Unit 5 - Neurologic Conditions I and Genetic Conditions
1/45
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
46 Terms
Cerebral Palsy Definition
“Cerebral palsy describes a group of permanent disorders of the development of movement and
posture, causing activity limitations that are attributed to nonprogressive disturbances that occurred in the developing fetal or infant brain”
CP
Typical Impairments
Motor
Cognition
Behavior
Communication
Sensation
Perception
CP
Etiology
Exact cause is often unknown
In utero disturbances in the developing brain
Significant contribution of prenatal factors
Premature birth or atypical intrauterine growth can increase risk
Cerebral vascular events occurring within the first 28 days after birth are a significant cause of CP
There may be a link to genetics
How is a Diagnosis of CP Made?
Combined findings from the neurological assessment, neuroimaging, and assessment of posture and movement
Clinical diagnosis
Physical therapists play a role in early referral
Pediatric physician specialist to rule out other causes
CP Medical Management
Surgical Interventions
Selective Dorsal Rhizotomy (SDR)
Tenotomy
Osteotomy
Tendon transfer
CP Medical Management
Medication Options
Spasticity and Dystonia Management – oral medications
Baclofen (oral or intrathecal), diazepam, tizanidine Artane, and dantrolene
Botox Injections
Prevents the release of ACH at neuromuscular junction
Lasts 4-6 months
Peak effects at 2 weeks postinjection
CP
Secondary Conditions
Contractures
Skeletal malalignment
Muscle disuse atrophy
Decreased cardiovascular endurance
Pain
Decrease in bone mineral density
CP-Specific Tests & Outcome Measures
Body Function and Structures
Modified Tardieu scale
Spinal Alignment Range of Motion Measure
Selective Control Assessment of the Lower Extremity
Accelerometers
Non-Communicating Children’s Pain Checklist/Pain Assessment Instrument for Cerebral Palsy
CP-Specific Tests & Outcome Measures
Activity & Participation
Timed distance tasks (walking or wheeled mobility)
Gait Laboratory Assessment/Video Assessment/Edinburgh Gait Score
Gross Motor Function Measure (GMFM)
Pediatric Evaluation of Disability Inventory (PEDI)/PEDI-CAT
Activity Scale for Kids
Child Engagement in Daily Life
Assessment of Life Habits
Lifestyle Assessment Questionnaire for Cerebral Palsy
Alberta Infant Motor Scales (AIMs)
Test of Infant Motor Performance (TIMP)
CP-Specific Tests & Outcome Measures
Environment
Craig Hospital Inventory of Environmental Factors
CP-Specific Tests & Outcome Measures
Quality of Life
Pediatric Quality of Life Inventory (PedsQL), version 3.0, Cerebral Palsy Module
Caregiver Priorities and Child Health Index of Life with Disabilities
Cerebral Palsy Quality of Life Questionnaire for Children
CP
Focus of PT Goals and Intervention
Minimizing the impact of primary impairments
Preventing secondary impairments, physical deterioration, and pain
Maximizing function
Promoting participation in age and developmentally appropriate home, school, leisure, social, and employment activities to optimize quality of life
CP
PT Intervention – Dosing
The number of direct service visits is less important than the total dose of an intervention
“Dose” includes:
Frequency of visits
Intensity or strenuousness of activities
Time per session
Type or focus of intervention
CP
PT Intervention Planning Considerations
Family-centered and relationship-focused services
Effective communication and coordination with other service providers
Goal-focused
Use of ICF and functional frameworks
Individualized or “tailored” intervention plans
Task-specific activities
Incorporate motor learning strategies
Problem-solving
Task specificity
Active trial and error
High-frequency of practice
Self-correction, exploration
Learning and practice in real-life environments
Compensations, task modifications, or environmental adaptations to accommodate a child
Life span approac
CP
PT Interventions
Task-Oriented Practice by Facilitating Motor Milestones
Muscle and Joint Extensibility through Serial casting, Orthoses, and/or Positioning
* Daily short-duration passive stretching programs to maintain muscle length lack evidence to support outcomes
Task-Specific Muscle Strength Programs
1–3 sets of 6–15 repetitions at 50%–85% repetition maximum at a frequency of 2–4 times a week on nonconsecutive days.
Training periods = 12–16 consecutive weeks
Additional Interventions with strong evidence:
Constraint Induced Movement Therapy (CIMT)
Bimanual Hand Function
Hippo Therapy
Partial-Body Weight Support Treadmill Training
Treadmill Training
CP is classified by:
Level of function (GMFCS)
Topographic distribution - impairments in body functions and structure/body part(s) affected
Atypical Movement type
CP
Classification by Level of Function
Gross Motor Function Classification System (GMFCS)
For children with CP
Birth through age 18
CP
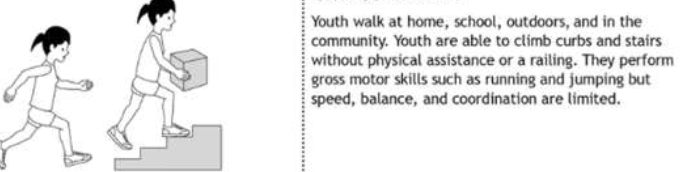
Gross Motor Function Classification System (GMFCS): Level 1
CP
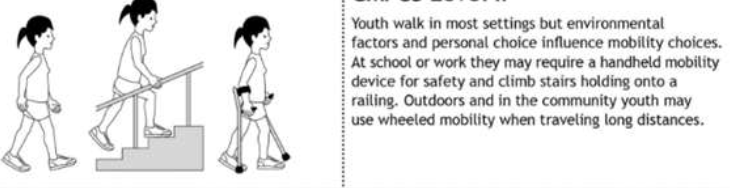
Gross Motor Function Classification System (GMFCS): Level 2
CP
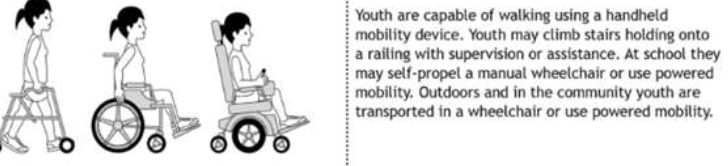
Gross Motor Function Classification System (GMFCS): Level 3
CP
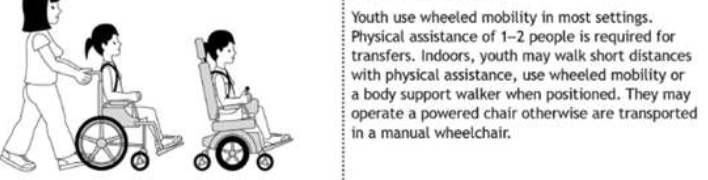
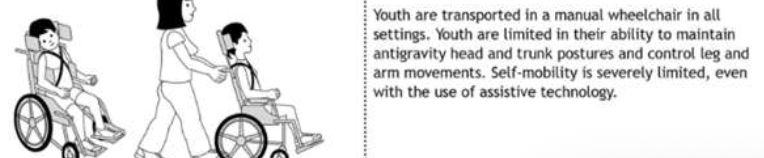
Gross Motor Function Classification System (GMFCS): Level 4
CP
Gross Motor Function Classification System (GMFCS): Level 5
CP
Classification by Topographic Distribution
Diplegia
Lower limbs affected more than upper
CP
Classification by Topographic Distribution
Hemiplegia or Hemiparesis
Upper and lower limbs on one side of the body
CP
Classification by Topographic Distribution
Quadriplegia or Tetraplegia
All limbs
CP
Classification by Atypical Movement Type
Spastic
Site of Lesion
Motor cortex or white matter projections to and from cortical sensorimotor areas of the brain
Objective Signs
Increased muscle tone and DTRs, Spasticity present
Movement Description
Spasticity and exaggerated reflexes result in abnormal patterns of posture and movement
CP
Classification by Atypical Movement Type
Dyskinetic (Dystonic, Athetotic)
Site of Lesion
Basal ganglia
Objective Signs
Fluctuating muscle tone
Movement Description
Atypical patterns of posture and involuntary, uncontrolled, recurring, and slow, continuous writhing movements with unstable posture
CP
Classification by Atypical Movement Type
Ataxic
Site of Lesion
Cerebellar
Objective Signs
Positive cerebellar signs
Movement Description
General instability, abnormal patterns of posture, and a lack of orderly, coordinated, rhythmic, and accurate movements
CP
Classification by Atypical Movement Type
Mixed – spasticity and dyskinesia
Symptoms of spasticity and dyskinesia may be present
Down Syndrome
Etiology
Genetic condition resulting from trisomy 21 (3 copies of 21st chromosome)
Occurs in ~1 in 700 live births, 6000 babies born yearly in the US
Most common chromosomal condition diagnosed in the US
Down Syndrome
Physical Characteristics
Every system of body can potentially be affected:
Hypotonia
Small head
Epicanthal folds
Flat nasal bridge
Upward-slanting palpebral fissures
Brushfield spots
Small ears and mouth
Excessive skin at nape of neck
Single transverse palmar crease
Short 5th finger with clinodactyly (curvature) and wide spacing
Deep plantar groove between 1st and 2nd toes
Down Syndrome
Diagnosis and Prognosis
Prenatal screening
Maternal blood tests
Ultrasound looking for nuchal translucency which tends to be more prominent
Down Syndrome
Secondary Conditions/Comorbidities
Cardiopulmonary Conditions
Congenital heart defects
Atrial septal defects
Ventricular septal defects
Atrioventricular septal defects
Obstructive sleep apnea
Down Syndrome
Secondary Conditions/Comorbidities
Endocrine disorders
Hypothyroidism
Type 1 diabetes mellitus
Down Syndrome
Secondary Conditions/Comorbidities
Gastrointestinal disorders
Gastroesophageal reflux disease (GERD)
Down Syndrome
Secondary Conditions/Comorbidities
Sensory system impairments
Hearing deficits
Vision deficits
Down Syndrome
Secondary Conditions/Comorbidities
Multisystem comorbidities
Obesity
Leukemia
Pain
Down Syndrome
Secondary Conditions/Comorbidities
Neurological Conditions
Seizures due to the reduced overall brain volume
Cognitive disability
Delayed language development
Alzheimer's type dementia
Depression
Down Syndrome
Secondary Conditions/Comorbidities
Musculoskeletal Abnormalities
Hypotonia
Ligamentous laxity
Joint hypermobility
Decreased bone mineral density
Down Syndrome
Diagnosis Specific Outcome Measures
Body Structure and Function
Height
Weight
Body Mass Index (BMI)
Head circumference
Down Syndrome
Diagnosis Specific Outcome Measures
Activity Level
Gross motor function
GMFM-88
Down Syndrome
Movement Characteristics
Gross motor delay-resulting from hypotonia
Decreased strength (upper and lower extremity)
Hypermobile joints
Increased flexibility
Rounded shoulder posture
Decreased activity tolerance
Skeletal malalignment- resulting from hypotonia and ligamentous laxity
Patellar instability, genu valgum, pes planus, hallux valgus
Impaired postural control- resulting from overuse of inefficient co-contraction strategies, insufficient balance reactions, impaired proprioceptive feedback
Down Syndrome
Gait
General qualitative differences
New walkers with DS have similar patterns to typically developing new walkers
Use more conservative strategies initially, more variability with age
Decreased gait velocity, stride length, increased step width
Increased hip and knee flexion
Increased knee flexion due to overall muscle weakness
Lower arches leads to increased foot external rotation & decreased ankle power
Down Syndrome
Precautions/Considerations
Ligamentous laxity affecting the atlanto-occipital region of cervical spine
Diagnosis is challenging and controversial requiring imaging
Symptoms of spinal cord compression include:
Easy fatiguability
Difficulty walking
Abnormal gait
Neck pain
Limited neck mobility
Torticollis
Change in hand function
New onset of urinary retention or incontinence
Incoordination and clumsiness
Sensory impairments
New onset of spasticity
Down Syndrome
Physical Therapy Management
Early Intervention (0-3yrs)
Task specific practice
High repetitions
Visual feedback
Modeling
Coaching parents on facilitating exploration, motivation, persistence, problem solving
Tummy time (early emphasis before 11wks)
Orthoses to support excessive pronation
Treadmill training
Down Syndrome
Physical Therapy Management
Intervention 3-18yrs
Progressive resistance training
Balance training
Whole body vibration
Orthoses
Aerobic training
Jumping
Biking
Dance