through passageway.
Deliberate
Specific
Very Precise
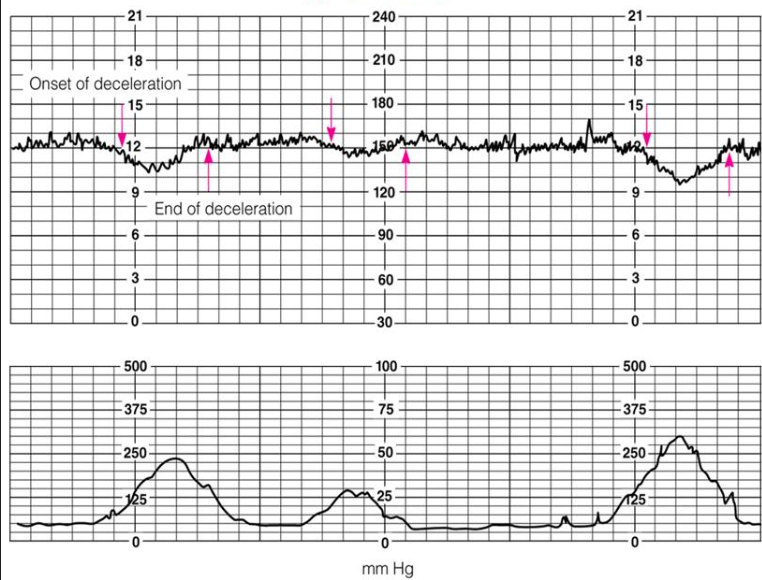
Early Decelerations
Symmetrical
Gradual decrease in FHR (lowest point) occurs @ peak of contraction.
Rarely decrease more then 30 bpm to 40 bpm below baseline.
Most often seen during active stage of labor (pushing, crowning, or vacuum extraction).
Result of fetal head compression.
“a mirror image of the contraction.”
An indication that mom is progressing to labor. Baby is low in that pelvis and getting ready.
NOT INDICATIVE OF FETAL DISTRESS & DOESN’T REQUIRE INTERVENTION
Late Decelerations
Usually symmetrical.
Decrease in FHR that occur after peak of contraction.
FHR doesn't return to baseline until well after contraction ends.
Associated w/ uteroplacental insufficiency (placenta stopped giving baby nutrients; not oxygenating baby well).
Peaks don’t match…the decel is happening after the contraction!
___________________________________________________________
Interventions:
1. Notify provider
2. Discontinue Oxytocin
3. Turn patient on left side
4. Administer Oxygen via mask
5. Increase IV fluids
6. Prepare for C-Section
7. Document all interventions
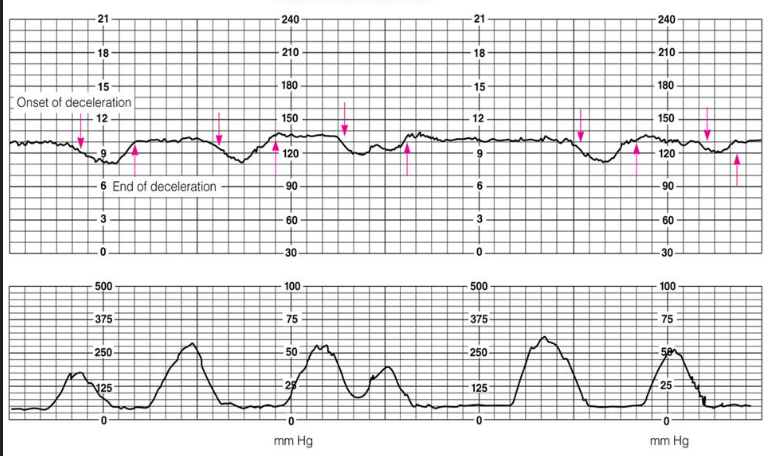
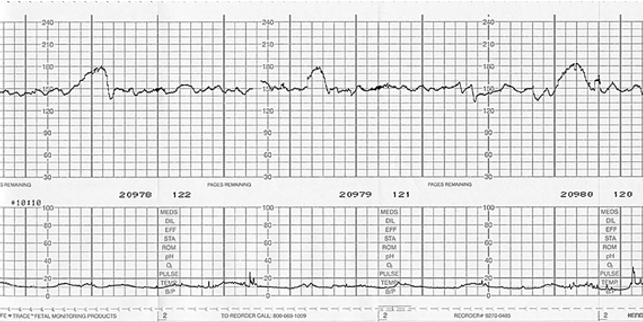
Variable Decelerations
Abrupt decrease in FHR below baseline & have unpredictable shape.
May have no consistent relationship to contraction.
Shape of variable may be U, V, or W or others.
Most common deceleration found on laboring women.
Usually transient & correctable.
Associated w/ cord compression (roll over to get compression off).
They decrease more than 30 bpm to 40 bpm.
_________________________________________________________________
Interventions:
1. Turn patient on left side
2. Administer Oxygen via mask
3. Increase IV fluids
4. Amnioinfusion - inject fluid through catheter in uterus to give cushion
VEAL CHOP
Variable Cord Compression
Early Head compression
Acceleration Ok
Late Placental insufficiency
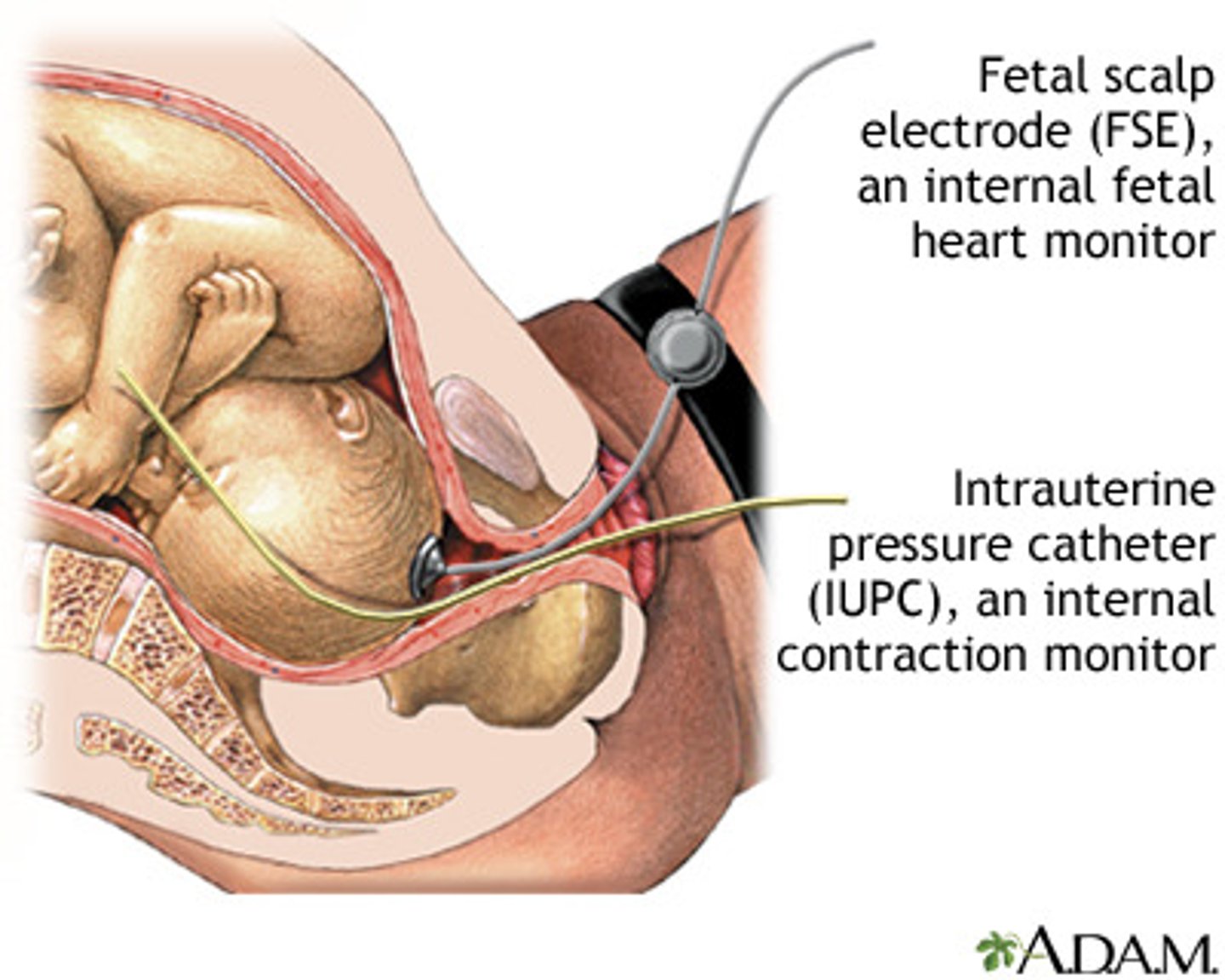
Internal Monitoring (Mom & Baby)
Internal Fetal Heart Monitor (Scalp Electrode) -- (FSE):
Placed on fetus’ presenting part.
Must have ruptured membranes!
Cervical dilation of at least 2 cm!
Most accurate measure for detecting fetal heart characteristics.
Not used in patient’s w/ HIV+, hepatitis, and some preterm fetuses.
Internal Uterine Pressure Transducer (catheter) (IUPC):
Provides actual strength of contraction; where we see the actual contraction pressure.
Can aid provider to determine if oxytocin needs to be increased or not.
**Can have one w/o the other**
Types of Pushing
Spontaneous Pushing: natural way during 2nd stage of labor.
Open glottis method: air is released during pushing to prevent buildup of intrathoracic pressure & support mother's voluntary bearing-down efforts. (latest recommendation)
Direct pushing: hold breath & count to 10, inhale, push again, and repeat the process -- NOT GOOD (interferes w/ oxygen exchange between the mother and the fetus).

Vaginal Cephalic Delivery
Fetal head descends, the woman has urge to push, when perineum bulges & then flattens.
Bloody show increases.
Labia part w/ each contraction, fetal head begins to show (crowning).
Anus protrudes.
Head is born between contractions & suctioned.
Body follows.
***Note & record time, status of mother & baby, estimated blood loss***

Early Cord Clamping is when the…
Cord is clamped in the first 60 seconds after birth.
Delayed Cord Clamping is when the…
Cord is not clamped during the first minute after birth, only when cord pulsation has ceased.
Benefits of Delayed Cord Clamping
Term Infants: increase hemoglobin levels & improves iron stores during 1st several months of life which may favorably effect developmental outcomes.
Preterm infants: decreases rate of intraventricular hemorrhage & decreases rate of necrotizing enterocolitis.
Mom: doesn't increase risk of postpartum hemorrhage or blood loss.
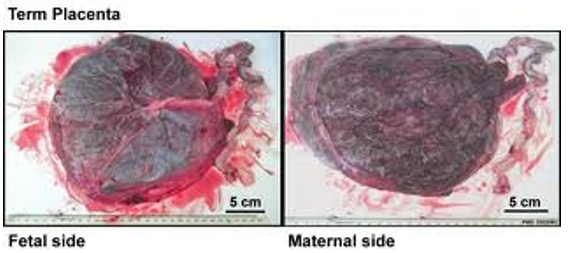
Signs of Placenta Separation
After delivery, uterus contractions seperate the placenta from the uterine wall.
Globular shaped uterus.
Rise of fundus in abdomen.
Sudden gush or trickle of blood.
Increase descent of cord.
**Record time of delivery of placenta. Note nuchal cords or knots. Make sure placenta is intact and no missing pieces.**

Placental Delivery
Record time of delivery.
Note nuchal (around neck) cords or knots.
Make sure placenta is intact & no missing pieces.
_________________________________________________________
Retained placenta: more than 30 min after delivery, placenta doesn't detach & descend.
Schultze mechanism: shiny (Fetal side) out
Duncan mechanism: maternal side (not shiny)
Pitocin IV after delivery of placenta: increase firmness of fundus (contracts uterus & prevents hemorrhage)
Nursing Interventions & Complications During Delivery
VS, fetal monitoring
Change position
Keep bed & patient clean & dry
Pain meds if requested
Prep for C-section if needed
Answer all questions from patient and family
Keep room quiet & relaxing
Monitor fluid & electrolyte balance
Monitor intake & output
Comfort measures:
breathing patterns; positioning; back rub; effleurage (form of massage on hands); cool wet washcloth on head or neck; glycerin swabs in mouth; NPO with ice chips; assist w/ pushing.
Complications: pain, bleeding, fetal distress as indicated by fetal monitoring, fear, uterine dystocia, med side effects, oxygen needs, S&S of infection.
Role of the Partner
Women need support during this time.
Partners can convey emotional support by offering a continued presence & words of encouragement.
Massage, light touch, hand-holding, stroking, relaxation.
Women who receive continuous labor support are more likely to give birth spontaneously, less likely to use pain meds, & more satisfied w/ experience.
Indications for Cesarean Birth (C-Section)
Cephalopelvic disproportion (CPD)
Placenta previa
Placental abruption
Fetal distress
Failure to progress (uterine dystocia)
Acute maternal illness (Severe pregnancy induced HTN, diabetes)
Maternal death
Active herpes
Umbilical Cord Prolapse
HIV+ with high viral load
Some breech presentations
Some multiple gestations
Ruptured membranes, infection
Previous C-section
---DON'T MEMORIZE---

Cesarean Birth (C-Section)
Higher mortality rates than vaginal!
Incisions are vertical or low transverse.
Preparations for sx:
consent
anesthesia
catheterization
skin prep
answer all questions momma asks
give support
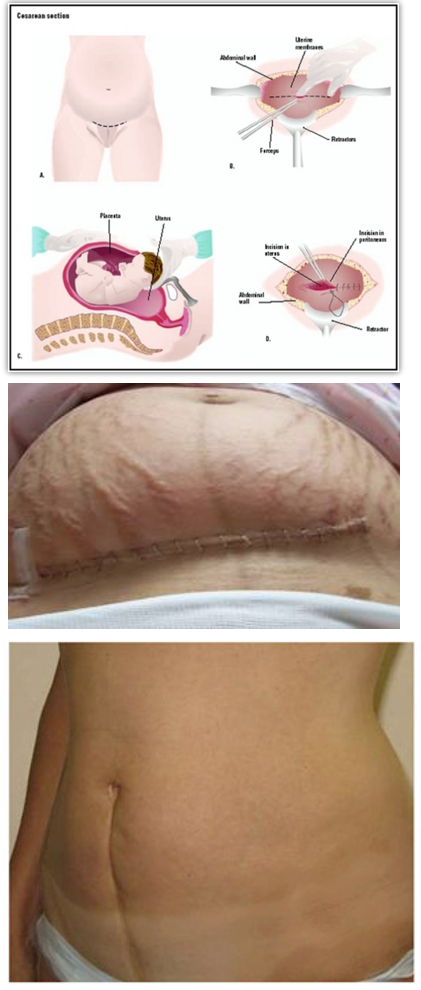
Recovery After Birth: Interventions
Assist w/ bonding
Vital signs
Hemorrhage
I & O
Incision
Fluids & Electrolytes
Comfort

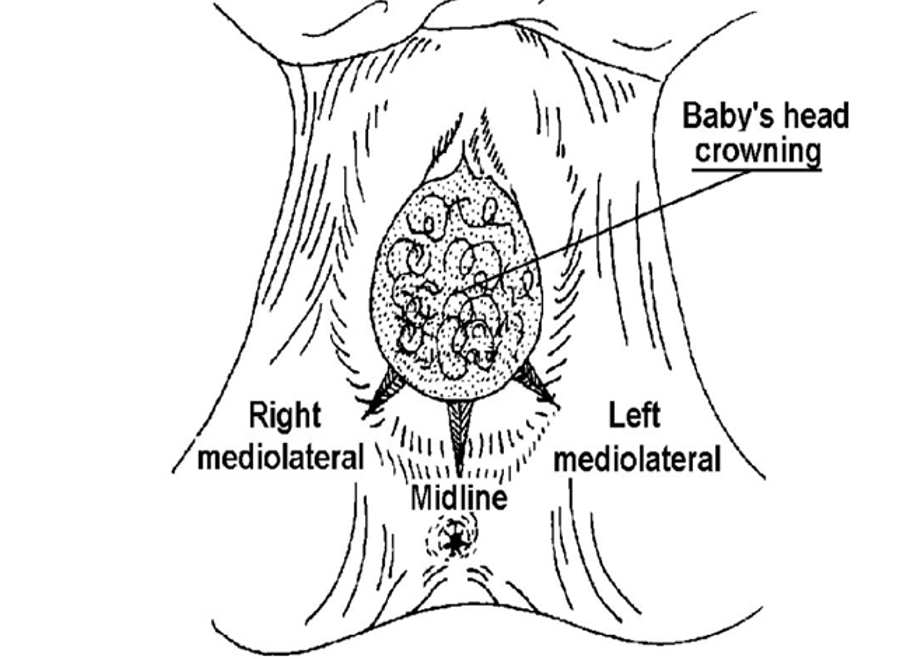
Episiotomy
A surgical incision of perineum; right or left mediolateral or midline.
Rational for use:
Prevent lacerations of the perineum.
Surgical incision easier to repair & heals faster than laceration.
Not used as much anymore; use more gel & patience.
Used to shorten 2nd stage of labor.
Right when the baby is crowning to give some more room.
***Done just prior to delivery, use Xylocaine before procedure.***
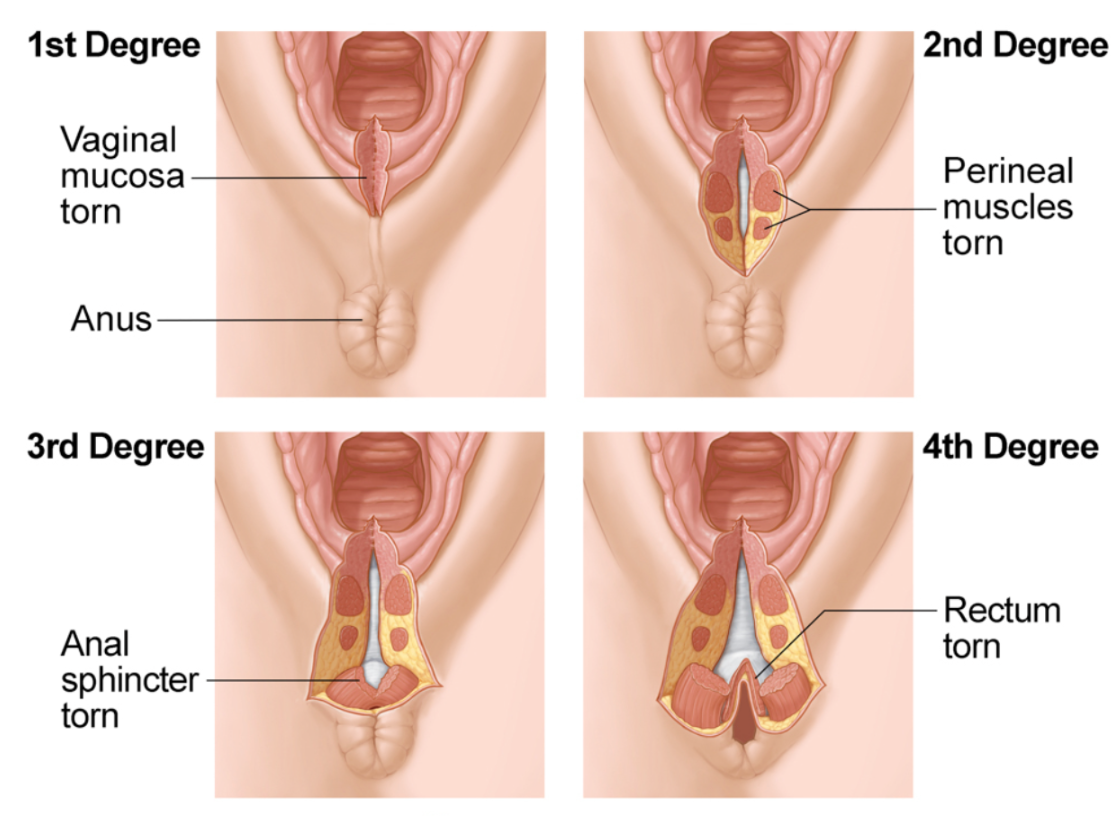
Repair of Lacerations
Perineal lacerations can occur when no episiotomy is done or as an extension of an incision.
Degrees:
1st degree: involves perineal skin & vaginal mucosa.
2nd degree: involves above plus underlying fascia & muscle.
3rd degree: involves all of above & extended into anal sphincter.
4th degree: all of above with tear into anal sphincter extending up to rectal wall.
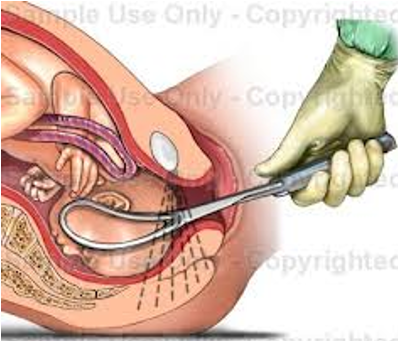
Forceps Delivery
Used to provide traction or rotate.
Types:
Low outlet forceps - used when fetal head is visible on perineum to provide control & guidance of fetal head. (seen more often)
Mid-forceps - fetal head is engaged, used to rotate OP or OT positions.
Can be dangerous!!
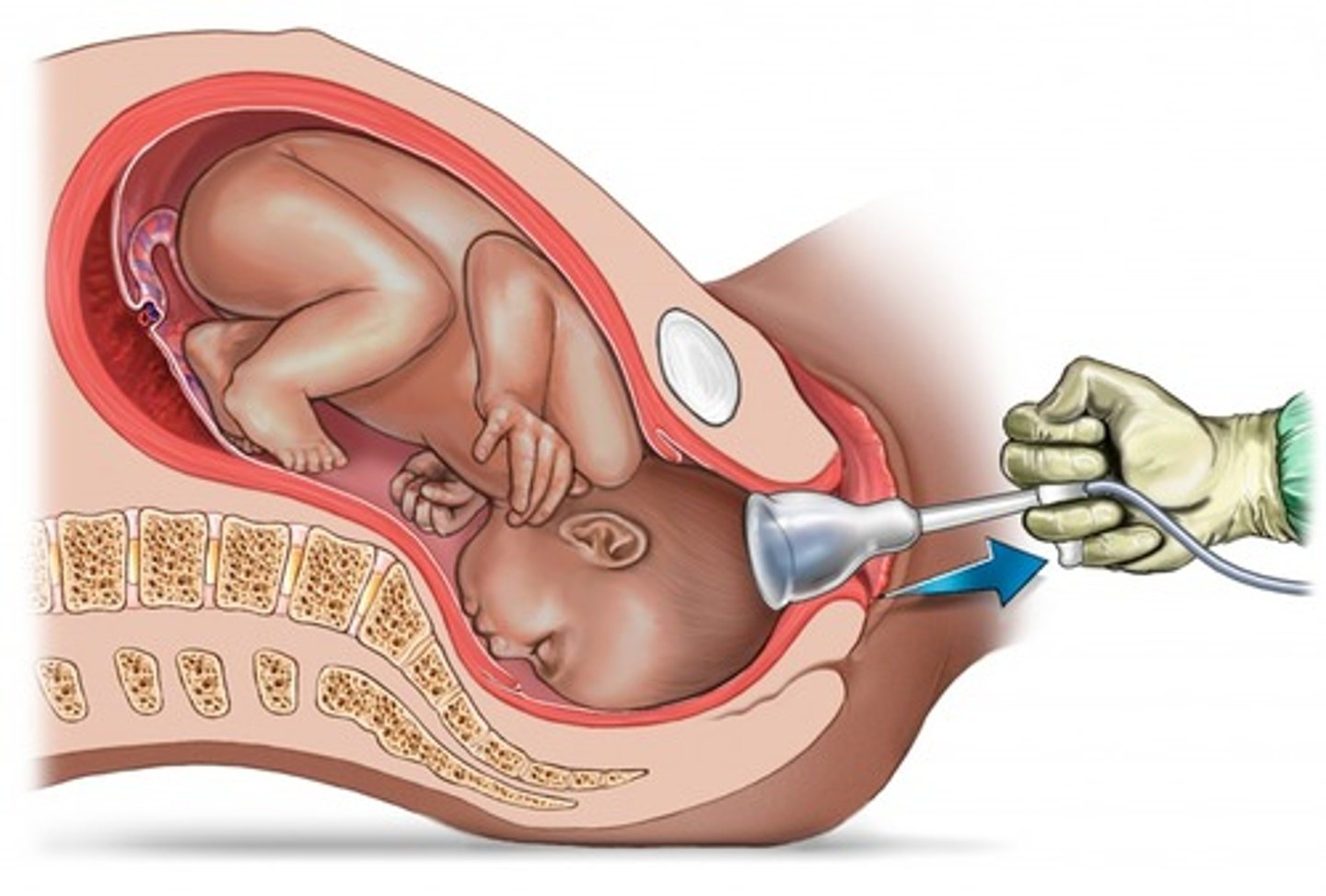
Vacuum Extraction
Suction cup attached to fetal head & suction or negative pressure is applied via a suction bottle or pump.
Problems: can cause soft tissue necrosis @ cup attachments, cephalohematoma, or cerebral trauma.
Labor Induction
Initiates labor by stimulating uterine contractions before spontaneous onset of labor.
Indications:
Continuation of pregnancy would affect maternal or fetal health (PIH, diabetes, post-maturity, fetal death, prolonged ROM).
To shorten early phase of labor.
Contraindications:
Fetal distress
Placenta previa
Placental abruption
Cephalopelvic disproportion (CPD)
Predisposition to uterine rupture
Grand-multiparty
Past history of traumatic delivery
What are the 3 Methods of Labor Induction?
AROM (if dialated)
Cervical Ripening: (if not dialated)
Prostaglandin gel
Cytotec—causes uterus to contract (can be give po, rectally—if hemorrhaging, vaginally)
Cervadil (seen in picture)
Mechanical Cervical Ripening—instrument forcing the cervix to open.
Pitocin: through secondary IV infusion-per pump.
Side Effects:
Placental abruption
Fetal hypoxia
Uterine tetany
Rupture
Decreased oxygen in fetus
***STOP use if SE are evident
***Monitor mother & fetus: VS, FHR, contractions
***Check dilation & effacement

Augmentation of Labor
Stimulates and facilitates uterine contractions. (mom is already in labor; this just helps it move it further along)
artificial stimulation of uterine contractions when spontaneous contractions have failed to result in progressive cervical dilation or the descent of the fetus.
Pitocin infusion: follow induction protocols.
AROM: caution, delivery must follow within 24 hrs.
Contraindicated for any fetal or maternal emergency.
