My Ultrasound tutor- Pancreas
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
53 Terms
Two types of function for the pancreas
Endocrine and exocrine functions
Exocrine gland
Acts as a Digestive role
Made by acinar cells.
Produces digestive enzymes
Types of acinar cells
-Amylase
-Lipase
-Sodium bicarbonate
-Trypsin
Endocrine function
Acts as a Hormone role
Controlled by Islets of Langerhans, which are clusters of hormone-producing cells:
Alpha cells → make glucagon (raises blood sugar)
Beta cells → make insulin (lowers blood sugar)
Delta cells → make somatostatin (regulates other hormones)
Easy way to remember exocrine and endocrine function
EXOcrine= EXIT thru ducts
ENDOcrine= INTO the blood
Main pancreatic duct
AKA duct of Wirsung
-Travels the length of pancreas and terminates when it meets with the CBD at the ampulla of Vater
-Empties via sphincter of Oddi (major)
Accessory duct
AKA duct of Santorini
-Branch of main empties via minor sphincter into duodenum
Vascular supply
Gastroduodenal artery supples head (seen anterolateral aspect of head)
Splenic artery and SMA supply body and tail
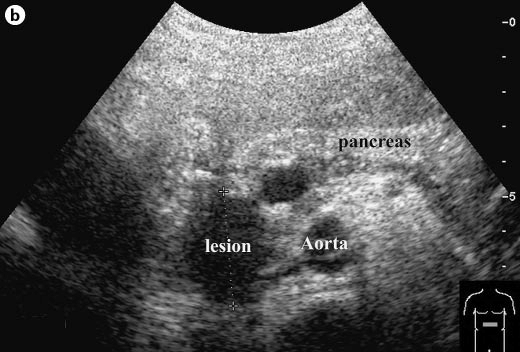
Sonographic appearance of the adult pancreas
Adult pancreas normally echogenic liver, isoechoic to the spleen
Sonographic appearance of the pediatric pancreas
Pediatric pancreas normally can be hypoechoic to liver
Sonographic appearance of the main pancreatic duct
Main pancreatic duct less than or equal to 2mm
May be see perpendicular to sound beam at level of body
-Color can be used to confirm its not the the splenic artery
In transverse pancreas head:
GDA: anterolateral aspect
CBD: posterolateral
Anatomical relationships:
-IVC
Posterior to head
Anatomical relationships
-Duodenum
Lateral to head
Anatomical relationships
-Portal confluence (or SMV)
Medial to head/ anterior to uncinate process/ posterior to neck
Anatomical relationships
-Splenic vein
Posterior to body/tail
Anatomical relationships
-Splenic artery
Superior to body/tail
Anatomical relationships
-SMA
Anterior to aorta/ posterior to pancreas body and splenic vein
Anatomical relationships
-left renal vein
Posterior to SMA
Anterior to aorta
Anatomical relationships
-right renal artery
Posterior to IVC
Variants
Divisum
Annular
Divisum
Most common
Shortened main pancreatic duct, forces accessory duct to become primary drainage= increases risk dilated duct and pancreatitis
Annular
pancreas head wraps around duodenum like a ring, may lead to bowel obstruction
What is the most common cause of acute pancreatitis
Choledocholithiasis (gallstones)
Causes of acute pancreatitis
Choledocholithiasis (gallstones)
Alcoholism
Trauma
How is the inflammation caused in acute pancreatitis?
The pancreas makes digestive enzymes (like amylase and lipase) that help break down food.
Normally, these enzymes are stored in an inactive form inside the pancreas and are only activated once they reach the small intestine.
In acute pancreatitis, something (like a gallstone or alcohol) disrupts the normal flow of these enzymes.
As a result, the enzymes may become activated too early—inside the pancreas instead of the intestine.
These active enzymes start to "digest" the pancreas itself, damaging its tissue.
This damage leads to inflammation
Labs associated with acute pancreatitis
-Amylase rises first
-Lipase within 72 hours but more specific for pancreatitis
Most common vasculature complications of acute pancreatitis
-Splenic vein thrombosis
-Splenic artery pseudoaneurysm
Clinical findings of acute pancreatitis
Acute -itis symptoms:
-Fever
-Pain
-Leuko
-Elevated amylase and lipase
-Elevated biliary obstructive labs if caused by stone
Sonographic appearance of acute pancreatitis
Initial= normal
If findings= hypoechoic, enlarged, phlegmon (perioancreatic fluid), pseudocyst (most common in lesser sac), possible ductal dilation
Phlegmon vs pseudocyst
Phlegmon: peripancreatic fluid
-rim of fluid surrounding pancreas, not encapsulated and only with acute
Pseudocyst: encapsulated fluid collection most commonly found in lesser sac
-Can be with acute and chronic
Chronic pancreatitis
Repeated bouts= damaged organ
-Not the active infection
Most commonly found in cases of pancreatitis caused by alcohol abuse
Clinical findings of chronic pancreatitis
Jaundice
Abnormal labs
Weight loss
Sonographic appearance of chronic pancreatitis
heterogeneous
Hyperechoic with calcifications
Possible pseudocyst
Possible ductal dilatation

Pancreatic adenocarcinoma
AKA ductal adenocarcinoma
Most common primary pancreatic cancer
Most common location is the head= related to biliary dilatation
Treatment for pancreatic adenocarcinoma
Whipple procedure: Removes pancreatic head, duodenum, gallbladder, and bile duct
Courvoisier gallbladder
This refers to an enlarged, palpable gallbladder that can be felt during an exam, often due to a mass in the pancreatic head blocking bile flow. This is considered a classic sign of pancreatic cancer.
-Associated with painless jaundice
Clinical findings of pancreatic adenocarcinoma
Weight loss, abnormal Labs= ALP (Alkaline Phosphatase), conjugated bilirubin
Sonographic appearance of pancreatic adenocarcinoma
Hypoechoic mass
Dilated ducts
Possible enlarged gallbladder
Pancreatic cystadenomas and cystadenocarcinoma
These are cystic (fluid-filled) tumors in the pancreas, and they come in two types: Serous and mucinous
Most commonly in body and tail
Serous
(Microcystic)
-Benign
Mucinous
(Macrocystic)
-May be malignant
Clinical findings of pancreatic cystadenomas and cystadenocarcinoma
Weight loss
Pain
Sonographic appearance of pancreatic cystadenomas and cystadenocarcinoma
Cystic or multilocular cystic mass
Islet cell tumor
These are endocrine tumors of the pancreas, meaning they originate from hormone-producing cells (the Islets of Langerhans).
Most are benign, but since they produce hormones, they can cause symptoms due to hormonal imbalances.
Types of islet cell tumor
Insulinoma
Gastrinoma
Insulinoma
More common out of the two
Causes hypoglycemia (low blood sugar) because too much insulin is being produced.
Gastrinoma
Produces excess gastrin, a hormone that increases stomach acid production.
This can lead to Zollinger-Ellison syndrome, which causes peptic ulcers or stomach ulcers due to too much stomach acid
Pancreatic cysts
Benign
Associated with other conditions:
-von Hippel-Lindau or renal cystic diseases
Pancreatic transplant
Pancreatic transplants are often done for people with severe Type 1 Diabetes (T1DM), where the endocrine function of the pancreas (insulin production) has failed.
Types of Exocrine Drainage in Pancreatic Transplants
-exocrine enteric drainage
-exocrine bladder drainage
Signs of rejection for a pancreas transplant
Increase RI in artery
Exocrine enteric drainage
Most common
Donor duodenum to recipient jejunum RUQ
Exocrine bladder drainage
The donor pancreas is connected to the urinary bladder instead of the small intestine. This is a less common technique.