Childhood age classes, Tissue Volumes and Other Helpful Facts and Numbers
1/69
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
70 Terms
Neonate
0-28 days
fe of renally cleared drugs
>30%
Amino acids that can be phosphorylated
Serine, threonine and tyrosine (just three!)
Chronic Kidney Disease
GFR <60mL/min/1.73 sqm OR evidence of injury (haematuria or proteinuria)
Surface area of the Small Intestine
Size of a tennis court (250 sqm); 7 metres long
Small Intestine pH
6-7.5 from duodenum to ileum
Plasma Volume
3 L
Blood Volume
7 L
Extracellular water volume
15 L
Intracellular water volume
27 L
Total body water volume
42 L
Infant
>28 days - 12 months
Tissue sequestration volume of distribution
>70 L
Toddler
12-23 months
Preschool Child
2-5 years
School age child
6-11 years
Adolescent
12-17 years
Nephron proximal tubule absorption
100% of filtered glucose and amino acids/proteins, 70% of filtered water and ions (Cl, Na, K, HCO3)
Nephron descending Loop of Henle reabsorption
Water only
(*no solutes reabsorbed*)
Nephron ascending Loop of Henle reabsorption
Solutes (Na, K, Cl, Ca, Mg) only (*no water reabsorbed!*)
Nephron distal tubule and collecting duct reabsorption
Solutes (ions) and water reabsorption
Water reabsorption is regulated by ADH (vasopressin) and aldosterone
Glomerular Filtration Rate in a healthy young adult
120 mL/min
Average GFR of a healthy elderly person 60+ years
75-85 mL/min
CrCl in moderate kidney impairment
< 50-60 mL/min
CrCl in severe kidney impairment
< 30 mL/min
Urine pH range
pH 5-8
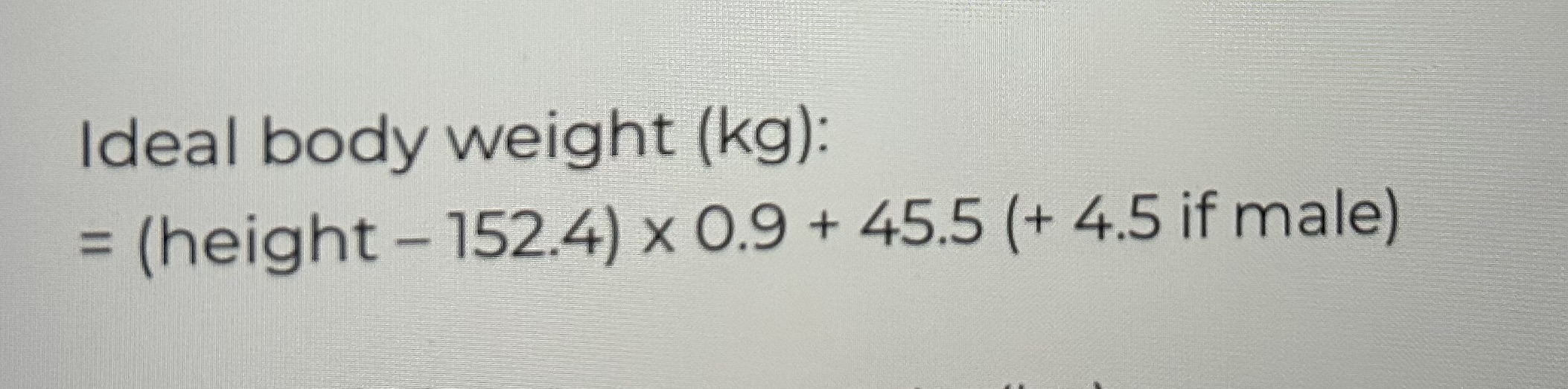
Ideal Body Weight
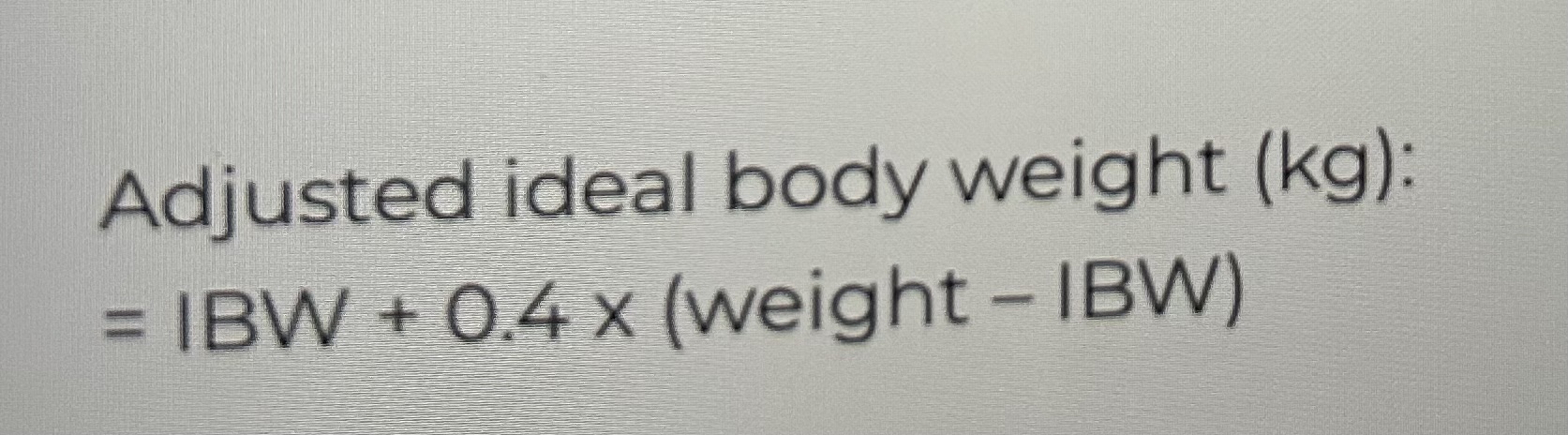
Adjusted Ideal Body Weight
Serum Creatinine Reference Levels (Male and Female)
Male: 60-120 micromol/L
Female: 50-110 micromol/L
Ideal Body Weight Formula (Male and Female)
Male: 50 + 0.9*(height - 152cm)
Female: 45.5 + 0.9*(height - 152cm)
When to adjust dose for renal impairment? And how?
When GFR <60 mL/min
By increasing dose interval or reducing dose
At what age is GI absorption comparable to adults?
By 3 months of age
At what age is enzyme metabolism activity greater than in adults?
At the ages 2-3 years old (toddlerhood)
Which enzymes exhibit increasing activity during pregnancy?
CYP3A4, CYP2C9, CYP2D6, UGT
Which enzymes exhibit decreasing activity during pregnancy?
CYP1A2, CYP2C19, NAT2
The AEIOU of when to initiate dialysis
A: Acidosis
E: Electrolyte disturbance (particularly hyperkalaemia)
I: Intoxication
O: Overload (of volume/fluids)
U: Uremia
The two driving forces of dialysis
Convection and diffusion
Dialysis should be started for patients with what GFR?
GFR <30 mL/min; CKD stages G4 and G5
Drugs banned in sport
Anabolic agents, diuretics, hormones, stimulants
Glucocorticosteroids (oral, injectable, rectal banned, EXCEPT inhaled and intranasal - no exemption required)
Beta-2-antagonists (EXCEPT salbutamol (Ventolin) when inhaled max 6 puffs in 8 hours, max 16 puffs in 24 hours for asthma/allergies; salmeterol (Seretide) max 8 puffs in 24 hours - no exemption required)
Beta-blockers for precision sports
A therapeutic use exemption (TUE) can be applied for at ASDMAC (Australian Sports Drug Medical Advisory Committee)
Best Sports Drug Resources
GlobalDro, Sports Integrity Australia, World Anti-doping Agency
Type A ADR treatment
Withhold and/or reduce dose
Type B ADR
Withhold drug and do not rechallenge (drug is now contraindicated) - use an alternative agent
Type I Hypersensitivity
Ig-E mediated; the foreign substance interacts with the Ig-E of mast-cells and basophils, causing the cells to degranulate and release factors
Anaphylaxis, urticaria (hives/rash), asthma, food allergies, hay fever, dermatitis
Type II Hypersensitivity
Ig-G and Ig-M (antibody) mediated; the foreign substance has interacted with surface receptors of cells, making them appear foreign to the immune system, such that the immune system launches an attack at the cells and causes cell death (they get phagocytosed by macrophages or lysed by cytotoxic cells and the complement system).
Onset of TENS/SJS vs Onset of DRESS
TENS/SJS: 4-28 days of first exposure (within days; within the month!)
DRESS: 2-6 weeks of first exposure
Rule of 3’s for epidemiology of events
If event occurs in 1 in x number of people, then you will have a 95% chance of seeing it occur at least once in 3x number of people.
When to TDM - “ACT”
Age - the very young and very old
Complex/Critical (ICU)/Comorbidities/Concomitant meds
Tricky drug (drug ADME)
What is a biosensor?
A device that measures levels of a substance in situ and produces a signal proportional with the concentration of substance present.
E.g. glucose sensors, INR units, urate sensors, aptamer-based biosensors
Random Testing vs Blanket Testing vs Targeted Testing vs Voluntary Testing
Random Testing: unannounced testing of persons
Blanket Testing: everyone tested at once
Targeted Testing: testing of suspicious persons
Voluntary Testing: people can choose to take the initiative to get tested if they want to
Hospital ICU levels requiring a pharmacist
Levels 4, 5 and 6.
Which drugs bind to which plasma proteins?
Acidic drugs bind to albumin (which has many basic sites)
Basic drugs bind to alpha-1-acid glycoprotein (which is acidic)
Neutral drugs bind to lipoproteins
Average difference of Cmax and AUC between bioequivalent brands
Less than 5%
Bioequivalence means that the…
90% confidence interval of the ratio of Cmax and AUC between brands conform within 0.80 to 1.25
Which drugs are most vulnerable to drug-drug interactions affecting renal clearance?
High fe (renally cleared), net secretion drugs
Where does tubular secretion and tubular reabsorption occur in the nephron?
Secretion into the proximal tubule
Reabsorption from the distal tubule
Which factors affect tubular reabsorption?
Urinary pH (pKa in the middle of 5-8) and urinary excretion rate.
Which drugs should we use with caution in renal impairment?
Drugs with high fe, narrow safety margin, long half-life and active metabolites.
Creatinine Clearance vs GFR?
CrCl makes GFR look better than it is by about 15%.
(CrCl overestimates GFR by about 15%)
Which hepatic zone does drug biotransformation take place?
Zone 3 (centrilobular): surrounding the central vein. This is the most anaerobic zone.
What biotransformed/metabolic by-products are excreted into bile?
Molecules that are polar and over 500 g/mol (the larger the molecule, the more biliary excretion it experiences). E.g. conjugates.
Does reduced CLint affect the bioavailability and AUC of high EH drugs?
Yes!
It does not affect hepatic CL (because it is not a determining factor) but it massively affects bioavailability because high EH drugs experience extensive first pass metabolism usually - so reduced CLint affects the amount of first pass metabolism!
Antidrug antibodies…
Increase clearance of therapeutic proteins; may or may not affect efficacy
FcRn…
prolongs the half-life of monoclonal antibodies. Will not affect peptide drugs, only monoclonal antibody drugs which have the Fc region!
Characteristics of metabolites
More polar, more acidic, more albumin (plasma protein) bound, smaller volume of distribution
Type of Phase I and Phase II metabolism of codeine
From codeine to morphine via O-demethylation by CYP2D6, then from morphine to morphine-6-glucuronide via glucuronidation by UGT2B7
Metabolism of Irinotecan (topoisomerase inhibitor prodrug)
From irinotecan to SN38 active but toxic metabolite via carbamate (ester) hydrolysis by CES1 or CES2, then elimination of the active yet toxic metabolite via glucuronidation by UGT1A1.
So, UGT1A1 poor metabolisers will suffer toxicity - neutropenia and diarrhoea - when treated by this drug.
How does Phase I and Phase II metabolism change in the elderly?
Phase I decreases because of reduced oxygen from reduced blood flow/perfusion (BUT the same number of enzymes are present!)
Phase II is unaffected by ageing.
MATE transporters
Renal secretion of cations via H+ or Na coupled antiport mechanisms
Bumetanide, frusemide
Loop diuretics
Distal tubule acting
Sodium-potassium-chloride co-transporter inhibition
Loss of water and sodium: Blocks reabsorption of sodium
Loss of potassium: hypokalaemia inducing
Diuresis: increases urine flow rate
Frusemide relies on active transport by OAT1 to enter tubule and reach site of action to exert its diuretic effect.