Reproductive System III
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
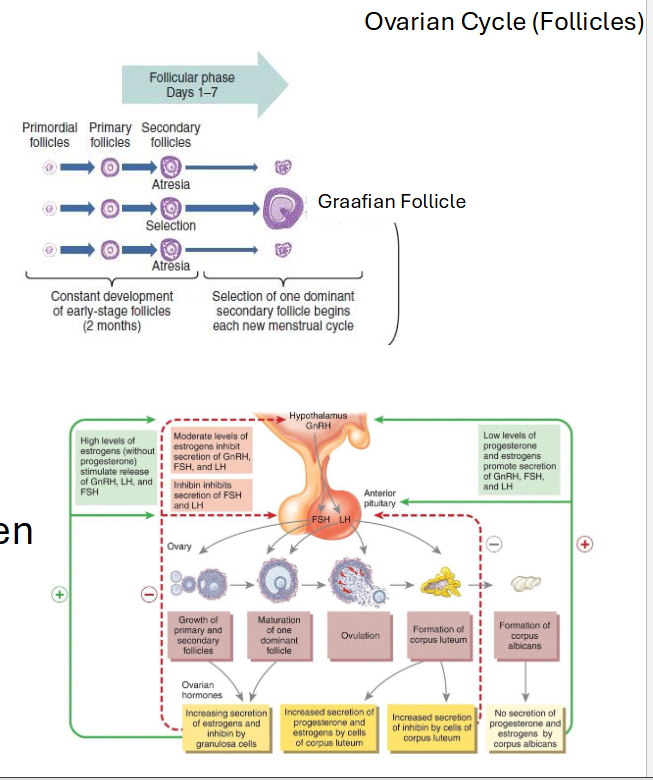
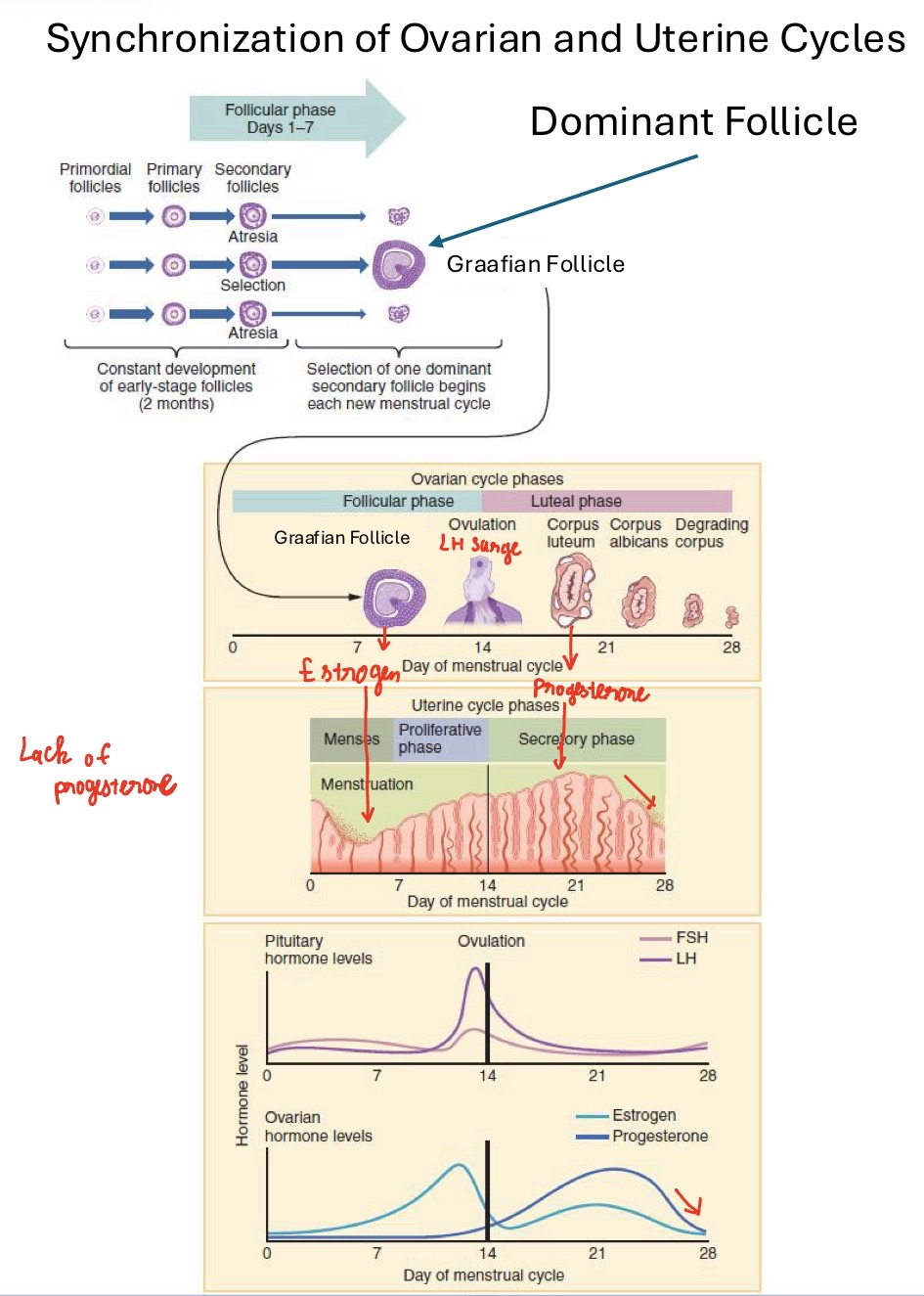
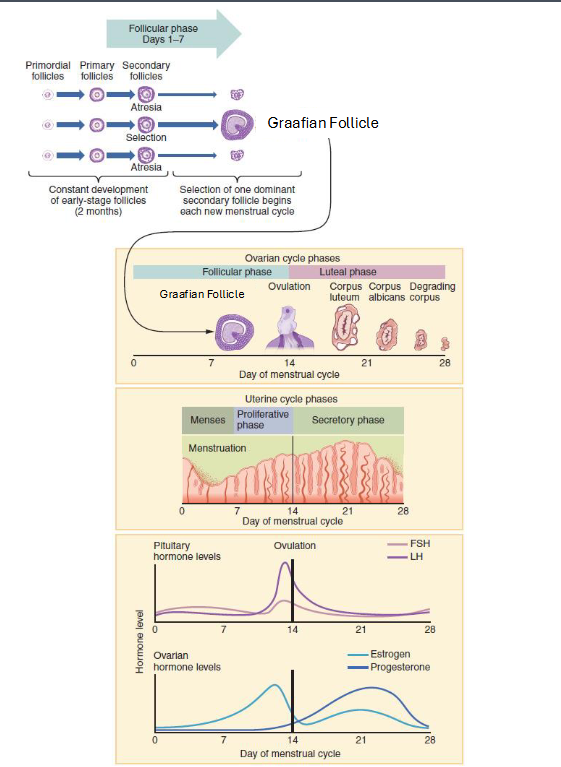
The Ovarian Cycle Overview
• Three Phases:
• Follicular: ~ day 1-13
• Ovulation: ~ day 14
• Luteal: ~ day 15-28
• ~28 days (but variable; luteal phase ~14 days is consistent)

Follicular Phase
• Days 1-13
• FSH stimulates follicle growth
• Granulosa cells → rising estrogen
• Dominant follicle selection
• Clarification from last lecture
• Key Idea: “Follicle grows and estrogen rises.”
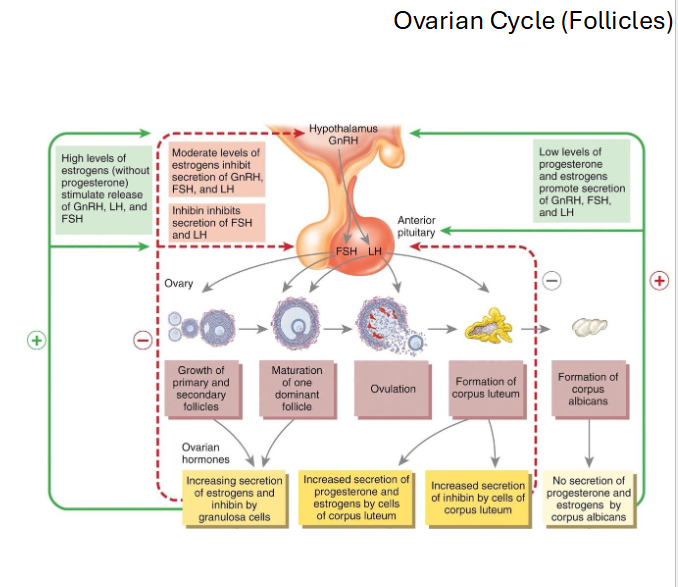
Ovulation
• Day ~14
• Rising estrogen → positive feedback → LH surge
• LH surge causes rupture of the Graafian follicle
• Secondary oocyte released (arrested in Metaphase II)
• Key Idea: “LH surge ruptures the follicle.”
Luteal Phase
• Days 15-28
• Ruptured follicle → corpus luteum
• Corpus luteum secretes progesterone + estrogen
• Purpose: maintain and thicken endometrium
• Key idea: Progesterone is the dominant hormone of this phase.
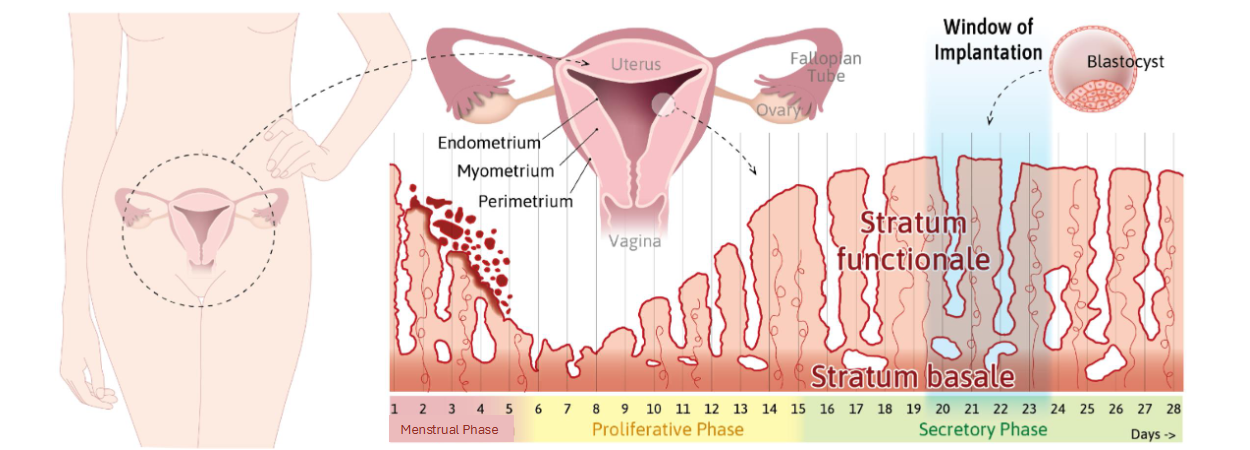
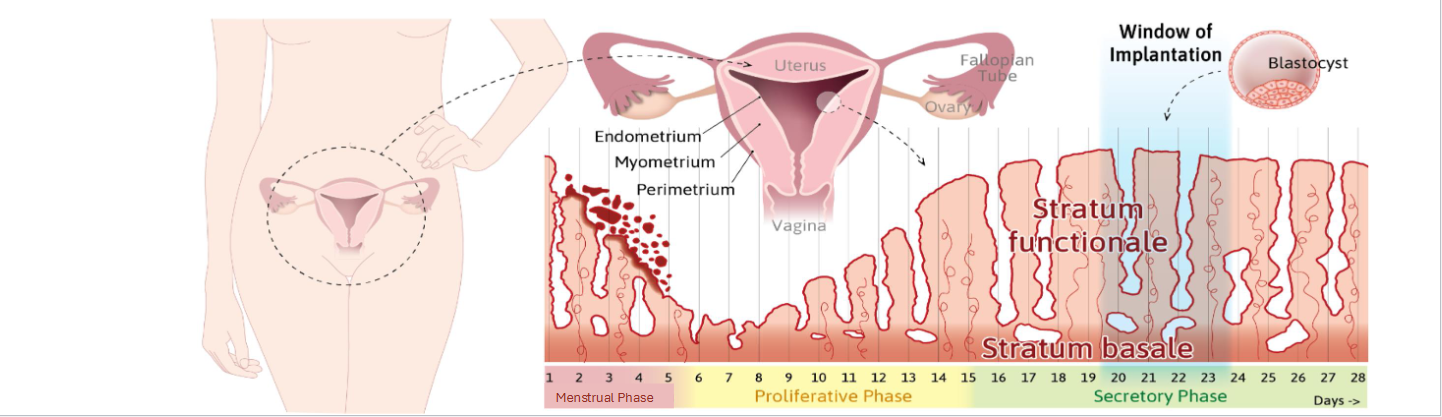
Uterine Cycle Overview
• Three Phases:
• Menstrual phase (days 1-5): Shelding
• Proliferative phase (days 6-14): Rebuiding - Estrogen
• Secretory phase (days 15-28): Sistaning →Progesterone
Menstrual Phase
• Shedding of functional layer of endometrium
• Triggered by the drop in estrogen/progesterone
• Corpus Luteum
• Spiral arteries constrict → tissue breaks down
• Key Idea: “Hormone drop = endometrium sheds.”
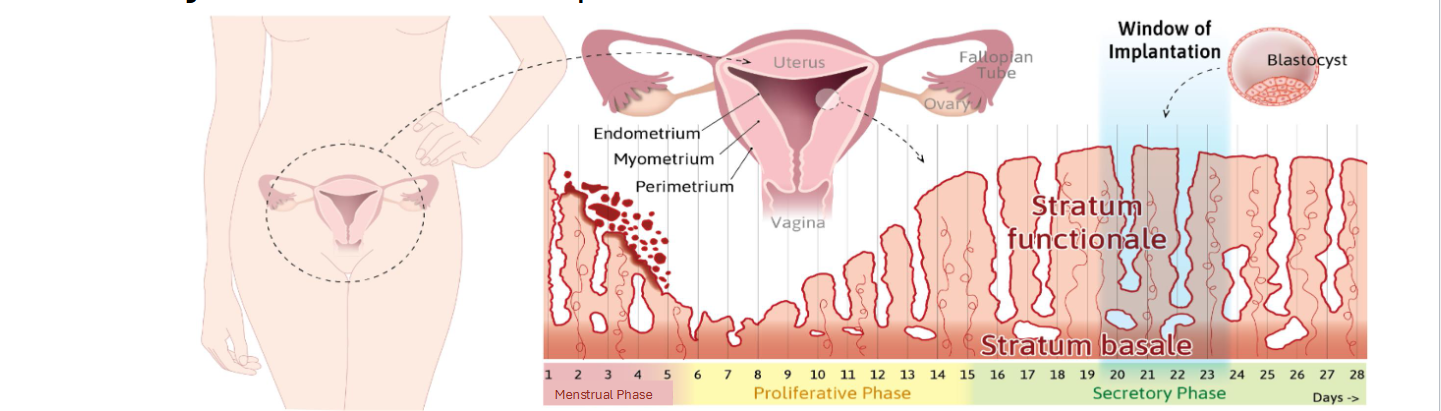
Proliferative Phase
• Estrogen from follicles rebuilds functional layer
• Endometrial glands lengthen
• Cervical mucus becomes thinner (fertile window)
• Key Idea: “Estrogen rebuilds the lining.”
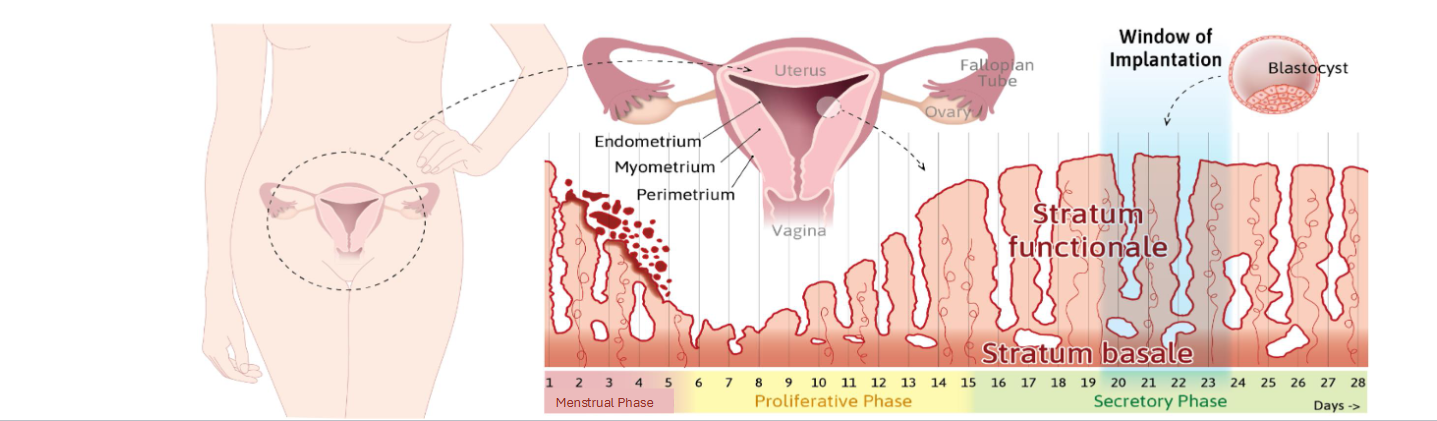
Secretory Phase
• Progesterone from corpus luteum stabilizes and thickens endometrium
• Glands coil and secrete nutrients
• Uterus readies for implantation
• Key Idea: “Progesterone prepares for pregnancy.”
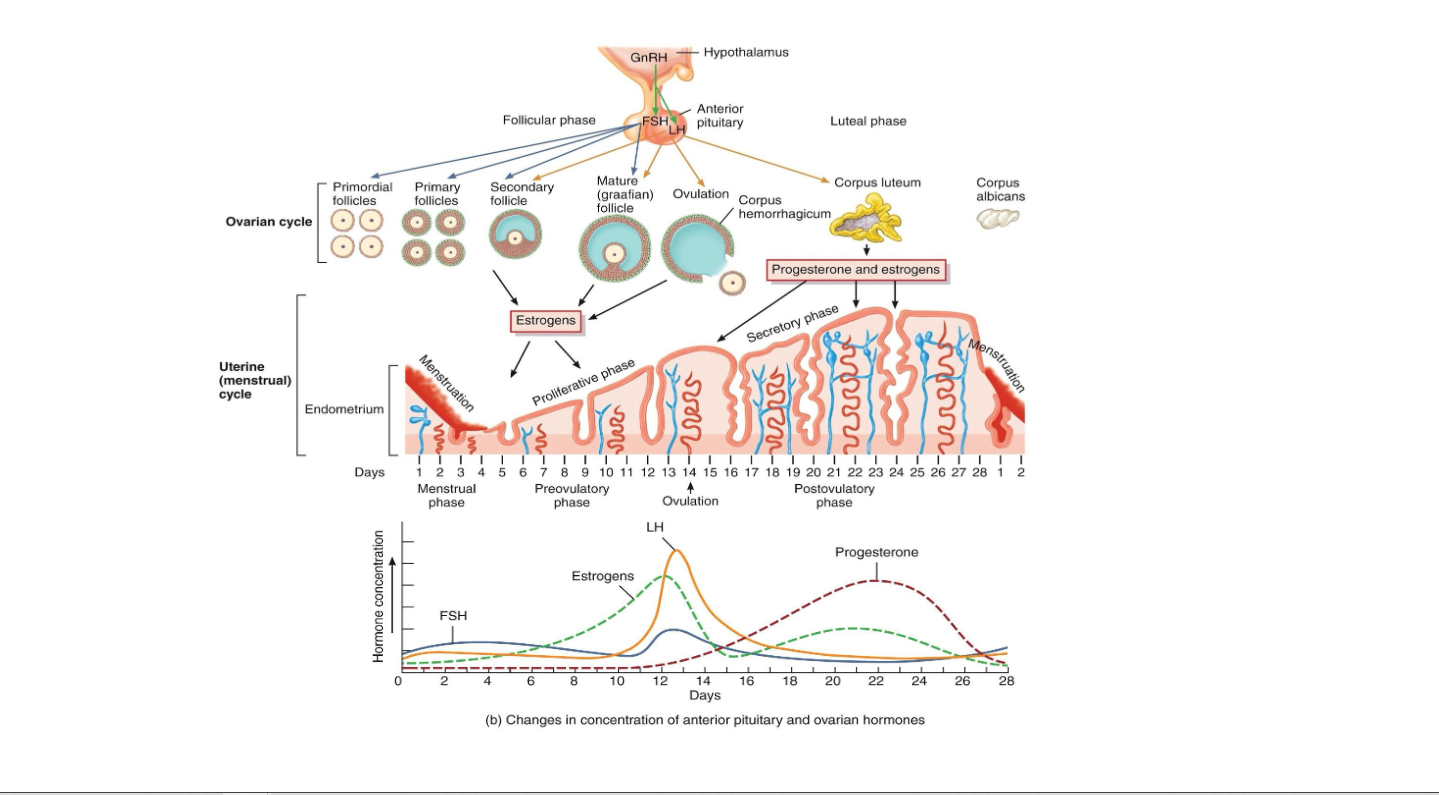
The Integration Diagram
• FSH, LH
• Estrogen, Progesterone
• Ovarian Cycle
• Uterine Cycle
• Notice:
• Estrogen peak → LH surge
• Progesterone peak → secretory phase
• Hormone drop → menstruation
Summary of Hormonal Role
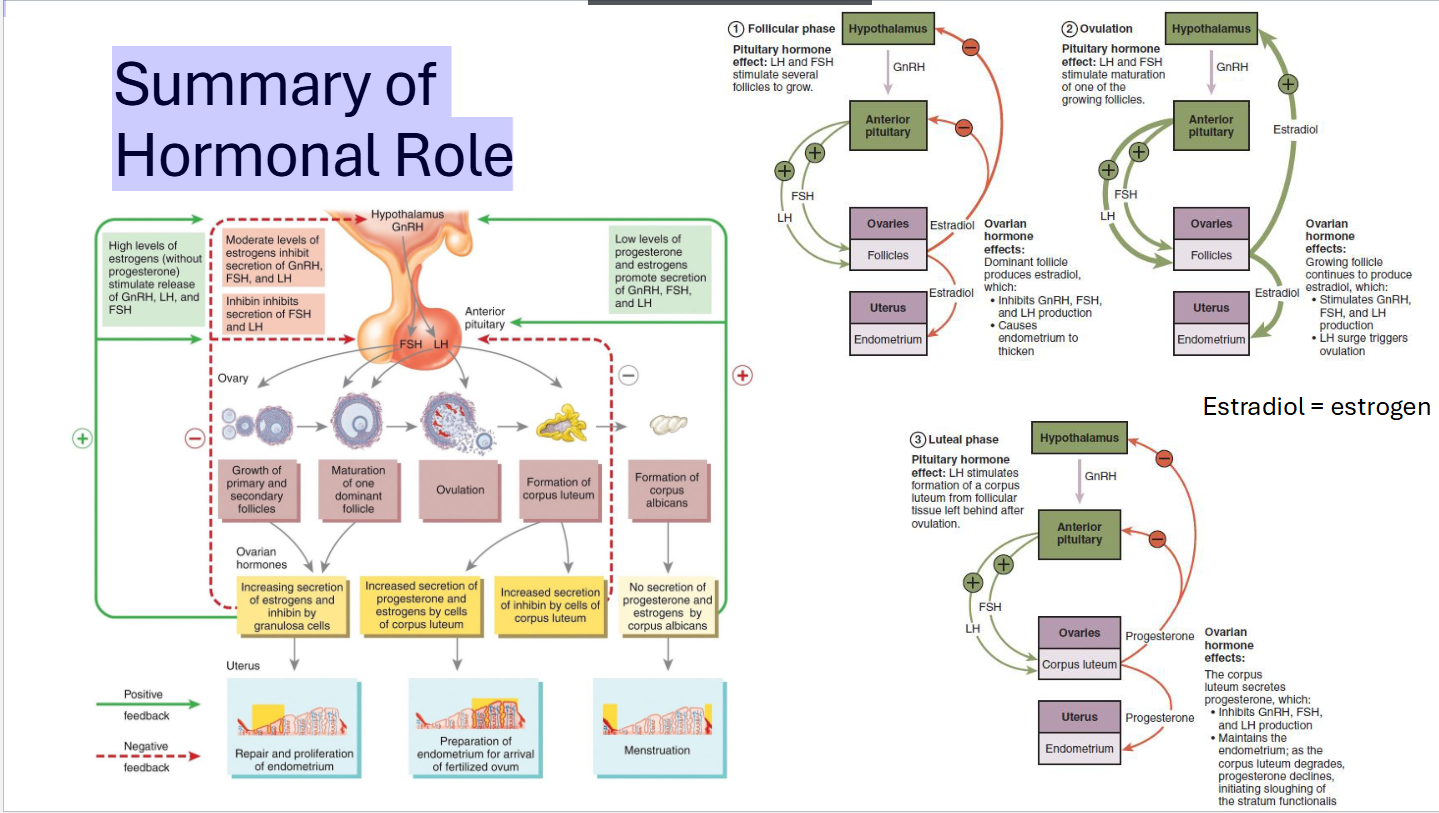
If no fertilization occurs...
• Corpus luteum → corpus albicans
• Progesterone & estrogen fall → menstruation begins
• FSH rises → next cycle begins
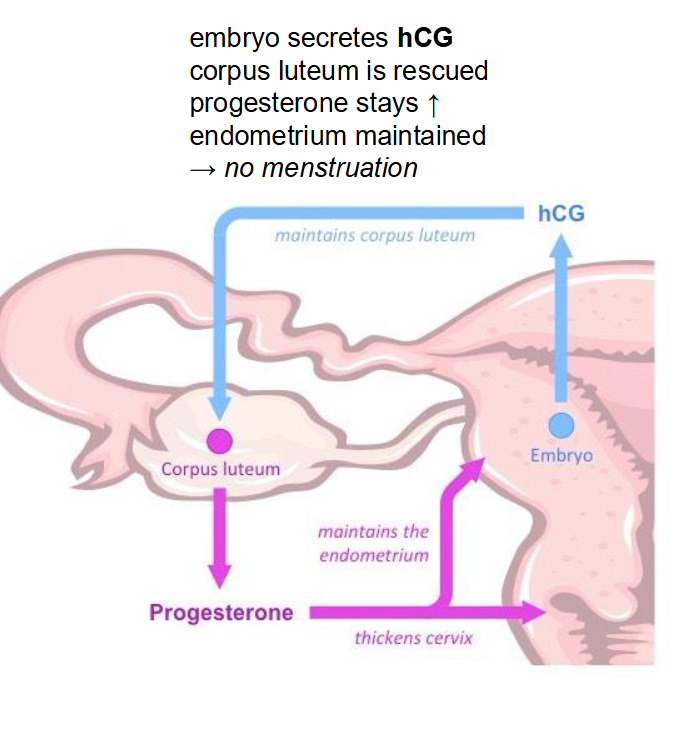
If fertilization (and implantation) does occur...
• Embryo secreting hCG
• hCG = human chorionic gonadotropin
• Acts like LH
• Keeps the Corpus Luteum alive
• Corpus Luteum keeps secreting progesterone
• If progesterone levels stay high, what won’t happen?
No Menstruation
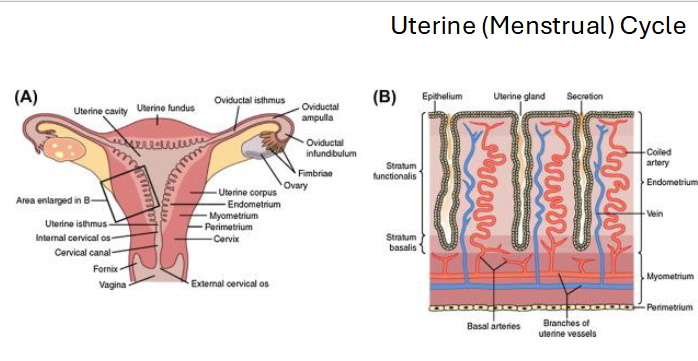
Uterine Environment Changes
• Before Ovulation: Estrogen Dominant
• Estrogen causes:
1. Cervical mucus thin/watery
2. Cervix to slightly open
3. Uterine Contractions
• Uterine/Cervical Environment is “Sperm-Friendly”
• After Ovulation: Progesterone Dominant
• Progesterone causes:
1. Cervical Mucus thick/sticky/impenetrable
• Protection for fertilized egg from infection
• Uterine/Cervical Environment is “Embryo-Friendly”

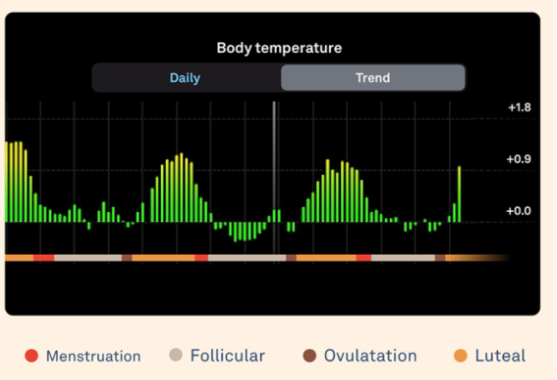
Basal Body Temperature Shift
• Progesterone slightly raises body temperature after ovulation
• 0.3–0.5°C
• Detectable with continuous charting
• Confirms ovulation has occurred
Implantation Window
• Secretory endometrium optimal around days 20–24
• Progesterone maintains uterus
• Corpus luteum survives only if hCG from embryo arrives
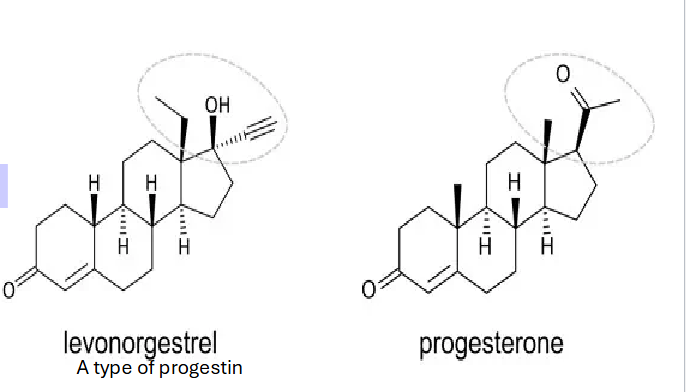
What hormonal birth control does
• Contains progestin (mimics progesterone)
• Negative feedback on Hypothalamus and Anterior Pituitary
• Prevents ovulation by blocking LH surge
• Thickens cervical mucus
• Thins endometrium
• Key Idea: “No LH surge = no ovulation.
Which best explains why only one follicle becomes dominant?
A. It has more LH receptors and survives high LH
B. It has more FSH receptors and survives falling FSH
C. It has more progesterone receptors and survives high progesterone
D. It produces less estrogen than other follicles
B. It has more FSH receptors and survives falling FSH
A fertilized embryo implants in the uterus approximately:
A. 12 hours after ovulation
B. 1–2 days after ovulation
C. 3–4 days after ovulation
D. 6–7 days after ovulation
D. 6–7 days after ovulation
Menstruation occurs primarily because:
A. FSH rises
B. LH rises
C. Progesterone and estrogen fall
D. Estrogen rises sharply
C. Progesterone and estrogen fall
If the corpus luteum fails to form, what
happens to the hormones?
A. Progesterone rises
B. Estrogen rises
C. FSH and LH rise
D. hCG rises
C. FSH and LH rise
Which hormone is primarily responsible for rebuilding the endometrium?
Estrogen
Which follicle ultimately becomes the dominant follicle?
Graagian Foolicle
What hormone is MOST responsible for preventing a second ovulation in the same cycle?
Progesterone
Write a 3-4 sentence essay for this prompt:
Explain how an implanted embryo maintains the
maternal endometrium during early pregnancy. In your
answer, describe the hormone the embryo produces,
what ovarian structure it affects, and how this prevents
menstruation
Embryo escreting HcG. It act like LH and keep corpus Luteum alive. Corpus can secreting progestion but progesterone need to maintain for endometrium so it wont be mentration.
Which of the following BEST explains why meiosis I, but not meiosis II, reduces chromosome number?
A. DNA replication occurs before meiosis II but not meiosis I
B. Homologous chromosomes separate in meiosis I, but sister chromatids separate in meiosis II
C. Cytokinesis fails to occur in meiosis I
D. Crossing over occurs only in meiosis II
B. Homologous chromosomes separate in meiosis I, but sister chromatids separate in meiosis II
Which event MOST directly contributes to genetic diversity in gametes?
A. Telophase II
B. Cytokinesis
C. Crossing over in prophase I
D. Random alignment of sister chromatids in meiosis II
C. Crossing over in prophase I
In oogenesis, the secondary oocyte is arrested in which phase until fertilization?
A. Prophase I
B. Metaphase II
C. Anaphase I
D. Telophase II
B. Metaphase II
Which statement correctly compares spermatogenesis and oogenesis?
A. Both produce four functional gametes
B. Only spermatogenesis involves meiosis II
C. Oogenesis begins before birth, but spermatogenesis begins at puberty
D. Crossing over occurs only in spermatogenesis
C. Oogenesis begins before birth, but spermatogenesis begins at puberty
A mutation reduces LH receptor expression on theca cells. Which outcome is MOST likely?
A. Excess androgen production → excess estrogen
B. Decreased androgen → decreased estrogen production
C. Increased FSH → increased estrogen production
D. No effect on estrogen production
B. Decreased androgen → decreased estrogen production
Which of the following BEST explains why more than one secondary follicle begins maturing each cycle? (if you are confused, we will clarify this today)
A. Only one follicle can respond to LH
B. Multiple follicles respond to early FSH, but only one survives falling FSH levels
C. The ovary needs multiple follicles to produce enough estrogen
D. The primary oocyte divides asymmetrically
B. Multiple follicles respond to early FSH, but only one survives falling FSH levels