Immuno Chapter 2- Cells, Organs, and microenvironments of the Immune System
1/116
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
117 Terms
Hematopoiesis
Hematopoietic Stem Cells (HSC)
Myeloid Lineage Cells
Lymphoid Lineage Cells
Primary Lymphoid Organs
sites where immune cells develop form immature precursors
Bone Marrow
Thymus
Secondary Lymphoid Organs
the site where the mature antigen-specific lymphocytes first encounter antigens and begin their differentiation into effector and memory cells
Lymph nodes
Spleen
Barrier Tissues (MALT and skin)
Lymphatic System
Tertiary Lymphoid Tissue
T- Cell zone
B- Cell follicle
Germinal Centers
Fibroblastic Reticular Cell Conduit (FRCC) System
Follicular Dendritic Cells (FDCs)
What does a successful immune response to a pathogen depend on?
a choreographed interaction among diverse cell types.
Innate immune cells
the first line of defense against pathogens
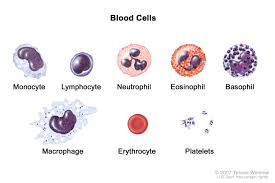
What are the major innate immune cells?
Phagocytic cells
inflammatory and defense cells
cytotoxic innate cells
What are the phagocytic cells and what do they do?
they engulf and destroy pathogens.
neutrophils
monocytes/ macrophages
dendritic cells

What is the function of the neutrophils?
to eat bacteria and die quickly (which forms pus)
these are the most abundant white blood cells (make up 50-70% of the leukocytes)
they’re the first cells to arrive at an infection
Once the neutrophils are released into the blood from the bone marrow, what happens?
they are then released in to the blood to circulate for 7-10 hours, then migrate into the tissues (they only last here for a few days)
leukocytosis
having too many white blood cells in the blood.
too many neutrophils in the bone marrow. - indicated infection
What is the function of the Monocytes?
they eat pathogens, clean up dead cells, and signal other immune cells
they circulate in the blood
they are long- lived
There are two types of monocytes
inflammatory
Patrolling
What is the function of inflammatory monocytes?
they enter tissues quickly in response to infections
What is the function of PAtrolling monocytes?
they crawl slowly along blood vessels, monitoring their repairs
What does monocytes turn into when they enter the tissues?
macrophages
What changes does macrophages undergo once stimulated by the tissue damage or pathogens?
They contribute directly to the clearance of pathogens from that tissue
they act as pAPCs for T-Lymphocytes
Tissue- Specific Macrophage
macrophage that lives in a particular tissue and is specially adapted to work there.
opsonin
a molecule that “tags” a pathogen so immune cells can recognize and eat it more easily.
What are the ways that immature Dendritic cells take in antigens?
engulf it by phagocytosis
internalize it by receptor- mediated endocytosis
imbibe it by pinocytosis
What is the function of the dendritic cells?
they capture antigens and present them to T cells
they act as a bridge between innate and adaptive immunity.
What does phagocytic means?
the ability of a cell to engulf, ingest, and destroy foreign particles, microbes, dead cells, and debris through a process (known as phayogcytosis )
What are some of the inflammatory and defense cells?
mast cells
basophils
eosinophils
What is the function of the mast cells?
they release histamine
they’re found in the tissues (skin, mucosa)
they are important in inflammation and allergies
What does histamine do?
What is the function of basophils?
they release histamine during allergic responses and help with parasites
they’re not phagocytic (they do not engulf other cells/germs)
they circulate in the blood
they stain blue in H&E staining

What is the function of eosinophils?
they are important for parasite defense
they cluster around the parasite and damage their membranes
they’re also involved in allergies and asthma
These cells migrate from blood and into tissues
these stain pink in an H&E staining
Where are the eosinophils mainly located?
small intestines
in other places, they tend to help with asthma and allergy symptoms
they secrete cytokines that regulate B and T lymphocytes- this influences the adaptive immune response
What is the function of Mast cells?
they fight parasitic worms and help with allergies
these are released from the bone marrow and into the blood as undifferentiated cells
These mature AFTER they leave the blood and go into tissues
These are very similar to basophils
What are the cytotoxic innate cells?
the natural killer cells (NK)
What is the function of Natural Killer cells?
the kill virus- infected and cancer cells
these do not need antigen presentation
they can detect abnormal cells missing normal markers
What are the primary lymphoid organs?
the bone marrow and thymus
What are the secondary lymphoid organs?
the spleen, lymph nodes, and specialized sites in the gut and other mucosal tissues
Where are the hematopoietic stem cells located? What are they?
in the bone marrow - self renewing
What does the HSC (Hematopoietic Stem cells) divide into?
Myeloid and lymphoid progenitor cells
Professional Antigen-Presenting cell (pAPC)
a specialized immune cell whose main job is to show pieces of pathogens to T cells to activate them. ( this is just a characteristic of the phagocytic cells)
Why are pAPCs important?
because they form important bridges between both the innate and adaptive immune systems
What are the three major activities that occur when pAPCs encounter pathogens?
they secrete proteins that attract and activate other immune cells
they internalize pathogens via phagocytosis, digest those pathogenic proteins into peptides, then present these peptides on their membrane surface
They upregulate costimulatory molecules(additional signals) that are required for the full activation of helper T cells
What are naive T lymphocytes?
Lymphocytes that have not been activated by binding antigen
What does the myeloid progenitor cell differentiates into once the cell leaves the bone marrow and enters the peripheral tissues?
Dendritic cells and monocytes
While in the bone marrow, what does the myeloid progenitor cells differentiate into?
granulocyte-monocyte progenitor
Eosinophil progenitor
Basophil progenitor
Megakaryocyte
Erythroid progenitor
Mast cell
What does the granulocyte- monocyte progenitor cells eventually differentiate into once the cells mature?
monocyte- which then differentiate into either a macrophage or dendritic cell (once it reaches the tissues)
neutrophils
What does the eosinophil progenitor cells eventually differentiate into once the cells mature?
eosinophils
What does the basophil progenitor cells eventually differentiate into once the cells mature?
basophils
What does the megakaryocyte cells eventually differentiate into once the cells mature?
platelets
What does the erythroid progenitor cells eventually differentiate into once the cells mature?
erythrocytes
Once the Lymphoid progenitor cell matures in the bone marrow, what does it then differentiate into?
a dendritic cell
a innate lymphoid cell
a b-cell progenitor, which then develops into a b-cell
Once the Lymphoid progenitor cell leaves the bone marrow, then enters into the thymus, what happens?
they then mature into the T-cell progenitor, then differentiate into the helper and cytotoxic T cells
What are the two capacities that defines stem cells?
their ability to regenerate/ self renew
their ability to differentiate into diverse cell types
What can embryonic stem cells do?
they can generate almost all of the special cell types in an organism. (Pluripotent )
Pluripotent
A cell that can turn into almost any type of cell in the body.
What can adult stem cells do?
can turn into several different cell types, but only within one specific tissue or system. (multipotent)
multipotent
A cell that can become several different, but closely related, types of cells.
What are tissue specific stem cells? What harbors them?
Stem cells that live in a particular tissue and only make the types of cells needed for that tissue.
multiple adult organs
What was the first tissue- specific stem cell identified? what is it the source of?
Hematopoietic stem cells
erythroid (red blood cells) cells and leukocytes (white blood cells)
Where does HSCs originate and reside? Where can some also be found?
originate in fetal tissues and reside in the bone marrow of adult vertebrates
sometimes in the spleen and liver
What is HSC controlled by?
to keep a balance- cell division, death, and differentiation
quiescent- this happens when the immune system is just being normal.
the HSCs are resting or inactive, but still alive and ready to act if needed.
Progenitor cells
have a limited self renewal capacity and becomes more committed to a particular cell lineage.
What is the relationship of HSCs and age? What does this show?
as age increases, the number of HSCs decreased (that there is a limit to HSCs self- renewal potential)
proliferative capacity
How much a cell is able to divide and make more cells.
What were expressed by the rare HSC population (during the classic experiment box 2-1)? What did this do?
some surface proteins- CD4, Sca-1, c-Kit
this allowed the HSCs to be isolated directly
Pluripotency
The ability of a cell to become almost any type of cell in the body.
What are the most quiescent (inactive but still alive) HSCs? What do they retain throughout the life of an organism?
Long-term HSCs
they retain pluripotency
What type of HSC divide more frequently and happen to have limited self-renewal capacity?
short term- HSCs
What promotes the development of multipotent progenitors (MPPs)?
c-Kit receptor
this is a receptor for cytokine SCF
Multipotent progenitors (MPPs)
early cells that come from stem cells and can turn into several different kinds of related cells, but not forever.
this means that they have a very limited ability to self renew
they also proliferate quickly
they can make lymphoid and myeloid cell lineages
Lymphoid primed, multipotent progenitors (LMPPs)
these cells tend to go into a certain lineage, then will not be able to turn into other cells in different lineages
early lymphoid progenitor (ELP)
a young blood cell that is just starting to commit to becoming an immune cell.
they can leave the bone marrow and enter the thymus (as T-Cell progenitors)
They can stay in the bone marrow as B-cell progenitors
What is the lifespan of a red blood cell?
120 days
What is the lifespan of a platelet cell?
5-10 days
What is the lifespan of a neutrophil? Why?
6 hours to 2 days
this is because they are the first responders and once they eat the germ, they die.
What is the lifespan of a monocyte?
days to months
What is the lifespan of Basophils and Mast cells?
hours to days
What is the lifespan of the lymphocytes? Why?
days to years
this is because they are part of the adaptive immune system, taking note of what germs were previously in the body and how they were fought off- committing them to memory
How can the hematopoietic cells be distinguished visually?
Using hematoxylin and eosin stains or fluorescent markers
What all falls under the myeloid lineage cells?
red blood cells
granulocytes
neutrophils
eosinophils
Basophils
monocytes
macrophages
Are myeloid lineage cells innate or adaptive?
Innate immune cells
When a dendritc cell has captured an antigen, what happens?
it loses the capacity for phagocytosis and large- scale pinocytosis.
What are the two lineage commitment choices that a cell can make?
myeloid progenitor cell (aka a common myeloid progenitor)
lymphoid progenitor cell (aka a common lymphoid progenitor)
What does a myeloid progenitor cell do?
it creates red blood cells, platelets, and myeloid cells (granulocytes,monocytes, macrophages, and some dendritic cell populations)
What does lymphoid progenitor cells do?
they created B-lymphocytes, innate lymphoid cells (ILC’s) and specific dendritic cell populations.
Which HSC’s stay inactive and keep the ability to become many different cell types throughout life?
Long-term HSC’s
Does Long- term HSC’s make short term HSC’s?
Yes
Which HSC’s are usually inactive but divide more often and have a limited ability to renew themselves?
Short-term HSC’s
What does short-term HSC’s develop into?
multipotent progenitors (MPP’s)- they do not self-renew, yet they divide quickly and can become both lymphoid and myeloid cells.
What happens to an HSC as it progresses from a LT-HSC →ST-HSC→MPP?
it loses its ability to self-renew