pathopharm 3: exam 2: intracranial regulation: spinal cord disorders and emergencies
1/100
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
101 Terms
what is the blood brain barrier
§ Specialized endothelium present in brain capillaries
§ Permits selective entry of substances
· Tight junctions between endothelial cells
· Few pinocytotic vesicles
· No fenestra
· Active transport
substances that can cross the blood brain barrier
· Highly lipophilic substances cross directly
· Water crosses membrane by simple diffusion
· Most nutrients cross barrier by facilitated diffusion
what is cerebral autoregulation
autoregulatory mechanisms fail; loss of match between O2 supply and demand of tissues
what is intracranial pressure
pressure exerted by brain tissue, blood, and CSF (contents of the cranium)
what is monro-kellie hypothesis
If the volume of one component of intracranial pressure increases slightly, it is offset by reduction in volume of the other two
-a brain tumor increases volume of brain tissue
-blood and CSF volume reduced in response
causes of intracranial pressure
-brain volume
-CSF
-blood volume
-other causes
how does brain volume cause ICP
brain edema, hemorrhage, tumor, abscess, infart
how does CSF cause ICP
increased production, choroid plexus tumor, hydrocephalus, meningeal inflammation
how does blood volume cause ICP
increased cerebral blood flow, venous stasis, elevated central venous pressure
what are the other causes of ICP
idiopathic intracranial HTN, skull deformities, tetracycline use
hx assessment for spinal cord injury
§ How injury occurred
§ Mechanism of injury
§ Pre-hospital care
physical assessment/S/S for SCI
-priority is ABCs
-spinal shock
what is spinal shock
complete but temporary loss of motor, sensation, reflex, and autonomic function that often lasts less than 48 hours but may continue for several weeks
what is the first priority after an SCI
respiratory status
respiratory status for SCI
§ involuntary respirations can be affected d/t a lesion at or above the phrenic nerve or swelling from a lesion immediately below C4; lesions in cervical or upper thoracic area will also impair voluntary movement of muscles used in respiration (increase in depth or rate)
§ Provide O2 and suction PRN
§ Assist with intubation and mechanical ventilation if necessary
§ Assist the pt to cough by applying abd pressure when attempting to cough
§ Teach pt about incentive spirometer use and encourage the pt to perform coughing and deep breathing regularly
neurogenic shock from SCI
· Complication of spinal trauma, causes a sudden loss of communication within the sympathetic nervous system that maintains muscle tone in blood vessel walls
· Neurogenic shock can occur within 24 hours of a SCI, resulting in peripheral vasodilation that leads to venous pooling in the extremities, a drop in cardiac output and heart rate, and a life-threatening decrease in BP
· Can last several days to weeks
interventions for neurogenic shock
o Ensure proper positioning of the pt by stabilizing the spinal cord following an injury
o Monitor for hypotension, bradycardia, dependent edema, loss of temp regulation (abrupt onset of fever)- common s/s
o Pts who experience neurogenic shock are at greater risk for development of venous thromboembolism (VTE)
§ Monitor for manifestations fo VTE (swelling of extremity, absent/decreased pulses, and areas of warmth/tenderness)
§ Pt may be on anticoagulants to prevent development of lower extremity emboli
muscle tone for pts with upper motor neuron injuries (above L1 and L2)
convert to a spastic muscle tone after neurogenic shock
muscle tone for pts with lower motor neuron injuries (below L1 and L2)
convert to a flaccid type of paralysis
interventions for muscle strength and tone after SCI
§ Encourage active ROM when possible and assist with passive ROM if pt lacks all motor function
§ Muscle spasticity can be so severe that pts develop pressure injuries- can make sitting in a wheelchair very difficult
§ Muscle spasms can be painful for some pts while others do not feel pain
can pts with complete injuries regain mobility
no
can pts with incomplete injuries regain mobility
can regain some function that will allow mobility with various types of braces
-functional mobility can still be best attained through the use of a wheelchair
what needs to be stabilized to prevent further injury in SCI's
head and neck
-cervical collars
-use log roll technique when transferring
-maintain traction if prescriped
common traction for SCI's
skeletal and halo
what may pts with high levels of SCI experience when in an upright position
postural hypotension
prevention of postural hypotension in high levels of SCI
o Raise HOB and be ready to lower the angle if the pt reports dizziness
o Transfer the pt into a reclining wheelchair with the back of the wheelchair reclined
o Be ready to lock and lean wheelchair back onto knee to a fully-reclined position if the pt reports dizziness after the transfer
o Do not attempt to return the pt to the bed
how to prevent secondary SCI
reduce and immobilize fracture
how to reduce and immobilize fracture to prevent secondary SCI
· External fixation
· Surgical intervention
· Hard collar
· Halo crown
· Med management
o PPI
o Muscle relaxants
o Celecoxib
· Surgical management
what is a TBI
head trauma
components of mild head trauma
· Loss of consciousness seconds to minutes
· Amnesia or loss of memory of event
· Change in mental status at time of event
· Persistent or transient focal neurologic deficit
· Sensitivity to light
· N/V
· GCS score 13-15
components of moderate/severe head trauma
· GCS score 9-12 (mod), less than 9 (severe)
· LOC for minutes to hours
· Seizures
· Extremity weakness and coordination challenges
· Aggression, depression
· Difficulty understanding, communicating, or concentrating
· Mortality rates very low
· Long-term disabilities as high as 50%
· Occur 1-2 days after TBI : ^^^^
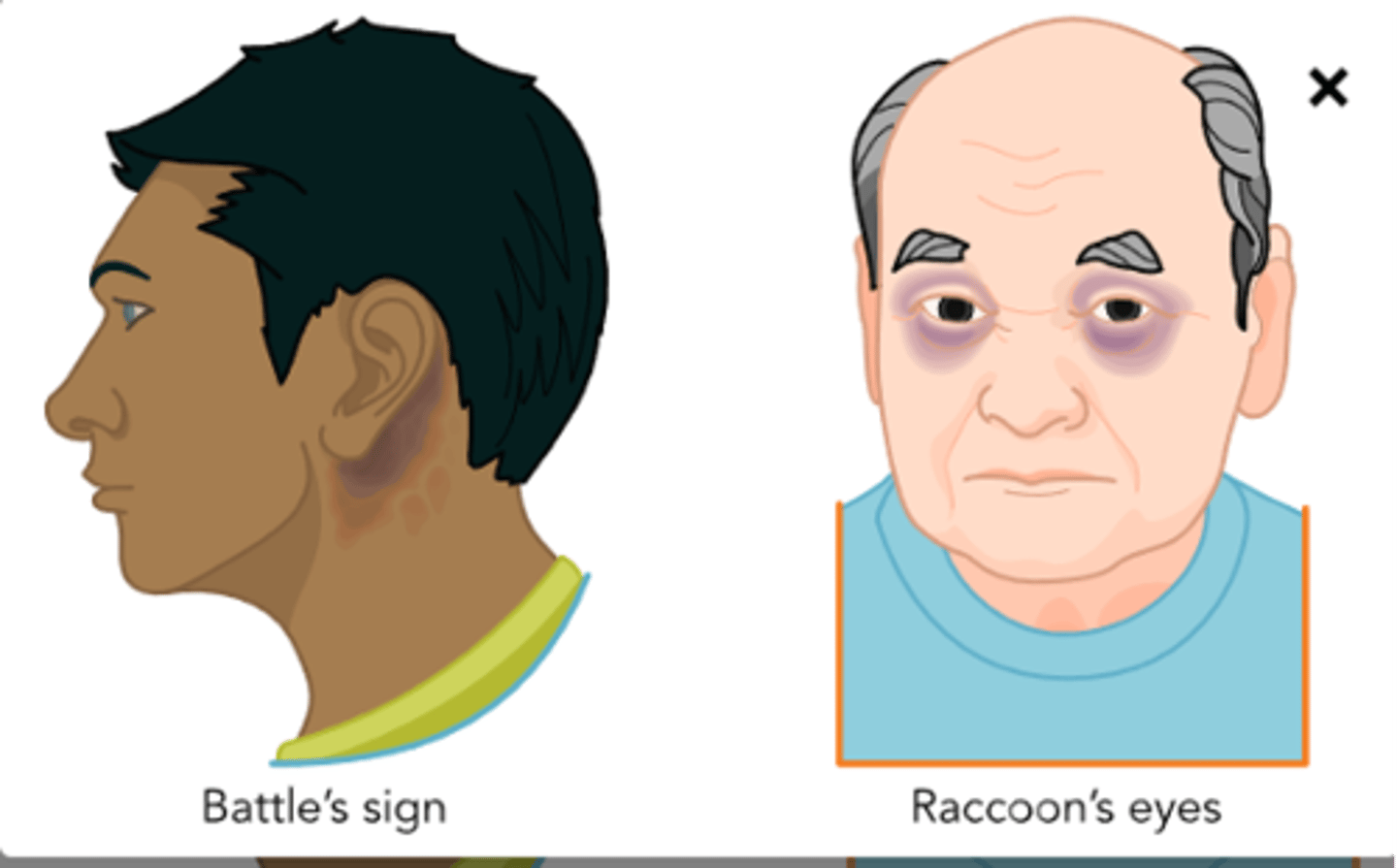
signs of severe head trauma
what is a TIA
temporary episode of neurologic dysfunction --> caused by focal brain, spinal cord, or retinal ischemia without acute infarction --> resolves in 1-24 hours
etiology/pathogenesis of TIA
-same as ischemic stroke
-clot blocking blood supply to region of brain
-atherosclerosis
TIA
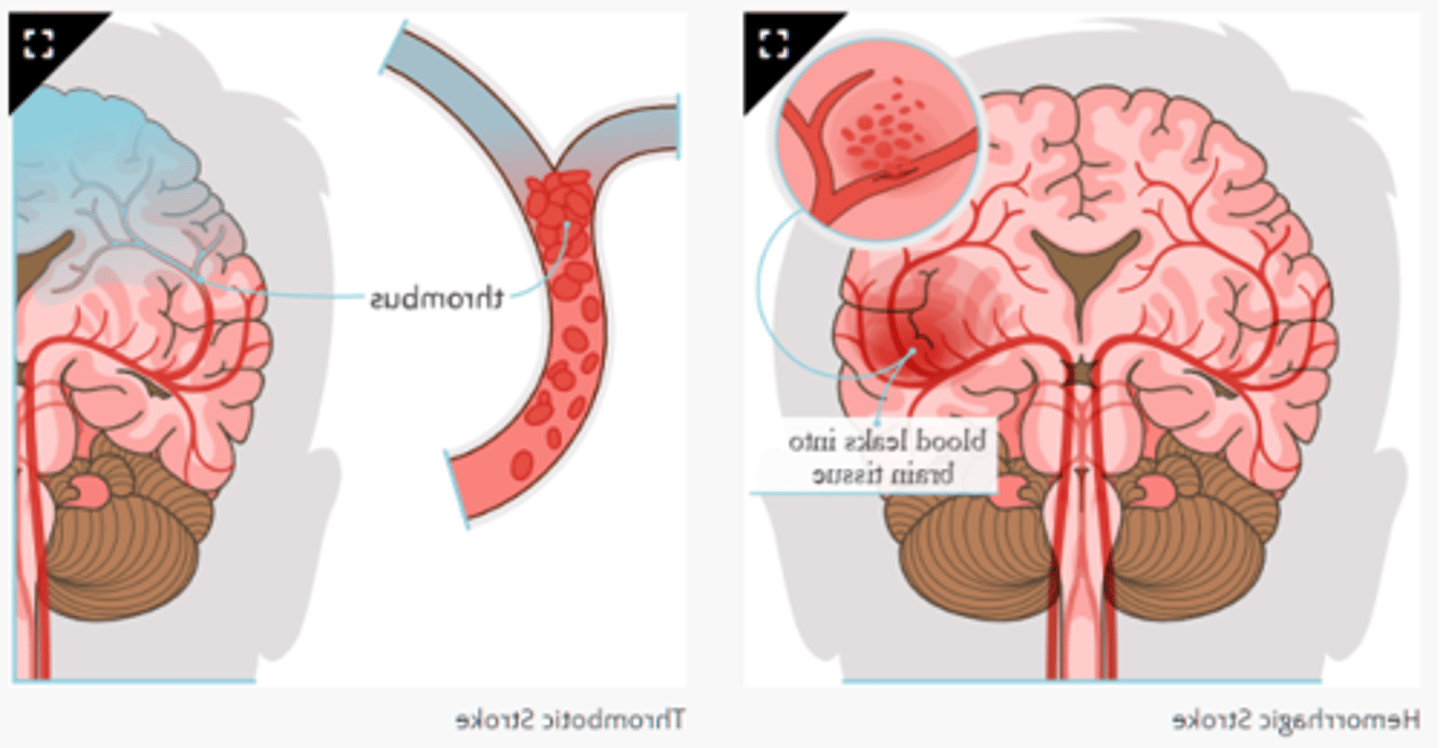
what is the most common type of stroke
ischemic stroke
what is a stroke
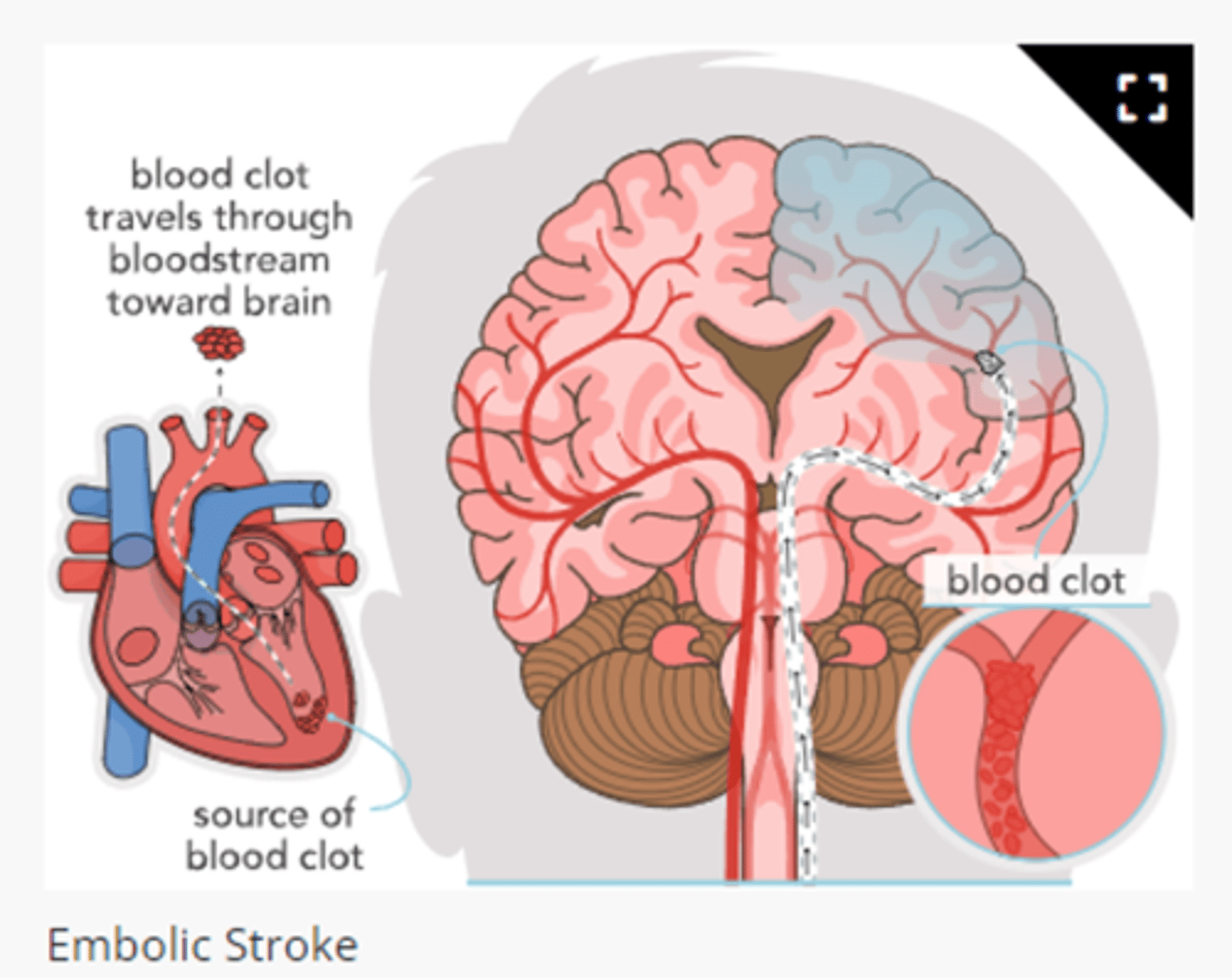
interruption in blood supply to region of brain/bleeding of vessel resulting in brain tissue damage or infarction
hemorrhagic stroke
embolic stroke
nonmodifiable risk factors for stroke
§ Age
§ Family hx
§ Prior TIA/stroke
§ Race
§ Sex
§ Sickle cell disease
modifiable risk factors for stroke
§ CVD
§ CAD
§ Diabetes
§ Excess weight
§ HTN
§ High cholesterol
§ Cigarette smoking
§ Heavy drinking
§ Physical inactivity
§ Poor nutrition
§ Use of birth control pills
s/s of right cerebral hemisphere stroke
-visual and spatial awareness and proprioception
-disoriented
-impulsivity and poor judgement
-depression, anger, and quick to become frustrated
-ataxia
-loss of depth perception
-left sided weakness/paresthesia
what is ataxia
decreased coordination/loss of balance
s/s of left cerebral hemisphere stroke
-speech, language, mathematic skills, analytic thinking
-alexia
-agraphia
-agnosia
-expressive and receptive aphasia
-right-sided weakness and paresthesia
what is alexia
reading difficulty
what is agraphia
writing difficulty
what is agnosia
unable to recognize familiar objects
etiology/pathogenesis of ischemic stroke
partial or complete occlusion of cerebral blood flow d/t thrombus or embolus
where do most embolisms come from
cardiac origin
-atherosclerosis
-Afib
-breakage of atherosclerotic plaque from carotid artery
most common cause of ischemic stroke
emboli that pass through carotid arteries typically occlude the middle cerebral artery
less common cause of ischemic stroke
emboli that pass through vertebral or basilar arteries lodge at the apex of the basilar artery or posterior cerebral arteries
etiology/pathogenesis of hemorrhagic stroke
· Bleeding into brain from burst blood vessel
o Intracerebral
o Intraventricular
o Extracerebral
· Subarachnoid hemorrhage
· Cerebral aneurysm
· Arteriovenous malformations (AVMs)
· Hematologic conditions that increase stroke risk:
o Thrombocytosis
o Hypercoagulable states- meds
non-surgical tx for hemorrhagic stroke
-priority of care depends on adequate ventilation and management of BP (reverse meds)
-osmotic diuretics (mannitol) decrease intracranial pressure
-glucose is monitored and normoglycemia maintained
surgical tx for hemorrhagic stroke
· Surgical evacuation for supratentorial intracranial hemorrhage
· Craniotomy for lobar and cerebellar hemorrhages
· Craniotomy with aneurysm clipping for aneurysmal subarachnoid hemorrhage
s/s of hemorrhagic/ischemic stroke
FAST
-facial drooping
-arm weakness
-speech impairment
-time to call 911
how to assess facial drooping
ask pt to smile- look for unilateral facial drooping
how to assess for arm weakness
ask pt to raise both arms- look for downward drift
how to assess for speech impairment/difficulty speaking
ask pt to repeat a simple phase- listen for unexpected findings such as slurred speech
s/s of hemorrhagic and ischemic stroke
-FAST
-sudden confusion, trouble speaking or understanding others
-sudden numbness/weakness in face, arm, or leg
-sudden trouble seeing in one or both eyes
-sudden dizziness, trouble walking, or loss of balance/coordination
stroke dx
· Exclusion of conditions that mimic TIA
· Blood glucose
· CBC, coag panel
· Electrocardiography
· Non-contrast CT
· MRI with diffusion-weighted image
· CT angiography/ magnetic resonance angiography
· Carotid doppler
· Dysphagia screening
joint commission core measures for stroke
· VTE prophylaxis
· Thrombolytic therapy
· Reevaluation of antithrombotic therapy
· Provide and document stroke education
· Determine the need for rehab
what is aphasia
cerebral hemisphere damage resulting in speech or language problems
types of aphasia
expressive, receptive, mixed/global
what is expressive aphasia
broca/motor
-motor speech problem
-pt can understand what is being said but cannot speak
what is receptive aphasia
Wernicke/sensory
-pt cannot understand the spoken or written word
what is mixed/global aphasia
reading and writing are equally affected
what is proprioception
body position sense and/or peripheral sensation to be free from injury
what is unilateral neglect
· most common with right cerebral stroke
o Teach the pt to touch and use both sides of the body
o Remind pt to dress the affected side
o Turn head from side to side to expand the visual field
o Place objects within field of vision
o Support affected arm: subluxation can occur from weight of arm
tx of ischemic stroke
-restoration of blood flow and reducing area of infarction
-penumbra
-know when symptoms started
-supplemental O2 (maintain 94%)
-frequent VS
-glycemic control
what is penumbra
tissue surrounding infarction
med therapy for ischemic stroke
-fibrinolytic therapy
-anticoagulants
-anti-HTN therapy
-cholesterol lowering agents
components of fibrinolytic therapy
-tissue plasminogen activator (t-PA)
-give within 45 mins
-can be within 3-4.5 hours
components of anti-coagulants
o Warfarin
o Dabigatran, apixaban, ribaroxaban
o Aspirin, clopidogrel
anti-htn therapy for ischemic stroke
ACE inhibitors, diuretics, CCB
components of cholesterol lowering agents with ischemic stroke
o Hypothermia
o Elevate HOB to 30 degrees to reduce ICP
o Seizure precautions
o NIHSS scoring
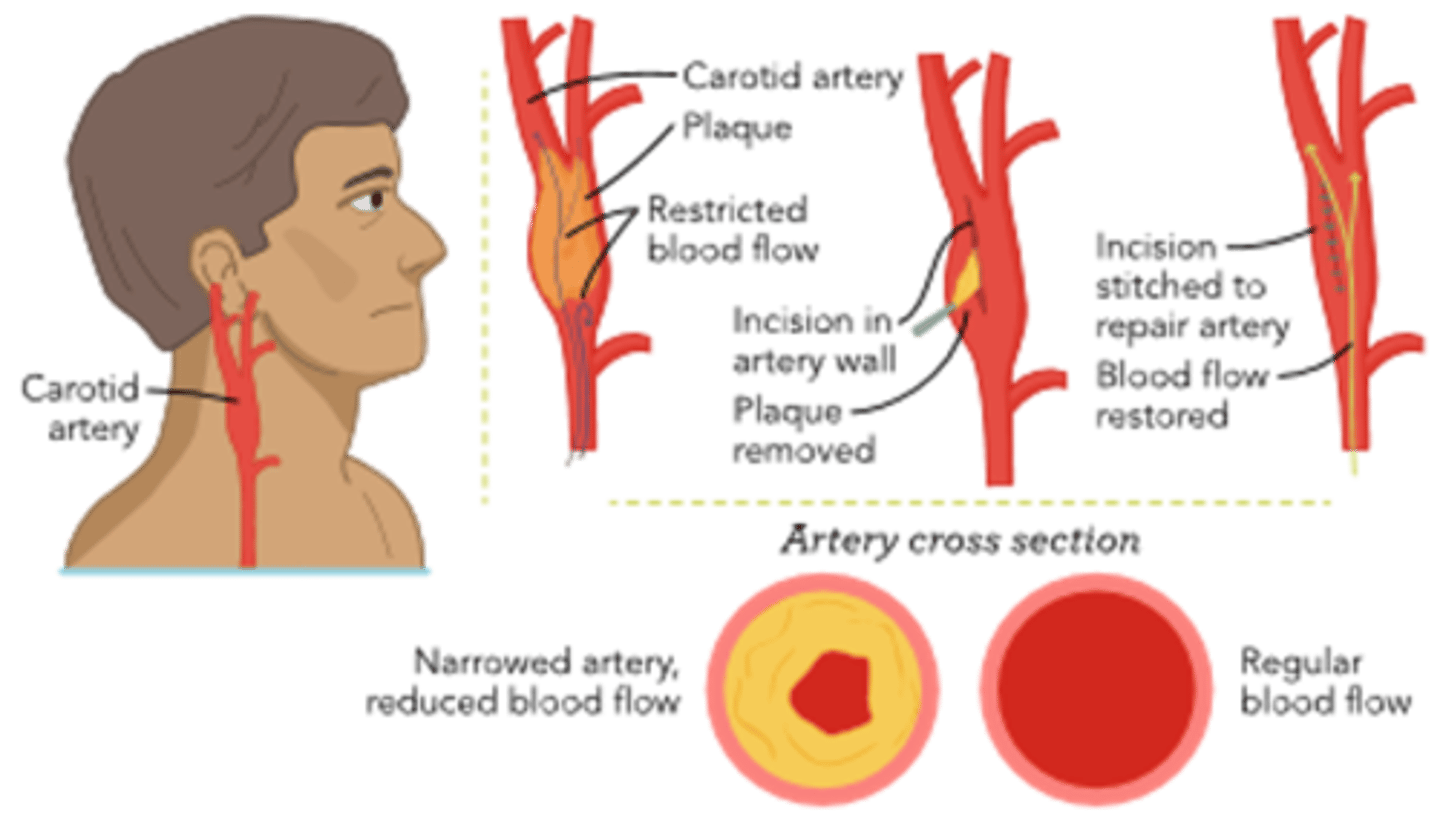
surgical interventions for ischemic stroke
-thrombectomy
-carotid artery angioplasty with stenting
-extra-cranial bypass
-carotid endarterectomy
types of thrombectomy
mechanical, endovascular, intra-arterial
components of carotid artery angioplasty with stenting
o involves inserting a catheter in the femoral artery and placing a distal/embolic protection device to catch clot debris during the procedure while a stent is being placed in the carotid artery to open a blockage
§ CAS is less invasive, blood loss is decreased, and length of hospitalization is shorter
§ Post op care is same as carotid endarterectomy
components of extracranial-intracranial bypass
o craniotomy performed to improve cerebral perfusion following a stroke or for pts who have had a TIA that is likely to progress to a stroke
§ Can decrease blood flow around a blocked artery and can help restore blood flow to affected areas of that brain
components of carotid endarterectomy
o opens the artery by removing atherosclerotic plaque
§ Performed when carotid artery is blocked or when pt is experiencing TIAs
§ Assess for increased HA, neck swelling, and hoarseness of voice
§ Have emergency airway equipment available for use
s/s of increased ICP
§ Change in LOC
§ Change in GCS- decreasing score
§ Change in motor and sensory function
§ Change in breathing pattern
§ Trends in VSagitation
§ Impending doom
early signs of ICP
-HA, N/V
-confusion
-blurred/double vision
late signs of ICP
-cushing's triad
-pupils fixed and dilated
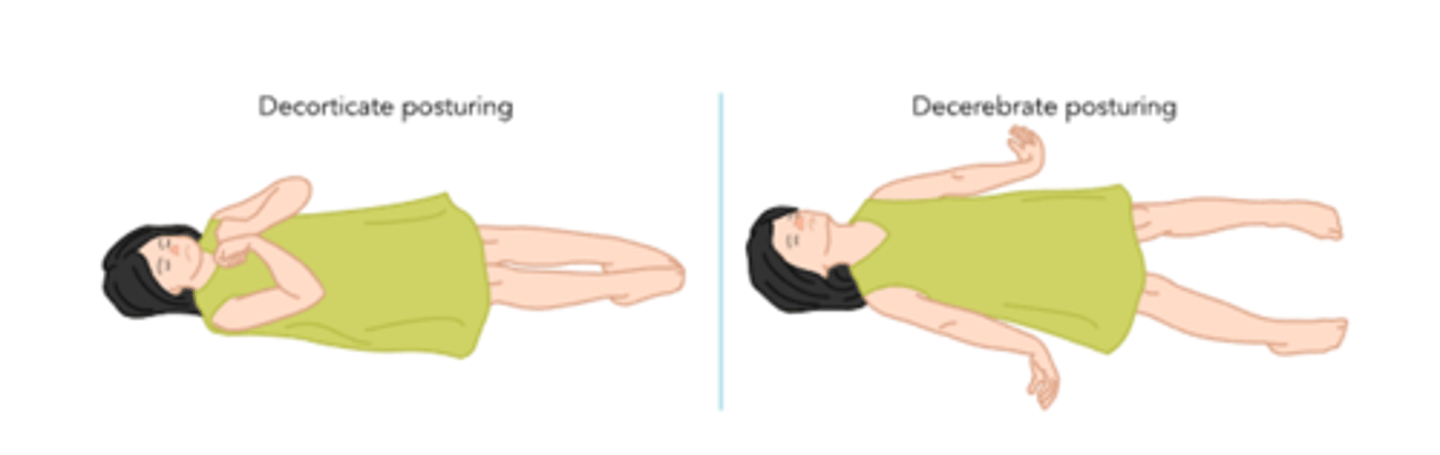
-posturing (decorticate/decerebrate)
-coma
what. is cushing's triad
widening of pulse pressure, bradycardia, irregular breathing patterns
decorticate/decerebrate posturing
interventions for increased ICP
§ ABC
§ Keep CPP >60 mmHg
· HOB 30-45 degrees
§ Maintain shunt
§ Sedation and analgesic
§ Skin integrity
§ Adequate nutrition: parenteral or enteral feedings
§ Prevent secondary injury
meds for increased ICP
§ Diuretics, osmotic agents
§ Sedation
§ Pain control
§ Barbiturates
§ Neuromuscular blocking agents
surgical tx for increased ICP
§ Hemicraniectomy
§ Ventriculostomy
§ Subarachnoid bolt
etiology/pathogenesis of post-concussive syndrome
persistence of symptoms following injury; may occur after TBI of any severity
s/s of post-concussive syndrome
· Lightheadedness
· Vertigo
· HA
· N/V
· Photophobia
· Cognitive and memory dysfunction
· Tinnitus
· Blurred vision
· Difficulty concentrating
· Amnesia
· Fatigue
· Personality change
· Balance disturbance
tx for ICP and subarachnoid hemorrhage
§ Mannitol, hypertonic saline, and barbiturates
§ Sedation and pain management: fentanyl and propofol
§ Seizure prophylaxis: start within 7 days of injury
§ Fever control- acetaminophen
§ Other: PPI, DVT prophylaxis, and insulin
§ Surgical:
· External ventricular drains or cistern ostomy
· Decompressive craniectomy
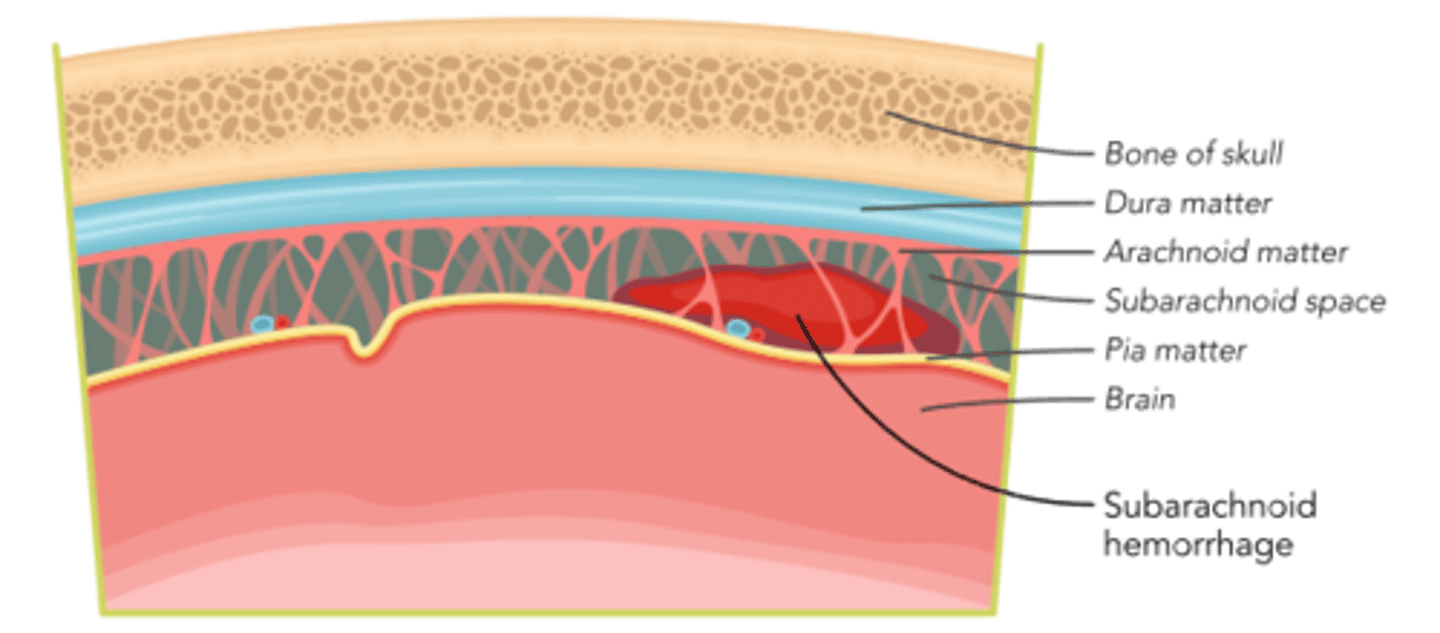
what is a subarachnoid hemorrhage
-blood enters space (arachnoid and pia membrane)
-initiates signaling cascade
-initiate multiple damaging processes within the brain; including disruption of the blood-brain barrier and damage brain cells
s/s of subarachnoid hemorrhage
-early brain injury, such as transient cerebral ischemia occurs within minutes of injury
-ICP begins increasing rapidly, decreasing the CPP and leading to reduced cerebral blood flow
-cerebral vasospasm typically can occur within 3 days after SAH and can continue for three weeks
optimal care guidelines for SAH
-reduce 1 year mortality
-admin of anti-HTNS (SBP greater than 160)
-admin of nimodipine
-coiling or clipping of ruptured aneurysm
pharm tx for SAH
o Antifibrinolytic therapy: tranexamic acid (TXA)
o Anti-HTN: CCB (nicardipine)
o Managing Vasospasms: CCB (Nimodipine)
o Anticonvulsants levetiracetam (Keppra)
o Anti-pyretic (acetaminophen)
o Managing hypotension norepinephrine (levophed)
surgical tx for SAH
o Clipping the rupture aneurysm: clip is placed on the neck of an aneurysm to prevent further blood flow
o Endovascular coiling: an aneurysm entails inserting a microcatheter into the femoral artery with a coil attached to the tip
hyperbaric O2 therapy for SAH
· using increased amount of atmospheric pressure and breathing of increased O2 amounts
o HBOT can also help improve cognitive functions, such as memory, executive function, attention, and motor skills
SAH
goals for end of life care
-managing symptoms of distress
-pain
how to manage symptoms of distress during end of life care
-pain
-weakness
-breathlessness/dyspnea
-N/V
-agitation/delirium
-seizures