Bio 155 - Skeletal Muscle: Anatomy & Excitation + Contraction + Force, Work, and Energy
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
24 Terms
What are skeletal muscles?
organs organized from smaller units
Describe the arrangement of thin and thick filaments in a sarcomere in terms of A&I bands
Describe Z&M lines in terms of the key biochemical features of thin and thick filaments
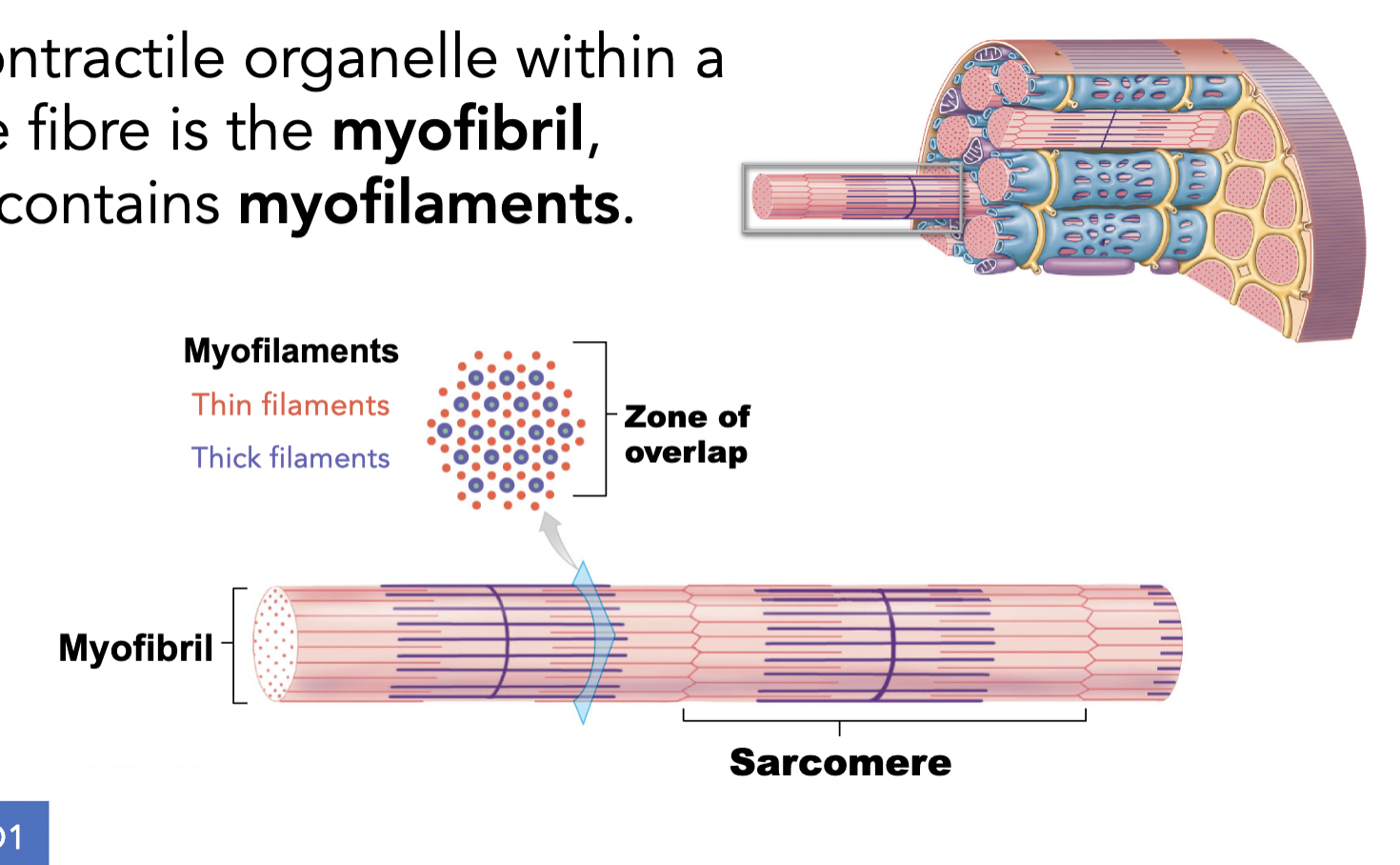
What is the contractile organelle within a muscle fibre? How are they organized?
the muscle fibre in a contractile organelle is called the myofibril, which contains myofilaments
these myofilaments are organized into repeating units called sarcomeres
Define the properties of muscle tissues, including key features shared between its subtypes
muscle tissues: contract and produce mechanical forces (ex. walking)
3 subtypes
skeletal muscle tissue: moves the skeleton (this is our focus for lecture 6-8)
cardiac muscle tissue: pumps blood through the heart
smooth muscle tissue: blood vessels, digestive tract, and many more
Describe the organization of a skeletal muscle and the tissue types that it contains, including the relationship of muscle fibres to fascicles, and muscles to fascial compartments.
each skeletal muscle is connected to the skeletal system via tendons (or aponeuroses)
skeletal muscles are organized within layers of FASCIAE = connective tissue around ur bone that provides support
skeletal muscle —> muscle fascicle —> muscle fiber
5 main anatomical components of the musculoskeletal system (muscle, bone, tendons, ligaments and cartilage) in terms of tissue type and give examples of their roles
the skeletal and muscular systems are connected by a variety of connective tissue structures
cartilage
supportive connective tissue
found on joint surfaces, ears, nose, and vertebral disc (in between vertabrae)
ligaments
dense regular connective tissue
anchor bones to other bones
tendons
dense regular connective tissue
anchor bones to muscles
compare and contrast the gross anatomy and histology of bone and cartilage, including the composition of the matrix and diversity of distinct cell types
both bone and cartilage are connective tissues (meaning they both have dense, solid matrix)
bones
their matrix (the ground substance) contains collagen, calcified and hydroxyapatite (calcium and phosphate perticpiated); more rigid
compact bone around the outside and spongy bone inside and on the ends of the bone
compact
always have layers and layers around central holes
lots of solid matrix with little cells in-between layers
dense tissue with hallow tubes
so its COMPACT so its very good at resisting compression
spongy
found on the inside of bone
all bones have a layer of compact bone around the outside and the inside will have hallow spaces filled with meshed work (aka. spongy bone)
doesn’t have as much tissues and matrix, so more spaces making it light and therefore can distribute forces
the hallow spaces in the sponge bone contains bone marrow
bone marrow
is a connective tissue but not a supportive connective tissue, instead it is where blood is created
bone tissues are highly vascularized (blood vessels running anywhere) and innervated (nerves through the bone tissue) and in the hallow spaces have bone marrow
ex. long bone (femur)
endosteum
the space between the spongy bone
endo = inside and osteum =bone
layer of epithelia tissue lining the surface of spongy bone between the bone and bone marrow
periosteum
on the outside of bone
perio = around perimeter, another epithelia layer
bone tissue contains many cell types with distinct roles
osteogenics cells
cells that create new bone tissues and bone cells (the stem cells for bones)
found in the endosteum
osteogenic cells divides then the osteoblasts lays the new bone tissues
osteoblasts
blast = builds
laying down the new bone tissues
MOST are found on the periosteum
once the osteoblasts become embedded in the bone matrix they become mature cells called osteocytes
osteocytes
mature bone cells
maintain bone matrix and do a little of modification but can’t lay down lots of new matrix at one time like osteoblasts
found in the bone matrix, lacunae
osteoclasts (maintains calcium levels)
clasts = clashes / removes bone matrix by dissolving it —> can make it rapidly
breaks down bone tissue by secreting acids and enzymes that dissolve the mineralized bone matrix, which contains calcium and phosphate
and as the bone matrix is broken down, calcium is released into the blood stream which helps increase blood calcium levels when they are low
found in the endosteum
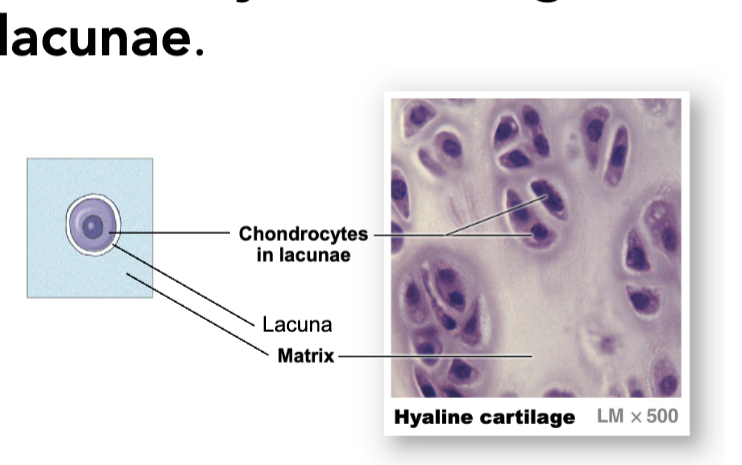
cartilage (cartilage are alrd matured, bc theyre not laying down new cartilage)
their matrix contains proteoglycans (glycoproteins which include chondroitin sulfates): more flexible, not as rigid as bone
cartilage are avascular (meaning no blood tissue)
all forms of cartilages contains cells called chondrocytes (cells responsible for cartilage formation)
chondrocytes resides in lacunae (the little holes in the matrix)
three subtypes of cartilage that differs in extracellular fibre composition
hyaline cartilage
lots of proteoglycans
will look smooth and glassy bc it absorbs water
found on joint surfaces
elastic cartilage
proteoglycans + elastin fibres
flexible and springs back and will look dark in histology
found in your ears and nose
fibrocartilage
proteoglycans + collagen fibres
not a connective tissue
found in vertebrae discs
bit more tougher, handles squishing better, not very smooth/slidy BUT ITS TUFF
compare and contrast the different mechanisms of growth that occur in bones and in cartilaginous tissues, including how these processes alter following puberty
cartilage
can grow through two methods
cell division / growth proliferation (interstitial growth):
chondrocytes undergoes division
additional matrix secreted pushes cell apart
growth by division stops after adulthood
increase the size of cartilage and contributes to lengthening of long bones
differentiation (new layer on top of the top surface, cartilage becomes thicker)
happens in childhood and continues on into adulthood
layers of cartilage is covered by a layer of connective tissue
cells differentiate into chondroblasts, then chondroblasts secrete new matrix and the chonroblasts will mature into chondrocytes
bone
can also grow in 2 diff ways
endochondral growth (means within cartilage)
taking a tissue that was cartilage and turning it into a bone
happens during embryological growth
as fetus grows, the initial skeletal is lay down with hyaline skeleton
as fetus grows and as blood vessels reach the bone, osteoblast colonizes the cartilage and starts growing from the inside and turning into bone tissue
you will grow LONGER
however, once the bone becomes ossified, your bone will stop growing longer
appositional growth (adding layers to the outside surface of the bone)
grows wider
osteoclasts eats away the matrix in the endosteum (the inside) while the osteoblasts add new layers of bone to the surface
this happens so the bone doesn’t get too thick and heavy
exceptions from bone growth
dermal (skull) and sesamoid bones ossify from non-cartilaginous connective tissue
bone tissues grow directly out from your connective tissue proper instead of cartilage
dermal bones ossify from within dermal tissue
sesamoid bones form within tendons
Describe the phases involved in bone repair and compare and contrast the capacity of repair in bone and cartilage
bone
bone tissues repair itself well through a series of stages
bone healing involves the growth of cartilage (only time when cartilage grows in adulthood)
bone repairs starts with forming a new callulus (a cartilage)
will continues to remodel over months to years
cartilage —> spongy bone —> compact
will takes a long time to fully remove cartilage
cartilage
cartilage DOES NOT repair itself well
intersitial growth no longer occurs after puberty
however, appositional growth can occur into adulthood for fibrous and elastic cartilage
activates a dense connective tissue repair process instead of elastic cartilage
ex. piericing ur ear
articular cartilage cannot undergo self-repair at all
therefore, if u damage ur joint surfaces ITS OVER
explain the pathological processes occurring in osteoarthritis and analyze the potential costs and benefits of treating osteoarthritis with total joint replacement
bones is an organ filled with bone tissues
bones are connected to each other using joints (articulations) with diff tissues which produces diff physical properties - 7 diff joints
diarthistis (free movement)
amphiarthrosis (little movement)
synarthrosis (no movement)
synovial joints - the most complex and involve a lot of diff tissues including hyaline cartilage
surfaces of the joins will be covered by a layer of hyaline cartilage called the articular cartilage
articular cartilage is a subtype of hyaline cartilage
has fluids that lubricate the surfaces
osteoarthritis
a degenerative disorder caused by damage to the articular cartilage
which will increase friction at the synovial joint —> inflammation —> more pressure on remaining cartilage —> more damage
explain the role of bone as mineral reservoir, and predict how the activity of the bone cells will respond to changes in body calcium levels
bones act as a mineral reservoir for minerals, specially for calcium
the balance between the amount of osteoblast and osteoclast activity help maintain calcium homeostasis
negative feedback loop
If your calcium level drops, then your osteoclast will increase and your calcium levels will increase
breaking down your matrix will release calcium to your bone
SO1. Describe how tension generation by a muscle can be affected by physiological differences between the types of myofibres that make up a muscle.
type l: generate low force but can sustain tension for long periods
type llA: produce moderate force and are suited for activities requiring both strength and endurance
type llB: generate highest force but fatigue quickly, perfect for short, explosive movements
SO2. Compare and contrast the different mechanisms skeletal muscles use to generate ATP at rest, at moderate activity and at peak activity, including nutrients used to generated ATP, aerobic vs anaerobic pathways, and the production of byproducts.
Muscles get ATP = break down glucoses and other nutrients from either anaerobic or aerobic metabolism
excitation and contraction in skeletal muscles are both a multi-step processes and requires ongoing energy input to maintain
anaerobic
doesn’t require oxygen
takes place in the cytosol of the cell (outside of mitochondria)
fewer steps, so can produce ATP faster, however less ATP produced from a single glucose
only source we can get ATP fromis glucose, and can’t use fatty acids or other sources
aerobic
requires oxygen
takes places in the mitochondria
remember function of mitochondria
needs steady oxygen supply, but will take longer to produce ATP
even tho its slow, it can produce a lot of ATP
can also use fatty acids
phosphocreatine (enzyme)
doesnt need oxygen
very very fast
important bc it stores ATP, but limited
how do they decide on how they’ll obtain their ATP?
resting muscles - aerobic metabolism
moderately active muscles (able to meet ATP demands) - aerobic metabolism
peak activity - anaerobic metabolism (lactate + creatine)
even if oxygen is available, its gonna take too long for aerobic to produce ATP
SO3. Define the term ‘muscle fatigue’ and identify at least two changes in physiological processes that contribute to the onset of fatigue.
muscle fatigue is the reduced contractile tension for the asame (excitation) stimulus
factors that affect excitation processes in skeletal muscle
depletion of ACh vesicle in MN axon terminal
Accumulation of potassium in T-tubules due to repeated APs
factors that affect contracion
leakage of Ca2+ back into sarcoplasm
micotears in myofibrils
build-up of lactate and H+
SO4. Identify the key anatomical and physiological characteristics that distinguish Type I and Type IIA & IIB muscle fibres and analyze how these physiological differences would contribute to performance differences and training effects in an individual.
type I: slow twitch
metabolism: primarily aerobic metabolism, utilizing oxygen for energy production
high fatigue resistance
slow contraction speed = less powerful but more enduring to muscle contractions
ideal for endurance activities (long-distance running, cycling)
type llA (fast-twitch, oxidative)
ultilize both areobic and anaerobic pathways, allowing for more versatile energy production
moderately resistant to fatigue
faster contraction speed than type l fibers, but slower than type llB (ex. team sports)
type llB
primarily anaerobic metabolism, relies on glycolysis for energy production
low fatigue resistance, leading to quick fatigue during prolonged exertion
fastest contraction speed, allowing for powerful bursts of force (ex. sprinting, heavy lifting)
SO5. Describe the patterns by which multiple motor units within the same muscle are used during synchronous and asynchronous recruitment.
synchronous recruitment
all targeted motor units activate simultaneously
maximizes force and speed for short bursts of activity
asynchronous recruitment
motor units activate in a staggered manner
sustains force and delays fatigue during longer-duration activities
SO6. Explain the difference between hypertrophy and hyperplasia in terms of muscle tissue growth and identify which mechanisms occur during adulthood.
hypertrophy: the increase in the size of individual muscle cells (muscle fibers)
mechanism: occurs when muscle cells undergo increased protein synthesis, particularly of actin and myosin filaments, leading to larger muscle fibers
triggered by strength training
occurs in adult hood
Hyperplasia: the increase in the number of muscle cells or fibers
mechanism: involves in the formation of new muscle fibers
does not occur in adulthood
Explain or apply different anatomical or functional rules for how to divide up the nervous system into components (e.g. CNS/PNS/ENS; Sensory/Integrative/Motor; Somatic/Autonomic)
Identify the four compartments of a neuronal cell and explain the basic functions of each compartment in
terms of information flow.
Explain the functions and key structural features of the four functional types of glia, and correctly identify which subtypes of glia are found in the CNS vs the PNS.
Compare and contrast the capacity of neurons in the CNS and PNS for repair, and the roles glial cells play
in neuronal repair
Identify which neuronal compartments and which glial cell types are associated with white vs gray matter
Use information about the organization of white and gray matter to make simple predictions about neurological symptoms arising from damage to different locations in spinal cord (e.g. sensory/motor,voluntary/involuntary)