Pelvis mcqs
1/113
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
114 Terms
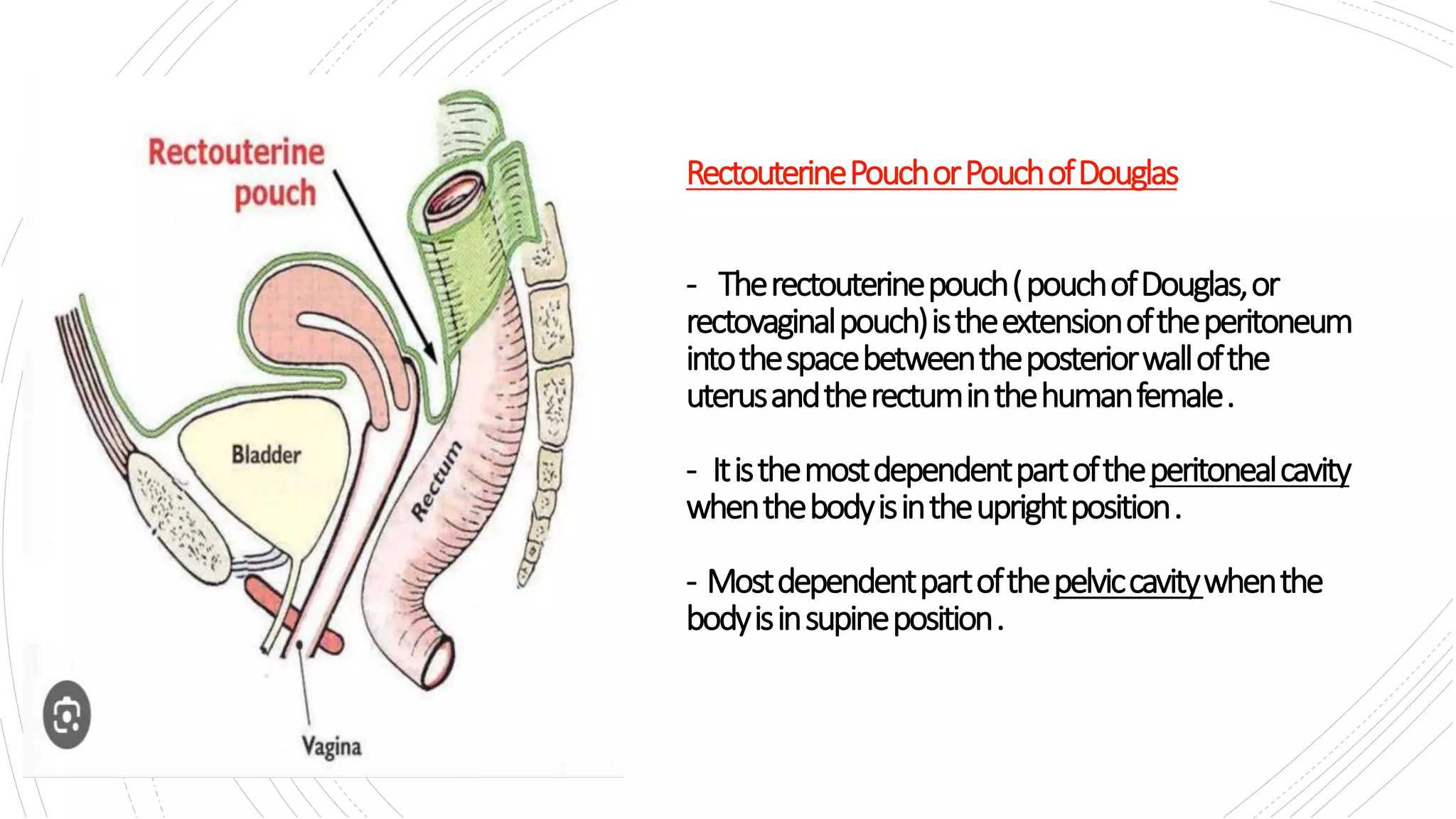
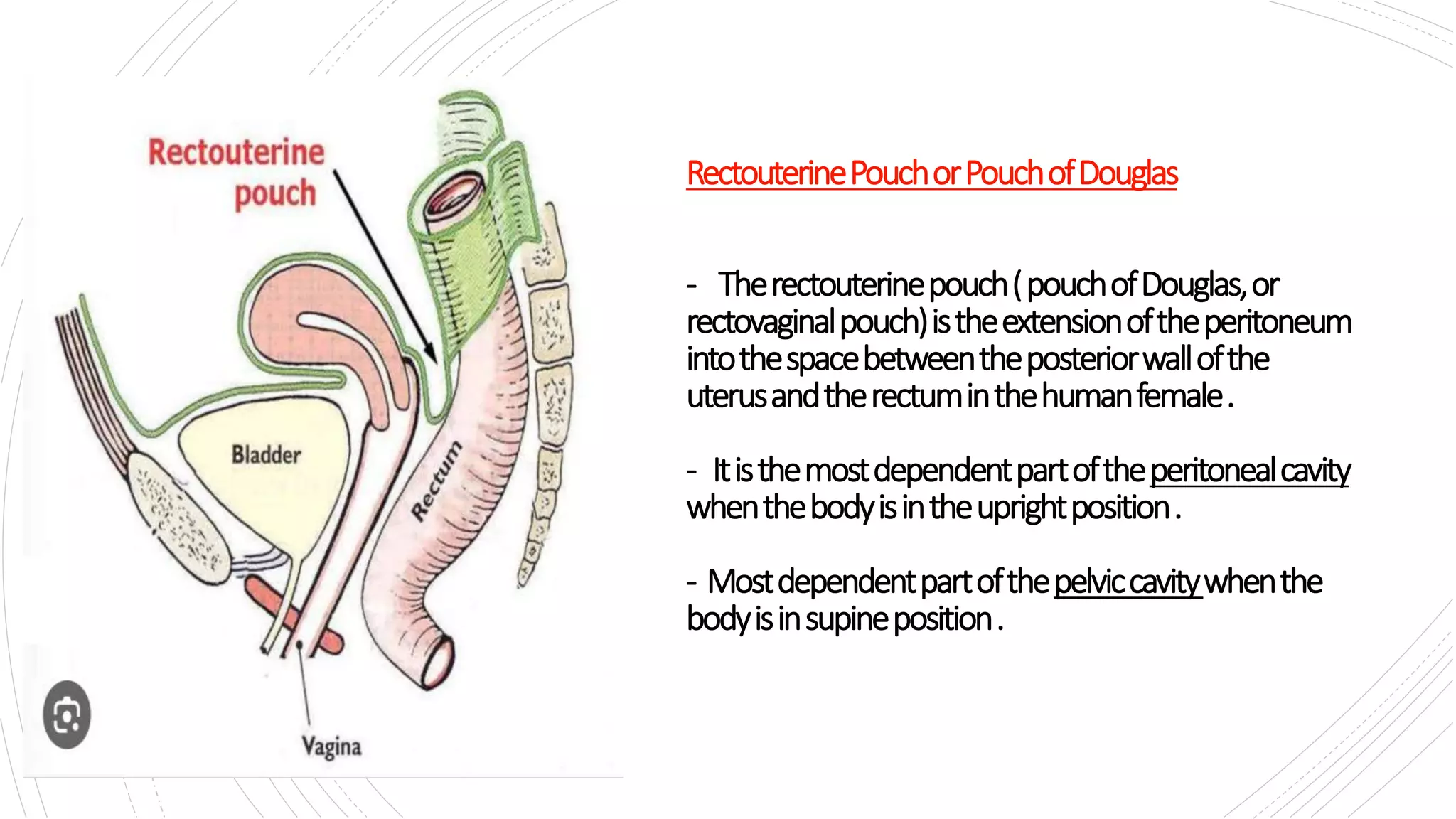
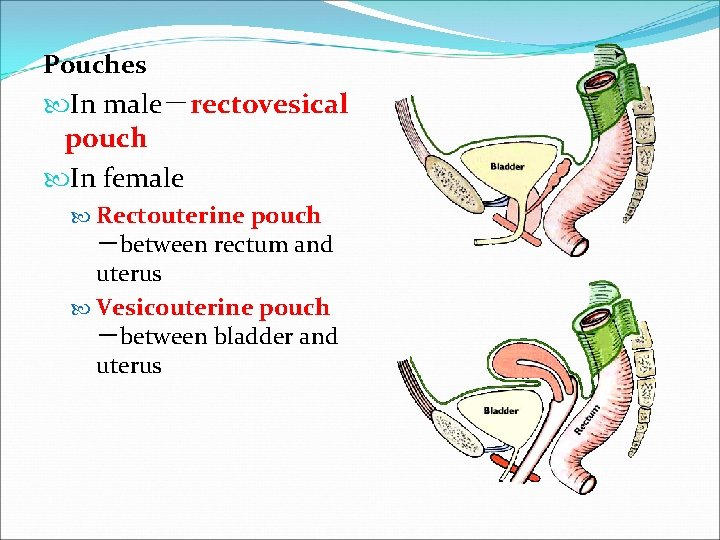
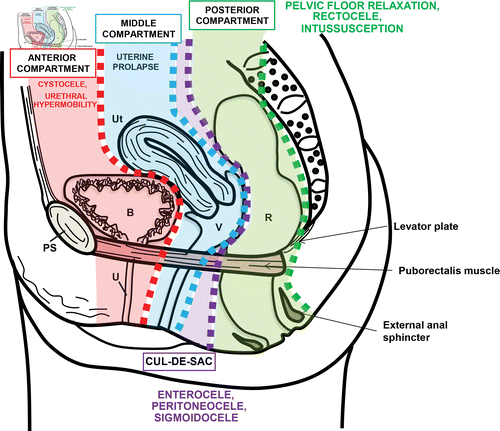
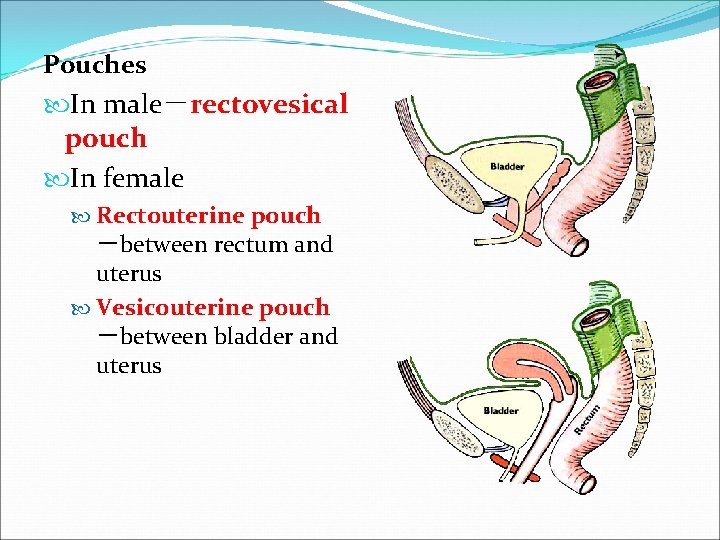
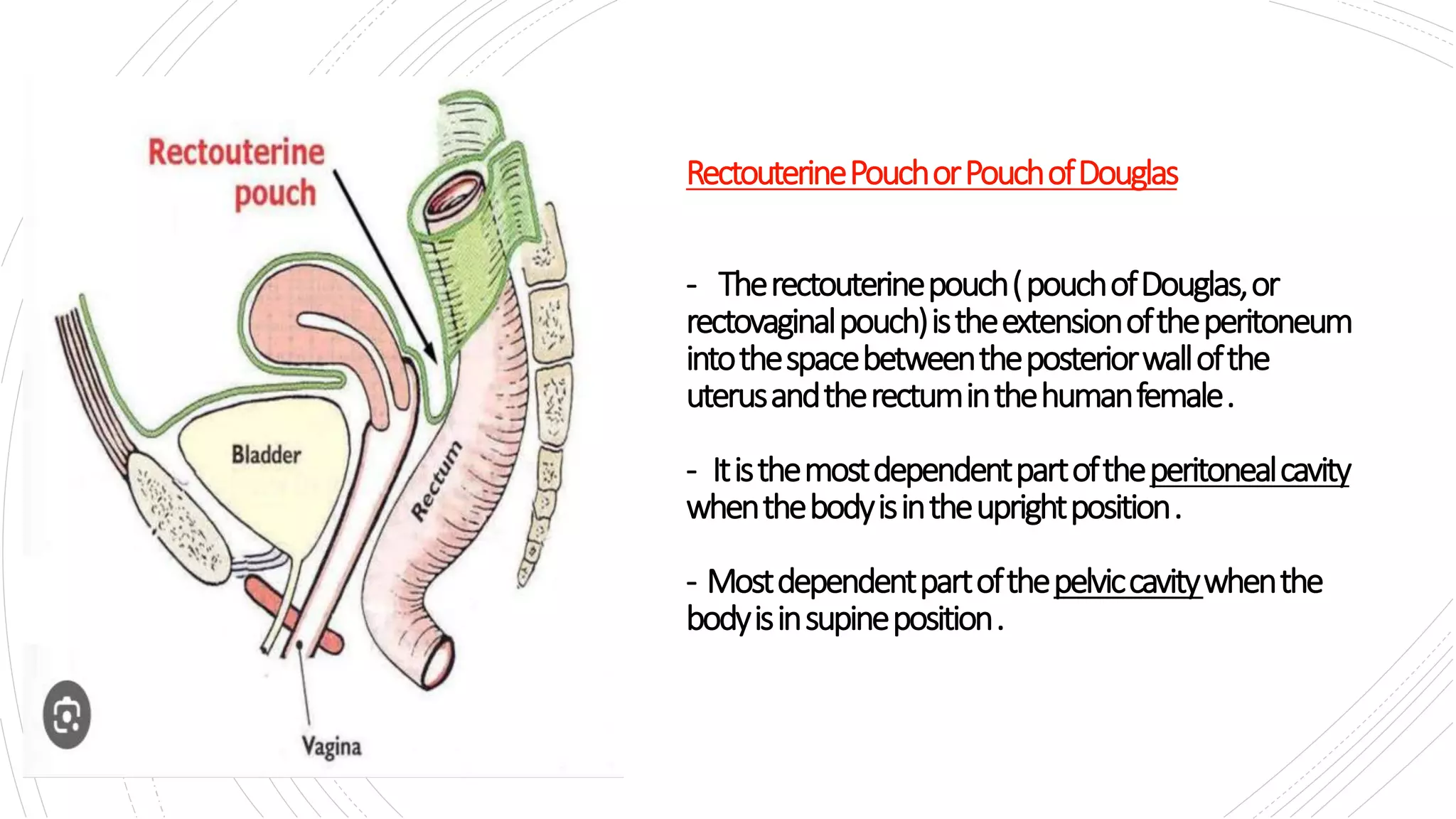
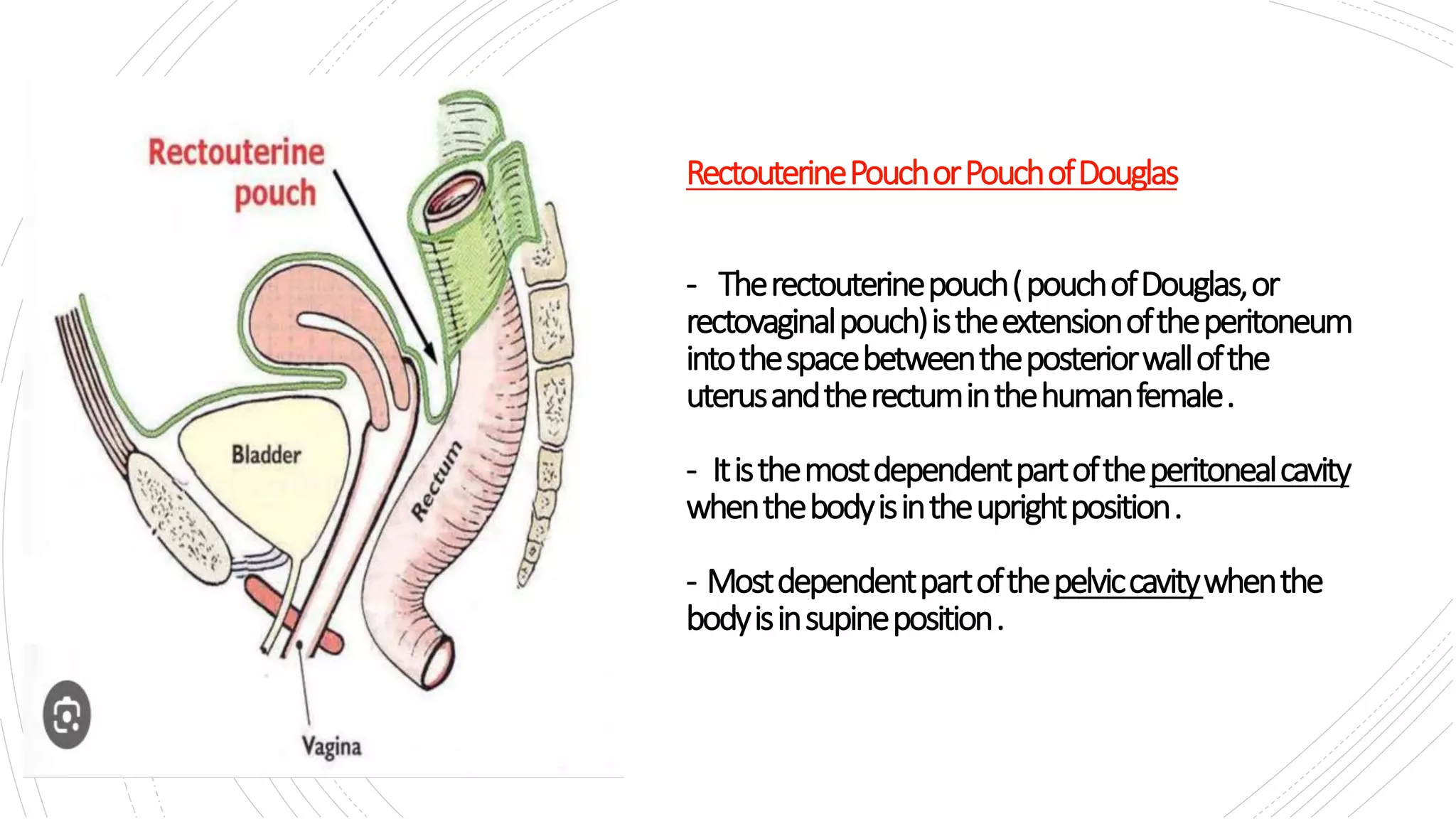
1. Rectovesical pouch is the most inferior spot of peritoneal cavity in female subjects
A. Yes
B. No
no - rectouterine is
rectovesical pouch only in males
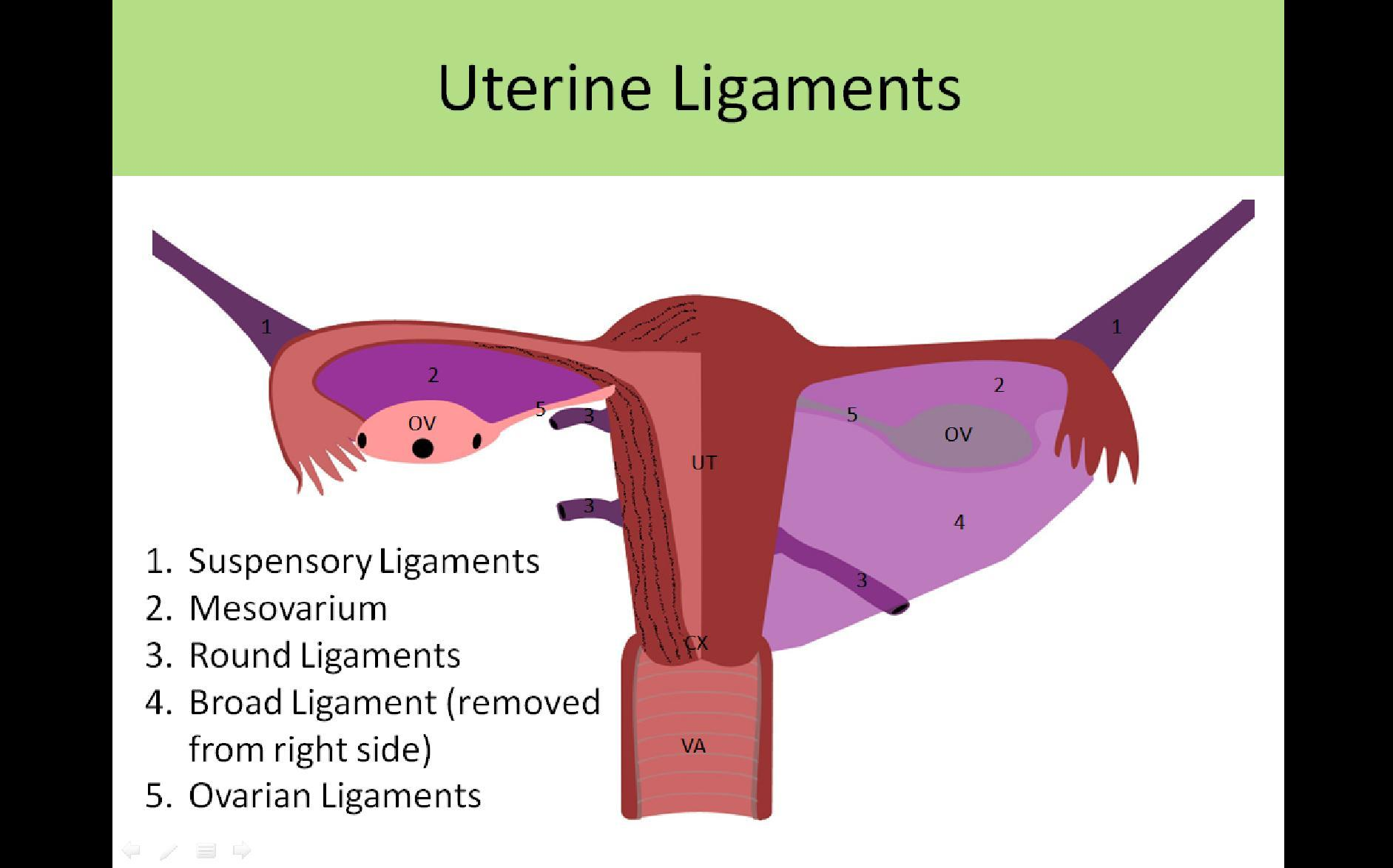
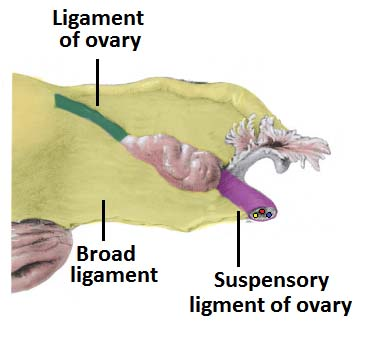
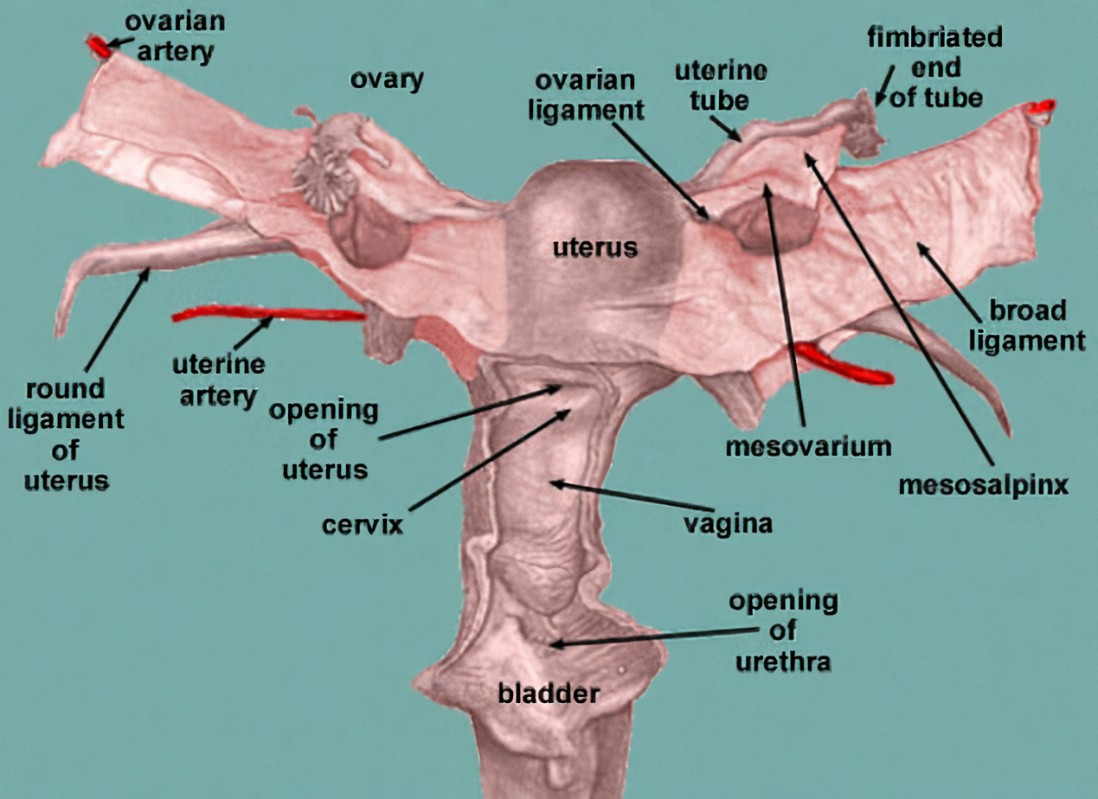
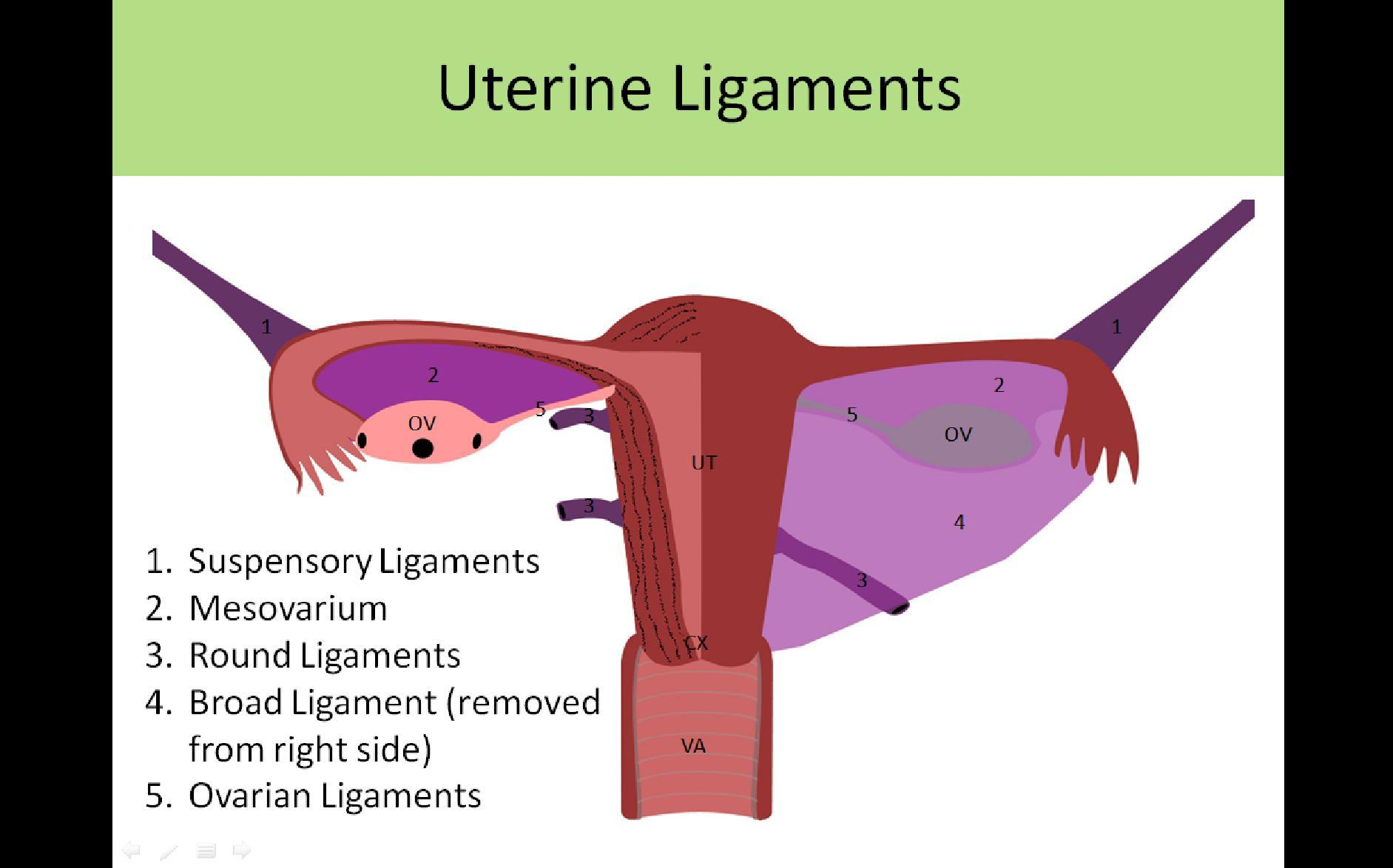
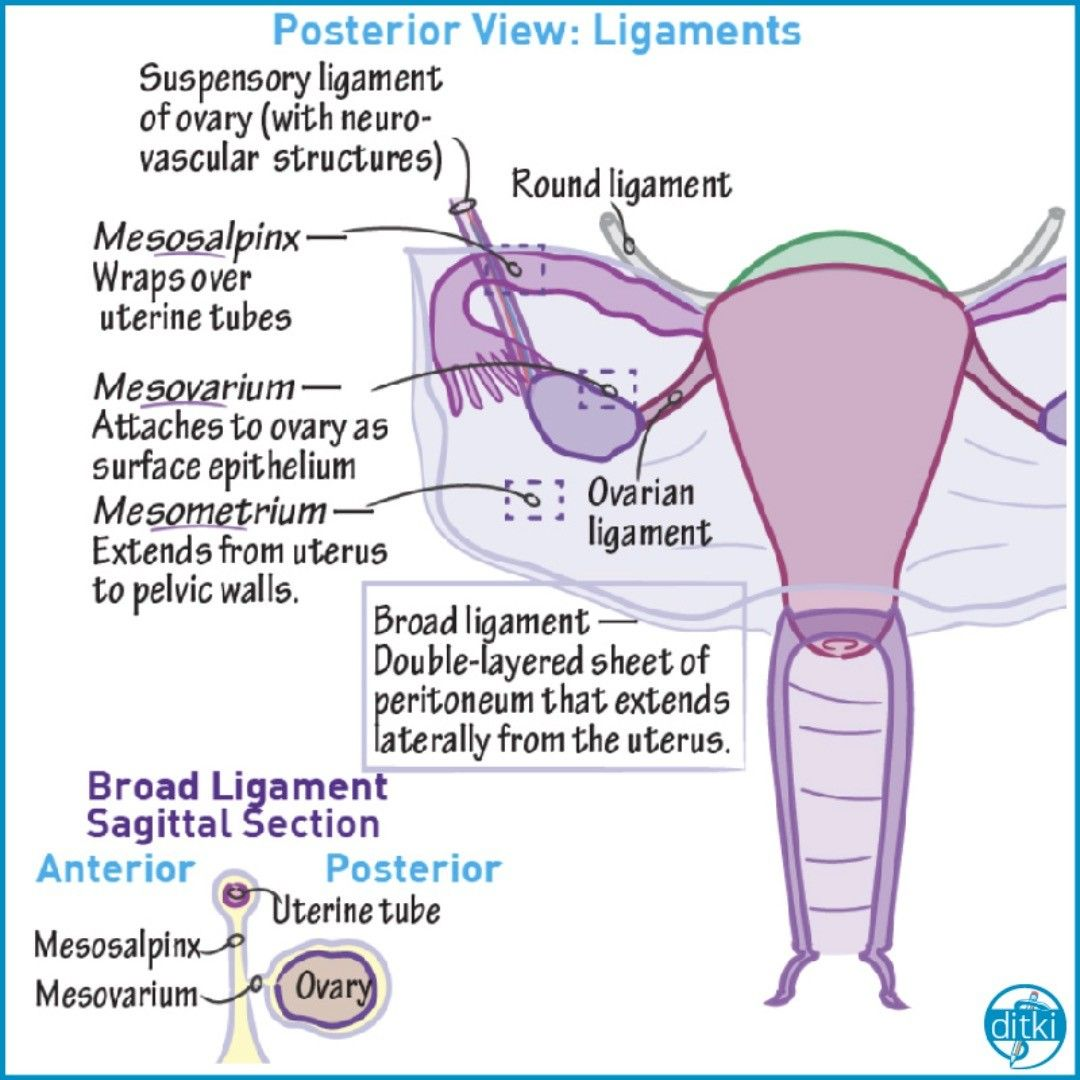
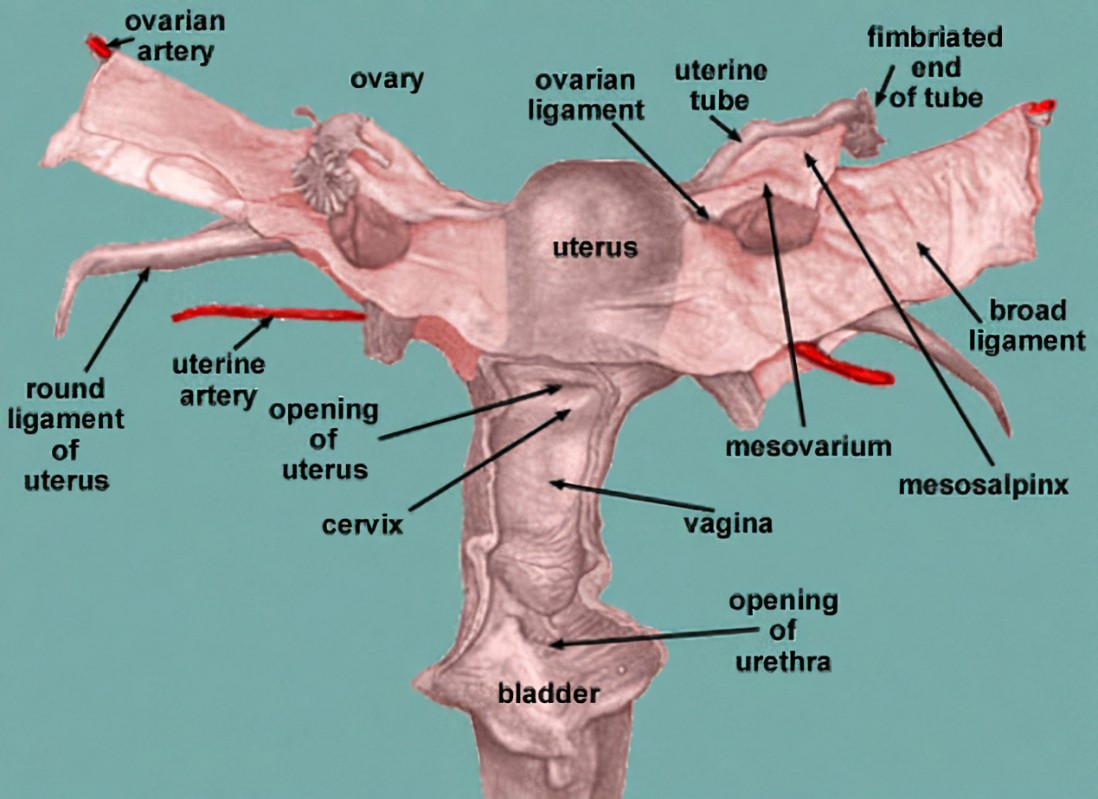
2. The broad ligament of the uterus serves to maintain its position
A. Yes
B. No
yes
3. Rectouterine pouch is the most inferior spot of peritoneal cavity in female subjects
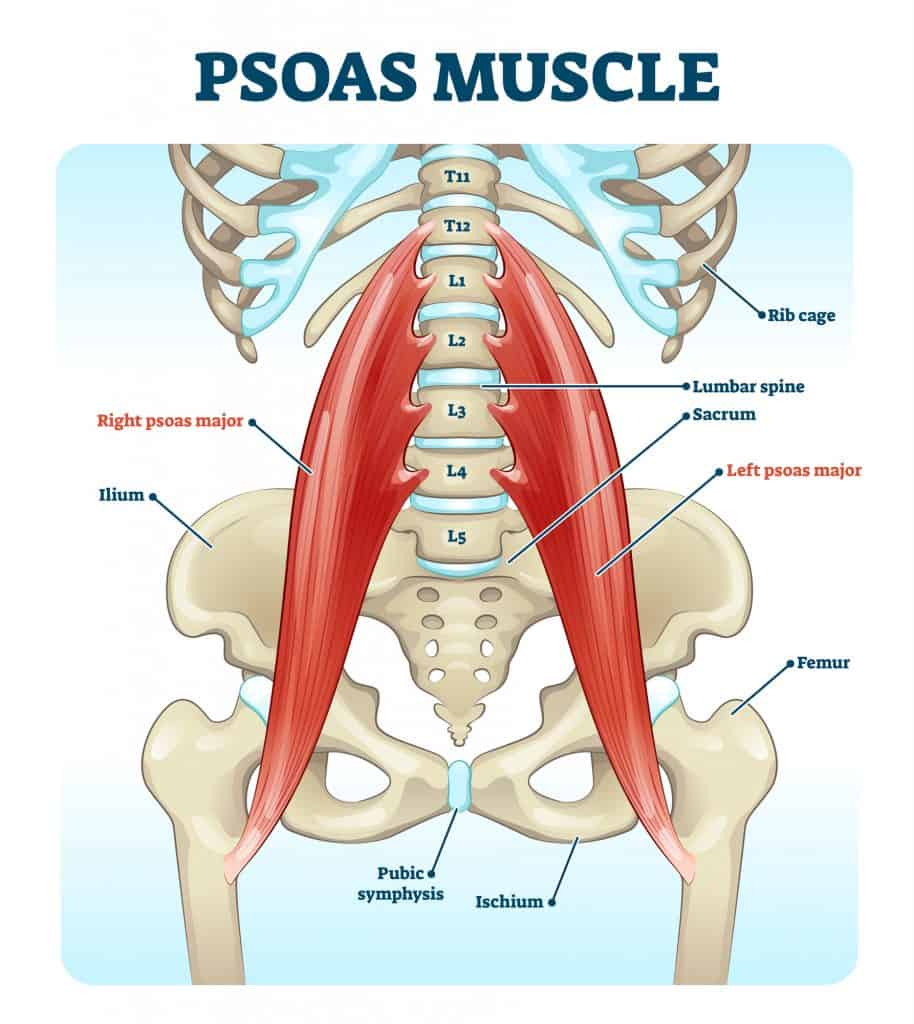
A. Yes
B. No
yes
4. The round ligament of uterus is part of its supporting structures
A. Yes
B. No
yes
5. Vesicouterine pouch is the most inferior spot of peritoneal cavity in female subjects
A. Yes
B. No
No
6. The ovarian ligament serves to maintain its position
A. Yes
B. No
yes
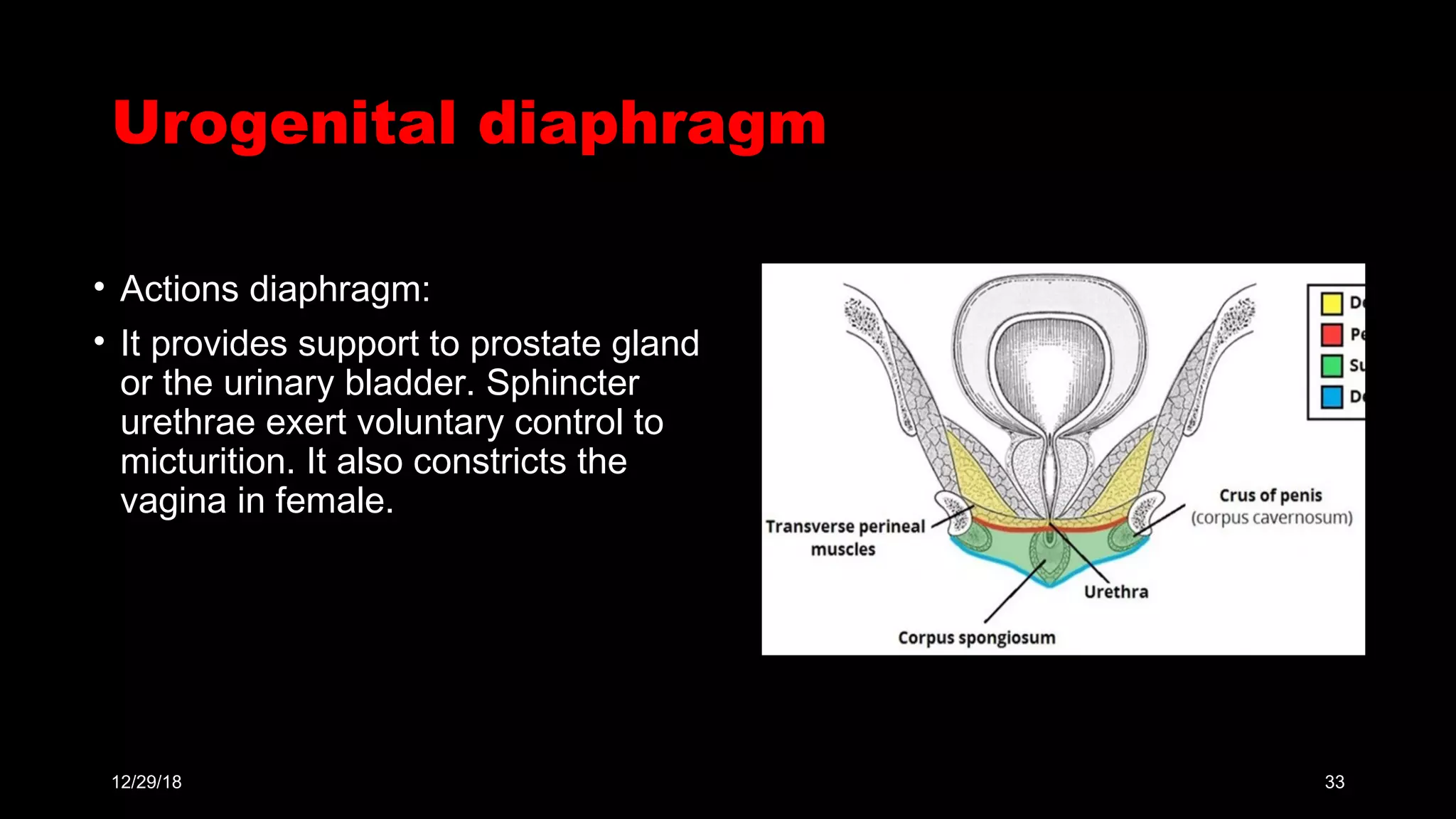
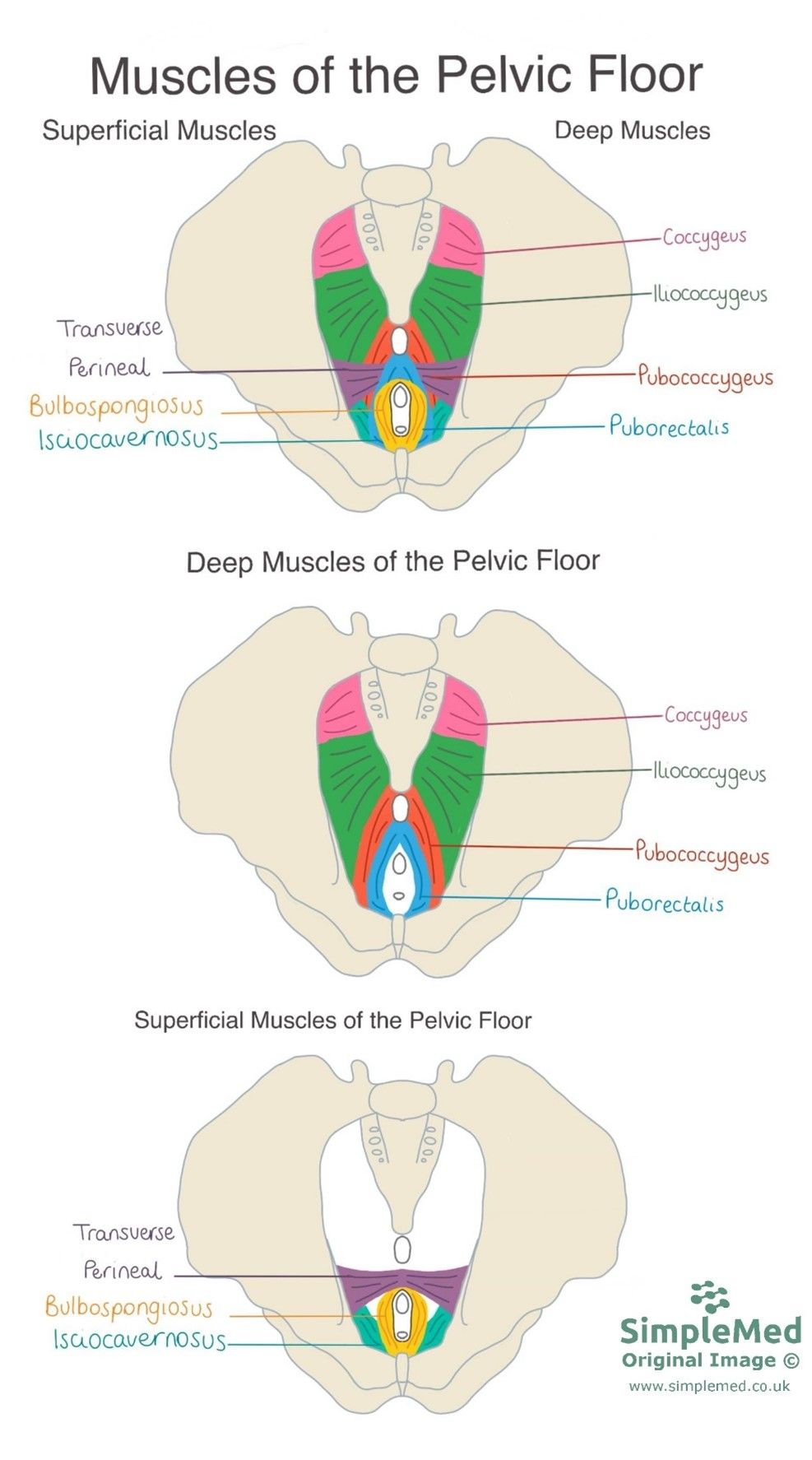
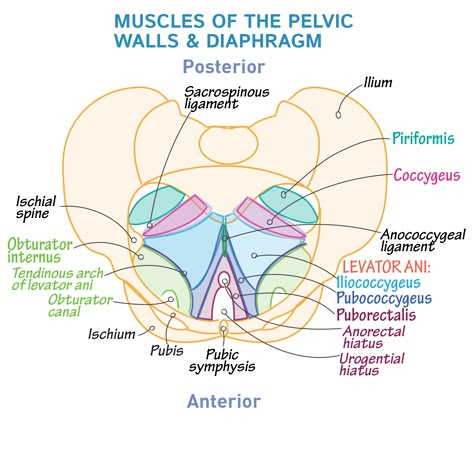
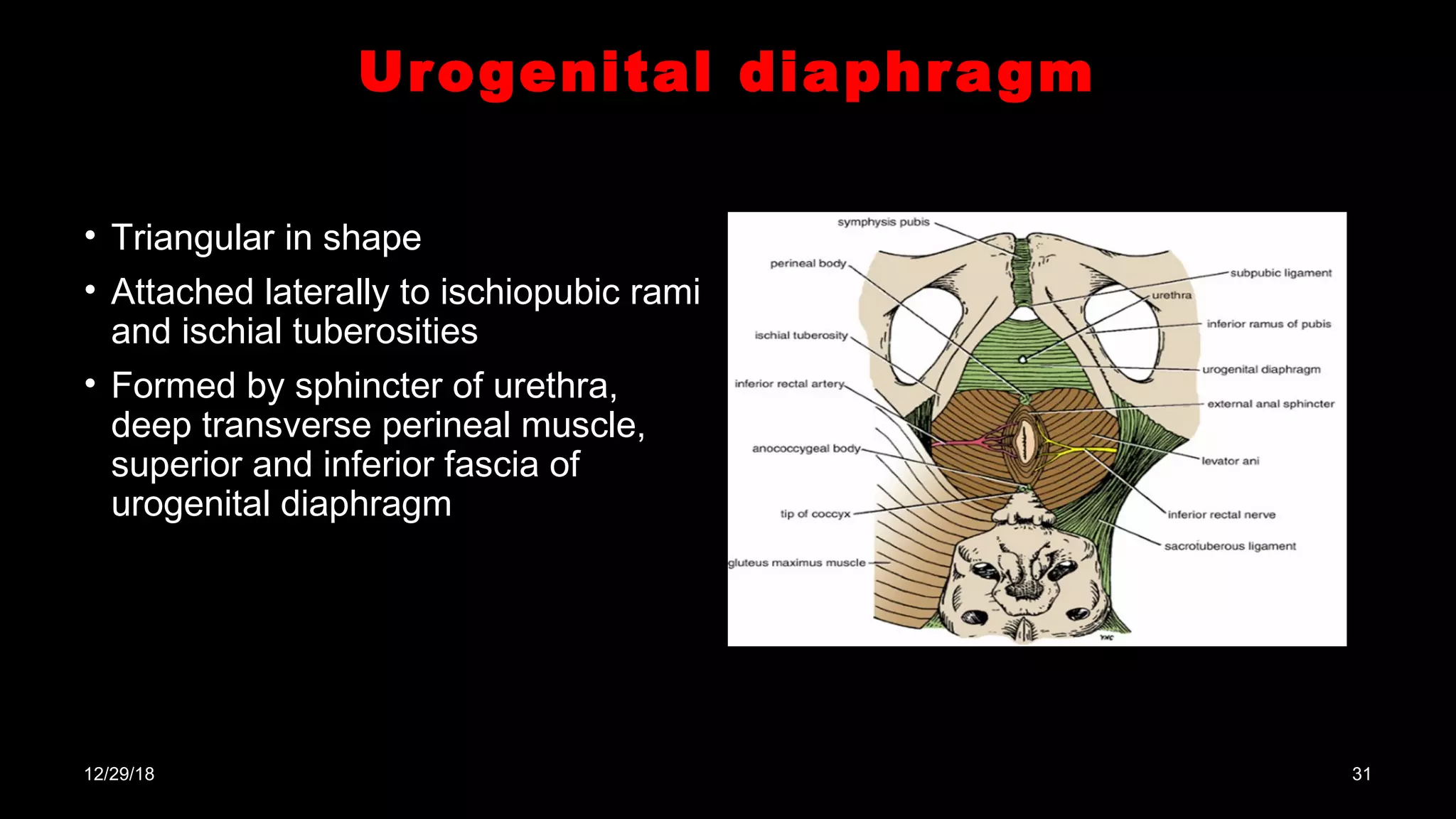
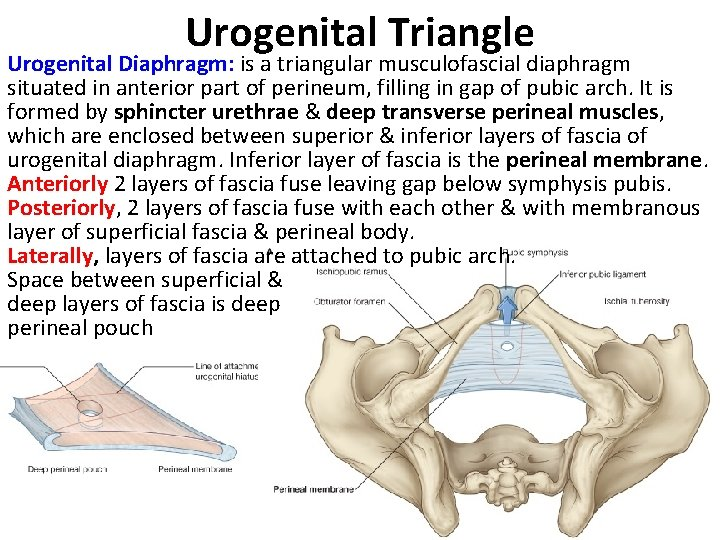
7. The coccygeus is a muscle of the urogenital diaphragm
A. Yes
B. No
no,
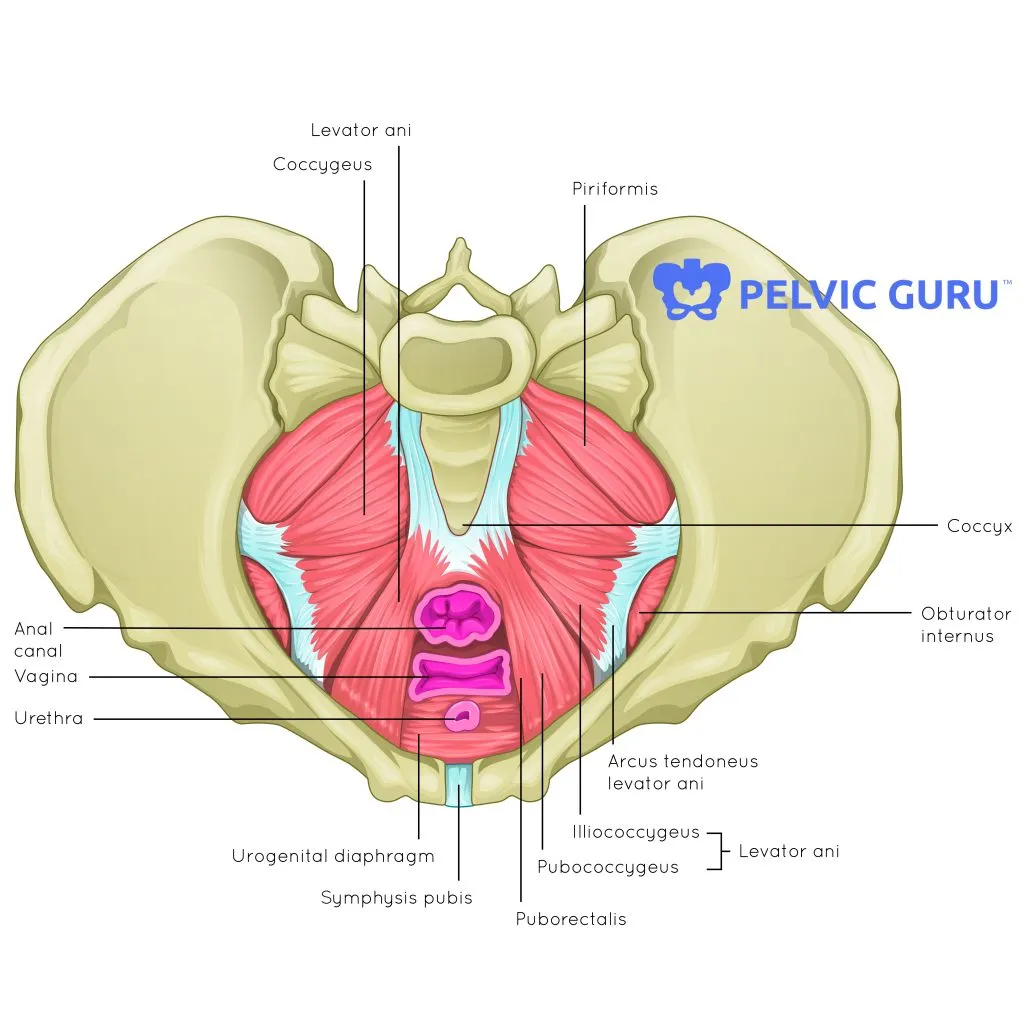
The Coccygeus is a muscle of the pelvic diaphragm
helps support the pelvic organs and is located posteriorly in the pelvic floor
urogenital diaphragm is primarily formed by the deep transverse perineal muscle and associated fascia
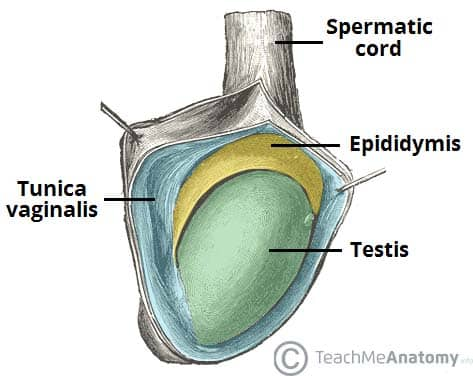
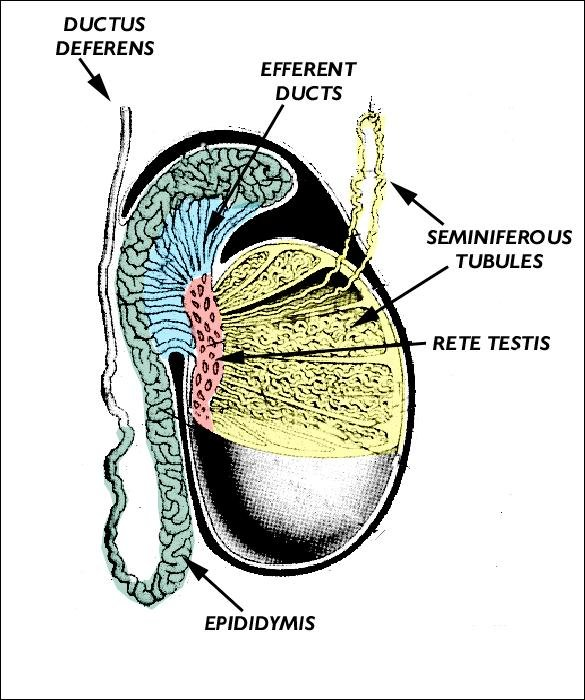
8. Tunica vaginalis testis is a derivative of peritoneum
A. Yes
B. No
yes
During fetal development, the testis descends from the abdomen into the scrotum, carrying a pouch of peritoneum with it, which forms the tunica vaginalis
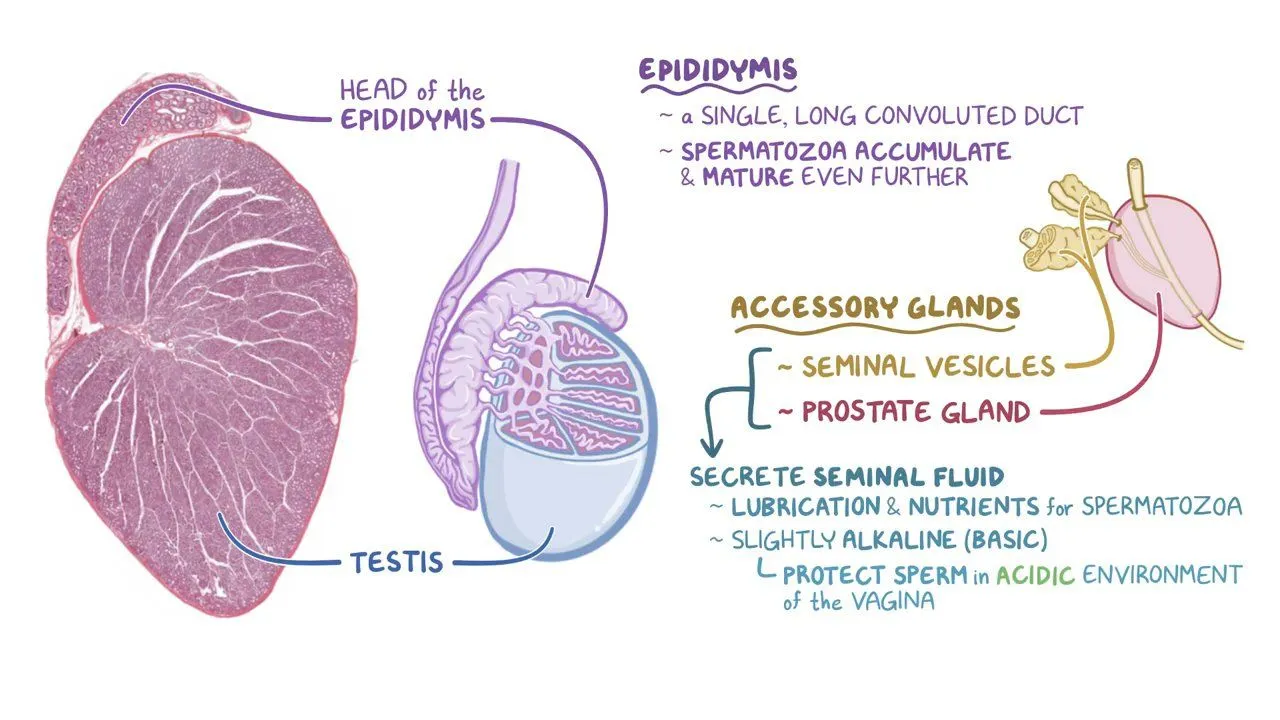
9. A sperm is stored in a seminal vesicle
A. Yes
B. No
No.
Sperm is not stored in the seminal vesicle
sperm is stored primarily in the epididymis before ejaculation
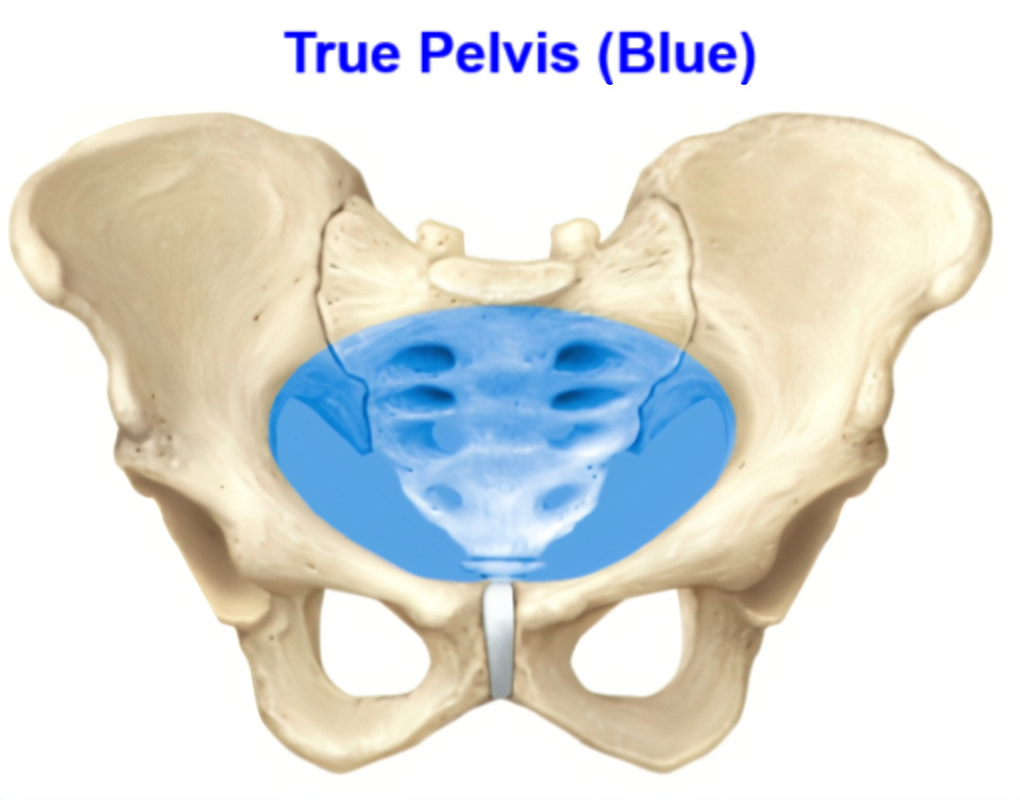
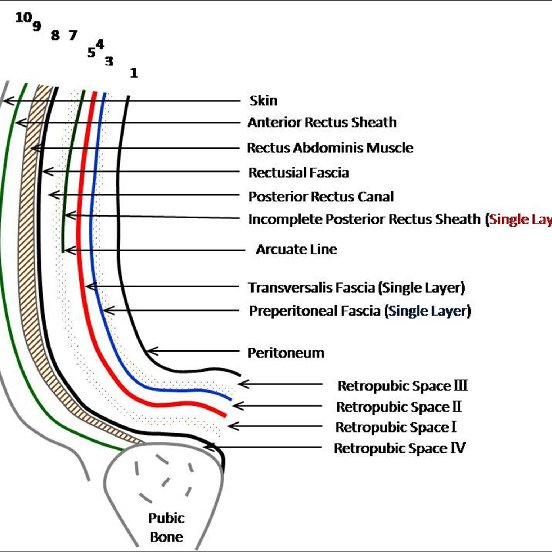
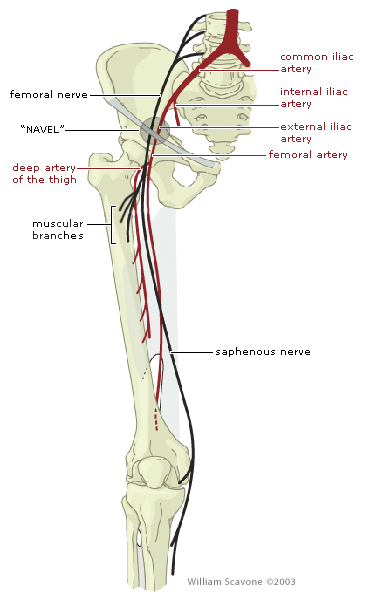
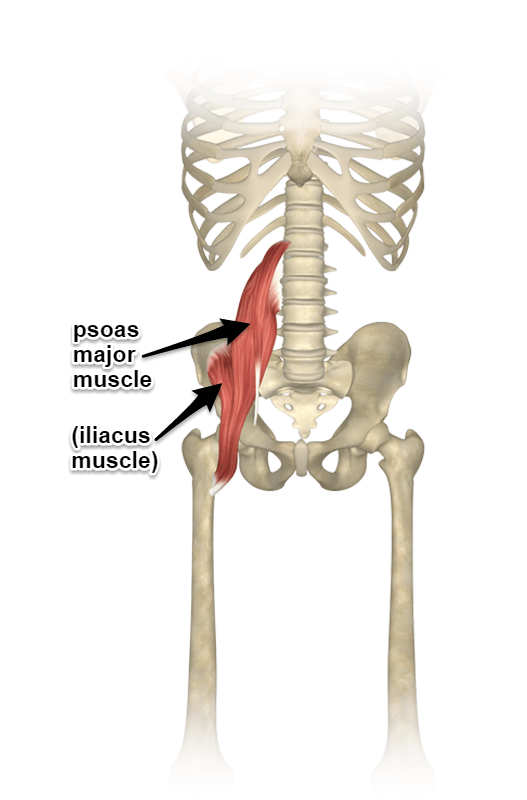
10. Psoas major is found in the true pelvis
A. Yes
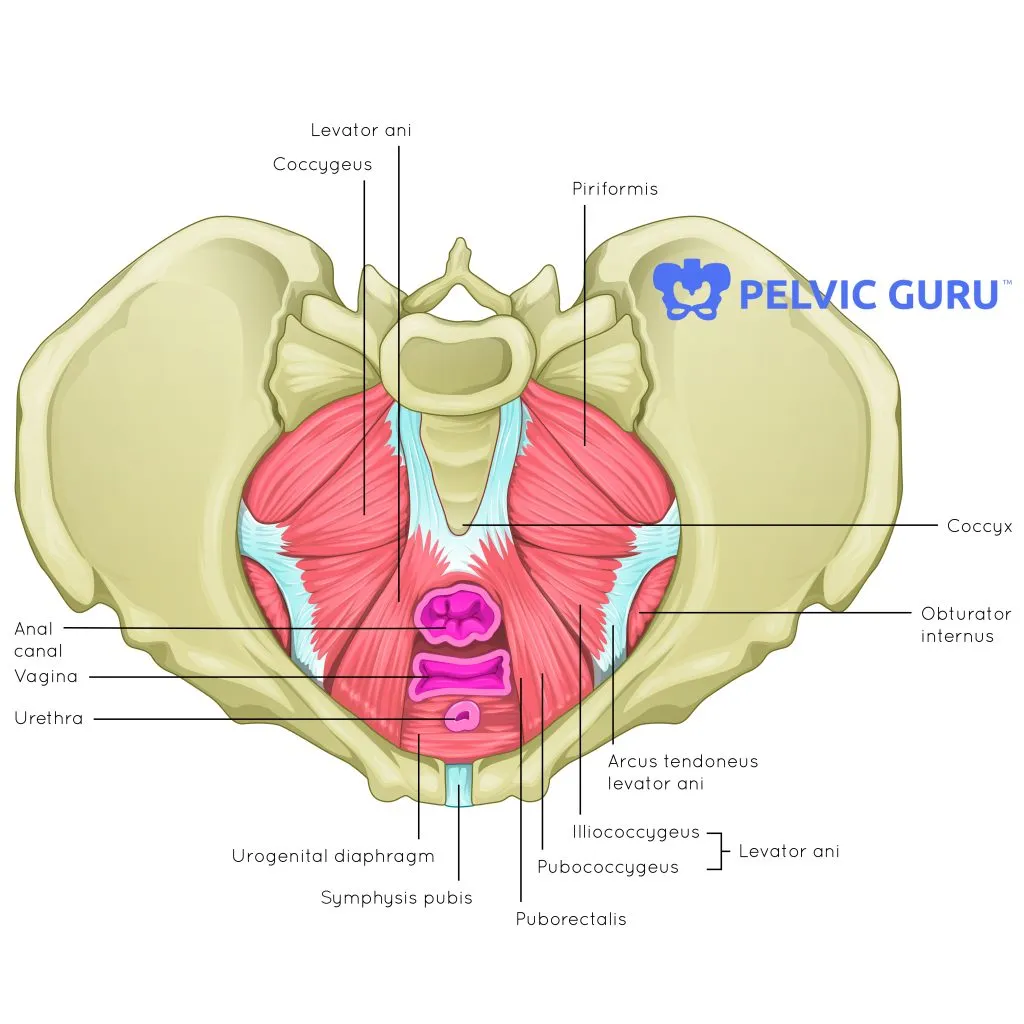
B. No
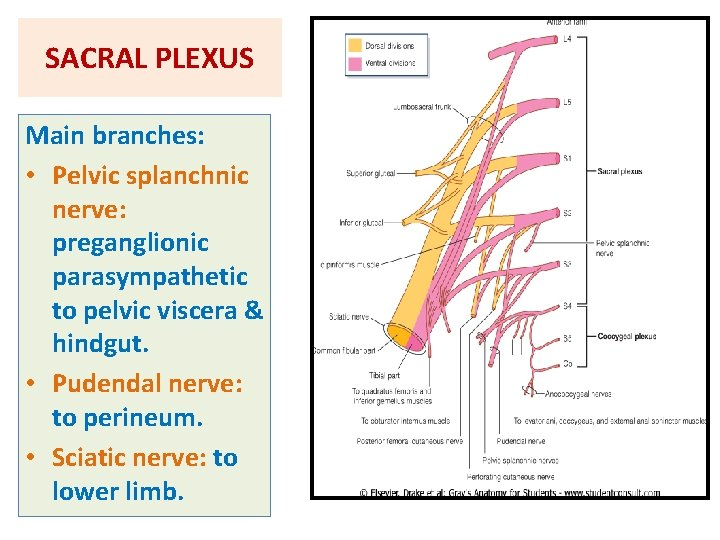
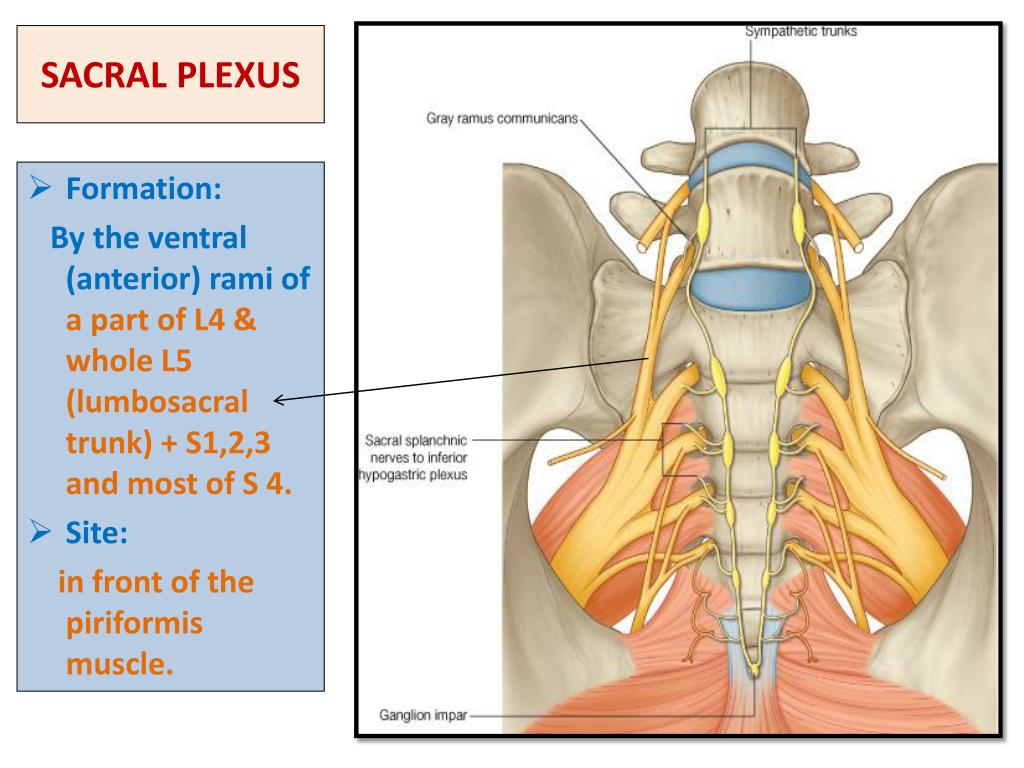
No
psoas major muscle lies in the posterior abdominal wall, outside the true pelvis
passes under the inguinal ligament to enter the thigh
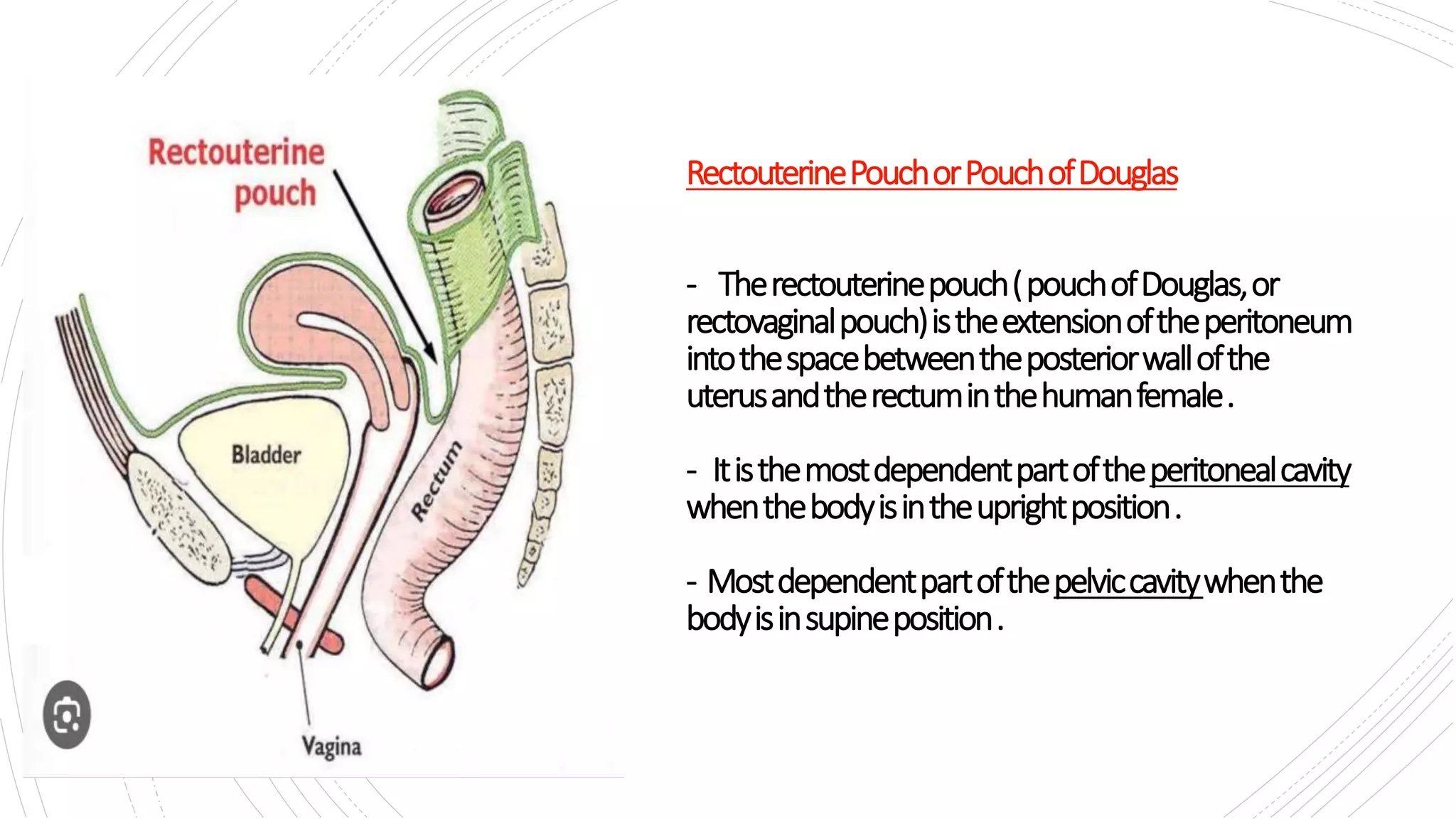
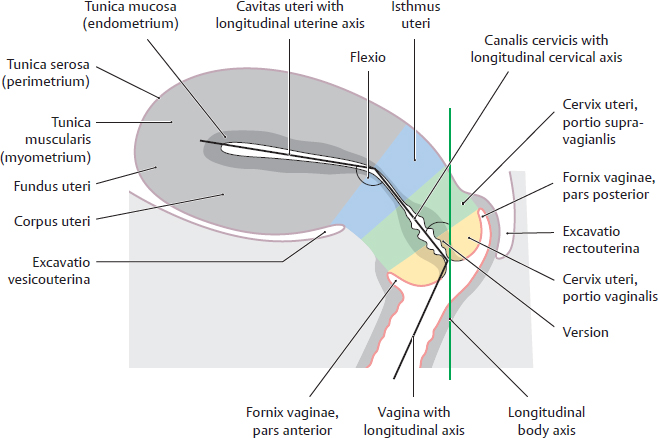
11. The anterior cul de sac is also known as the utero- vesicle space
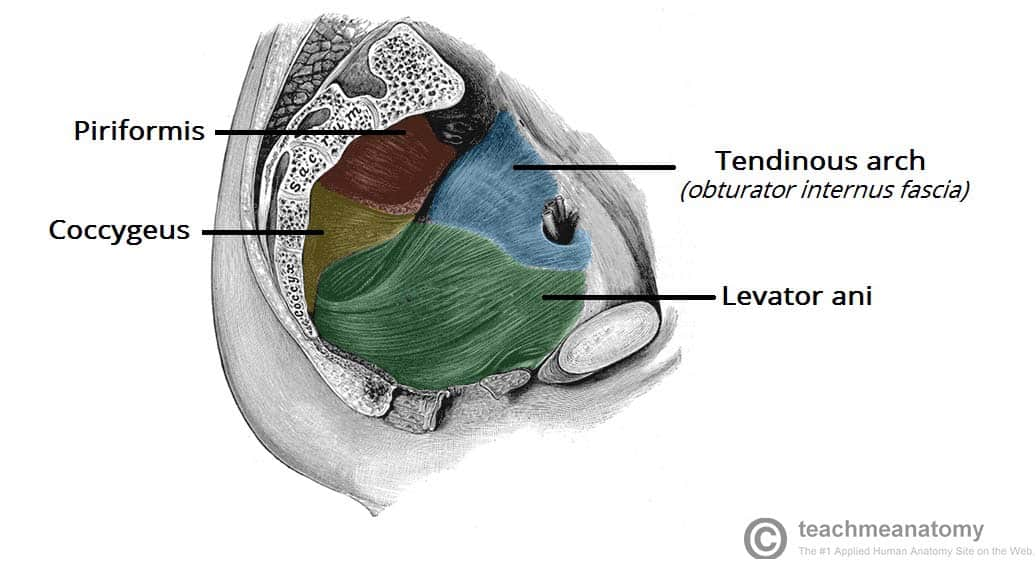
A. Yes
B. No
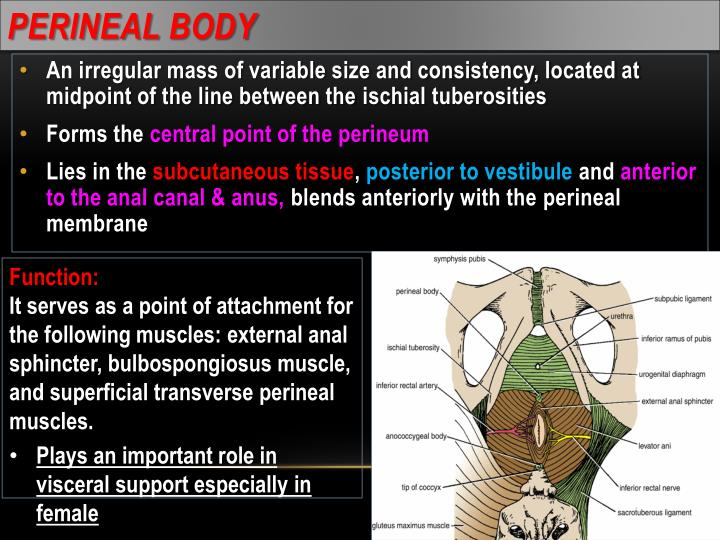
Yes
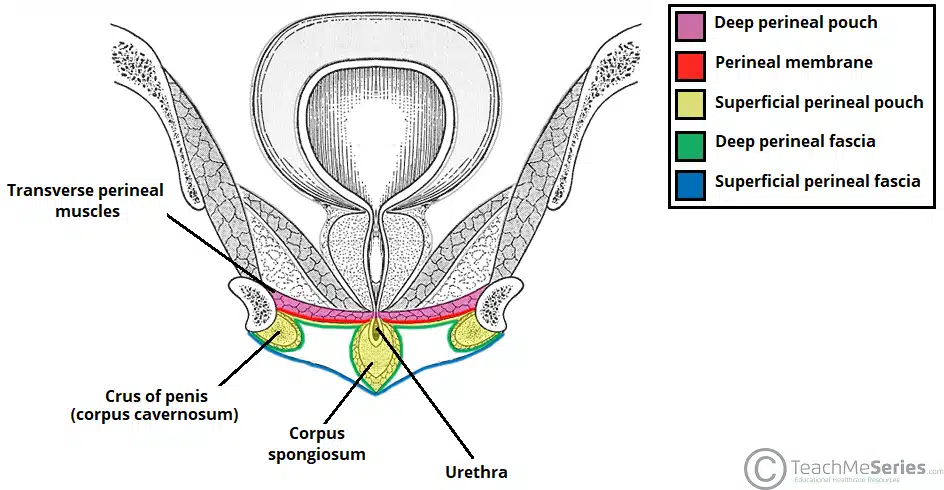
anterior cul-de-sac refers to the uterovesical pouch or uterovesical space
which is the peritoneal recess between the uterus and the urinary bladder
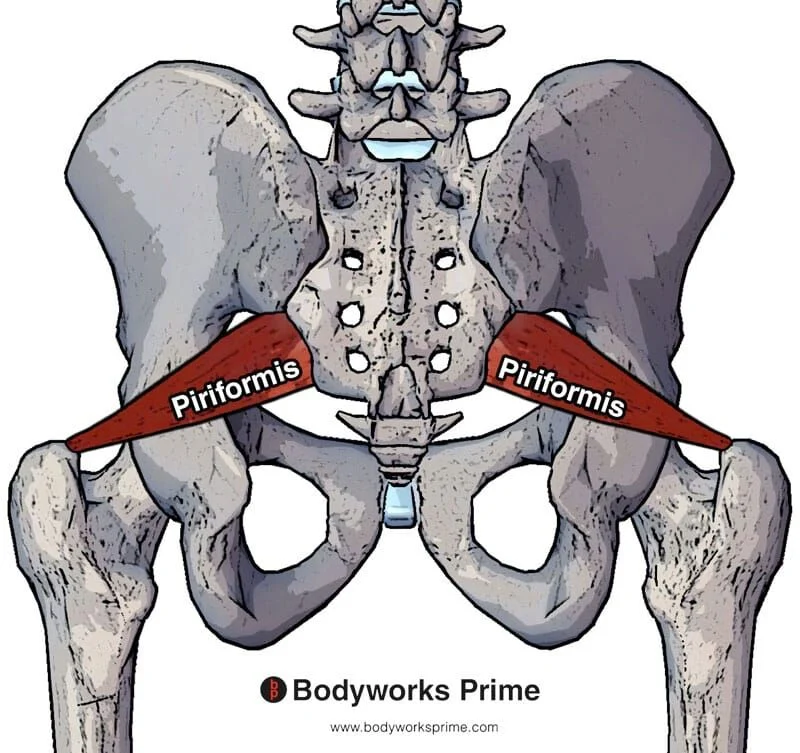
12. In relation to the levator ani muscles , the piriformis muscle is posterior and medial
yes or no
no
piriformis muscle is posterior and lateral to the levator ani muscles, not medial
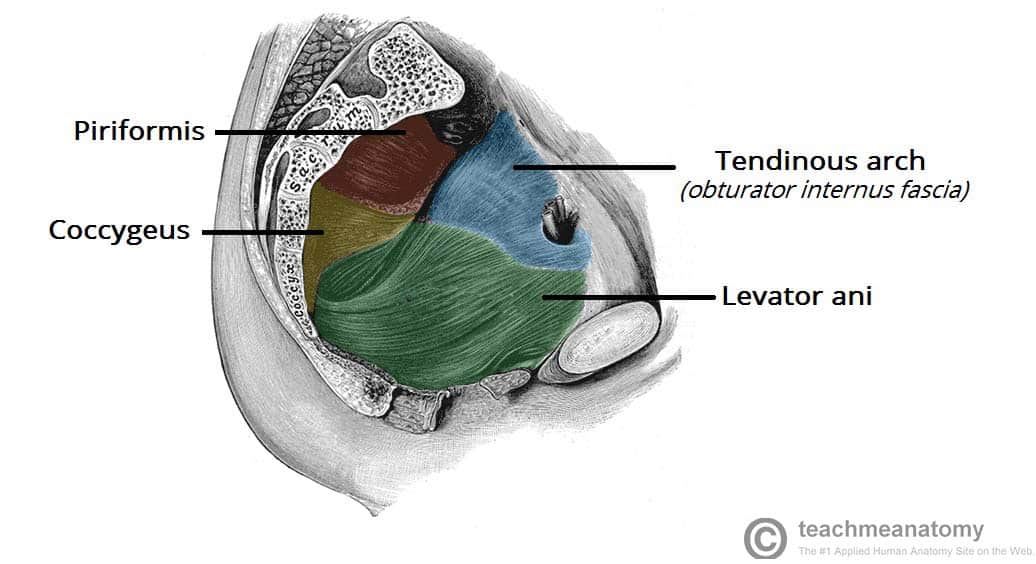
13. The portion of the uterus lying superior to the interstitial portion of the fallopian tubes is called the uterine fundus
yes or no
yes
uterine fundus is the part of the uterus that lies above (superior to) the openings of the fallopian tubes (interstitial portions)
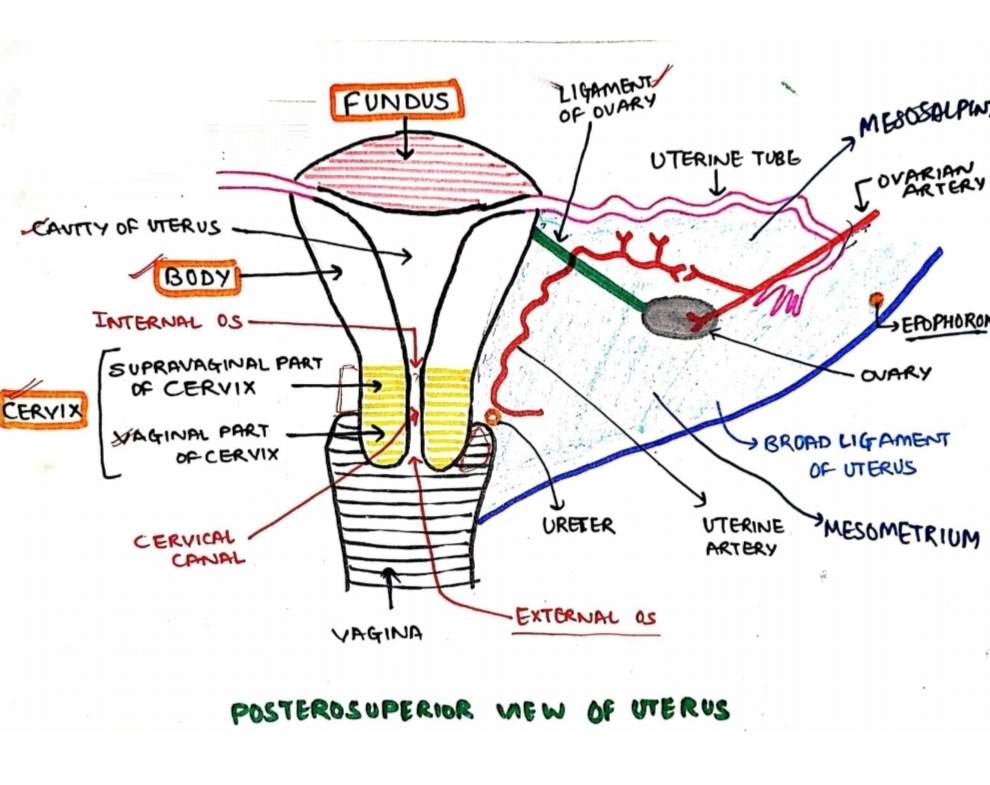
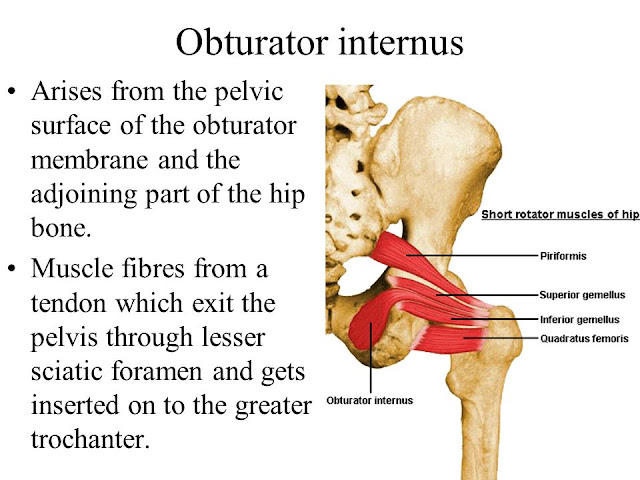
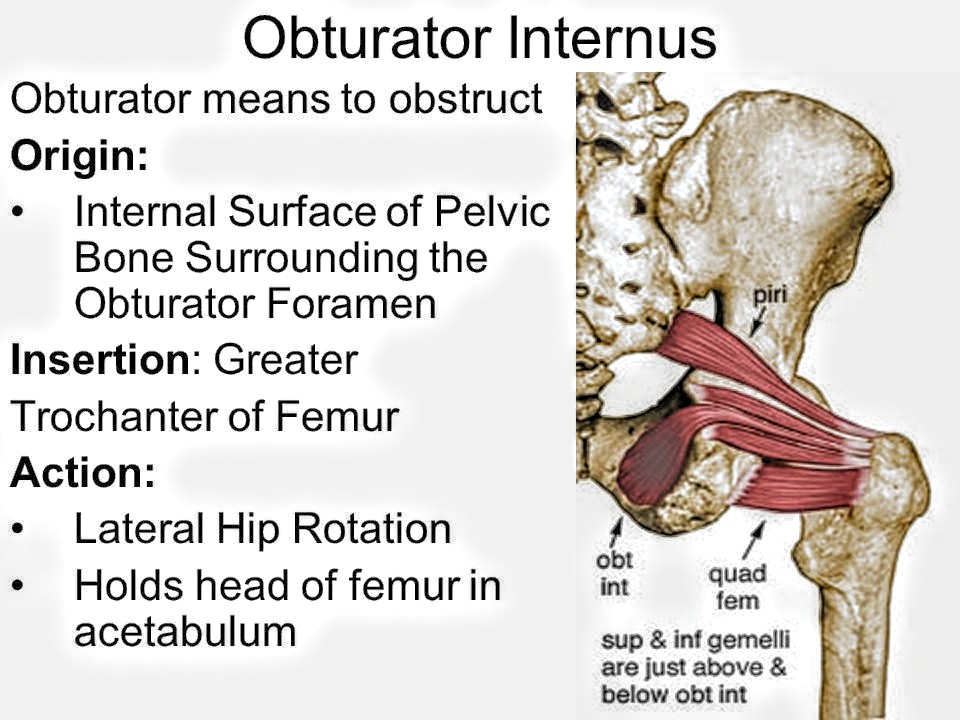
14. The thin plate- like muscles that line the lateral aspect of the pelvic space are the obturator interni
A. Yes
B. No
yes
obturator internus muscles are thin, flat muscles that cover the lateral walls of the true pelvis
15. The normal ovary is found anterior to the broad ligament
A. Yes
B. No
no
ovary is actually posterior (or behind) to the broad ligament, specifically attached to its posterior border by the mesovarium
lies in the ovarian fossa, which is behind the broad ligament
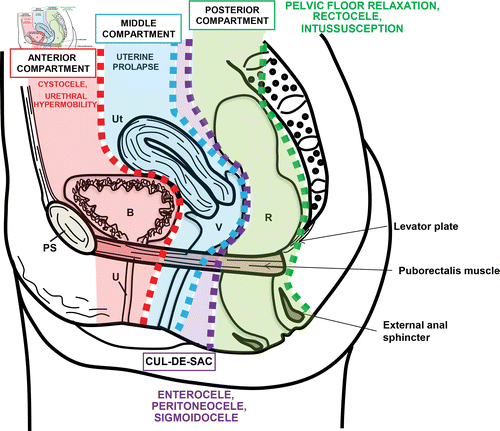
16. The retropubic space is also called the anterior cul de sac
A. Yes
B. No
No,
retropubic space (space of Retzius) is located between the pubic bone and the bladder, but it is not called the anterior cul-de-sac
anterior cul-de-sac refers specifically to the space between the bladder and the uterus in females (also called the vesicouterine pouch)
17. Is uterus perotinealized?
A. Yes
B. No
yes
uterus is partially covered by peritoneum, meaning it is peritonealized
peritoneum covers the fundus and body of the uterus anteriorly and posteriorly
forming pouches such as the vesicouterine pouch (in front) and rectouterine pouch (pouch of Douglas) (behind)
cervix is mostly not covered by peritoneum.
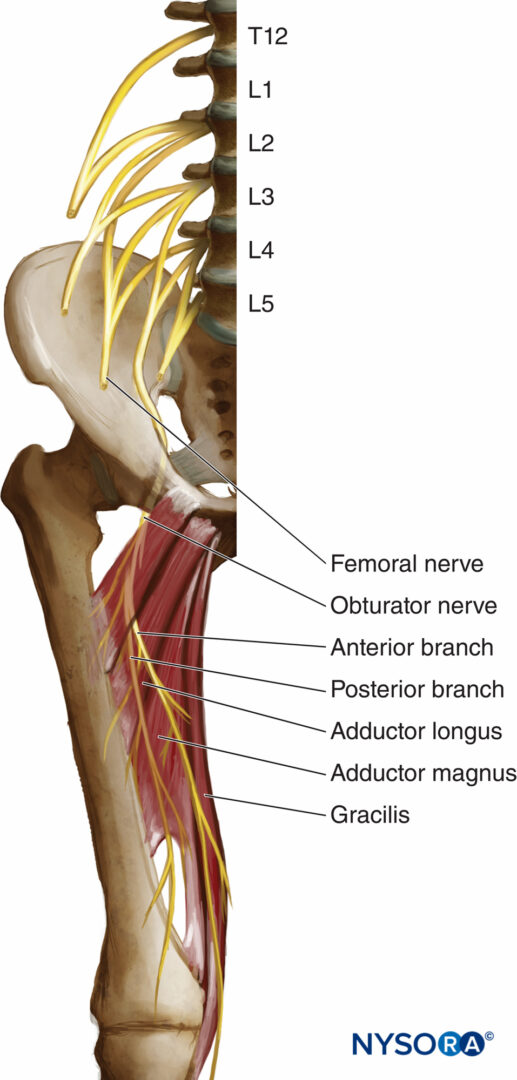
18. A 19yr old male suffers a tear to the psoas major muscle during the course of a football game. A scar, which formed on the medial part of the belly of the muscle , involved an adjacent nerve, immediately medial to the muscle. The nerve is called the:
A. femoral
B. genitofemoral
C. iliohypogastric
D. iliolingual
E. obturator
E. obturator
The obturator nerve runs along the medial border of the psoas major muscle
then travels into the pelvis to supply the medial thigh muscles.
The femoral nerve is lateral to the psoas major.
The genitofemoral nerve pierces the psoas but is on its anterior surface.
The iliohypogastric and ilioinguinal nerves are more superficial and lateral in the abdominal wall.
The iliolingual nerve isn’t an anatomical term (likely a confusion with iliolingual nerve, a branch of the lumbar plexus but less relevant here).
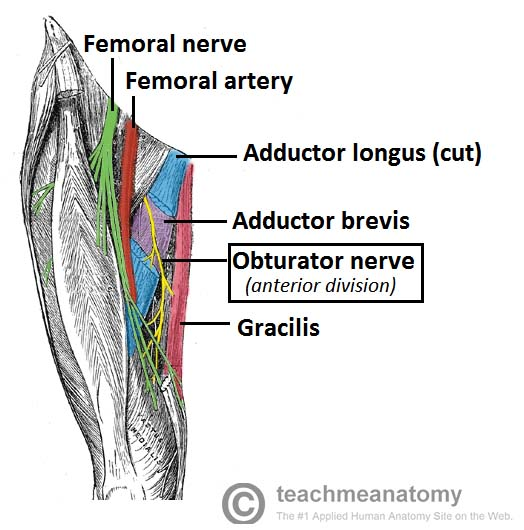
19. The nerves of the lumbar plexus are arranged around specific muscles of the posterior abdominal wall. Which of these nerve lies immediately medial to the psoas major muscle ?
A. femoral
B. genitofemoral
C. iliolingual
D. obturator
D. obturator
obturator nerve lies immediately medial to the psoas major muscle as it emerges from the lumbar plexus.
femoral nerve lies lateral to the psoas major.
The genitofemoral nerve pierces the anterior surface of the psoas muscle.
The ilioinguinal (likely what you meant by "iliolingual") nerve arises from the lateral border of psoas and runs more laterally
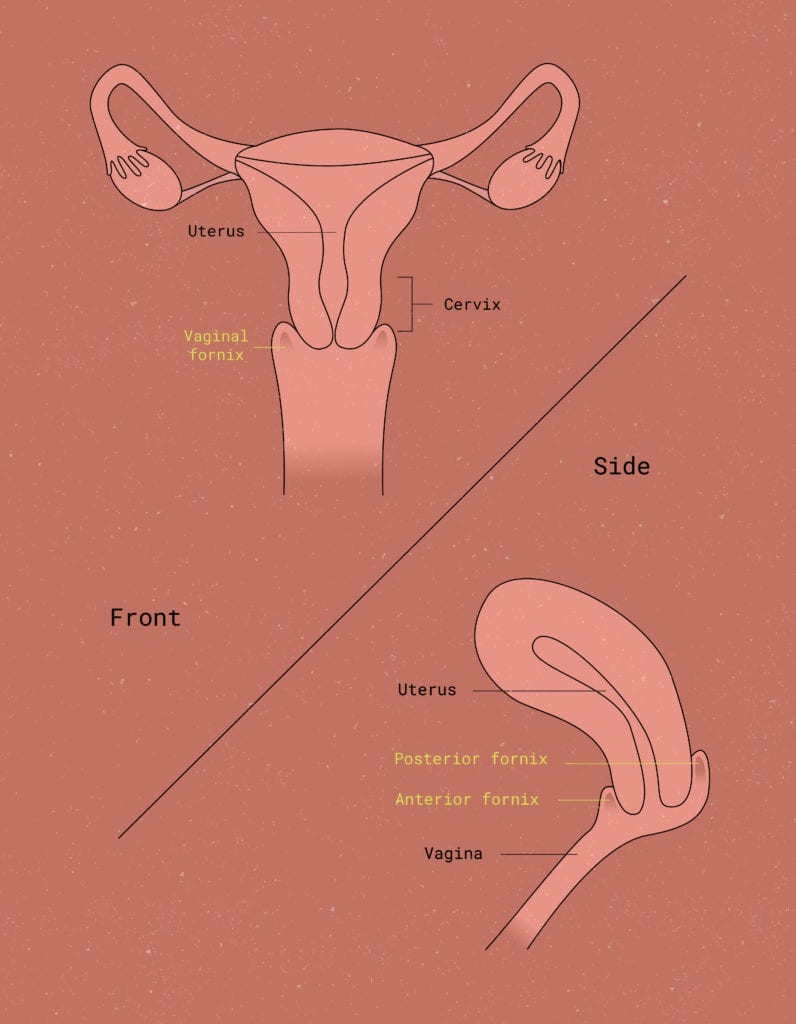
20. The extension of the vaginal lumen around the intravaginal part of the uterine cervix is the:
A. cervical canal
B. uterine lumen
C. fornix
D. rectouterine pouch
E. uterovesical pouch
C. fornix
fornix is the recess or extension of the vaginal lumen that surrounds the intravaginal part of the cervix
divided into anterior, posterior, and lateral fornices around the cervix.
cervical canal is the passage within the cervix itself.
The uterine lumen is the cavity inside the body of the uterus.
The rectouterine pouch (pouch of Douglas) is the peritoneal space between the uterus and rectum.
The uterovesical pouch is the peritoneal space between the uterus and bladder.
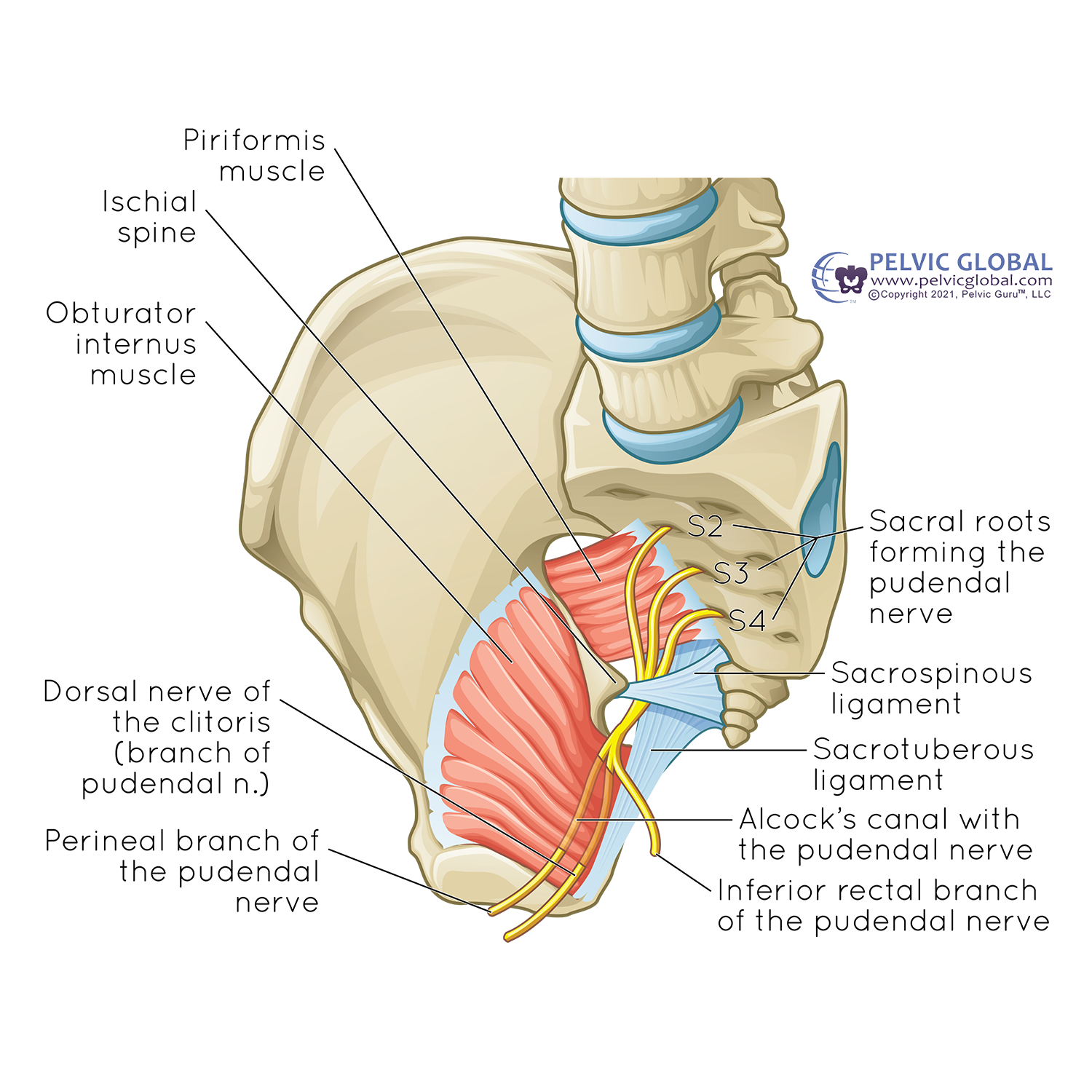
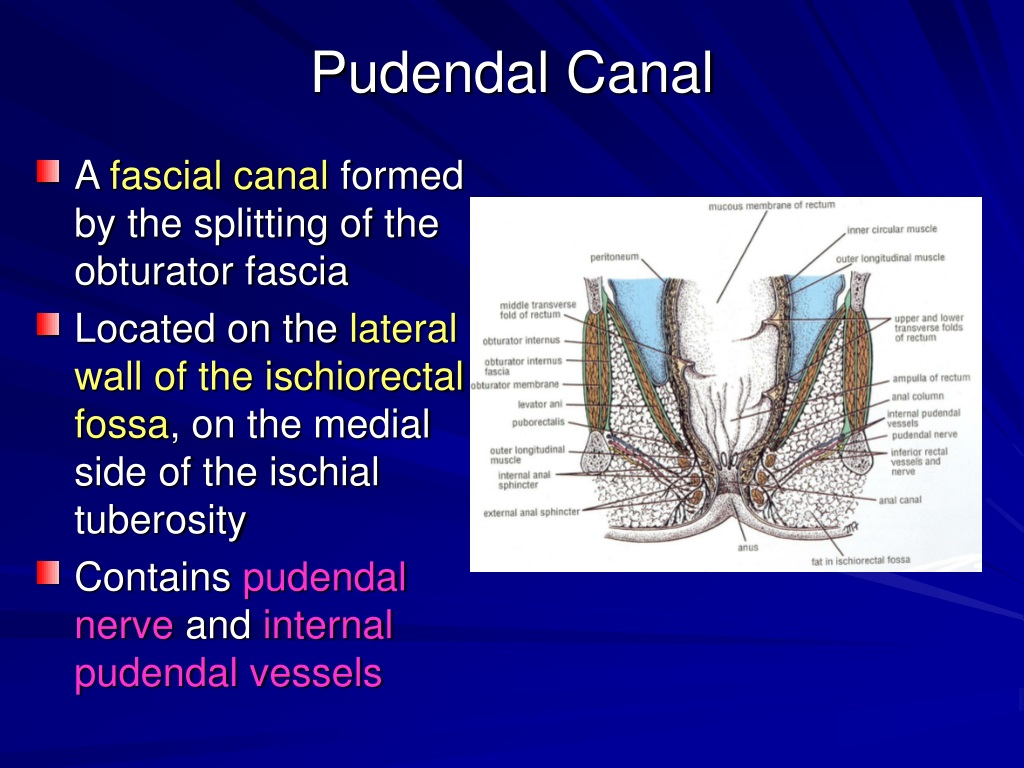
21. Which of the following would be most likely to be damaged by a stab wound into the ischiorectal (ischioanal) fossa 2cm lateral to the anal canal ?
A. crus of the penis
B. perineal body
C. pudendal nerve
D. inferior rectal artery
E. vesicular bulb
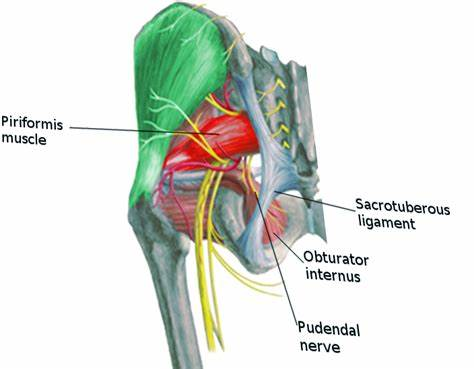
C. pudendal nerve
pudendal nerve runs through the ischiorectal (ischioanal) fossa within Alcock's canal (pudendal canal), which is located on the lateral wall of this fossa
stab wound 2 cm lateral to the anal canal can directly injure the pudendal nerve
supplies sensation to the perineum and motor innervation to the perineal muscles
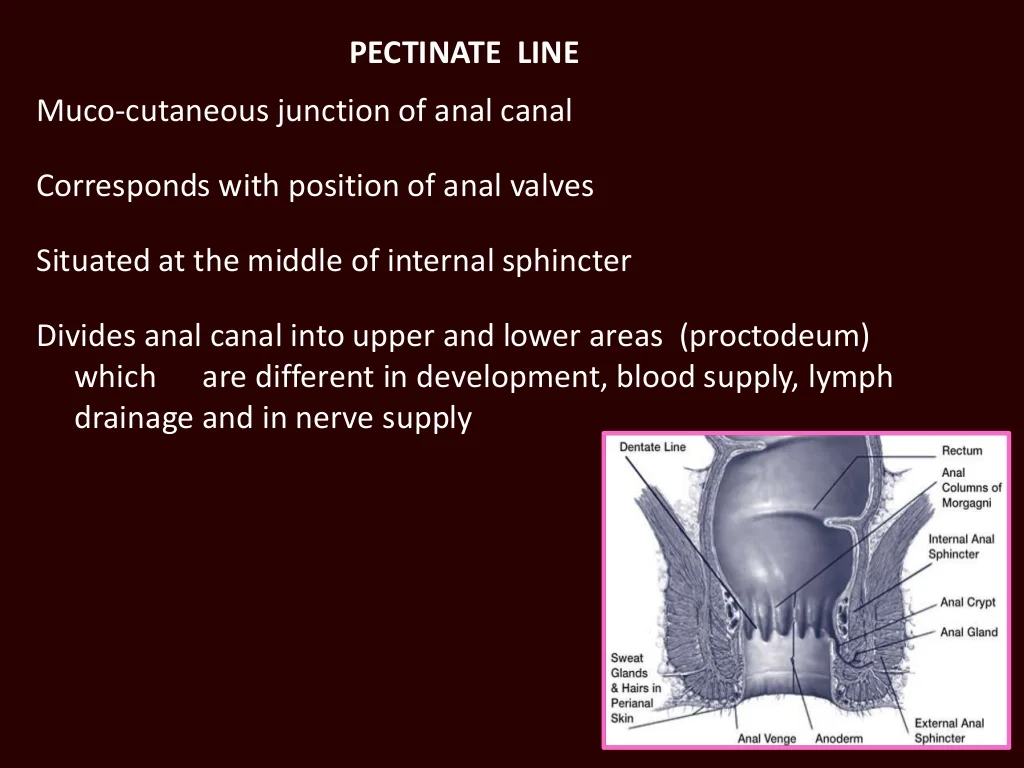
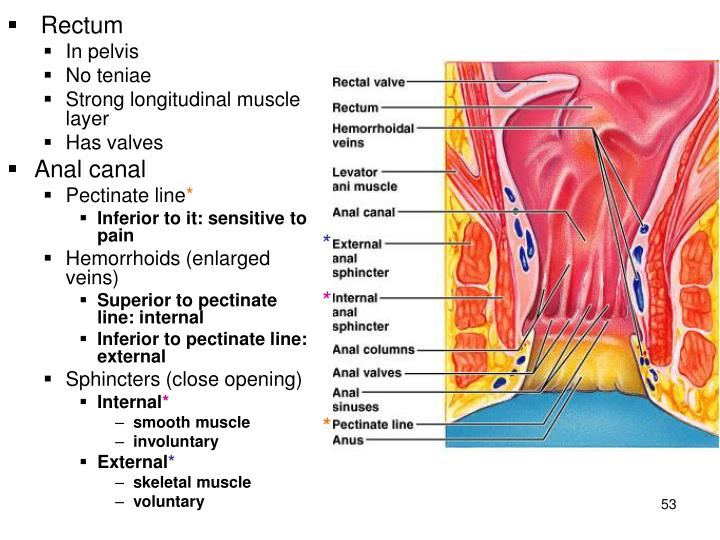
22. Lymphatic drainage of the terminal portion of gastrointestinal tract may flow initially into either the superficial inguinal nodes or the pararectal nodes, depending upon whether the lymph is formed above or below the:
A. anorectal junction
B. muscular sling of the puborectalis muscle
C. pectinate line
D. white line
E. cutaneous zone
C. pectinate line
pectinate line (also known as the dentate line) is the key anatomical landmark that divides the upper and lower parts of the anal canal
have different lymphatic drainage patterns:
Above the pectinate line: Lymph drains into the pararectal nodes and then to the internal iliac nodes.
Below the pectinate line: Lymph drains into the superficial inguinal nodes.
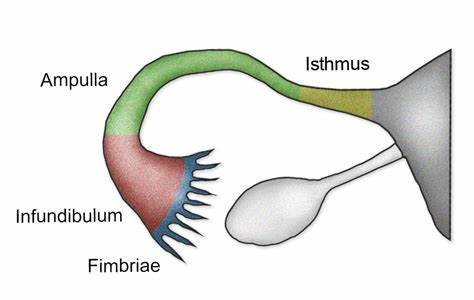
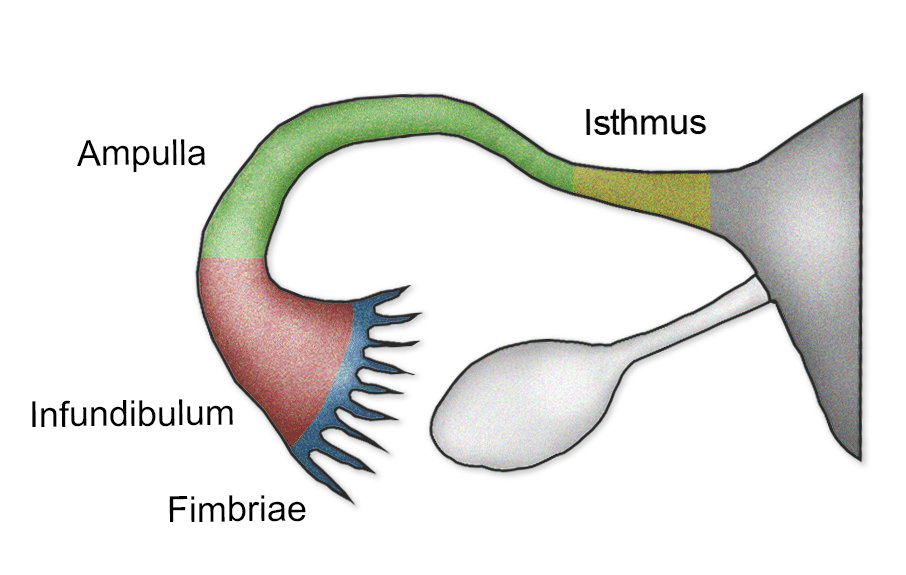
23. Under normal conditions, ferilization occurs in which part of the female reproductive tract?
A. infundibulum of the uterine tube
B. ampulla of the uterine tube
C. isthmus of the uterine tube
D. uterine lumen
E. cervical canal
B. ampulla of the uterine tube
! Fertilization normally takes place in the ampulla of the uterine tube.
!This is the middle segment of the uterine tube, and it is the longest and widest segment
infundibulum is the funnel-shaped opening with fimbriae that capture the ovulated egg but is not the usual site of fertilization
isthmus is the narrow section closer to the uterus and is primarily a passage for the fertilized egg
uterine lumen is where the fertilized egg implants, not where fertilization occurs
cervical canal is the passage between the vagina and the uterus, not involved in fertilization
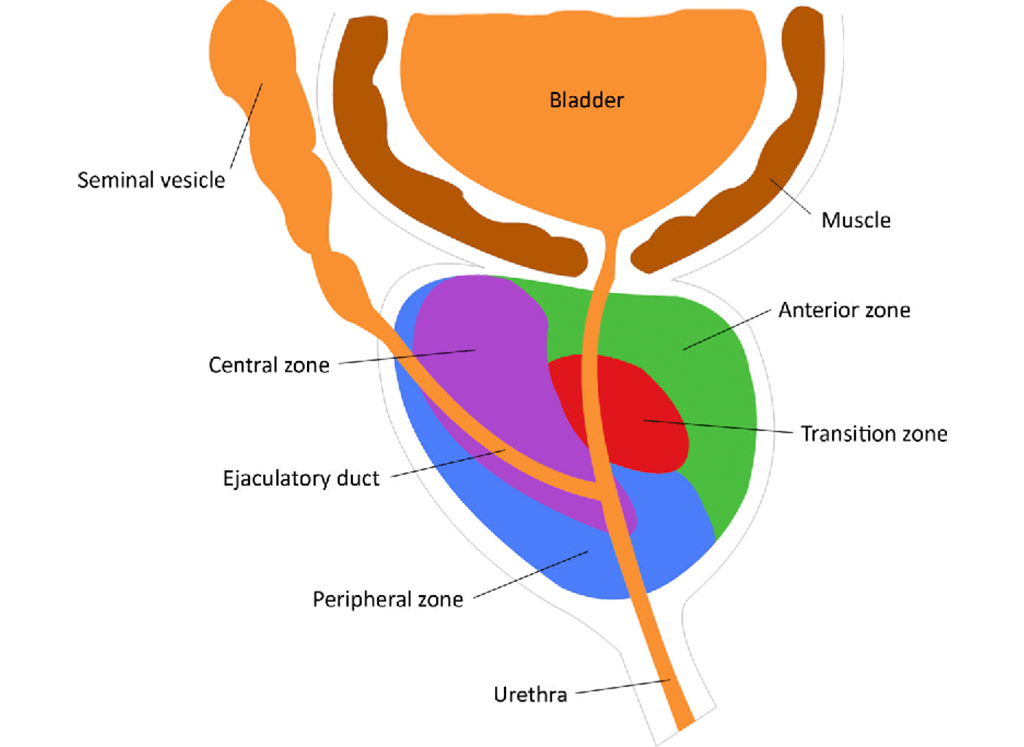
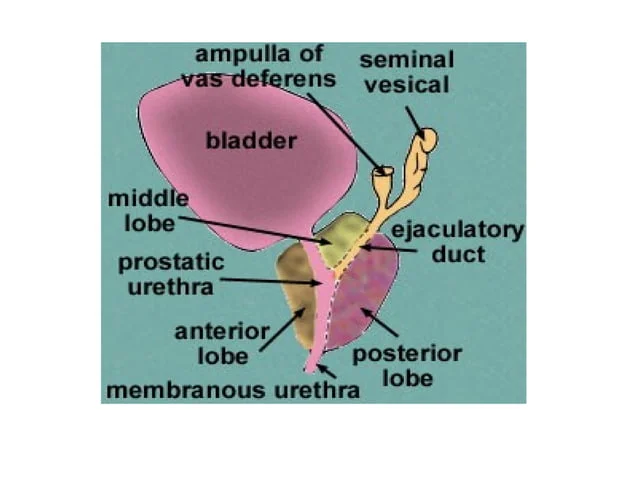
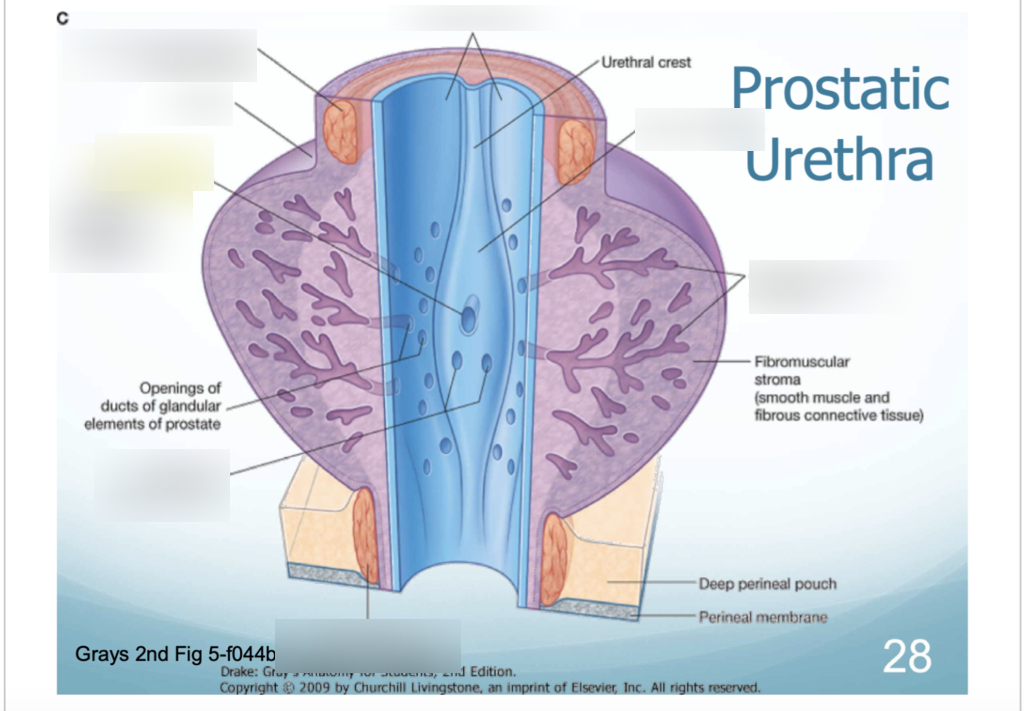
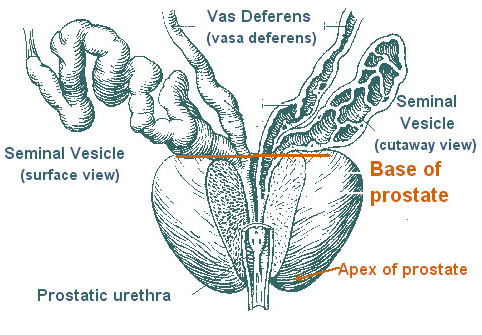
24. Benign hyperplasia ( excessive growth of cells ) of which part of the male reproductive system would be most likely to interfere with the passage of urine?
A. periurethral zone of the prostate
B. central zone of the prostate
C. peripeheral zone of the prostate
D. ejaculatory duct
E. seminal vesicle
A. periurethral zone of the prostate
This zone surrounds the prostatic urethra, and hyperplasia here directly compresses the urethra
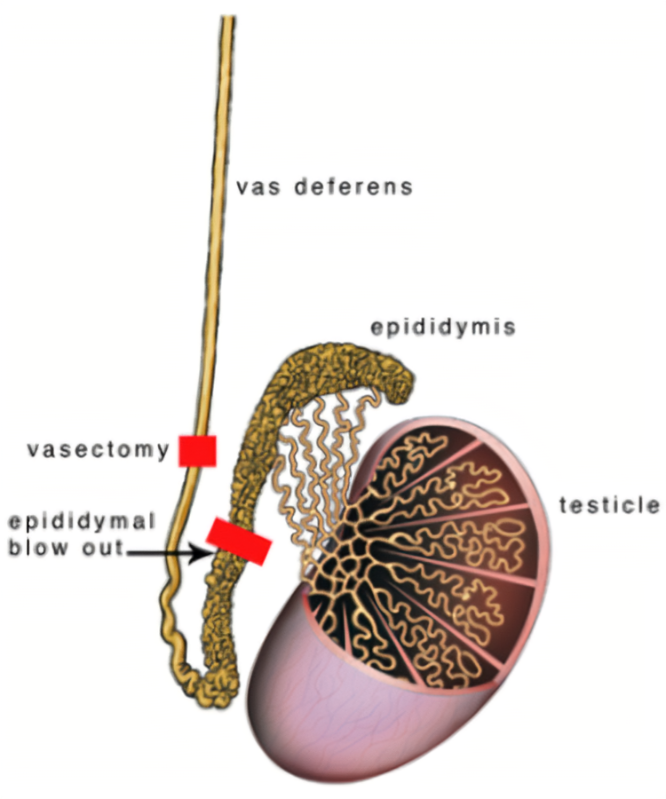
25. After agreeing to have no more children, a man and his wife decided he should has a vasectomy. What structure would then be surgically ligated ?
A. ductus deferens
B. ejaculatory duct
C. epididymis
D. fossa navicularis
E. seminal vesicle
A. ductus deferens
ductus deferens (vas deferens) is ligated (cut and sealed).
prevents sperm from traveling from the testes to the urethra, making the man sterile
ejaculatory duct is further downstream and is not directly cut.
The epididymis is where sperm matures but is not surgically manipulated in a vasectomy.
The fossa navicularis is part of the penile urethra, unrelated to sperm transport.
The seminal vesicle produces seminal fluid but does not carry sperm.
26. Which pair of structures does NOT differentiate from comparable embryonic structures in the male and female?
A. Bulb of corpus spongeosum and vestibular bulb
B. Shaft of penis and labia majora
C. Glans of penis and glans of clitoris
D. Crus of corpus cavernosum penis and crus of corpus
cavernosum clitoris
B. Shaft of penis and labia majora
shaft of the penis in males is derived from the genital tubercle and urethral folds, while the labia majora in females develop from the genital swellings, making them non-homologous structures
bulb of the corpus spongiosum (male) and the vestibular bulb (female) are homologous, both derived from the urogenital sinus
glans of the penis (male) and the glans of the clitoris (female) are homologous, both derived from the genital tubercle
crura of the corpus cavernosum in both males and females are homologous, derived from the same genital tubercle structure
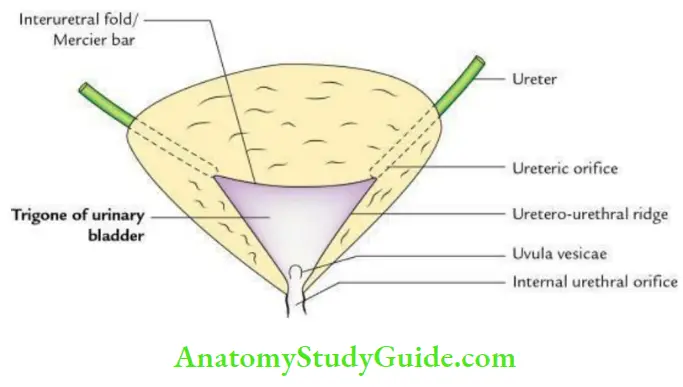
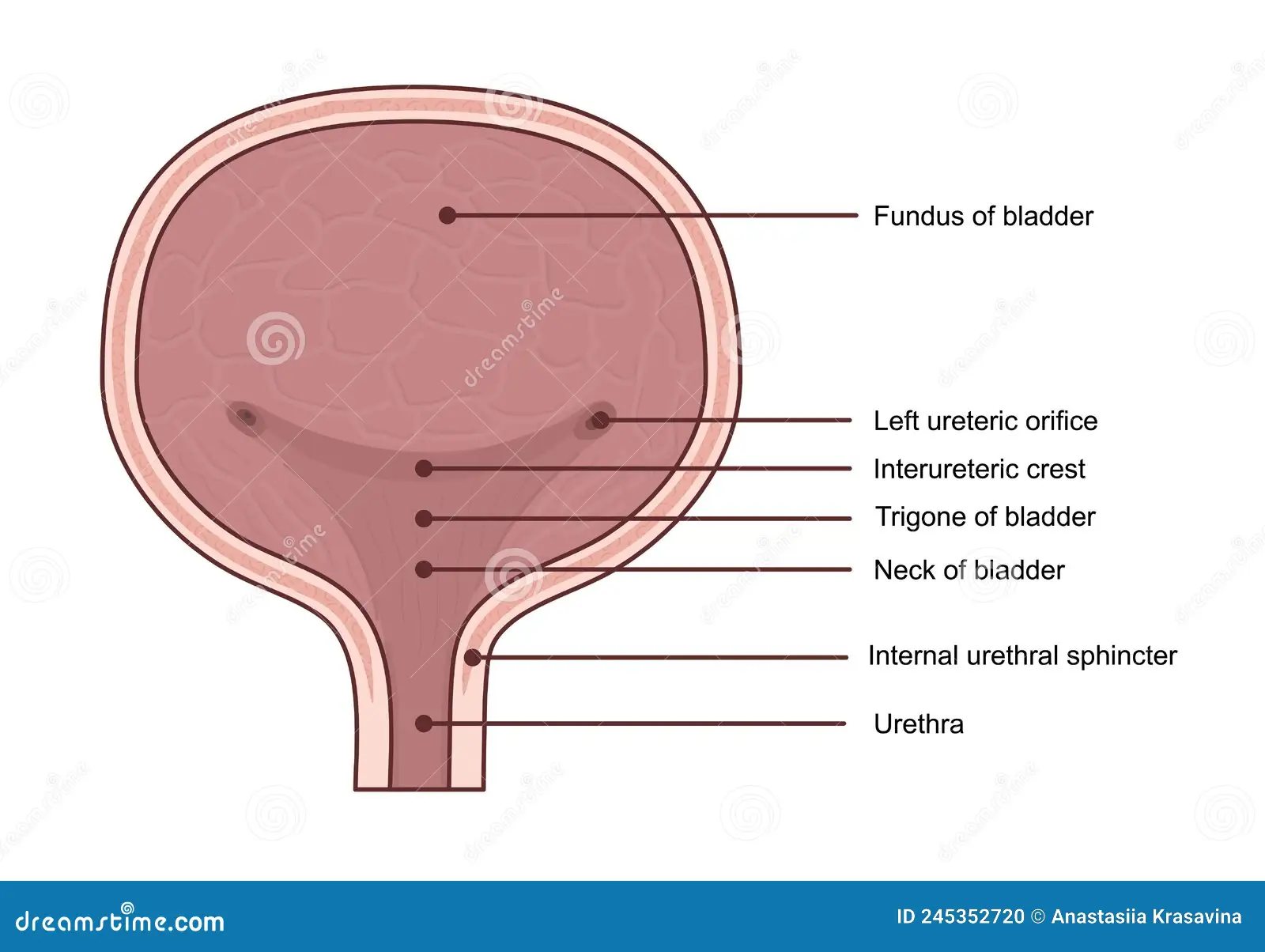
27. Which structure does NOT form part of the boundary
defining the trigone of the bladder?
A. Interuteric crest
B. Left Ureteric Orifice
C. Right Ureteric Orifice
D. Urachus
E. Urethral Orifice
D. Urachus
trigone of the bladder is a triangular area on the internal surface of the bladder formed by three key structures:
The left ureteric orifice (superior corner)
The right ureteric orifice (superior corner)
The urethral orifice (inferior corner)
interureteric crest is a ridge connecting the two ureteric orifices, forming the upper boundary of the trigone.
The urachus is a fibrous remnant of the allantois (an embryonic structure) that extends from the bladder's apex to the umbilicus, and it is not part of the trigone.
28. Which structure is found in males?
A. anterior recess of ischioanal fossa
B. genital hiatus
C. ischiocavernosus muscle
D. rectovesical pouch
E. sphincter urethrae muscle
D. rectovesical pouch
found only in males
located between the rectum and the bladder
forms as a result of the peritoneum draping over these organs
anterior recess of the ischioanal fossa and ischiocavernosus muscle are present in both sexes
genital hiatus and sphincter urethrae muscle are also present in both males and females, associated with the pelvic floor and urogenital diaphragm
29. Which structure is outlined with contrast on a CT using
intraperitonoal contrast material?
A. Ovary
B. Prestate
C. Rectum
D. Seminal Vesicles
E Vagina
A. Ovary
The ovary is entirely covered by a layer of peritoneum called the mesovarium.
On a CT scan with intraperitoneal contrast, structures within the peritoneal cavity become highlighted.
prostate, rectum, seminal vesicles, and vagina are all extraperitoneal or subperitoneal, meaning they lie outside or below the peritoneal cavity. As a result, they do not directly come into contact with the intraperitoneal contrast and are not outlined
30. The prostate is often imaged using an ultrasound transducer place in which location ?
A. Penis
B. Perineum
C. Rectum
D. Urethra
E Urinary Bladder
C. Rectum
ultrasound probe is inserted into the rectum, which lies directly posterior to the prostate, providing clear, close imaging
Imaging via the penis or urethra is not standard or practical.
The perineum is external and doesn’t provide as clear an image as transrectal ultrasound.
The urinary bladder is superior to the prostate, but imaging through the bladder is less common for detailed prostate exams.
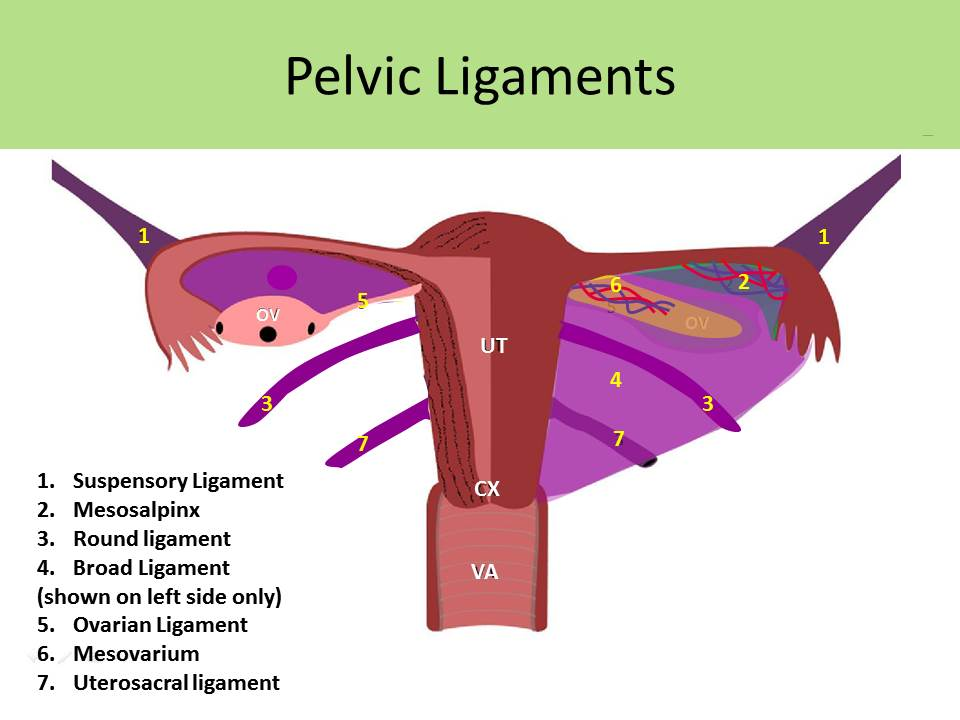
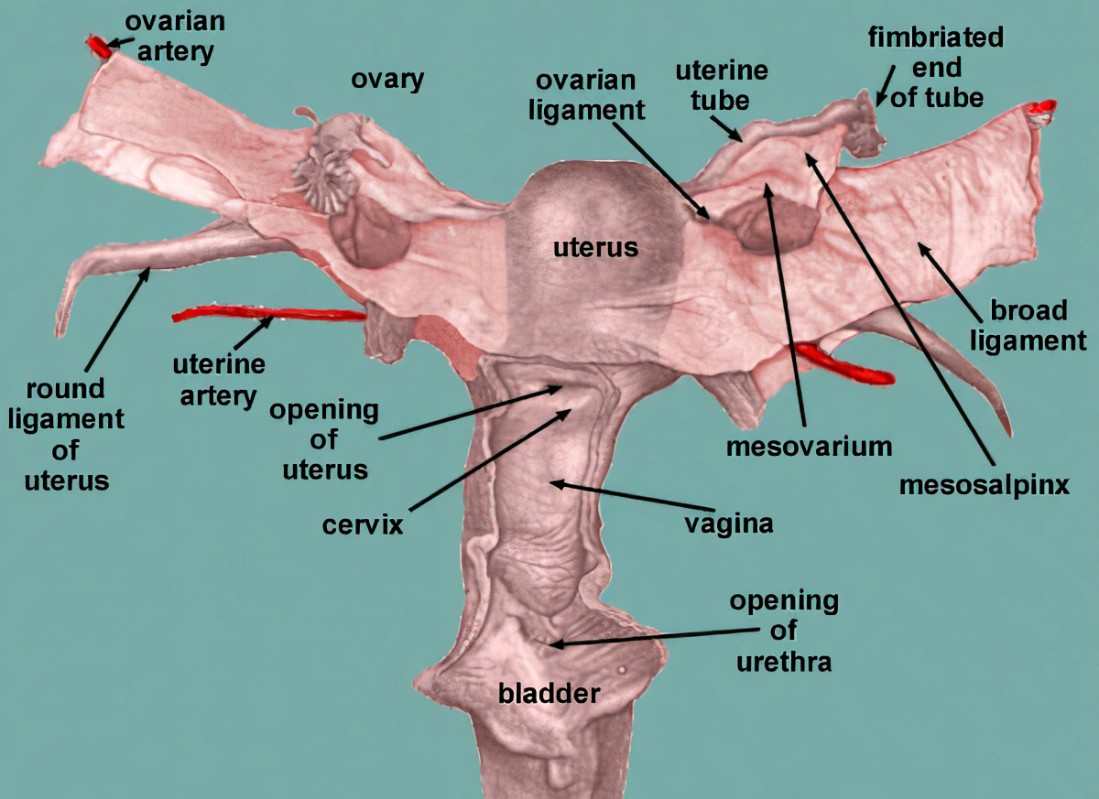
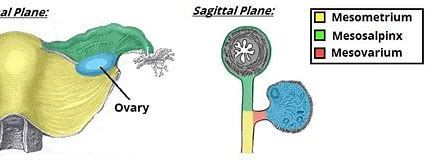
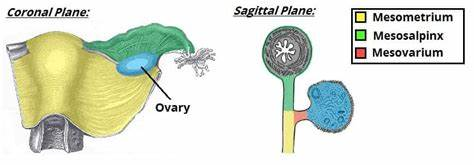
31. Which of the following is considered a part of the broad ligament?
A. Mesovarium
B. Ovarian ligament
C. Round ligament of the uterus
D. Suspensory Ligament of the ovary
E Uterosacral ligament
A. Mesovarium
broad ligament is a wide fold of peritoneum that supports the uterus, fallopian tubes, and ovaries. It has three parts:
Mesometrium: largest part, adjacent to the uterus
Mesosalpinx: surrounding the fallopian tubes
Mesovarium: a small part that attaches the ovary to the broad ligament and contains the ovarian vessels
32. Which of the following does not conduct spermatozoa?
A Ampulla of the ductus deferens
B. Duct of the seminal vesicle
C. Epididymis
D. Prostatic Urethra
B. Duct of the seminal vesicle
it transports seminal fluid that mixes with sperm in the ejaculatory duct but does not contain spermatozoa itself
ductus deferens (ampulla) carries sperm from the epididymis toward the ejaculatory duct.
The epididymis stores and conducts sperm from the testes.
The prostatic urethra carries sperm during ejaculation
33. During the course of surgery for benign prostatic hypertrophy (benign enlargement of the prostate tissue which occludes the prostatic urethra) an electrical cutting device is inserted into the penile, then prostatic urethra, to remove the hypertrophic tissue. The posterior wall of the prostatic urethra is by necessity removed as well.
Which part of the male seminal tract may also be partially removed?
A. duct of seminal vesicle
B. ductus deferens
C. ejaculatory duct
D. fossa navicularis
E. seminiferous tubule
C. ejaculatory duct
ejaculatory ducts open into the posterior wall of the prostatic urethra at the seminal colliculus
During surgery to remove hypertrophic prostate tissue affecting the prostatic urethra, the posterior wall may be partially removed, potentially damaging the ejaculatory ducts.
duct of seminal vesicle joins the ductus deferens to form the ejaculatory duct but does not open directly into the urethra.
The ductus deferens leads to the ejaculatory duct but does not open into the urethra itself.
The fossa navicularis is part of the penile urethra, distal from the prostate.
The seminiferous tubules are inside the testes and unrelated to this surgery.
34. The most inferior extent of the peritoneal cavity in the
female is the:
A. Pararectal fossa
B. Paravesical fossa
C. Rectouterine pouch
D. Rectovesical pouch
E. Vesicouterine pouch
C. Rectouterine pouch
is the space between the uterus and the rectum
rectovesical pouch is found in males (between rectum and bladder).
The vesicouterine pouch lies between the bladder and uterus but is higher than the rectouterine pouch.
Pararectal and paravesical fossae are lateral extensions of the peritoneal cavity, but not the lowest point.
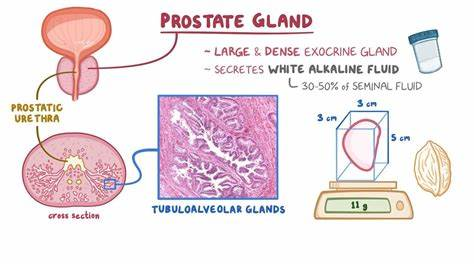
35. The prostate gland:
A. Contains upper, middle and lower lobes
B. Encircles the urethra
C. Is well imaged radiologically using an intravenous urogram
D. Is extraperitoneal
E. B and D
E. B and D
prostate gland
-Encircles the urethra
- Is extraperitoneal
does not have distinct upper, middle, and lower lobes anatomically described that way (A is false).
The prostate is not well visualized by intravenous urogram (IVU), which mainly images the urinary tract (kidneys, ureters, bladder) via contrast in urine (C is false).
36. A 64-year-old woman was diagnosed as having carcinoma of the distal gastrointestinal tract. At surgery, lymph nodes from the sacral, internal iliac and inguinal lymph node groups were removed and sent to pathology for study. Only the superificial inguinal nodes contained cancerous cells. In which part of the GI tract was the tumor localized?
A. cutaneous portion of anal canal
B. distal rectum
C. mucosal line of anal canal
D. pectinate line of anal canal
E. proximal rectum
A. cutaneous portion of anal canal
lymphatic drainage of the anal canal differs based on the location relative to the pectinate (dentate) line:
Below the pectinate line (cutaneous portion of anal canal): drains to the superficial inguinal lymph nodes.
Above the pectinate line (mucosal portion and proximal rectum): drains mainly to internal iliac and sacral lymph nodes.
only the superficial inguinal nodes contained cancer, the tumor is most likely in the cutaneous portion (below the pectinate line) of the anal canal.
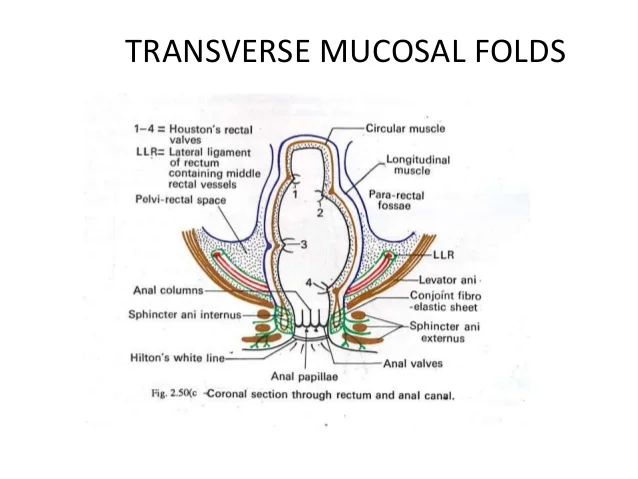
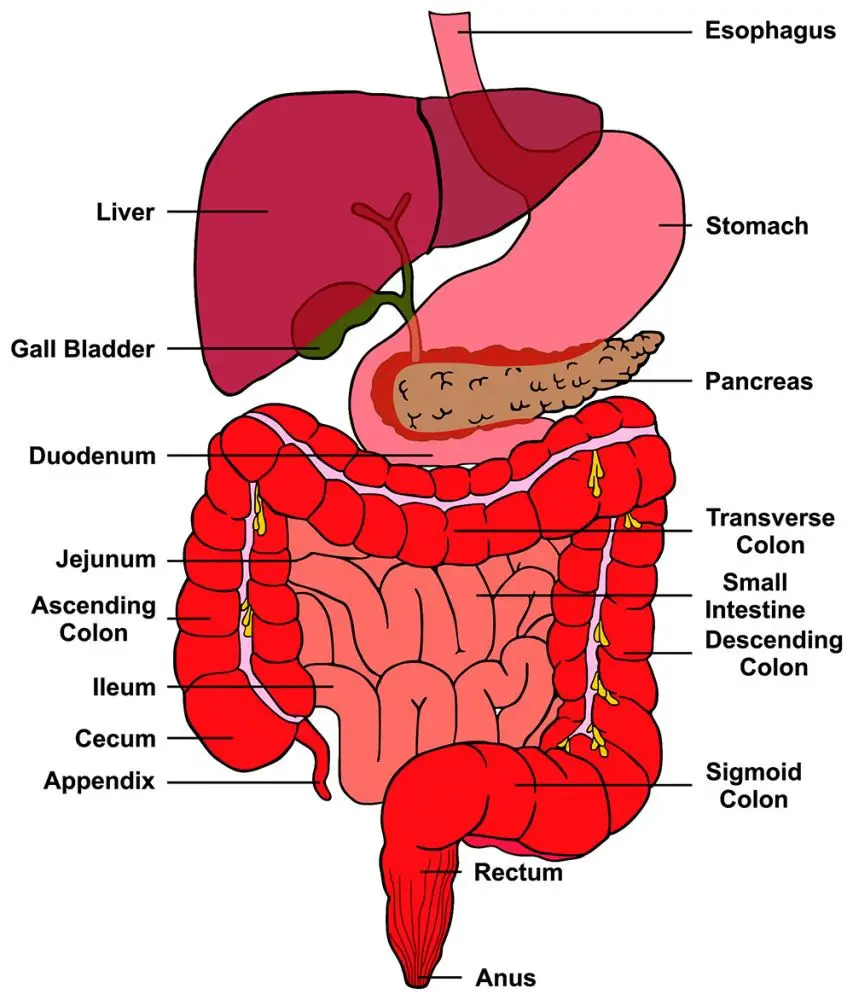
37. Structures within the lower gastrointestinal tract
specialized for physical support of fecal material are the:
A. Transverse rectal folds
B. Circular folds
C. Anal valves
D. Anal columns
A. Transverse rectal folds
specialized folds of the rectal wall that help support and retain fecal material, preventing its premature movement toward the anal canal
Circular folds (plicae circulares) are found in the small intestine, not the lower GI tract.
Anal valves are small crescent-shaped folds at the lower end of anal columns and help with sealing the anal canal but don’t support fecal matter.
Anal columns are vertical folds in the upper anal canal containing blood vessels but are not primarily for supporting feces
38. A malignant tumor in the cutaneous zone of the anal canal would most likely metastasize (spread) to which group of lymph nodes?
A. Inferior mesenteric
B. Pararectal
C. Sacral
D. Superficial inguinal
D. Superficial inguinal
cutaneous zone of the anal canal (below the pectinate line) drains lymph primarily to the superficial inguinal lymph nodes.
The inferior mesenteric nodes drain the proximal colon and upper rectum.
The pararectal nodes drain the rectum and upper anal canal (above the pectinate line).
The sacral nodes drain deeper pelvic structures but are not the primary drainage for the cutaneous anal region
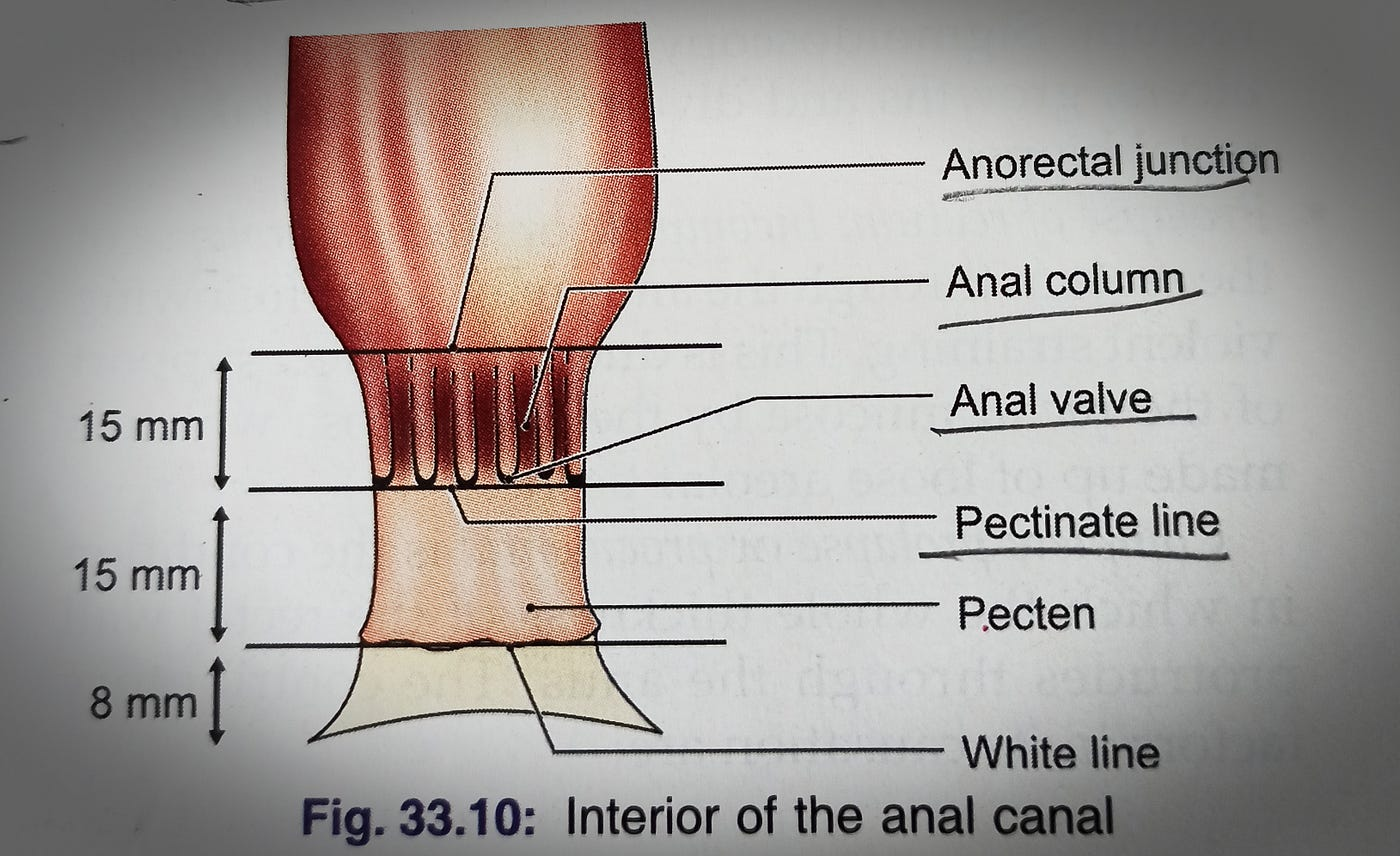
39. Which of these features of the anal canal serves to
indicate the point where the mucosal covering of the
gastrointestinal tract ends and a skin-like covering begins?
A. Mucosal zone
B. White line
C. Transitional zone
D. Pectinate line
D. Pectinate line
pectinate line divides the upper part of the anal canal (lined by columnar mucosa) from the lower part (lined by stratified squamous epithelium, like skin).
40. During a vasectomy, the ductus deferens is ligated in the superior part of the scrotum. Two months following this sterilization procedure, the subsequent ejaculate contains:
A. Prostatic fluid only
B. Seminal fluid and prostatic fluid
C. Sperm only
D. Sperm and seminal fluid
E Sperm, seminal fluid, and prostatic fluid
B. Seminal fluid and prostatic fluid
During a vasectomy, the ductus deferens is cut and ligated, blocking the transport of sperm from the testes/epididymis to the urethra.
Sperm production continues but cannot enter the ejaculate because the pathway is interrupted.
Seminal fluid (from the seminal vesicles) and prostatic fluid (from the prostate gland) still contribute to the volume of ejaculate
ejaculate contains seminal fluid and prostatic fluid, but no sperm
41. An elderly male patient presents with dysuria and urgency. You suspect benign prostatic hypertrophy which has caused an enlargement of the:
A. interureteric crest
B. prostatic utricle
C. seminal colliulus
D. sphincter urethrae
E. uvula
E. uvula
hypertrophied median lobe protruding into the bladder neck
dysuria- painful or difficult micturition
benign prostatic hypertrophy (BPH), the median lobe of the prostate enlarges and can push into the prostatic urethra, forming a prominent fold called the uvula of the bladder. This can cause urinary symptoms like dysuria and urgency due to obstruction.
The interureteric crest is a ridge between the ureteric orifices in the bladder, unrelated to BPH.
The prostatic utricle is a small midline pouch in the prostatic urethra but doesn’t enlarge in BPH.
The seminal colliculus is an elevation in the prostatic urethra but not the site of hypertrophy.
The sphincter urethrae is a muscle controlling urine flow but not involved in hypertrophy
42. During a hysterectomy and an oophorectomy, the uterine and ovarian vessels must be ligated. These vessels can be found in which ligaments?
A. Broad and ovarian
B. Broad and suspensory
C. Round and ovarian
D. Round and suspensory
E. Suspensory and ovarian
B. Broad and suspensory
uterine vessels run within the broad ligament (specifically the mesometrium).
The ovarian vessels travel within the suspensory ligament of the ovary (also called the infundibulopelvic ligament)
ovarian ligament connects ovary to uterus but does not contain major vessels.
The round ligament has no major vessels related to these structures.
43. An elderly patient is having difficulty in voiding (urinating). He complains that after voiding, he still feels as though he needs "to go" again. You suspect that this patient suffers from benign prostatic hypertrophy, which has caused enlargement of the ___________of the bladder.
A. seminal colliculus
B. interureteric crest
C. ampulla
D. trigone
E. uvula
E. uvula
benign prostatic hypertrophy (BPH), the median lobe of the prostate enlarges and protrudes into the neck of the bladder
forming a prominent swelling called the uvula of the bladder
can obstruct urine flow
seminal colliculus is a structure in the prostatic urethra, not part of the bladder.
interureteric crest is a ridge between ureteric openings in the bladder but not related to BPH.
The ampulla is part of the ductus deferens.
The trigone is a smooth triangular area in the bladder but is not typically enlarged in BPH.
44. The prostate gland:
A. encircles the urethra
B. is well imaged using an intravenous urogram
C. is partially intraperitoneal
D. contains upper, middle and lower lobes
A. encircles the urethra
prostate gland surrounds the prostatic urethra
is extraperitoneal
prostate is not well visualized by intravenous urogram (IVU), which images the urinary tract via contrast excreted in urine
traditional anatomical description of the prostate divides it into zones (peripheral, central, transitional), not into upper, middle, and lower lobes
45. The part of the broad ligament giving attachment and support to the uterine tube is the:
A. mesometrium
B. mesovarium
C. mesosalpinx
D. round ligament
C. mesosalpinx
The mesosalpinx is the part of broad ligament that supports the uterine tube
mesometrium supports the uterus itself.
mesovarium attaches to the ovary, carrying vessels and nerves
round ligament is a separate ligament that helps maintain uterine position but does not support the uterine tube
46. Which structure is NOT found within the true pelvis?
A. Femoral nerve
B. Hypogastric nerve
C. Internal pudendal artery
D. Obturator artery
E. Pelvic splanchnic nerves
A. Femoral nerve
true pelvis: area beneath the pelvic brim (pelvic inlet), where the pelvic viscera are located.
hypogastric nerve, internal pudendal artery, obturator artery, and pelvic splanchnic nerves are all structures found within the true pelvis.
false pelvis: area above the pelvic brim, bounded by the iliac blades
femoral nerve is located in the false (greater) pelvis
mainly supplies the anterior thigh. It does not enter the true pelvis
47. Which skeletal feature would you consider to be most characteristic of the female pelvis?
A. Subpubic angle of 90 degrees or greater
B. Marked anterior curvature of the sacrum
C. Tendency to vertical orientation of the iliac bones
D. Prominent medial projection of the ischial spines
A. Subpubic angle of 90 degrees or greater
wider subpubic angle (≥ 90 degrees), which facilitates childbirth
female sacrum is generally less curved (flatter) than the male's, not more curved (so B is incorrect).
Female iliac bones tend to be flared laterally rather than vertical (C is incorrect).
The ischial spines are less prominent medially in females to provide a larger pelvic outlet (D is incorrect).
48. A female patient is found to have an ectopic (tubal pregnancy. In order to gain access to the peritoneal cavity endoscopically to remove the tubal embryo, the instrument can be passed through the posterior fornix of the vagina piercing into the:
A. external os
B. internal os
C. rectouterine pouch
D. rectovesical pouch
E. vesicouterine pouch
C. rectouterine pouch
posterior fornix of the vagina lies directly adjacent to the rectouterine pouch (also called the pouch of Douglas), which is the lowest part of the peritoneal cavity in females
external os and internal os are parts of the cervical canal, not related to accessing the peritoneal cavity.
The rectovesical pouch is found only in males between the rectum and bladder.
The vesicouterine pouch lies between the bladder and uterus, anterior to the uterus, not adjacent to the posterior fornix
49. The male pelvis tends to differ from the female pelvis in that the male pelvis often has a:
A. larger pelvic inlet
B. smaller subpubic angle
C. straighter sacral curvature
D. larger pelvic outlet
E. rounder pelvic inlet
B. smaller subpubic angle
smaller subpubic angle (usually less than 90 degrees), whereas the female pelvis has a wider angle (≥ 90 degrees) to facilitate childbirth
pelvic inlet in males is generally narrower and less spacious than in females (so A is incorrect).
more curved (not straighter) sacrum (so C is incorrect).
smaller pelvic outlet compared to females (so D is incorrect).
heart-shaped pelvic inlet rather than round (so E is incorrect)
50. The rectouterine pouch is the lowest extent of the female peritoneal cavity. At its lowest, it provide a coat of peritoneum to a portion of the:
A. urinary bladder
B. urethra
C. uterine cervix
D. vagina
D. vagina
At its deepest point, the peritoneum reflects onto the posterior vaginal wall, providing a peritoneal covering to part of the vagina
urinary bladder and urethra are anterior and covered by the vesicouterine pouch, not the rectouterine pouch.
The uterine cervix is covered by peritoneum but the deepest reflection of the rectouterine pouch is onto the vagina, especially the posterior fornix.
51. In a CT scan of the pelvis, the uterus is located:
A posterior to the bladder and rectum
B. posterior to the bladder and anterior to the rectum
C anterior to the bladder and rectum
D. anterior D the bladder and posterior to the rectum
B. posterior to the bladder and anterior to the rectum
Anatomically, the uterus is positioned in the pelvis between the urinary bladder and the rectum:
It lies posterior (behind) to the bladder.
It lies anterior (in front) to the rectum
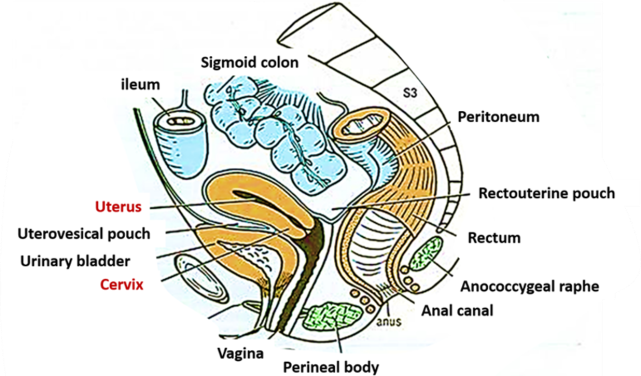
52. Which statement is true regarding pelvic veins?
A The external iliac vein lies medial to the external iliac artery
B. The external iliac veins join to form the inferior vena cava
C The inferior vena cava cannot be imaged
D. Pelvic veins are usually imaged using an arteriogram
A The external iliac vein lies medial to the external iliac artery
-external iliac veins join the internal iliac veins to form the common iliac veins, which then merge into the inferior vena cava (B false)
-inferior vena cava can be imaged by CT, ultrasound, and other methods (so C is incorrect)
-Pelvic veins are typically imaged by venography, not arteriograms (D is incorrect).
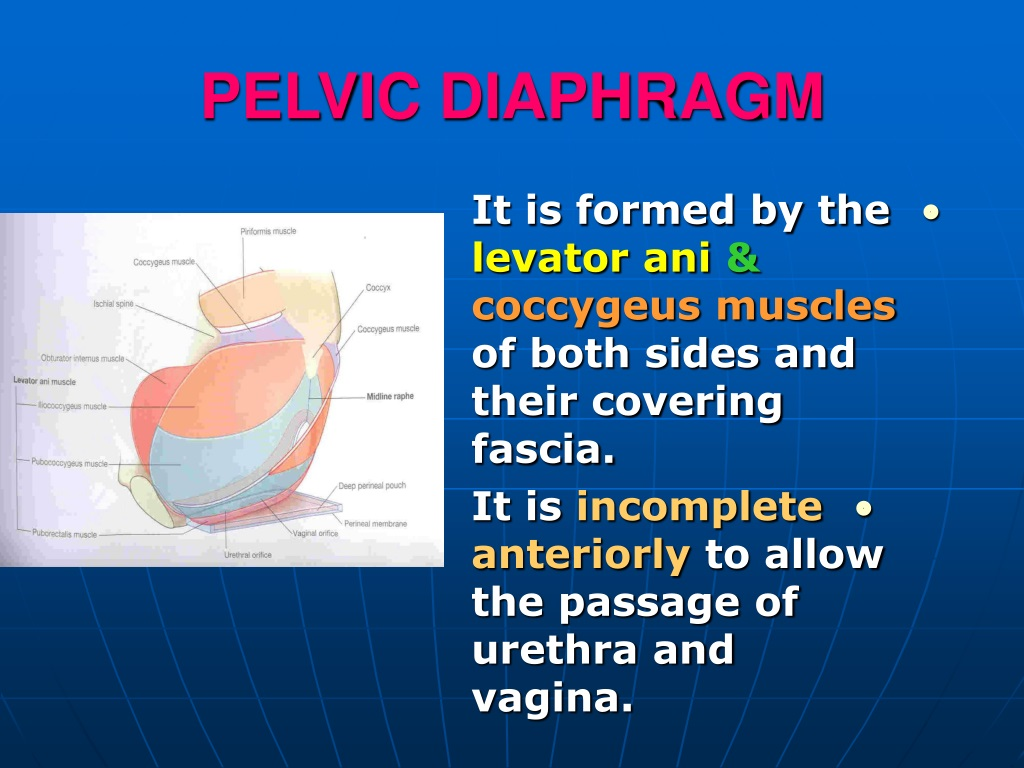
53. Which statement about the pelvic floor is NOT correct?
A. Along with the pelvic brim, it defines the true pelvic cavity
B. It is a funnel-shaped skeletal muscle
C. It is referred to as the pelvic diaphragm
D. It is tensed during defecation
E. It projects into the anal triangle
D. It is tensed during defecation
The pelvic floor is not tensed during defecation--it is relaxed so that feces can be released from the rectum
pelvic floor (or pelvic diaphragm) is a funnel-shaped sheet of skeletal muscles that supports pelvic organs (B and C are correct)
forms the inferior boundary of the true pelvic cavity, together with the pelvic brim defining the true pelvis (A is correct)
projects into the anal triangle of the perineum (E is correct)
54. Preganglionic parasympathetic nerve fibers within the pelvic (inferior hypogastric) plexus arise from S2, 3, 4 and enter the plexus via:
A. gray rami communicantes
B. hypogastric nerves
C. pelvic splanchnic nerves
D. sacral splanchnic nerves
E. white rami communicantes
C. pelvic splanchnic nerves
Preganglionic parasympathetic fibers to the pelvic organs arise from the S2, S3, and S4 spinal cord segments and enter the pelvic (inferior hypogastric) plexus via the pelvic splanchnic nerves
Gray rami communicantes carry postganglionic sympathetic fibers to spinal nerves (A is incorrect).
Hypogastric nerves carry mainly sympathetic fibers, not parasympathetic (B is incorrect).
Sacral splanchnic nerves are sympathetic fibers from the sacral sympathetic trunk (D is incorrect).
White rami communicantes carry preganglionic sympathetic fibers from spinal nerves to sympathetic trunk, not parasympathetic (E is incorrect)
55. A caudal epidural block is a form of regional anaesthetic used in childbirth. Within the sacral canal, the anesthetic agent bathes the sacral spinal nerve roots which would anesthetize all of the following nerves except:
A. Pelvic splanchnics
B. Pudendal
C. S2 dorsal root
D. Sacral splanchnics
E. S2 ventral primary ramus
D. Sacral splanchnics
caudal epidural block anesthetizes the sacral spinal nerve roots (both dorsal and ventral roots) within the sacral canal, so it affects:
Pelvic splanchnic nerves (parasympathetic fibers from S2–S4 ventral roots)
Pudendal nerve (somatic nerve from S2–S4 ventral roots)
S2 dorsal root (sensory input)
S2 ventral primary ramus (motor and autonomic fibers)
Sacral splanchnic nerves are sympathetic fibers that arise from the sacral part of the sympathetic trunk, not from the spinal nerve roots themselves, so they are not directly anesthetized by a caudal epidural block.
56. After giving birth, a patient complains of dribbling of urine while coughing, sneezing, or laughing. Which muscle was most likely damaged during the vaginal delivery?
A. Coccygeus
B. Levator ani
C. Obturator internus
D. Piriformis
E. Transverse perineal
B. Levator ani
levator ani muscle is a major part of the pelvic floor and plays a crucial role in supporting the pelvic organs and maintaining continence
coccygeus muscle also supports the pelvic floor but is less involved in continence.
The obturator internus and piriformis are lateral rotators of the hip, not directly related to urinary continence.
The transverse perineal muscle supports the perineal body but is less significant for urinary control compared to the levator ani
57. In a patient with rectal cancer located in the wall of the ampulla, you find that the cancer has spread to the muscle immediately lateral to the ampulla. This muscle is the:
A. Piriformis
B. Obturator internus
C. Levator ani
D. Sphincter urethrae
E. Bulbospongeosis
C. Levator ani
levator ani muscle forms the main part of the pelvic floor and lies immediately lateral and inferior to the rectal ampulla
supports the rectum and surrounds the anal canal
58. The arcus tendineus levator ani is a thickening of fascia of the:
A. Coccygeus
B. Obturator externus
C. Obturator internus
D. Piriformis
C. Obturator internus
serves as the origin for part of the levator ani muscle, providing important attachment for this key pelvic floor muscle.
It is not related to the coccygeus, obturator externus, or piriformis muscles.
The obturator internus lines the lateral walls of the pelvis and its fascia forms this tendinous arch.
59. The sacral outflow of the parasympathetic (craniosacral) system enters the pelvic plexus via:
A. Hypogastric nerves
B. Pelvic splanchnic nerves
C. Pudendal nerves
D. Sacral splanchnic nerves
B. Pelvic splanchnic nerves
parasympathetic sacral outflow arises from spinal segments S2, S3, and S4 and reaches the pelvic (inferior hypogastric) plexus via the pelvic splanchnic nerves
Hypogastric nerves carry mostly sympathetic fibers (A is incorrect).
Pudendal nerves are somatic nerves controlling perineal muscles, not autonomic (C is incorrect).
Sacral splanchnic nerves are sympathetic fibers from the sacral sympathetic trunk (D is incorrect)
60. A condensation of fibrous tissue in the female located at the center of the posterior border of the perineal membrane is the:
A. Frenulum
B. Posterior labial commissure
C. Perineal body
D. Anococcygeal ligament
E. Pubovesical ligament
C. Perineal body
perineal body is a fibrous mass of connective tissue located at the center of the posterior border of the perineal membrane in females (and males).
important attachment point for muscles of the pelvic floor and perineum, providing structural support
frenulum is usually a fold of tissue under the tongue or associated with the clitoris/labia, not the perineal membrane.
The posterior labial commissure is where the labia majora meet posteriorly.
The anococcygeal ligament is a fibrous structure between the anus and coccyx.
The pubovesical ligament supports the bladder neck
61. The vestibular bulbs/bulb of the corpus spongiosum are firmly attached to the:
A. Perineal membrane
B. Superior pubic rami
C. Ischiopubic rami
D. Pubic symphysis
E. Ischial tuberosities
A. Perineal membrane
The bulbs of the vestibule/bulb of the corpus spongiosum are pieces of erectile tissue that attach to the perineal membrane.
The perineal membrane is an anatomical term for a fibrous membrane in the perineum
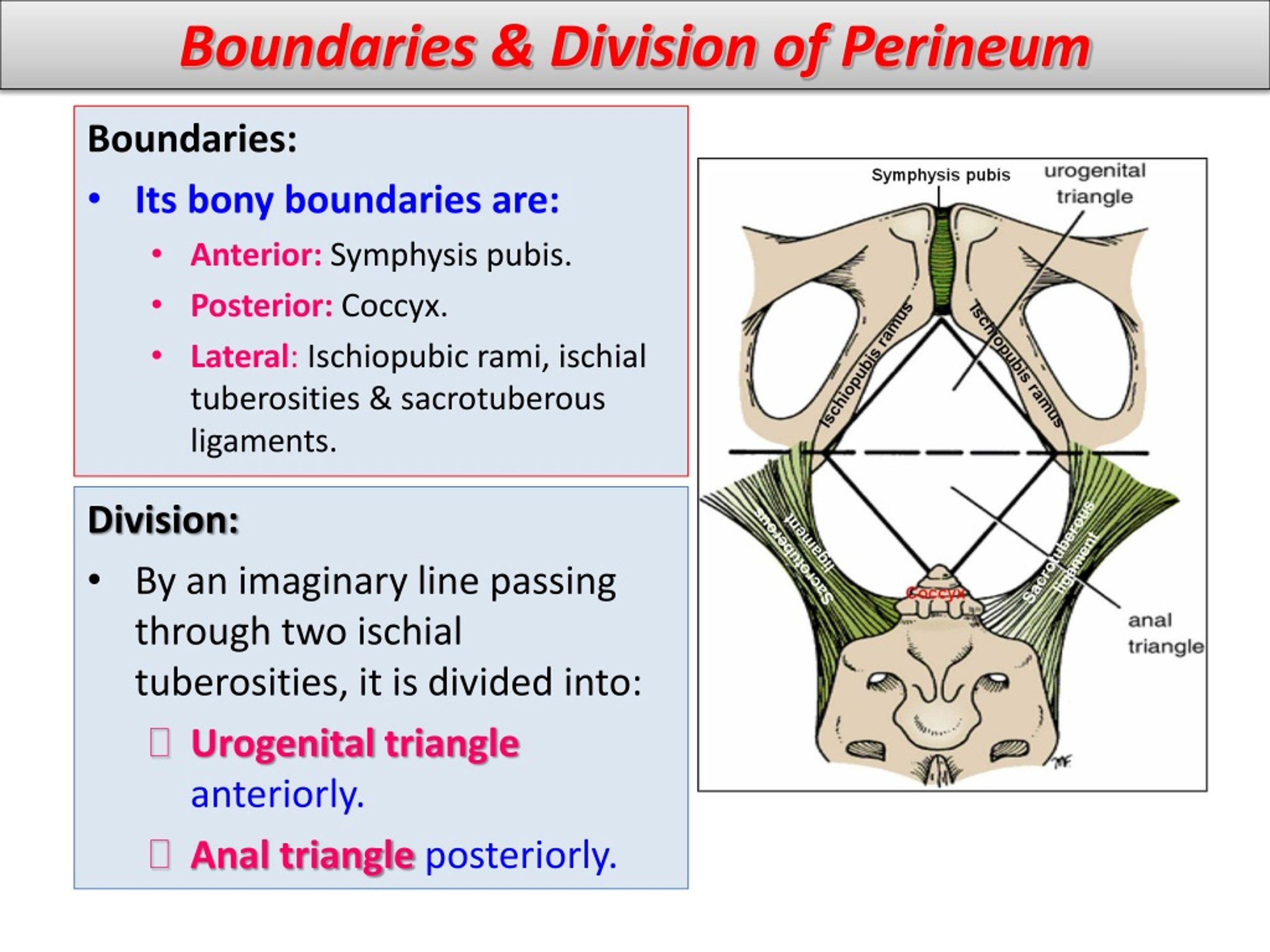
62. The perineum is bounded by all of the following skeletal elements except:
А. соссух
B. ischiopubic ramus
C. spine of ischium
D. symphysis pubis
C. spine of ischium
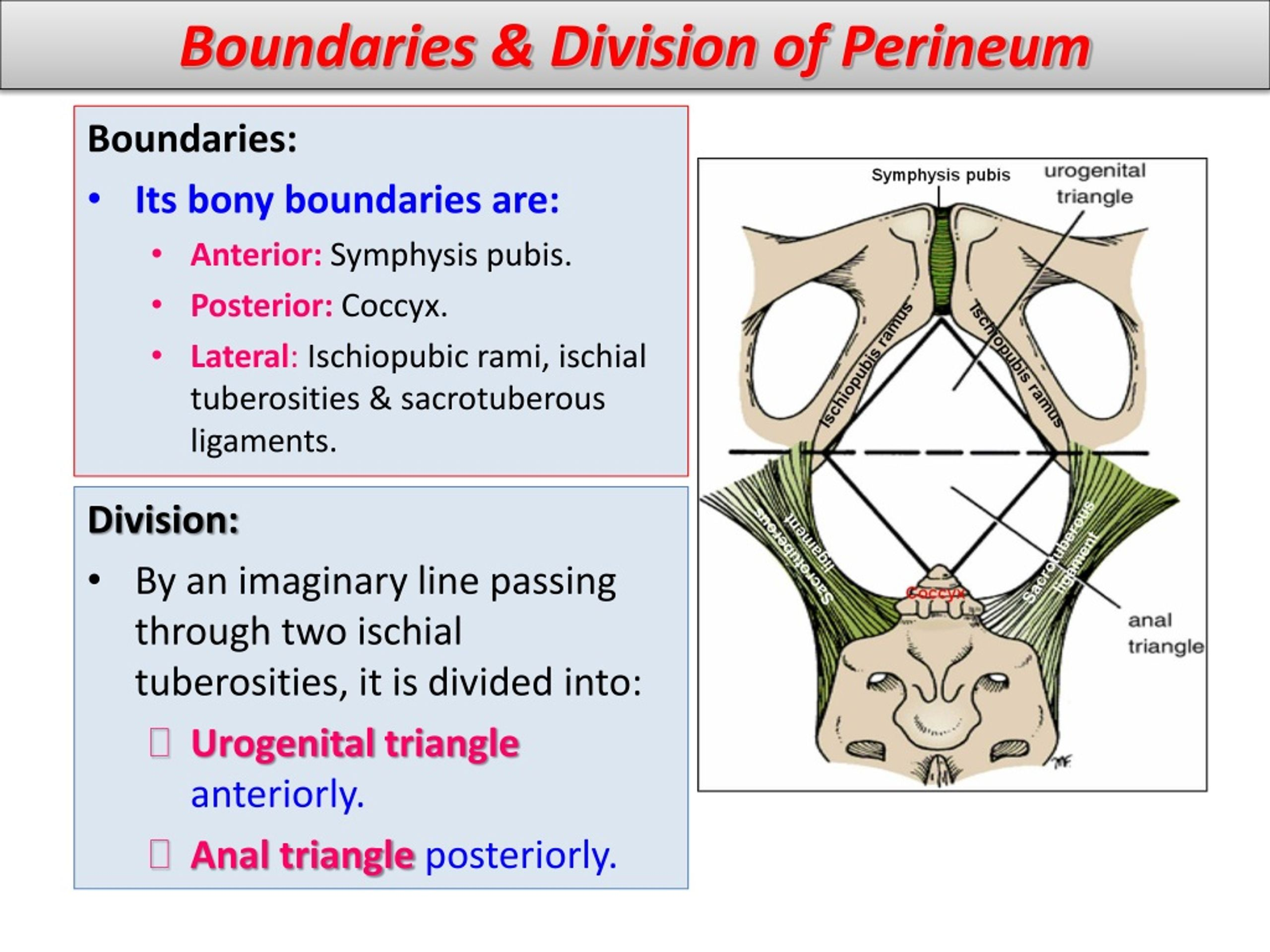
The bounderies of the perineum are !! memorize
Anterior: pubic symphysis;
Anterolateral: ischiopubic rami;
Lateral: ischial tuberosities;
Posterolateral: sacrotuberous ligament;
Posterior: tip of the coccyx
spine of the ischium is not a boundary of the perineum; it lies higher and more laterally on the pelvic bone
63. In order to perform an episiotomy prior to childbirth, the perineum must be anesthetized. By inserting a finger in the vagina and pressing laterally, what palpable bony landmark can be used as the posterior limit of the pudendal canal?
А. Соссух
B. Ischial tuberosity
C. Ischiopubic ramus
D. Obturator groove
E. Ischial spine
E. Ischial spine
pudendal canal (Alcock’s canal) runs along the obturator internus muscle fascia and ends near the ischial spine.
The ischial spine is a key bony landmark used in pudendal nerve blocks and episiotomy anesthesia because it lies close to where the pudendal nerve exits the pelvis
be palpated through the vaginal wall by pressing laterally
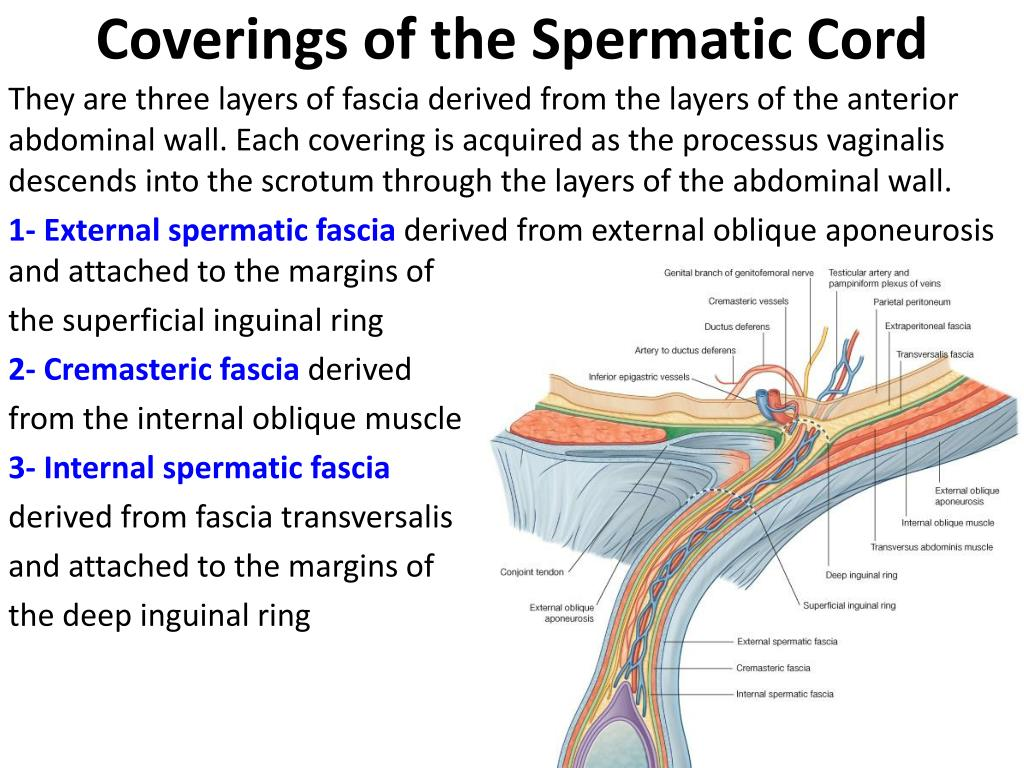
64. The spermatic cord T/F
A. contains lymphatic vessels from the epididymis
B. is surrounded by the tunica vaginalis
C contains lymphatics from the scrotum
D. is surrounded by a fascial process derived from transversus abdominis muscle
E. contains the femoral branch of the genitofemoral nerve
A. contains lymphatic vessels from the epididymis T
B. is surrounded by the tunica vaginalis F
tunica vaginalis surrounds the testis, not the spermatic cord. The cord is enclosed by fascial layers derived from the abdominal wall.
C contains lymphatics from the scrotum F
Lymphatics from the scrotum drain to superficial inguinal lymph nodes, not through the spermatic cord
D. is surrounded by a fascial process derived from transversus abdominis muscle F
transversus abdominis muscle does not contribute to the spermatic cord coverings. The layers come from the internal oblique (cremasteric fascia), external oblique (external spermatic fascia), and transversalis fascia (internal spermatic fascia).
E. contains the femoral branch of the genitofemoral nerve F
spermatic cord contains the genital branch of the genitofemoral nerve, not the femoral branch. The femoral branch supplies the upper thigh
65. The anal canal TF
A. is lined entirely by mucous columnar epithelium
B. is developed entirely from the hind gut
C. has a blood supply from the internal pudendal artery
D. has a sphincter consisting of smooth muscle
E. has lymph vessels which drain to the superficial inguinal lymph nodes
The anal canal
A. is lined entirely by mucous columnar epithelium F
lined by two types of epithelium:
Upper part (above pectinate line): Columnar epithelium (mucous).
Lower part (below pectinate line): Stratified squamous epithelium (skin-like).
B. is developed entirely from the hind gut F
develops from two sources:
Upper part (above pectinate line): Derived from the hindgut (endoderm).
Lower part (below pectinate line): Derived from the proctodeum (ectoderm).
C. has a blood supply from the internal pudendal artery T
D. has a sphincter consisting of smooth muscleT
E. has lymph vessels which drain to the superficial inguinal lymph nodes T
66. The left ureter TF
A. receives its main blood supply from branches directly from the aorta
B. is adherent to the overlying peritoneum
C. is posterior to the uterine artery as they lie lateral to the cervix of the uterus
D. is medial to the obliterated umbilical artery on the lateral wall of the pelvis
E. is lined by pseudostratified columnar epithelium
left ureter:
A. receives its main blood supply from branches directly from the aorta T
B. is adherent to the overlying peritoneum F
ureter is retroperitoneal, meaning it lies behind the peritoneum but is not adherent to it. It is only covered by the peritoneum but can move independently
C. is posterior to the uterine artery as they lie lateral to the cervix of the uterus T
D. is medial to the obliterated umbilical artery on the lateral wall of the pelvis F
ureter is lateral to the obliterated umbilical artery (a fibrous remnant of the fetal umbilical artery) on the lateral pelvic wall
E. is lined by pseudostratified columnar epithelium T
67. Which of the following organs are not extraperitoneal? TF
A. tuba uterina
B. pancreas
C. colon ascendens
D. vesica urinaria (Urinary bladder)
E. prostate
Not extraperitoneal:
A. tuba uterina T
B. pancreas F
retroperitonealretroperitoneal
C. colon ascendens F
retroperitoneal
D. vesica urinaria (Urinary bladder) F
subperitoneal
E. prostate F
subperitoneal
68. The right ovary TF
A. has a blood supply from the abdominal aorta
B. is attached to the anterior (inferior) layer of the broed
ligament
C. has the ovarian ligament attached to its lateral pole
D. is covered by peritoneum in the adult
E. is drained by veins which go to the inferior vena cava.
The right ovary:
A. has a blood supply from the abdominal aorta T
B. is attached to the anterior (inferior) layer of the broad
ligament F
Instead, it is suspended by the mesovarium, which is a posterior extension of the broad ligament
C. has the ovarian ligament attached to its lateral pole F
ovarian ligament attaches to the medial pole of the ovary and connects it to the uterus.
The suspensory ligament of the ovary is attached to the lateral pole and contains the ovarian vessels
D. is covered by peritoneum in the adult F
Instead, it has a special surface layer called germinal epithelium, which is a modified mesothelium
E. is drained by veins which go to the inferior vena cava. T
69. The obturator internus muscle TF
A. leaves the pelvis through the greater sciatic foramen
B. is a medial rotator of the thigh at the hip
C. forms the lateral wall of the ischiorectal fossa
D. is innervated by a nerve from the lumbar plexus
E. has the levator ani muscle attached to its upper border
The obturator internus muscle:
A. leaves the pelvis through the greater sciatic foramen F
obturator internus muscle exits the pelvis through the lesser sciatic foramen, not the greater
B. is a medial rotator of the thigh at the hip F
obturator internus is a lateral rotator of the thigh at the hip
C. forms the lateral wall of the ischiorectal fossa T
D. is innervated by a nerve from the lumbar plexus F
obturator internus is innervated by the nerve to obturator internus, which is a branch of the sacral plexus (L5-S2), not the lumbar plexus
E. has the levator ani muscle attached to its upper border F
levator ani muscle attaches to the tendinous arch of the obturator fascia, which is a thickening of the fascia over the obturator internus, not directly to the muscle itself
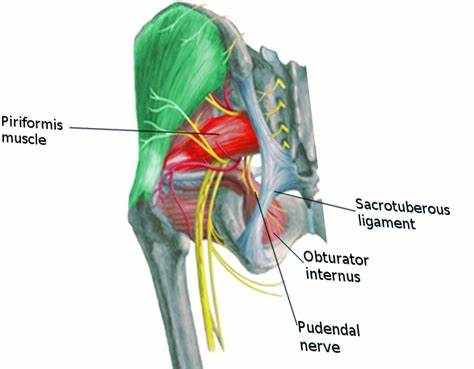
70. Pudendal nerve: TF
A. passes above the piriformis muscle
B. passes through lesser sciatic foramen
C. is a branch of the sacral plexus
D. supplies the medial surface of the thigh
E. innervates the perineum
Pudendal nerve:
A. passes above the piriformis muscle F
pudendal nerve passes below the piriformis muscle, not above. It exits the pelvis through the greater sciatic foramen below the piriformis and re-enters through the lesser sciatic foramen
B. passes through lesser sciatic foramen T
C. is a branch of the sacral plexus T
D. supplies the medial surface of the thigh F
Instead, it supplies the perineum, including the external genitalia, anus, and surrounding areas.
The obturator nerve is responsible for the medial thigh
E. innervates the perineum T
71. The prostate TF
A. develops from the urogenital sinus
B. has no muscle in its structure
C. has a plexus of veins inside its own capsule
D. contains the widest part of the urethra
E. is the homologue of the urethral glands (Skene's tubules) in the female
The prostate:
A. develops from the urogenital sinus T
B. has no muscle in its structure F
prostate contains smooth muscle fibers within its stroma. These muscle fibers play a role in expelling prostatic secretions during ejaculation.
C. has a plexus of veins inside its own capsule F
prostatic venous plexus is not located inside the capsule. Instead, it is found around the capsule of the prostate, forming a dense network that drains into the internal iliac veins.
D. contains the widest part of the urethra T
E. is the homologue of the urethral glands (Skene's tubules) in the female T
72. The cervix of the uterus TF
A. has a canal lined by stratified squamous epithelium
B. undergoes cyclical changes during the menstrual cycle
C. has an acid secretion
D. loses the whole of its lining during menstruation
E. has the same proportion of muscle in its wall as has the body of the uterus
The cervix of the uterus:
A. has a canal lined by stratified squamous epithelium F
cervical canal is lined by simple columnar epithelium, which secretes mucus. The vaginal (external) part of the cervix is lined by stratified squamous non-keratinized epithelium, but this does not line the canal itself.
B. undergoes cyclical changes during the menstrual cycle T
C. has an acid secretion F
cervical canal secretes alkaline mucus, especially during the fertile period of the menstrual cycle. The vagina has an acidic environment due to lactic acid, but the cervix does not
D. loses the whole of its lining during menstruation F
cervix does not shed its lining during menstruation. Only the endometrium of the uterine body is shed. The cervical lining remains intact
E. has the same proportion of muscle in its wall as has the body of the uterus F
cervix has more fibrous tissue and less smooth muscle compared to the uterine body. It is more rigid to maintain support during pregnancy.
73. The ductus (vas) deferens: TF
A. is lateral to the inferior epigastric artery at the deep inguinal ring
B. is medial to the obliterated umbilical artery
C.is lateral to the ureter on the back of the bladder
D. is lateral to the seminal vesicle
E. opens on to the anterior wall of the prostatic urethra
The ductus (vas) deferens:
73. The ductus (vas) deferens:
A. is lateral to the inferior epigastric artery at the deep inguinal ring T
B. is medial to the obliterated umbilical artery T
C.is lateral to the ureter on the back of the bladder F
ductus deferens is actually medial to the ureter on the posterior surface of the bladder, where it crosses over the ureter ("water under the bridge").
D. is lateral to the seminal vesicle F
ductus deferens is medial to the seminal vesicle. It travels downward and medially to join the duct of the seminal vesicle, forming the ejaculatory duct.
E. opens on to the anterior wall of the prostatic urethra F
ductus deferens (through the ejaculatory ducts) opens on the posterior wall of the prostatic urethra, at the level of the seminal colliculus.
74. The trigone of the bladder TF
A. is paler than the rest of the lining of the bladder
B. is developed from endoderm
C. is the least mobile part of the bladder
D. is the least sensitive part of the bladder
E lies between the urachus and the openings of the ureters
The trigone of the bladder:
74. The trigone of the bladder
A. is paler than the rest of the lining of the bladder T
B. is developed from endoderm F
trigone is actually derived from mesoderm, specifically from the incorporation of the mesonephric ducts into the bladder wall during development, unlike the rest of the bladder which develops from endoderm.
C. is the least mobile part of the bladder T
D. is the least sensitive part of the bladder F
trigone is actually more sensitive than other parts of the bladder because it contains many sensory nerve endings, which is why irritation there causes a strong urge to urinate
E lies between the urachus and the openings of the ureters F
trigone lies between the two ureteric orifices and the internal urethral orifice, not between the urachus and the ureteric openings. The urachus is a fibrous remnant of the allantois located superiorly on the bladder dome, away from the trigone
75. The female pelvis differs from the male pelvis in TF
A. having greater transverse diameter
B. having obtuse greater sciatic notch
C. having greater anteroposterior diameter
D. having shallower pelvic cavity
E. having wider subpubic angle
The female pelvis differs from the male pelvis in : all true
A. having greater transverse diameter
B. having obtuse greater sciatic notch
C. having greater anteroposterior diameter
D. having shallower pelvic cavity
E. having wider subpubic angle
76. The urinary bladder TF
A. is developed entirely from ectoderm
B. is lined by transitional epithelium
C. has a parasympathetic nerve supply from the vagus nerve
D. has a sensory nerve supply which is derived from sympathetic and parasympathetic nerves
E. has a base posteriorly which is completely covered by
peritoneum
The urinary bladder
A. is developed entirely from ectoderm F
bladder develops mostly from the endoderm (specifically the urogenital sinus), not ectoderm.
B. is lined by transitional epithelium T
C. has a parasympathetic nerve supply from the vagus nerve F
Parasympathetic innervation to the bladder comes from the pelvic splanchnic nerves (S2-S4), not the vagus nerve, which mainly supplies thoracic and abdominal organs up to the transverse colon
D. has a sensory nerve supply which is derived from sympathetic and parasympathetic nerves T
E. has a base posteriorly which is completely covered by peritoneum F
bladder’s base (or fundus) is only partially covered by peritoneum on its superior surface, not completely. The rest lies against pelvic organs and connective tissue
77. The uterine (Fallopian) tube TF
A. is lined by non-ciliated columnar epithelium
B. is attached at its lateral end to the lateral pole of the ovary
by the ovarian fimbria
C. undergoes cyclical changes during the menstrual cycle
D. is narrower at its lateral than its medial end
E. is developed from the paramesonephric duct
The uterine (Fallopian) tube:
A. is lined by non-ciliated columnar epithelium F
uterine tube is actually lined by both ciliated and non-ciliated columnar epithelial cells. The ciliated cells help move the egg toward the uterus
B. is attached at its lateral end to the lateral pole of the ovary
by the ovarian fimbria T
C. undergoes cyclical changes during the menstrual cycle T
D. is narrower at its lateral than its medial end F
tube is narrower medially (near the uterus) and wider at the lateral end (near the ovary). The widest part is the ampulla, which is closer to the ovary
E. is developed from the paramesonephric duct T
78. The piriformis muscle TF
A. is attached to the greater trochanter
B. emerges from the pelvis through the greater sciatic foramen
C. is a lateral rotator of the thigh at the hip
D. is inferior to the gluteus medius in the buttock
E. has the sciatic nerve emerging inferior to its lower border
The piriformis muscle:
A. is attached to the greater trochanter T
B. emerges from the pelvis through the greater sciatic foramen T
C. is a lateral rotator of the thigh at the hip T
D. is inferior to the gluteus medius in the buttock T
E. has the sciatic nerve emerging inferior to its lower border T
79. The pudendal nerve TF
A. leaves the pelvis through the greater sciatic foramen
B. enters the perineum lateral to the nerve to the obturator internus muscle
C. runs in the roof of the ischiorectal fossa
D. is sensory to the skin of the scrotum
E. innervates the internal sphincter of the rectum
The pudendal nerve:
A. leaves the pelvis through the greater sciatic foramen T
B. enters the perineum lateral to the nerve to the obturator internus muscle F
pudendal nerve enters the perineum medial to the nerve to obturator internus after passing through the lesser sciatic foramen
C. runs in the roof of the ischiorectal fossa F
pudendal nerve runs in the pudendal (Alcock’s) canal, which is on the lateral wall of the ischiorectal fossa, not the roof
D. is sensory to the skin of the scrotum T
E. innervates the internal sphincter of the rectum F
internal anal sphincter is smooth muscle and is innervated by autonomic nerves (mainly sympathetic), not the pudendal nerve, which supplies the external (skeletal) anal sphincter
80. The male urethra TF
A. is lined along its whole length by transitional epithelium
B. is narrowest in its membranous part
C. receives the ducts of the bulbourethral glands in its
membranous part
D. receives the ejaculatory ducts in its prostatic part
E. develops entirely from the urogenital sinus
The male urethra:
A. is lined along its whole length by transitional epithelium F
proximal part (near the bladder and prostatic urethra) is lined by transitional epithelium. The penile urethra is mostly lined by pseudostratified columnar or stratified squamous epithelium
B. is narrowest in its membranous part T
C. receives the ducts of the bulbourethral glands in its membranous part F
bulbourethral glands open into the spongy (penile) urethra, not the membranous part
D. receives the ejaculatory ducts in its prostatic part T
E. develops entirely from the urogenital sinus F
male urethra develops from the urogenital sinus and the ectodermal urethral plate (for the distal penile urethra).
81. The broad ligament TF
A. has the ovary attached to its posterior (superior) surface
B. has the uterine (Fallopian) tube in its upper (anterior) free border
C. has the ovarian artery in its lower attached border
D. has the ovarian ligament forming a ridge on its posterior (superior) surface
E. has the ureter passing forwards in its lower attached border
The broad ligament:
A. has the ovary attached to its posterior (superior) surface T
B. has the uterine (Fallopian) tube in its upper (anterior) free border T
C. has the ovarian artery in its lower attached border F
ovarian artery travels within the suspensory ligament of the ovary, which is continuous with the upper (lateral) free border of the broad ligament, not the lower attached border.
D. has the ovarian ligament forming a ridge on its posterior (superior) surface T
E. has the ureter passing forwards in its lower attached border T
82. The levator ani muscle TF
A. has no attachment to bone inside the pelvis
B. is supplied by nerves from the lumbar plexus
C. has no sphincter action in relation to the rectumor anal canal
D. plays no part in maintaining the position of the uterus
E. consists of smooth muscle
82. The levator ani muscle
A. has no attachment to bone inside the pelvis F
levator ani does attach to pelvic bones, mainly the pubis and the tendinous arch of the obturator internus fascia on the pelvic side wall.
B. is supplied by nerves from the lumbar plexus F
levator ani is mainly innervated by the nerve to levator ani, from the sacral plexus (S3–S4), not the lumbar plexus
C. has no sphincter action in relation to the rectum or anal canal F
levator ani contributes to sphincter function, particularly by supporting and constricting the anal canal (part of the pelvic diaphragm)
D. plays no part in maintaining the position of the uterus F
levator ani supports pelvic organs, including the uterus, helping maintain their position
E. consists of smooth muscle F
levator ani is a skeletal muscle
83. The rectum: TF
A is covered anteriorly by peritoneum along its whole length
B. has no teniae coli
C has appendices epiploicae
D. has a blood supply from the terminal branches of the
superior mesenteric artery
E has permanent transverse folds consisting of mucous
membrane and circular smooth muscle
The rectum:
A. is covered anteriorly by peritoneum along its whole length F
rectum is only partially covered by peritoneum:
Upper third: Anterior and lateral peritoneal covering.
Middle third: Anterior covering only.
Lower third: No peritoneal covering (subperitoneal).
B. has no teniae coli T
C has appendices epiploicae F
does not have appendices epiploicae (small fat-filled pouches), which are a feature of the colon, not the rectum
D. has a blood supply from the terminal branches of the superior mesenteric artery F
rectum is primarily supplied by:
Superior rectal artery (from the inferior mesenteric artery),
Middle rectal artery (from the internal iliac artery),
Inferior rectal artery (from the internal pudendal artery)
E. has permanent transverse folds consisting of mucous membrane and circular smooth muscle T
84. The right ureter TF
A. is posterior to the gonadal (testicular or ovarian) vessels
B. is posterior to the genitofemoral nerve
C. is posterior to the right colic vessels
D. is anterior to the internal iliac artery
E is posterior (inferior) to the ductus (vas) deferens
The right ureter:
A. is posterior to the gonadal (testicular or ovarian) vessels T
B. is posterior to the genitofemoral nerve F
right ureter is actually anterior to the genitofemoral nerve, which runs along the surface of the psoas major muscle
The ureter crosses over the nerve on its way down to the pelvis
C. is posterior to the right colic vessels T
D. is anterior to the internal iliac artery T
E is posterior (inferior) to the ductus (vas) deferens T
85. Which of the following statements are true and false: TF
A. The duodenum receives a blood supply from both the coeliac trunk and the superior mesenteric artery because the duodenum is developed from both the foregut and the midgut.
B. The pelvic compartment of the abdominal cavity is placed in the lesser pelvis
C. The rectouterine pouch (rectouterine excavation or Pouch of Douglas) could be examined through the vagina and rectum
D. The prostate could be examined through rectum
E. The colon is entirely retroperitoneal structure
A. The duodenum receives a blood supply from both the coeliac trunk and the superior mesenteric artery because the duodenum is developed from both the foregut and the midgut. T
B. The pelvic compartment of the abdominal cavity is placed in the lesser pelvis T
C. The rectouterine pouch (rectouterine excavation or Pouch of Douglas) could be examined through the vagina and rectum T
D. The prostate could be examined through rectum T
E. The colon is entirely retroperitoneal structure F
colon is not entirely retroperitoneal. Only the ascending, descending colon, and rectum are retroperitoneal, while the cecum, transverse colon, and sigmoid colon are intraperitoneal
86. Which one of the following relations of the vagina are true TF
A. The anterior wall is in contact with the bladder and urethra
B. The posterior wall is in contact with the rectum
C. The anterior fornix is the deepest of all four fornices
D. The posterior fornix is in front of the Douglas pouch
E. The posterior fornix is frequently injured during instrumental vaginal examination
Which one of the following relations of the vagina are true?
A. The anterior wall is in contact with the bladder and urethra T
B. The posterior wall is in contact with the rectum T
C. The anterior fornix is the deepest of all four fornices F
posterior fornix is the deepest of all the vaginal fornices, not the anterior fornix. This is because it lies directly beneath the rectouterine pouch (Pouch of Douglas)
D. The posterior fornix is in front of the Douglas pouch T
E. The posterior fornix is frequently injured during instrumental vaginal examination T
87. The penis TF
A. has a corpus spongiosum which ends posteriorly in the superficial perineal pouch as the bulb of the penis
B. has corpora cavernosa which end anteriorly as the glans of the penis
C. has skin which is innervated by the lumbar nerves
D. has skin whose lymphatics pass to the paraortic lymph nodes
E. is the homologue of the clitoris in the female.
The penis:
A. has a corpus spongiosum which ends posteriorly in the superficial perineal pouch as the bulb of the penis T
B. has corpora cavernosa which end anteriorly as the glans of the penis F
corpora cavernosa do not form the glans of the penis. Instead, the corpus spongiosum extends to form the glans. The corpora cavernosa terminate in blunt rounded ends
C. has skin which is innervated by the lumbar nerves F
skin of the penis is innervated by the pudendal nerve (S2-S4) and ilioinguinal nerve (L1), which are sacral and lumbar nerves but not exclusively lumbar
D. has skin whose lymphatics pass to the paraortic lymph nodes F
lymphatics of the skin of the penis drain primarily into the superficial inguinal lymph nodes, not the para-aortic lymph nodes. The deep structures of the penis drain to the internal iliac nodes.
E. is the homologue of the clitoris in the female. T
88. The psoas major muscle TF
A. is innervated by the anterior primary rami of the first three lumbar spinal nerves
B. is attached to the lesser trochanter
C. is an extensor of the thigh at the hip
D. is lateral to the femoral nerve
E. in its upper part is posteromedial to the ureter.
The psoas major muscle:
A. is innervated by the anterior primary rami of the first three lumbar spinal nerves T
B. is attached to the lesser trochanter T
C. is an extensor of the thigh at the hip F
psoas major is actually a flexor of the thigh at the hip joint, not an extensor. It helps in hip flexion
D. is lateral to the femoral nerve F
psoas major is medial to the femoral nerve, which runs along its lateral border
E. in its upper part is posteromedial to the ureter. T
89. Which one of the following structures support the uterus? TF
A. cardinal ligament
B. obturator internus muscle
C. levator ani muscle
D. sacrouterine ligament
E. broad ligament
structures support the uterus:
A. cardinal ligament T
cardinal ligament (transverse cervical ligament) provides strong lateral support to the uterus by attaching it to the pelvic wall
B. obturator internus muscle F
obturator internus muscle is a muscle of the lateral pelvic wall and has no direct role in supporting the uterus
C. levator ani muscle T
levator ani muscle (part of the pelvic floor) supports the uterus from below, preventing prolapse
D. sacrouterine ligament T
sacrouterine (uterosacral) ligament extends from the uterus to the sacrum, providing posterior support
E. broad ligament T
broad ligament is a peritoneal fold that provides a limited degree of support to the uterus by stabilizing it laterally
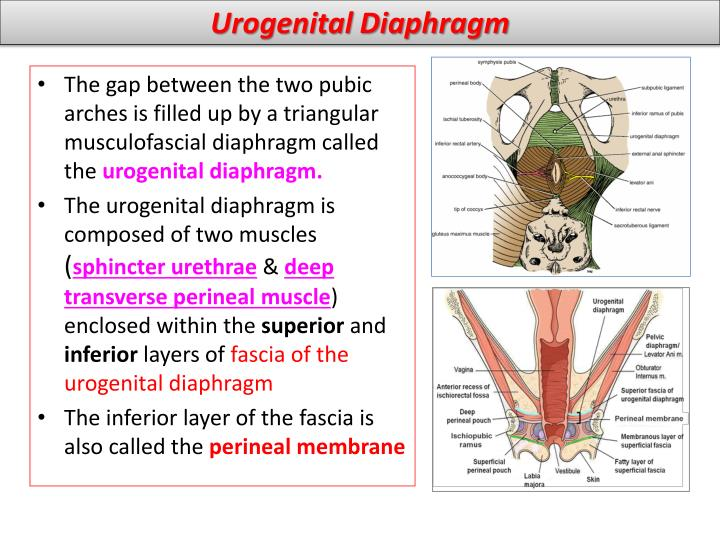
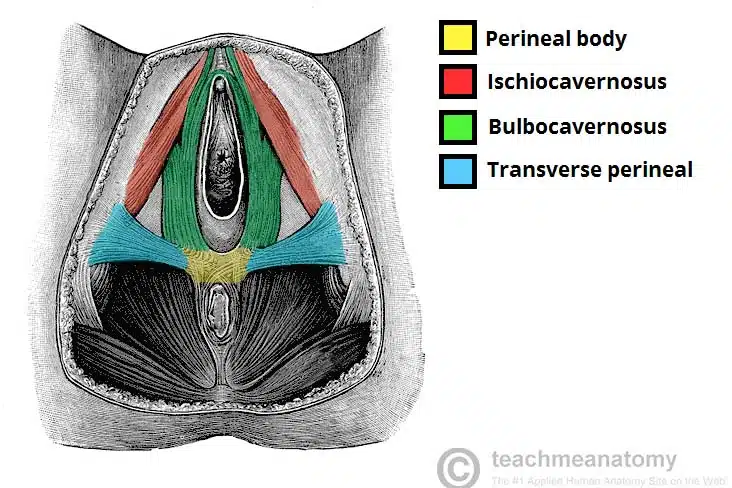
90. The muscles of the urogenital diaphragm are: TF
A. m. levator ani
B. m. sphincter urethrae
C. m. sphincter vesicae
D. m. ischicavernosus
E. m. obturatorius internus
muscles of urogenital diaphragm:
A. m. levator ani F
levator ani is not part of the urogenital diaphragm. It is part of the pelvic diaphragm, forming the major portion of the pelvic floor
B. m. sphincter urethrae T
sphincter urethrae (external urethral sphincter) is a key muscle of the urogenital diaphragm, providing voluntary control of urination.
C. m. sphincter vesicae F
sphincter vesicae (internal urethral sphincter) is a smooth muscle found in the bladder neck, not part of the urogenital diaphragm.
D. m. ischicavernosus T
ischiocavernosus muscle is a superficial muscle of the urogenital region that helps maintain erection by compressing the crus of the penis or clitoris
E. m. obturatorius internus F
obturator internus muscle is part of the lateral pelvic wall, not part of the urogenital diaphragm
91. Which of following statements about the rectum are true or false:
A. It is supplied only by one artery
B. There is a porto-caval anastomosis in its wall
C. Its smooth musculature is innervated by somatic nerves.
D. There is no circular layer in its wall
E. It is entirely covered by peritoneum
ABOUT RECTUM:
A. It is supplied only by one artery F
rectum receives blood from three arteries:
Superior rectal artery (from inferior mesenteric artery)
Middle rectal artery (from internal iliac artery)
Inferior rectal artery (from internal pudendal artery)
B. There is a porto-caval anastomosis in its wall T
C. Its smooth musculature is innervated by somatic nerves. F
smooth muscle of the rectum is innervated by autonomic nerves (sympathetic and parasympathetic), not somatic nerves.
Somatic innervation affects only the external anal sphincter via the pudendal nerve.
D. There is no circular layer in its wall F
the rectum has two layers of smooth muscle: an inner circular and an outer longitudinal layer. The circular layer contributes to the internal anal sphincter
E. It is entirely covered by peritoneum F
rectum is only partially covered by peritoneum:
The upper third is covered anteriorly and laterally
The middle third is covered only anteriorly
The lower third is not covered by peritoneum (it is subperitoneal/extraperitoneal)
92. The peritoneal formations which are found in the peritoneal compartment of pelvis are: TF
A. mesocolon transversum
B. mesenterium
C. broad ligament of uterus
D. lig. pubovesicale
E. mesosalpinx
peritoneal formations which are found in the peritoneal compartment of pelvis:
A. mesocolon transversum F
transverse mesocolon is a peritoneal fold of the abdominal cavity suspending the transverse colon. It is not located in the pelvis.
B. mesenterium F
usually refers to the peritoneal fold attaching the small intestine (jejunum and ileum) to the posterior abdominal wall, not a pelvic structure
C. broad ligament of uterus T
D. lig. pubovesicale F
pubovesical ligament is a fibrous ligament (not peritoneal) that supports the bladder. It is not a peritoneal fold
E. mesosalpinx T
93. The pelvic diaphragm is composed of : TF
A. m. levator ani and m. piriformis
B. m. piriformis and m. obturatorius internus
C. m. levator ani and m. coccygeus
D. m. obturatorius internus and m. coccygeus
E. m. levator ani and m. obturatorius internus
pelvic diaphragm is composed of:
A. m. levator ani and m. piriformis F
piriformis not component
B. m. piriformis and m. obturatorius internus F
obturator internus not component
C. m. levator ani and m. coccygeus T
D. m. obturatorius internus and m. coccygeus F
E. m. levator ani and m. obturatorius internus F
94. The testes TF
A. receive their blood supply from the abdominal aorta
B. has a venous drainage which ends on both sides in the renal veins
C. have a lymphatic drainage to the superficial inguinal lymph nodes
D. are in the scrotum by the fifth month of intrauterine life
E. have an appendix which is a remnant of the mesonephros
Testes:
A. receive their blood supply from the abdominal aorta T
B. has a venous drainage which ends on both sides in the renal veins F
right testicular vein drains into the inferior vena cava, but the left testicular vein drains into the left renal vein. So, venous drainage is asymmetric, not ending on both sides in the renal veins
C. have a lymphatic drainage to the superficial inguinal lymph nodes F
Testicular lymphatics drain primarily to the lumbar (para-aortic) lymph nodes, not superficial inguinal nodes.
The superficial inguinal nodes drain lymph from the scrotum and perineum, not the testes themselves
D. are in the scrotum by the fifth month of intrauterine life F
Testes usually descend into the scrotum by around the 7th to 9th month of fetal development, not as early as the 5th month
E. have an appendix which is a remnant of the mesonephros F
testicular appendix (appendix testis) is a remnant of the Müllerian (paramesonephric) duct, not the mesonephros
95. Which one of the following structures lies in the mesosalpinx? TF
A. ovarium
B. a. vaginalis
C. uterine tube
D. lig. teres uteri (round lig)
E. uterus
lies in the mesosalpinx:
A. ovarium F
ovary is attached to the mesovarium, not the mesosalpinx
B. a. vaginalis F
artery to the vaginalis is not a main structure in the mesosalpinx
C. uterine tube T
D. lig. teres uteri ( round lig ) F
round ligament passes through the broad ligament but is not within the mesosalpinx
E. uterus F
uterus is supported by the broad ligament but is not within the mesosalpinx
96. The perineum is bounded by : TF
A. os coccygis
B. ramus inferior ossis pubis
C. spina ischiadica
D. tuber ischiadicum
E. lig. sacrospinale
The perineum is bounded by:
A. os coccygis T
B. ramus inferior ossis pubis T
C. spina ischiadica F
ischial spine is not a boundary of the perineum; it lies more superiorly in the pelvis.
D. tuber ischiadicum T
E. lig. sacrospinale F
ligament is internal and not considered a boundary of the perineum.
97. Which one of the following statements about uterus are true or false:
A. In adult fertile woman the position of uterus is anteversion-anteflexion
B. Fundus of uterus is the part close to the vagina
C. Cardinal ligaments provide support to the uterus
D. Broad ligament is a double-layered fold of peritoneum
which extends from both sides of the uterus
E. The main blood supply is by uterine arteries
true or false about uterus
A. In adult fertile woman the position of uterus is anteversion-anteflexion T
This is the typical position: the uterus is anteverted (tilted forward over the bladder) and anteflexed (bent forward at the body relative to the cervix).
B. Fundus of uterus is the part close to the vagina F
fundus is the top rounded part of the uterus, farthest from the vagina. The part close to the vagina is the cervix
C. Cardinal ligaments provide support to the uterus T
D. Broad ligament is a double-layered fold of peritoneum which extends from both sides of the uterus T
E. The main blood supply is by uterine arteries T
98. The uterus TF
A. derives its entire blood supply from the uterine arteries
B. is posteriorly covered by peritoneum to a greater extent
than anteriorly
C. is kept in position mainly by the round ligaments
D. has in the wall of its body as much fibrous tissue as
muscular tissue
E. has no sympathetic autonomic nerve supply
The uterus:
A. derives its entire blood supply from the uterine arteries F
uterus receives blood mainly from the uterine arteries, but also from ovarian arteries, so not entirely from uterine arteries
B. is posteriorly covered by peritoneum to a greater extent than anteriorly T
C. is kept in position mainly by the round ligaments F
round ligaments help maintain anteversion, but the main support comes from the cardinal and uterosacral ligaments, plus the pelvic floor muscles
D. has in the wall of its body as much fibrous tissue as muscular tissue F
uterine wall (myometrium) is mainly muscle, with much less fibrous tissue
E. has no sympathetic autonomic nerve supply F
uterus has both sympathetic and parasympathetic autonomic innervation, mainly from the hypogastric and pelvic plexuses
99. The deep layer of the urogenital diaphragm in male: TF
A. contains bulbourethral glands
B. transmits the membranous part of the urethra
C. contains mm. ischiocavernosi
D. contains gll. vestibulares majores
E. contains sphincter urethrae externus m.
deep layer of the urogenital diaphragm in male
A. contains bulbourethral glands T
bulbourethral (Cowper’s) glands are located within the deep perineal pouch, which is part of the urogenital diaphragm
B. transmits the membranous part of the urethra T
C. contains mm. ischiocavernosi F
ischiocavernosus muscles are in the superficial perineal pouch, not the deep layer
D. contains gll. vestibulares majores F
greater vestibular glands (Bartholin’s glands) are in the female superficial perineal pouch
E. contains sphincter urethrae externus m. T
100. The pudendal nerve
A. enters the perineum through the lesser sciatic foramen
B. lies on the sacrospinous ligament
C. contains fibres from the third, fourth and fifth sacral spinal
segments
D. is sensory to the skin of the scrotum
E. is sensory to part of the urethra
The pudendal nerve
A. enters the perineum through the lesser sciatic foramen T
B. lies on the sacrospinous ligament T
C. contains fibres from the third, fourth and fifth sacral spinal segments F
pudendal nerve arises from S2, S3, and S4 spinal nerve roots, not S5.
D. is sensory to the skin of the scrotum T
E. is sensory to part of the urethra T