121_Female Reproductive System
1/179
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
180 Terms
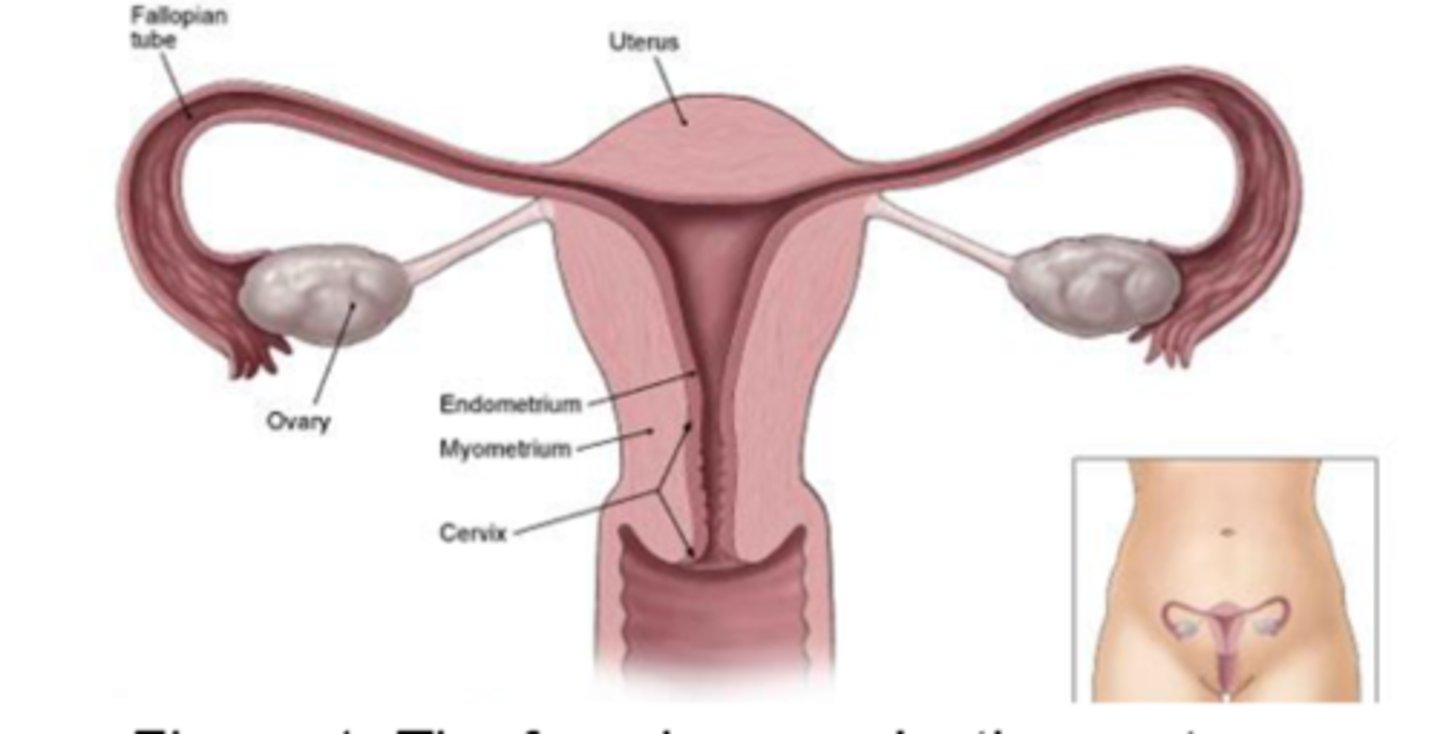
Main parts of the Female Reproductive System [6]
- Ovaries
- Uterine tubes
- Uterus
- Vagina
- External organs
- Mammary glands
[Main Part of the Female Reproductive System]
part of the female reproductive system that produces gametes
Ovaries
[Main Part of the Female Reproductive System]
transports the egg
Uterine Tubes
[Main Part of the Female Reproductive System]
where fetal development occur
Uterus
[Main Part of the Female Reproductive System]
serves as the birth canal
Vagina
[Main Part of the Female Reproductive System]
AKA external genitalia; constitutes the vulva
External Organs
[Main Part of the Female Reproductive System]
produces milk
Mammary Glands
5 Functions of the Female Reproductive System
read
- The ovaries produce secondary oocytes and hormones, including progesterone and estrogens (female sex hormones), inhibin, and relaxin
- The uterine tubes transport a secondary oocyte to the uterus and normally are the sites where fertilization occurs.
- The uterus is the site of implantation of a fertilized ovum, development of the fetus during pregnancy, and labor.
- The vagina receives the penis during sexual intercourse and is a passageway for childbirth.
- The mammary glands synthesize, secrete, and eject milk for the nourishment of the newborn.
[Term]
produce secondary oocytes and hormones, including progesterone and estrogens (female sex hormones), inhibin, and relaxin
ovaries
3 multiple choice options
[Term]
transport a secondary oocyte to the uterus and normally are the sites where fertilization occurs.
uterine tubes
3 multiple choice options
[Term]
is the site of implantation of a fertilized ovum, development of the fetus during pregnancy, and labor.
uterus
3 multiple choice options
[Main Part of the Female Reproductive System]
- Often referred to as egg receptacles
- They are the female gonads
- They are a pair of glands similar in size to unshelled almonds
- They are homologous to the testes
Ovaries
3 multiple choice options
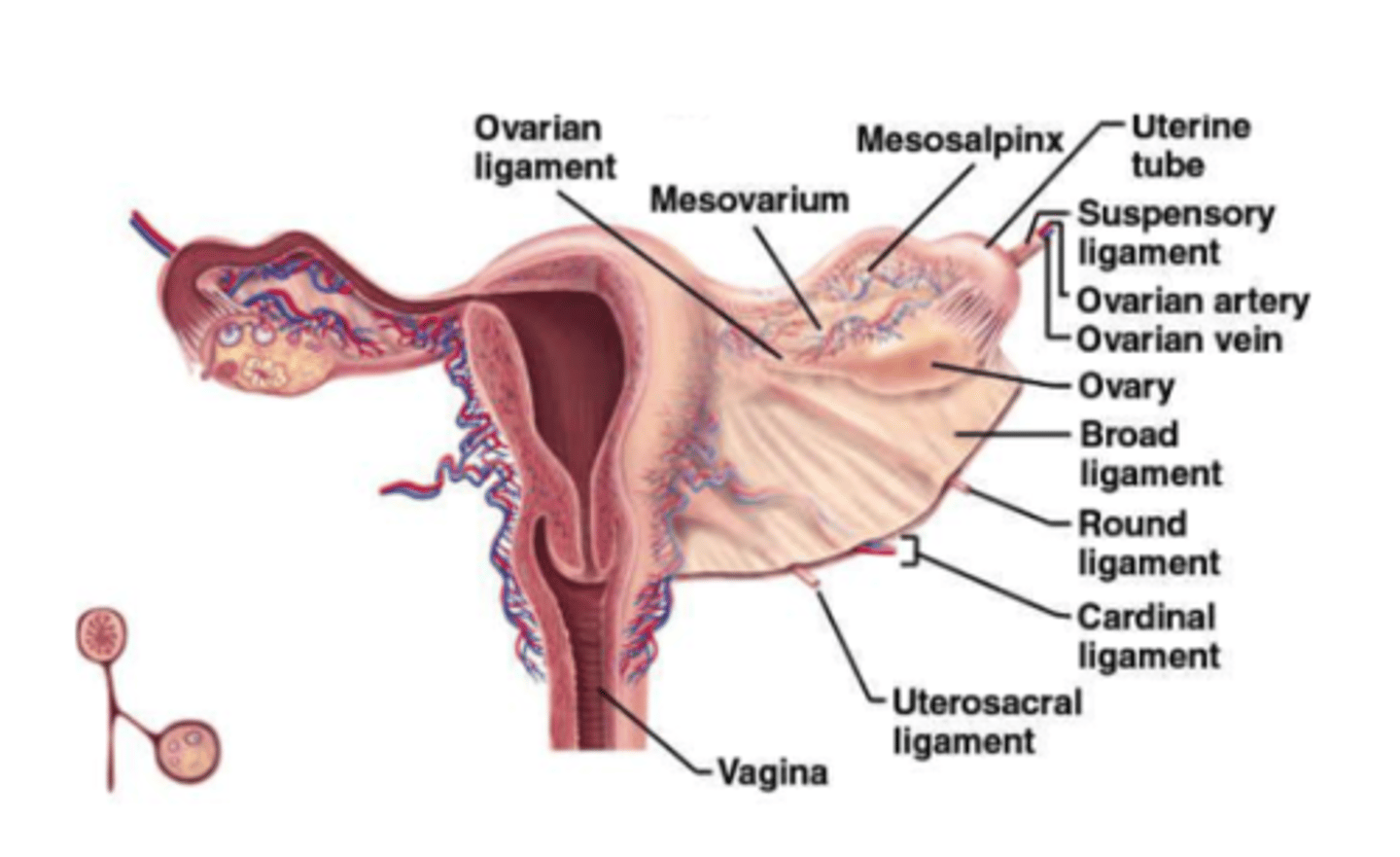
There are 3 types of ovarian ligaments
- Broad ligament
- Ovarian ligament
- Suspensory ligament
[Type of Ovarian Ligament]
attached to the ovaries by the mesovarium
Broad ligament
3 multiple choice options
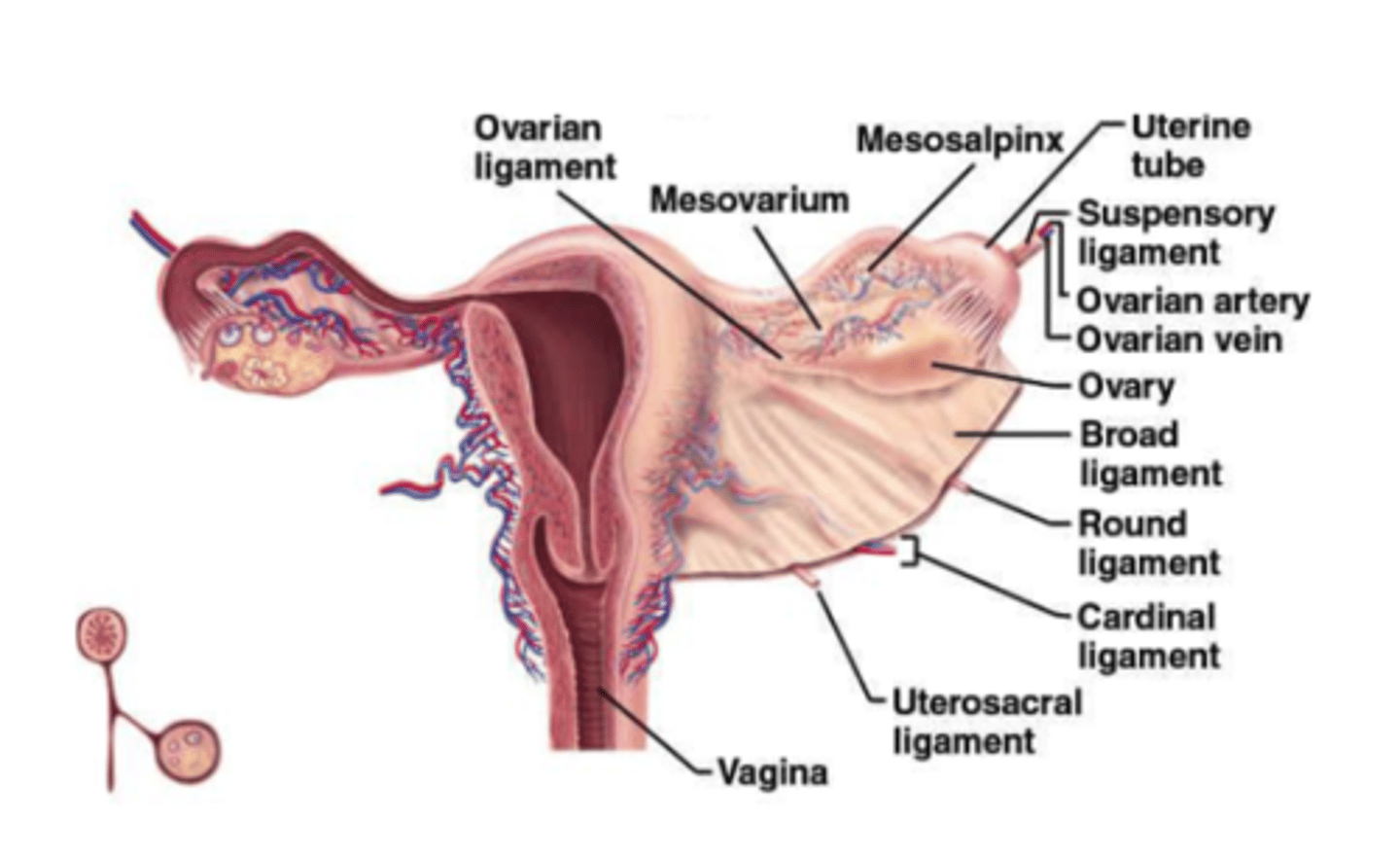
[Type of Ovarian Ligament]
anchors the ovaries to the uterus
Ovarian ligament
3 multiple choice options
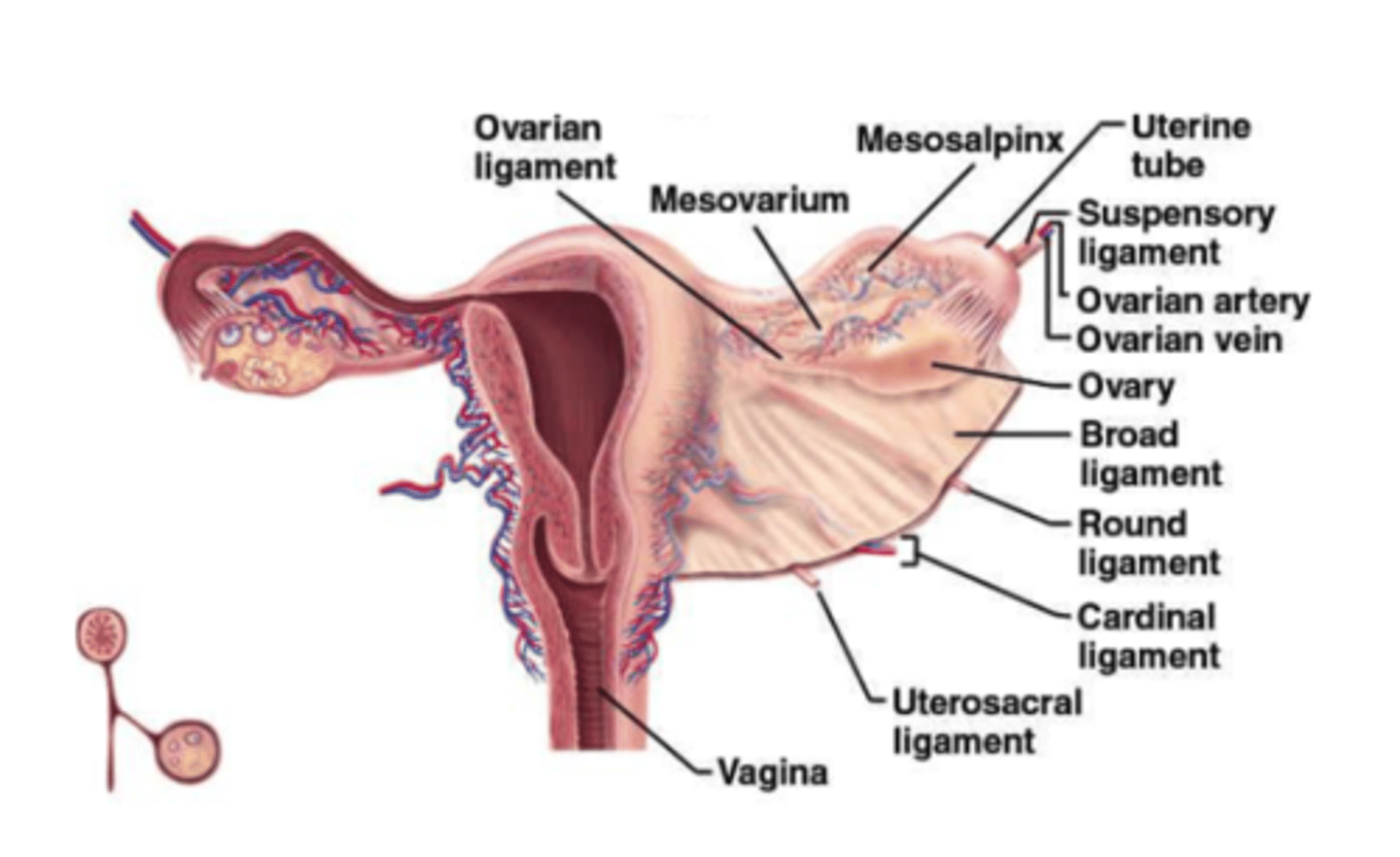
[Type of Ovarian Ligament]
attaches ovaries to pelvic wall
Suspensory ligament
3 multiple choice options
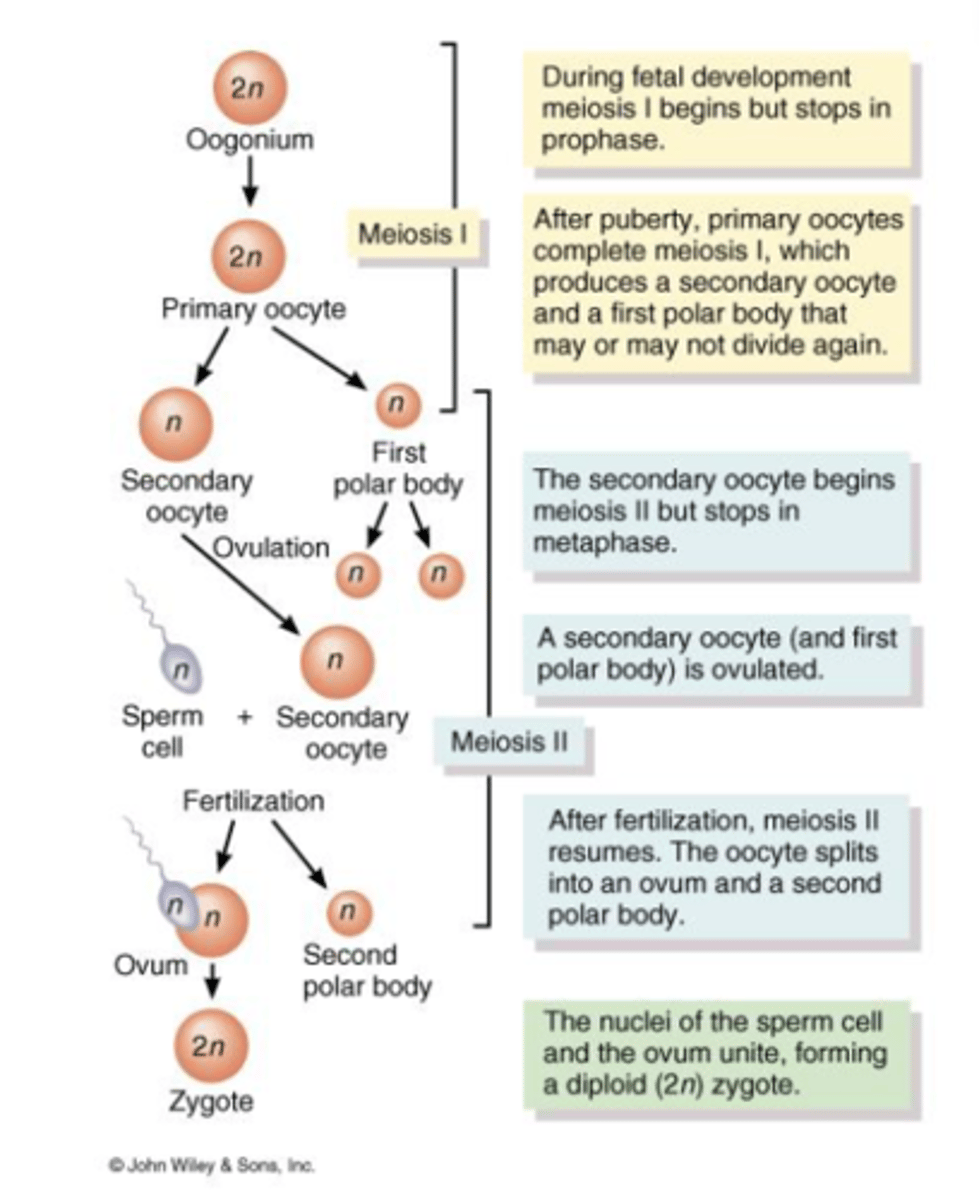
Oogenesis 🥚✨
read tamad na
- 🧬 Germ cells migrate from the yolk sac (umbilical vesicle) to the ovaries during fetal development.
- 🌱 In ovaries, germ cells differentiate into oogonia.
- 🔬 Oogonia (diploid stem cells) divide mitotically to form millions of germ cells.
- ⏸️ Some oogonia become primary oocytes that enter prophase I of meiosis but pause until puberty.
- 🏵️ Each primary oocyte is encased in flat follicular cells, forming a primordial ovarian follicle.
- 🧵 The ovarian cortex consists of collagen fibers and stromal cells.
- 👶 At birth, each ovary contains 200,000 to 2,000,000 primary oocytes.
- 🌸 By puberty, only about 40,000 oocytes remain.
- 🗓️ Throughout reproductive years, only about 400 oocytes mature.
- 🎯 Monthly, about 20 primary oocytes begin development, but usually only 1 ovulates.
Egg-forming cells (oocytes) divisions 🔄:
- ➡️ Start with 1° oocyte (2n = 46).
- ➗ Division produces two n = 23 cells:
🌟 One large 2° oocyte.
⚪ One small 1st polar body (may divide again).
- 💘 Second division occurs only if the 2° oocyte is fertilized.
- ➡️ Produces:
🥚 One large ovum (n = 23).
⚪ One small 2nd polar body.
- 👶 End result: One large fertilized egg (zygote) and possibly three small polar bodies.
1. Where do germ cells originate before migrating to the ovaries? 🧬
A) Amniotic sac
B) Yolk sac
C) Placenta
D) Uterus
2. What type of cell division do oogonia use to multiply? 🔬
A) Meiosis
B) Binary fission
C) Budding
D) Mitosis
3. During fetal development, in which phase of meiosis are primary oocytes arrested? ⏸️
A) Prophase I
B) Metaphase II
C) Anaphase I
D) Telophase II
4. How many primary oocytes typically remain at puberty? 🌸
A) 4,000
B) 40,000
C) 400
D) 200,000
5. What is the end result of oogenesis?
👶
A) Two ova
B) Multiple zygotes
C) One large fertilized ovum and up to three polar bodies
D) One sperm and one ovum
B) Yolk sac (umbilical vesicle)
D) Mitosis
A) Prophase I
B) 40,000
C) One large fertilized ovum and up to three polar bodies
Why is the result of oogenesis asymmetrical?
Only 1 cell is destined to become the ovum out of 4 potential daughter cells. It will get all the nutrients. Other tiny cells (polar bodies) don’t need much nutrients; they don’t last long and usually die pretty quickly. Only the ovum survives.
I. Secondary oocyte: product of 2nd division
II. Ovum: product of 1st division
A. The first statement is true. The second statement is false.
B. The first statement is false. The second statement is true.
C. Both statements are true.
D. Both statements are false.
D. Both statements are false.
Each ovary consists of the following parts: [7]
- Germinal Epithelium
- Tunica Albuginea
- Ovarian Cortex
- Ovarian Medulla
- Ovarian Follicles
- Tertiary Ovarian Follicle
- Corpus Luteum
[Part of the Ovary]
covers surface of ovary
Germinal Epithelium
[Part of the Ovary]
located immediately deep to the germinal epithelium
Tunica Albuginea
[Part of the Ovary]
immediately lower to tunica albuginea; consists of ovarian follicles and oocytes
Ovarian Cortex
[Part of the Ovary]
contains blood vessels, lymphatic vessels, nerves
Ovarian Medulla
[Part of the Ovary]
little bags in the cortex that consists of oocytes in various stages of development
Ovarian Follicles
[Part of the Ovary]
large, fluid-filled ovarian follicle that is ready to rupture and expel secondary oocytes during ovulation
Tertiary Ovarian Follicle
[Part of the Ovary]
contains the remnants of tertiary follicle after ovulation
Corpus Luteum
[Term]
Consist of oocytes in various stages of development plus surrounding cells
- Oocytes are immature ova
Ovarian follicles
[Ovarian follicles]
When the surrounding cells form a single layer, they are called _______
When they form several layers, they are referred to as __________
follicular cells, granulosa cells.
The surrounding cells of Ovarian follicles secrete estrogen for the purpose of the ff: [4]
- Growth and repair of the uterine lining
- Regulation of the monthly female cycle
- Female sexual characteristics
- Maintenance of bones and muscles
Follicular development [2]
- Primordial Follicle
- Primary (pre-antral) follicle
[Follicular development]
Single layer of squamous follicular cells around the oocyte
Primordial Follicle
[Follicular development]
- Layer of cuboidal follicular cells
- Layers cuboidal and columnar granulosa cells around the oocyte
Primary (pre-antral) follicle
Follicle development [5]
- Zona pellucida
- Corona radiata
- Secondary follicle
- Mature follicle
- Corpus luteum
[Follicle Development]
- It is a clear glycoprotein layer between the oocyte and granulosa cells
- It is formed as the primary ovarian follicle grows
Zona pellucida
[Follicle Development]
- It is the innermost layer of granulosa cells that are firmly attached to the zona pellucida
Corona radiata
[Follicle Development]
Secondary follicle [2]
- Theca folliculi
- Antrum
[Secondary follicle]
- It encircles the basement membrane
- 2 layers: Theca interna & Theca externa
Theca folliculi
[Secondary follicle]
- A cavity located in the middle of the secondary follicle
- Follicular fluid secreted by the granulosa cells build up in this cavity
Antrum
[Follicle Development]
- Also known as Graafian follicle
- It is large and fluid-filled
- It is ready to rupture and expel secondary oocyte in the process of ovulation
- This occurs on a monthly basis
Mature follicle
The ovarian follicles consist of the oocytes and the surrounding cells: [2]
- Follicular cells are single-layered
- Granulosa cells form several layers
[Follicle Development]
After ovulation, the empty follicles become this
corpus luteum
Corpus luteum secretes the following: [4]
- Progesterone
- Estrogen
- Relaxin
- Inhibin
[Hormone]
hormone that helps in the completion of the preparation of the uterine lining. This preparation process happens monthly
Progesterone
[Hormone]
works with progesterone with the preparation of the uterine lining
Estrogens
[Hormone]
relaxes the uterine muscles and the pubic symphysis
Relaxin
[Hormone]
decreases the secretion of follicular stimulating hormone (FSH) and luteinizing hormone (LH)
Inhibin
The white scar tissue that is left after the corpus luteum dies is called ?
Corpus Albicans
[Main Part of the Female Reproductive System]
- Also referred to as fallopian tubes or oviducts
- Females normally have two fallopian tubes that extend laterally from the uterus
- They are characterized as narrow, 4-inch tubes
Uterine tubes
Functions of the Uterine Tubes [3]
- They provide a route for sperm to reach an ovum
- They transport secondary oocytes
- They transport fertilized ova from the ovaries to the uterus
Parts of the Uterine [4]
- Infundibulum
- Fimbriae
- Ampulla
- Isthmus
[Parts of the Uterine]
- The funnel-shaped portion of each tube
- Located near the ovary but is open to pelvic activity
Infundibulum
[Parts of the Uterine]
- Fingerlike projections at the end of the infundibulum
- They are attached to the lateral end of the ovary
Fimbriae
[Parts of the Uterine]
- The longest and widest portion of the uterine tube
- It makes up about 2/3 of the overall length
- Located in the central region
Ampulla
[Parts of the Uterine]
- The medial, short, narrow, and thick-walled portion of the uterine tube
- It joins the uterus and the uterine tube
Isthmus
Occurrences in the uterine tubes [6]
read
- 🌸 Fimbriae sweep the secondary oocyte into the uterine tube
- 🌬️ Cilia and peristalsis guide the secondary oocyte from the peritoneal cavity to the uterine tube
- 💫 Sperm meets the oocyte in the ampulla
- 🤝 Ampulla is the meeting point of the sperm and oocyte
- 🕰️ Fertilization occurs within 24 hours after ovulation
- 🚀 The zygote reaches the uterus roughly 7 days after ovulation
- 💔 Unfertilized secondary oocytes disintegrate
- 🍽️ This happens because all the nutrients will be provided to the zygote/primary oocyte instead
Uterine tubes is composed of 3 layers [3]
- Mucosa
- Muscularis
- Serosa
[Layer of Uterine Tubes]
- Innermost
- Contains ciliated columnar epithelial cells which act like a conveyor belt moving the secondary oocyte along
Mucosa
[Layer of Uterine Tubes]
- Middle layer
- Composed of an inner, thick, circular ring of smooth muscle and an outer thin region of longitudinal smooth muscle
Muscularis
[Layer of Uterine Tubes]
Outer layer
Serosa
[Main Part of the Female Reproductive System]
- Womb
- Site of implantation of a fertilized ovum, development of fetus and labor
- Source of menstrual flow
- 3 inches long by 2 in. wide and 1 in. thick
Uterus
Weight gain in pregnancy
read
During pregnancy, it is normal for women to gain weight, with a total of 13-15 kilos
- Baby: 7.5 pounds (The weight of the baby is not the sole factor in the weight gain)
- Placenta: 1.5 pounds
- Amniotic fluid: 2 pounds
- Uterine enlargement: 2 pounds
- Maternal breast tissue: 2 pounds
- Maternal blood volume: 4 pounds
- Fluids in maternal tissue: 4 pounds
- Maternal fat stores: 7 pounds
Subdivisions of the Uterus [3]
- Fundus
- Body
- Cervix
[Subdivision of the Uterus]
dome-shaped, superior portion
Fundus
[Subdivision of the Uterus]
tapering central portion
Body
[Subdivision of the Uterus - Body]
located between the body and the cervix
Isthmus
[Subdivision of the Uterus - Body]
interior of the body
Uterine cavity
[Subdivision of the Uterus]
inferior narrow portion
Cervix
[Subdivision of the Uterus]
interior of cervix, opens into the uterine cavity at the internal os and into the vagina at external os
Cervical canal
Normal position based on tilting of the uterus: [3]
- Anteverted
- Retroverted
- Vertical
[Normal position based on tilting of the uterus]
tilted forward towards the bladder
Anteverted
[Normal position based on tilting of the uterus]
tilted backwards toward the spine
Retroverted
[Normal position based on tilting of the uterus]
no tilting, upright position
Vertical
Normal position based on location of the fundus: [2]
- Anteflexed
- Retroflexed
[Normal position based on location of the fundus:]
fundus bends forward; looks like a C going forward
Anteflexed
[Normal position based on location of the fundus:]
fundus bends backwards
Retroflexed
Most babies will move into the delivery position a few weeks prior to birth. This is when the head moves closer to the birth canal. However, if this fails to happen, the baby's feet or buttocks will be positioned to be delivered first. This is because there is a failure in the movement to the delivery position. When the baby is upright (feet and buttocks positioned to be delivered first), this position is called ?
breech position.
I. The normal delivery position (head first) is more common, but breech positions still happen.
II. It occurs approximately in 1 out of 25 full term births.
A. The first statement is true. The second statement is false.
B. The first statement is false. The second statement is true.
C. Both statements are true.
D. Both statements are false.
C. Both statements are true.
[Term]
Maintain the normal position of the uterus
Uterine ligaments
Uterine ligaments [4]
- Broad ligaments
- Uterosacral ligaments
- Cardinal (lateral cervical) ligaments
- Round ligaments
[Uterine ligament]
attach the uterus to either side of the pelvic cavity
Broad ligaments
[Uterine ligament]
connect the uterus to the sacrum
Uterosacral ligaments
[Uterine ligament]
extend from the pelvic wall to the cervix and vagina
Cardinal (lateral cervical) ligaments
[Uterine ligament]
located between the layers of the broad ligaments (sandwiched)
Round ligaments
[Histology of the Uterus]
Innermost layer of the uterus, consists of simple columnar epithelia
Endometrium
2 layers of Endometrium
- Stratum functionalis
- Stratum basalis
[Layer of Endometrium]
lines the uterine cavity; sloughs off during menstruation
Stratum functionalis
[Layer of Endometrium]
gives rise to a new s. functionalis after each cycle of menstruation
Stratum basalis
[Histology of the Uterus]
- Middle layer of the uterus
- Consists of 3 layers of smooth muscle
- Thickest in fundus; thinnest in cervix
Myometrium
[Histology of the Uterus]
- Outer layer
- Anteriorly, it covers the bladder and forms a shallow pouch (vesicouterine pouch)
- Posteriorly, covers the rectum and forms rectouterine pouch (pouch of Douglas)
Perimetrium
[Histology of the Uterus]
- Downward displacement of uterus
- Varies in severity
- May result from weakening of supporting ligaments and pelvic musculature
Uterine prolapse
[Degree of Uterine Prolapse]
cervix remains within the vagina
First degree (mild)
[Degree of Uterine Prolapse]
cervix protrudes to the exterior through the vagina
Second degree (marked)
[Degree of Uterine Prolapse]
entire uterus is outside the vagina
Third degree (complete)
I. Clinically, depending on the severity, usually it is possible that the patient will not experience any signs or symptoms of uterine prolapse (First degree)
II. However, depending on severity again (Second/third degree), the patient can experience different types of symptoms (e.g. feeling of heaviness, pulling in pelvis area, urinary problems, urine retention/leakage, lower back pain, bowel movement problems, observed protruding of tissue from vagina)
A. The first statement is true. The second statement is false.
B. The first statement is false. The second statement is true.
C. Both statements are true.
D. Both statements are false.
C. Both statements are true.
There are certain factors that can increase the risk of patient for uterine prolapse: [8]
- Giving birth to a large baby
- Having one or more pregnancies or vaginal births
- Frequent heavy lifting
- Age (as a woman gets older, there is higher risk for uterine prolapse)
- Genetic (if there is a genetic predisposition to having a weak connective tissue)
- Pelvic surgeries (if patient had pelvic surgery before)
- Chronic coughing
- Straining during bowel movements (Especially if the force is strong)
1. True or False: In uterine prolapse, the uterus can slip down or protrude out of the vagina.
2. True or False: Only post-menopausal women can experience uterine prolapse
3. True or False: Vaginal births can increase the risk of uterine prolapse.
T
F
T
[Term]
Surgical removal of uterus, usually the purpose is normally to improve sexual well-being (e.g. sexual problems such as pain)
Hysterectomy
Type of Hysterectomy [3]
- Partial
- Complete or Total
- Radical