Chapter 7
7A - Detecting pathogens
Immune system: Uses antigens to recognise if a cell or molecule is self or non-self. If identified as non-self, an immune response is initiated.
Definitions:
Pathogen: An agent that causes disease
Antigen: Any molecule that may trigger an immune response (can be free flowing)
Non-self antigen: A molecule from outside the body that is recognised by the immune system
Self antigens: Located on the surface of cells, mark the cells as self so the immune system does not attack, this is done by MHC markers.
Major histocompatibility complex (MHC) marker class 1: Expressed on all nucleated cells in the body (all cells except those without a nucleus e.g red blood cells)
MHC Class II markers: Found on specialised cells of the immune system (antigen presenting cells)
Non-self antigen example:
MHC markers differ between individuals. In an organ transplant, the MHC marker class 1 expressed on the donor oragn will be different to the MHC marker class 1 on the reciever, which can cause the reciever’s immune system to attack the organ.
Antigen malfunction:
Autoimmune disease: Recognition of self anitgens as non-self. Immune system then attacks self cells.
Allergen: Non-pathogenic antigens that the immune system recognises as non-self and initiates a strong immune response towards.
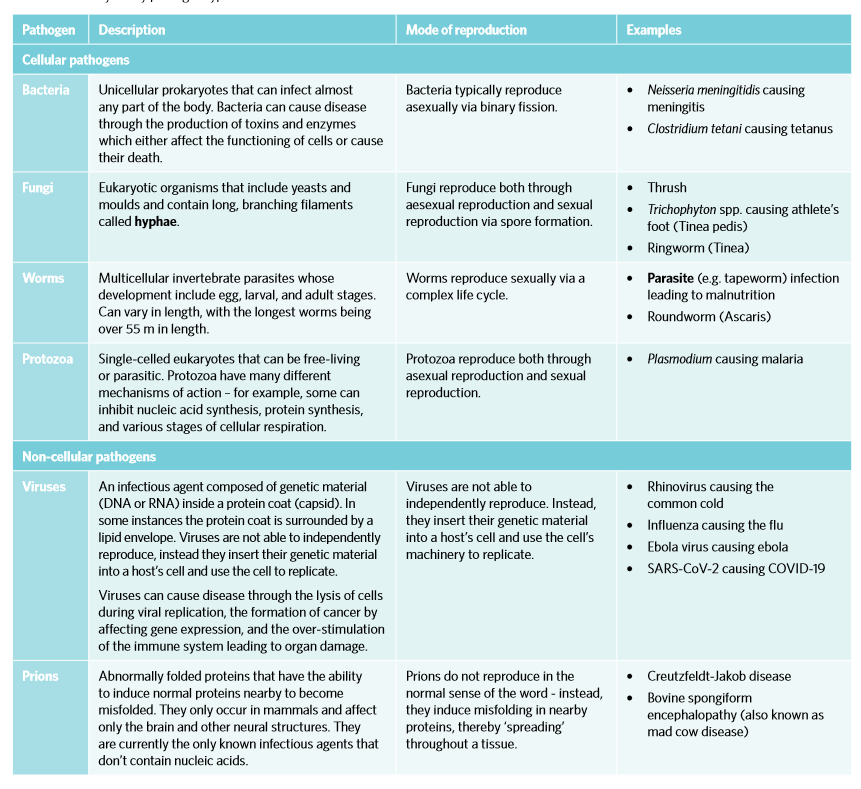
Types of pathogens:
Cellular: Have a cellular structure and are living organisms (bacteria, fungi, worms, protozoa)
Non-cellular: Non-living, no cellular structure (viruses, prions)
7B - The First Line of Defence
Innate immune system (generalised or non-specfic responses-responding within minutes to hours)
Plant barriers:
Physical: Thick bark, closing of stomata, waxy cuticles of leaves
Chemical: Production of various chemicals (e.g. peppermint oil)
Animal barriers:
Physical: Intact skin, mucus secretions and cilia
Chemical: Digestive enzymes, enzymes in tears, enzymes in sweat, stomach acid
Biological: Gut flora, bacteria on skin
7C - The Second Line of Defence
Second line - Innate immune system: Composed of a variety of cells and molecules that destroy pathogens which have entered the body preventing the spread of infection.

Phagocytosis (process):
Process in which phagocytes (neutrophils, macrophages and dendritic cells) consume and destroy dead or foreign material present in the body by engulfing it through the process of endocytosis.
Once engulfed, lysosomes containing antimicrobal enzymes called lysozymes in the cell destroy the foreign or dead material by fusing with vesicles which contain it.
Cytokines: Phagocytes release cytokines which are signalling molecules that help protect against pathogens and can guide immune cells to site of infection.
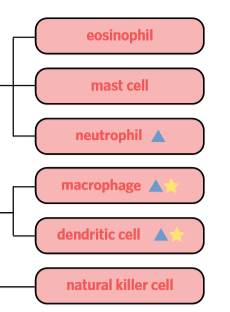
Phagocytes:
Neutrophils: The most common type of leukocyte in the body. Engages in phagocytosis of pathogens and foreign material, as well as the release of cytokines
Macrophages: A type of leukocyte found throughout the body that engages in phagocytosis and antigen presentation. Initiate actue inflammatory responses by releasing cytokines.
Dendritic cells: A type of leukocyte that engages in phagocytosis and antigen presentation.
Antigen-presenting cells:
Subgroup of phagocytes that display antigens from consumed pathogens on their surface and interact with the adaptive immune system
Present MHC class II markers
Natural killer (NK) cells:
Large granulated cells which target both virally and abnormally infected cells.
Edrolo textbook:
Killer inhbtory receptor: Examine the surface of cells for MHC class I markers. The abscene of MHC I marker could be due to the presence of a viral infection, or the gene expression affected in cancer cells. If there are missing MHC markers, then a killer activation signal is released and the cell will undergo apoptosis.
Mrs Rajulu:
Granules degranulate to release granzymes (proteases and perforin). Proteases initiate apoptosis. Perforin make holes in virally infected (cancer) cells. Macrophage cleans apoptopic body.
Mast cell:
Location: Connective tissues
Mast cells activate when injury is detected in surrounding cells, or when a antigen or allergen stimulates them.
When activated, they degranulate and release histamines. Histamines play a part in the inflammatory response.
Eosinphills:
WBC containing many vesicles whih contain various chemicals which combat pathogens
Non-cellular part of 2nd line of defence (complement proteins, interfrons etc)
Interfrons (type of cytokine)
Released by virally infected cells. They interact with receptors on neighbouring cells, making changes to them which make them less susecptible to a viral infection. This means the virus will not spread between cells.
Complement proteins
Complement proteins react with each other and then cause a series of reactions called a complement cascade
3 outcomes of cascade:
Opsonisation: Complement proteins stick on the outside of the pathogen so it is easily recognised by the immune system (phagocytes) to recognise it as foreign.
Chemotaxis: Gather near pathogen attract phagocytes so it is more likely to be destroyed
Lysis: Complement proteins join together on the surface of the pathogen forming a MAC (membrane attack complex) which creates pores in the membrane. Fluid enters into the pathogen making it swell and burst (osmotic shock).
Inflammatory response
Inflammation: Increase blood flow to injured area which attracts immune cells to fight pathogens which may have entered. Increase in blood and fluid causes swelling, pain, redness.
Initiation: Cells release cytokines and mast cell degranulate releasng histamines.
Vasodilation: Histamine binds to specific receptors which causes vasodilation of blood vessels. Blood vessels widen which increases blood flow to the area causing redness. The more blood there is the more WBC there will be.
Migration: Cytokines increases permability of the membrane of the blood vessel as well as causes leakiness of blood vessels. This allows for phagocytes and complement proteins to leave the blood stream and enter site of injury. Area swells due to accumalated fluid which puts pressure on pain receptors on the neighbouring cells which causes pain.
7D - The Third Line of Defence - TEXTBOOK HAS AWESOME DIAGRAMS
Adaptive immune response: Specfic
Antibodies: Protein produced by plasma cells during adaptive response that is specifc to an antigen and combats pathogens (immunogoblins)
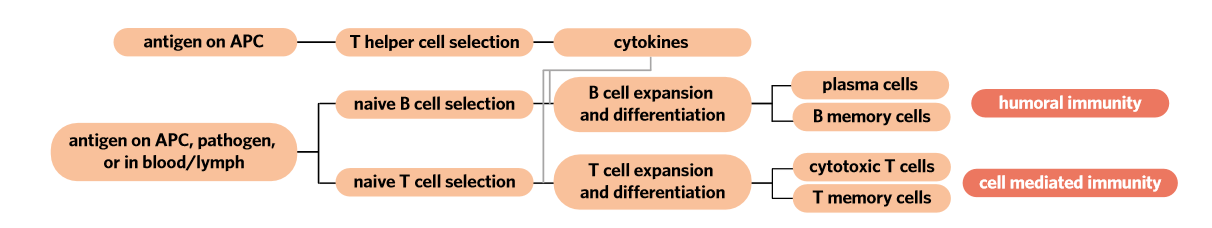
 Antigen presenting cell (APC) process
Antigen presenting cell (APC) process
APC engulf and digest pathogens via phagocytosis displaying pathogenic antigens on their MHC II markers.
After this process they travel via the lymphatic system to the lymph nodes to present foreign antigens on their surface using MHC Class II proteins.
MHC Class II proteins interact with complementary T cell receptors on T helper cells. When this interaction occurs, T helper cell is activated and selected.
This facilitates immune response - either humoral or cell-mediated.
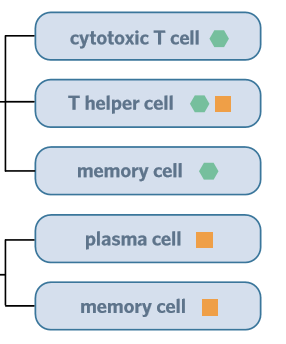
The Humoral response (extracellular pathogens)
Involves the neutralisation and destruction of extracellular pathogens via the production and secretion of antibodies
B lymphocytes: type of WBC with a surface covered with antibodies. They travel in the bloodstream and reside in lymph nodes. The antibodies are different on one to the other
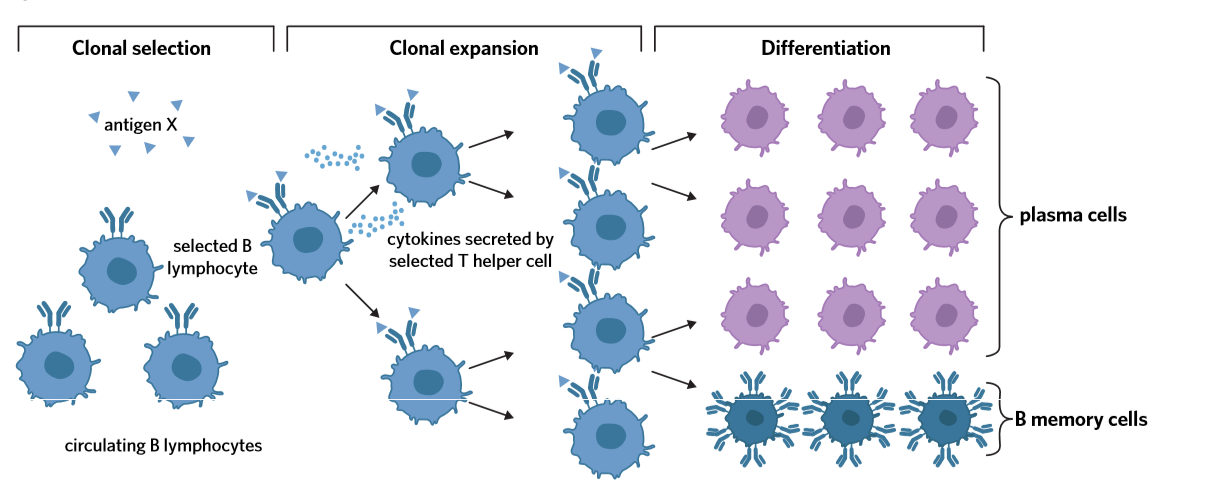
Response broken down:
Pathogen with an antigen that is complementary in shape to the antigen binding site on a B cell will then interact. B cell is selected.
T helper cell (selected through antigen presentation) which has complementary receptor to the antigen will recognise selected B cell and secrete cytokines - cytokines cause B cell to undergo clonal expansion - copies of B cell produced. Cytokines also stimulate B cell to differentiate - B cell clones divide into 2 types of B cells - B memory cells and effector cells - which are plasma cells.
Plasma cells produce and release antibodies to defend against pathogen.
B memory cells provide immunological memory
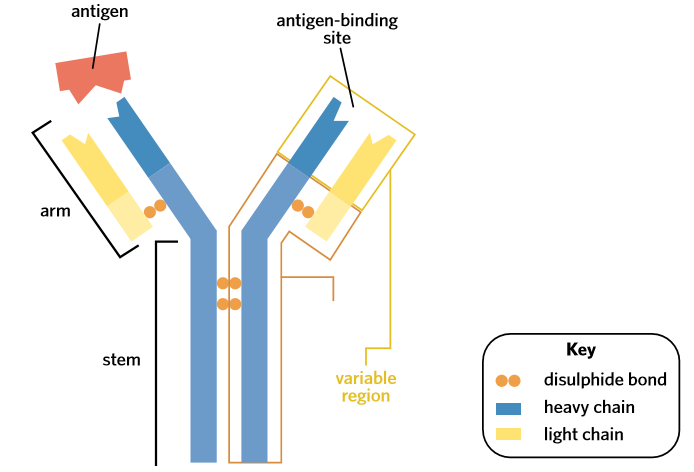
Antibodies
Quaternary structure
Four polypeptide chains
Two heavy chains joined by disulphide bond
Antibody can bind with two antigens at once, as there are two antigen binding sites
Different types of antibodies:
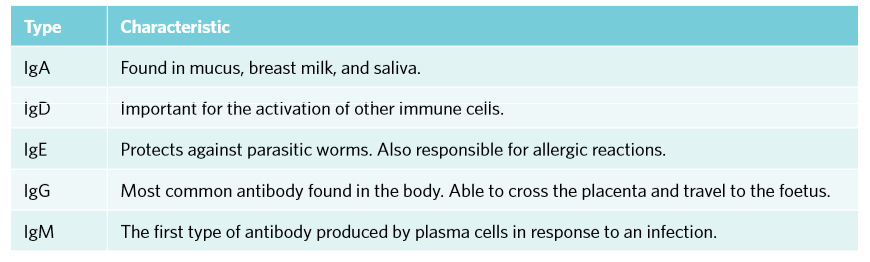 Key functions of antibodies:
Key functions of antibodies:
Neutralisation: Anitbodies block sites of pathogens that are used to attack host cell and can block active sites of toxins
Immobilisation: Antibodies restrict movements of pathogens around the body through forming a large antigen-antibody complex
Opsonisation: Antibodies bind on pathogen surface to make it easier to phagocytose
(Aggulation: clump pathogens together) (Activation of complement proteins)
The Cell Mediated response (intracellular pathogens and cancer cells)
Involves destruction of infected or abnromal cells via the clonal selection of a cytotoxic T cell
T lymphocyte: Type of lymphocyte that differentiates into cytotoxic T cells, T memory cells and T helper cells
Cytotoxic T cells (Tc): Destroys infected or abnormal cells
MHC Class I can display antigens that have been broken down in a cell on its surface
Response broken down:
At the same time as APC response, APCs come across naive T cell with a T cell receptor that matches the antigen being presented, initiating the process of clonal selection.
Selected T helper cells release cytokines which stimulate naive T cell to undergo the process of clonal expansion and differentiation - T cells differentiate into effector cells called cytotoxic T cells (leave lymph node and travel to site of infection) and T memory cells (form immunological memory)
Cytotoxic T cell finds abnormal cell that is presenting complementary foreign antigens on its MHC class I marker. T cell receptor binds to the antigen MHC class I marker. Chemicals (perforin) are secreted by cytotoxic T cell to induce apoptosis in the cell.
 Immunological memory
Immunological memory
B and T memory cells
B memory cells: Rapidly dividing and forming new antibody-producing plasma cells when they encounter an antigen that matches their receptor - they also secret small amounts of the antibody.
T memory cells: Multiply rapidly into T helper cells and cytotoxis T cells upon simulation by an antigen-presenting cell that is presenting a previously encountered antigen
7E - Lymphatic system
Act as a transport system for antigen-presenting cells to secondary lymphoid tissues for antigen recognition and intiation of the adaptive immune response
Location of clonal selection
Production of leukocytes including lymphocytes in primary lymphoid tissues
Absorption of fatty acids from the digestive system
Removal of fluid from tissues
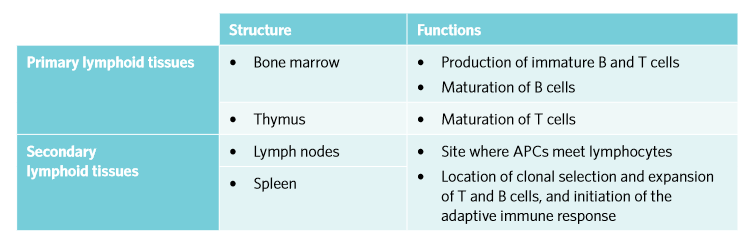
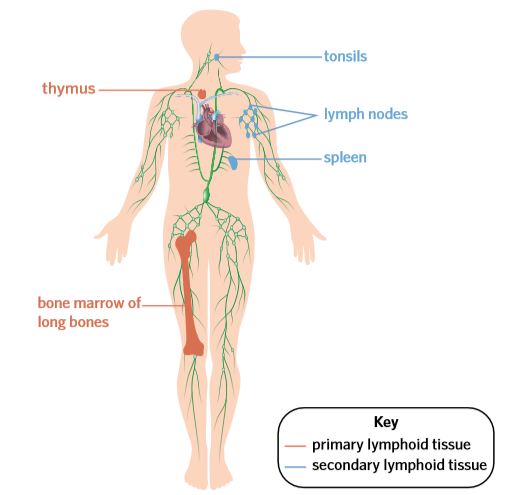
Primary lymphoid tissues:
Main primary lymphoid tissues: Bone marrow and thymus
B and T lymphocytes are produced in bone marrow
B lymphocytes mature in bone marrow
T lymphocytes leave and mature in thymus
Secondary lymphoid tissues:
Matures lymphocytes and initiates adaptive immune response
Main secondary lymphoid tissues: Lymph nodes (tonsils) and spleen
Mature lymphocytes ‘scan’ passing lymph for prescene of antigen-presenting cells or pathogens
If foreign antigen is found and matches receptors on specific lymphocytes, lymphocytes then undergo clonal selection and differentiation.
Large amount of B and T cells created, resulting in swelled lymph nodes
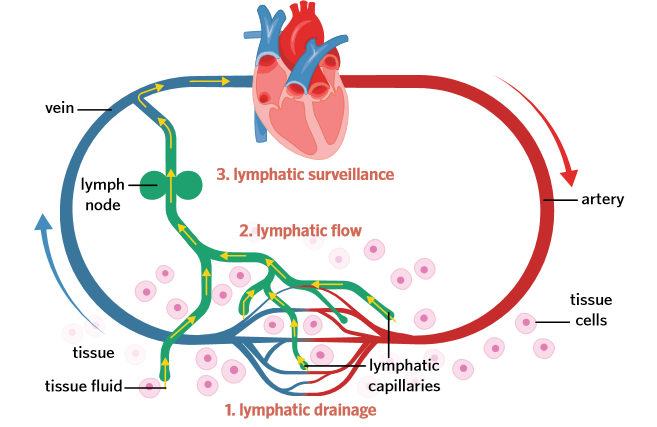
Lymphatic capillaries are small vessels that collect fluid in tissues as well as pathogens then carry it to lymph nodes. Capillaries join together to form vessels.
Lymphatic vessels use muscle movement to squeeze the vessles in one direction, so that the lymph moves away from tissues and to lymph nodes. Transports through afferent lymphatic vessels
At the lymph nodes, the lymph travels through B and T cell clusters and it drains through the clusters. This makes it more likely for pathogens and antigen-presenting cells to meet with a lymphocyte that has a matching antigen-binding site.
If immune response is activated, lymph travels away from lymph nodes through efferent lymphatic vessels. Lymph returns to circulation