StemUp: OCR A A level Biology 4.1.1 Communicable diseases, disease prevention and the immune system
1/87
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
88 Terms
What is a disease? (1)
A condition that impairs the normal functioning of an organism
What is a pathogen? (1)
An organism that causes disease
What is a communicable disease? (1)
A disease that is spread between organisms
What are the types of pathogens? (4)
- Bacteria
- Viruses
- Fungi
- Protoctista
What are some examples of bacterial communicable diseases? (3)
- Tuberculosis = affects animals, mainly humans and cattle
- Bacterial meningitis = affects humans.
- Ring rot = affects potatoes and tomatoes
What are some examples of viral communicable diseases? (3)
- HIV/AIDS = affects humans
- Influenza = affects animals, including humans
- Tobacco mosaic virus = affects plants
What are some examples of fungal communicable diseases?
- Black sigatoka = affects bananas
- Ringworm = affects cattle
- Athlete's foot = affects humans
What are some examples of protoctista communicable diseases? (2)
- Potato/tomato late blight = affects potatoes and tomatoes.
- Malaria = affects animals, including humans.
What is direct transmission of a disease? (2)
- When a disease is transmitted directly from one organism to another
- Examples: droplet infection (coughing/sneezing), sexual intercourse, touching an infected organism
What are some examples of diseases transmitted through direct transmission? (2)
- HIV = transmitted via sexual intercourse
- Athlete's foot = spread via touch
What is indirect transmission of a disease? (2)
- When a disease is transmitted from one organism to another via an intermediate
- E.g., air, water, food, or another organism like a vector
What are some examples of diseases transmitted through indirect transmission? (2)
- Potato/tomato late blight = spread when spores are carried between plants via air and water
- Malaria = spread between humans and animals via mosquitos (mosquitos act as vectors)
What factors affect disease transmission? (3)
- Overcrowded living conditions
- Climate
- Social factors
How do overcrowded living conditions affect disease transmission e.g. TB? (3)
- Spread directly via droplet infection and indirectly because bacteria can survive in the air for long periods
- increasing infection risk in crowded environments
How does climate affect disease transmission? (4)
- E.g. Potato/tomato late blight
- Common in wet summers because spores need water to spread
- E.g. Malaria
- Common in hot, humid climates, which provide ideal conditions for mosquitos to breed
How do social factors affect disease transmission? (4)
- Limited access to good healthcare increases the risk of diseases like HIV
- Because people are less likely to be diagnosed and treated
- Limited access to health education increases the risk of HIV transmission
- Because people are less informed on how HIV is transmitted and how to prevent it
What are three physical defences plants use against pathogens? (3)
- Waxy cuticle
- Cell walls
- Callose
How does a waxy cuticle act as a physical defence against pathogens? (2)
- Physical barrier against pathogen entry
- Prevents water collection on the leaf, reducing infection by waterborne pathogens
How does the cell wall act as a physical defence against pathogens? (1)
Physical barrier against pathogens that get past the waxy cuticle
How does callose act as a physical defence against pathogens? (2)
- A polysaccharide deposited between plant cell walls and membranes during stress (e.g., pathogen invasion
- Callose deposition at plasmodesmata limits virus spread between cells
What are four chemical defences plants use against pathogens? (4)
- Antimicrobial chemicals
- Saponins
- Phytoalexins
- Chemicals toxic to insects
How do antimicrobial chemicals act as a chemical defence against pathogens? (1)
Kill pathogens or inhibit their growth
How do saponins act as a chemical defence against pathogens? (1)
Thought to destroy the cell membranes of fungi and other pathogens
How do phytoalexins act as a chemical defence against pathogens? (1)
Inhibit the growth of fungi and other pathogens
How do chemical toxins act as a chemical defence against pathogens? (2)
- Reduce insect feeding on plants
- Lowering the risk of viral infections carried by insect vectors
How does skin function as a defence mechanism? (2)
- Acts as a physical barrier, blocking pathogen entry
- Acts as a chemical barrier by producing antimicrobial chemicals that lower pH and inhibit pathogen growth
What is the role of mucous membranes in defense? (3)
- Protect body openings exposed to the environment (e.g., mouth, nostrils, ears, genitals, anus)
- Mucus traps pathogens.
- Mucus contains antimicrobial enzymes.
How does blood clotting defend the body? (2)
- Forms a mesh of fibrin fibers that plug wounds
- To prevent blood loss and pathogen entry
What triggers blood clotting? (2)
- A series of reactions initiated
- When platelets are exposed to damaged blood vessels
What are the signs of inflammation? (4)
- Swelling
- Pain
- Heat
- Redness
What is the purpose of inflammation? (3)
- Tissue damage releases molecules that increase blood vessel permeability
- Causing fluid leakage and swelling, isolating pathogens
- Molecules cause vasodilation, increasing blood flow to bring white blood cells to the area
How does vasodilation contribute to inflammation? (3)
- Increases blood flow to the affected area
- Raises temperature
- Brings white blood cells to fight pathogens
How does wound repair occur? (3)
1. Outer skin cells divide and migrate to wound edges
2. Underlying tissue contracts to bring wound edges together
3. Collagen fibers repair the wound, possibly resulting in scars.
What triggers expulsive reflexes, and what do they do? (2)
- Triggered by irritation of mucous membranes (sneezing) or the respiratory tract (coughing)
- Expel foreign objects, including pathogens, from the body automatically
What is a phagocyte? (2)
- A type of white blood cell that carries out phagocytosis (the engulfment of pathogens).
- Phagocytosis is non-specific (same for every pathogen)
What are neutrophils? (2)
- A type of phagocyte
- First white blood cells to respond to pathogens inside the body
How do neutrophils respond to wounds? (2)
- Neutrophils move towards wounds in response to cytokines (proteins that act as messenger molecules).
- Cytokines are released by cells at the site of the wound
What are the steps involved in phagocytosis? (6)
1. Phagocyte recognizes the antigens on a pathogen
2. Phagocyte engulfs the pathogen
3. Pathogen is contained inside a phagosome in the cytoplasm of the phagocyte
4. Lysosome fuses with the phagosome, and hydrolytic enzymes break down the pathogen
5. Phagocyte presents the antigens from the pathogen on its surface,
6. Activating other immune system cells (acting as an antigen-presenting cell (APC))
What are opsonins? (1)
Molecules in the blood that attach to foreign antigens to aid phagocytosis
What is a blood smear? (2)
- A sample of blood smeared on a microscope slide
- Often stained to make different cells easier to see
How can red blood cells be identified in a blood smear? (1)
By their lack of a nucleus
What are the characteristics of neutrophils in a blood smear? (2)
- Neutrophils have a multi-lobed nucleus (3 interconnecting blobs)
- Their cytoplasm is grainy
What are the characteristics of lymphocytes in a blood smear? (2)
- Smaller than neutrophils
- The nucleus takes up most of the cell, with very little cytoplasm
What are the characteristics of monocytes in a blood smear? (3)
- Largest white blood cell
- Kidney-shaped nucleus
- Non-grainy cytoplasm
What are T lymphocytes? (3)
- A type of white blood cell covered with receptors
- Receptors bind to antigens presented by APCs (antigen-presenting cells)
- Each T lymphocyte has a different receptor on its surface
How are T lymphocytes activated? (3)
- Activated when the receptor on the surface of the T lymphocyte
- Binds to a complementary antigen (clonal selection)
- Undergo clonal expansion, dividing to make clones of themselves
What are the four types of activated T lymphocytes? (4)
- T helper cells: Release substances to activate B lymphocytes and T killer cells
- T killer cells: Attach to and kill virus-infected cells
- T regulatory cells: Suppress the immune response to prevent immune cells from attacking host cells
- Memory T cells: Remember specific antigens for faster responses in the future
What are B lymphocytes? (2)
- A type of white blood cell covered with proteins called antibodies
- Each B lymphocyte has a different-shaped antibody on its surface
How are B lymphocytes activated? (4)
- Activated when antibodies on the surface
- Bind to complementary antigens to form an antibody-antigen complex (clonal selection)
- T helper cells release interleukins (cytokines)
- Which bind to B lymphocyte receptors and activate them (cell signalling)
What happens after B lymphocytes are activated? (5)
- Undergo clonal expansion, dividing by mitosis into
- Plasma cells
-Which secrete lots of antibodies into the blood, which bind to antigens and form antibody-antigen complexes
- Memory B lymphocytes
- That stay in the body to provide long-term immunity
What is the primary immune response? (3)
- Occurs when a pathogen enters the body for the first time and activates the immune system
- Slow response because it takes time to produce enough B lymphocytes with the right antibodies
- The infected person shows symptoms during this time
What happens after the primary immune response? (3)
- Memory T and B lymphocytes are produced and remain in the body for a long time
- Memory T cells remember the antigen for future recognition.
- Memory B cells quickly produce the antibodies needed to bind to the antigen if encountered again
What is the secondary immune response? (2)
- Occurs after the body is exposed to the same pathogen for a second time
- Faster and stronger than the primary response
How does clonal selection work in the secondary immune response? (3)
- Memory T cells are activated and divide into the correct type of T lymphocytes to kill infected cells
- Memory B cells are activated and divide into plasma cells that produce the right antibodies
- The pathogen is often eliminated before the person shows symptoms
Draw and label the general diagram of an antibody (5)
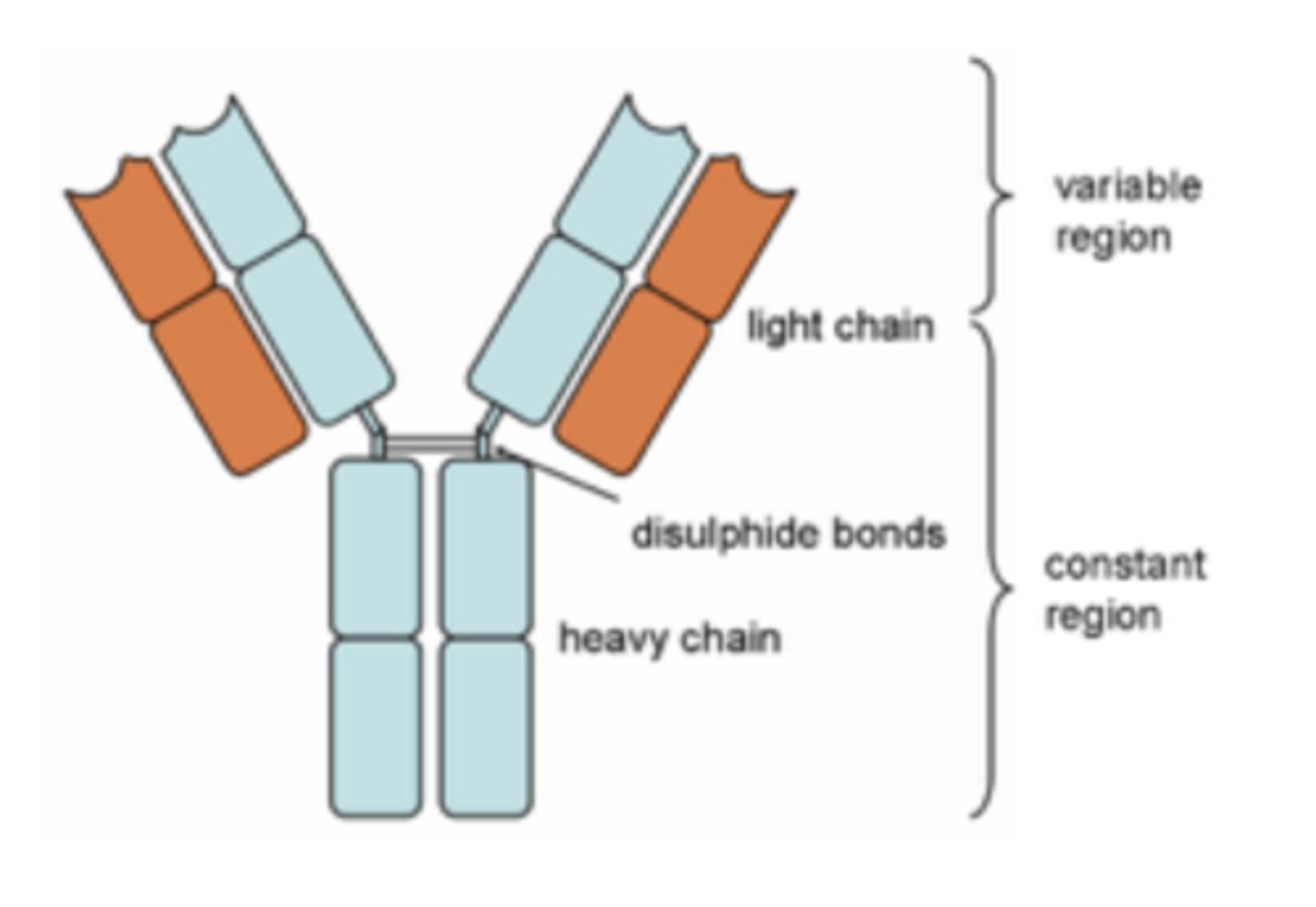
What forms the antigen-binding sites of an antibody? (3)
- The variable regions form the antigen-binding sites
- The shape of the variable region is complementary to a specific antigen
- The variable region differs between antibodies
What is the function of the constant region in antibodies? (2)
- Allows the antibody to bind to receptors on immune system cells (e.g., phagocytes)
- The constant region is the same in all antibodies
What is the role of the hinge region in antibodies? (1)
Provides flexibility when the antibody binds to an antigen
How are the polypeptide chains of antibodies held together? (1)
By disulphide bridges
What is agglutination, and how do antibodies help with this process? (2)
- Each antibody has two antigen-binding sites, allowing it to bind to two pathogens at the same time, clumping them together
- Phagocytes can bind to the antibodies and phagocytose many pathogens at once - agglutination
How do antibodies neutralise toxins? (3)
- Antibodies called anti-toxins bind to toxins produced by pathogens, neutralising them.
- This prevents the toxins from affecting human cells
- The toxin-antibody complexes are phagocytosed
How do antibodies prevent pathogens from infecting human cells? (2)
- By blocking the cell surface receptors that pathogens need to bind to host cells
- This prevents the pathogens from attaching to and infecting host cells
What are the key characteristics of active immunity? (4)
- Requires exposure to antigen
- Takes a while for protection to develop
- Protection is long-term
- Memory cells are produced
What are the key characteristics of passive immunity? (4)
- No exposure to antigen required
- Protection is immediate
- Protection is short-term
- Memory cells are not produced
What is natural active immunity? (1)
Immunity acquired after catching a disease
What is artificial active immunity? (1)
Immunity acquired after being given a vaccination containing a harmless dose of an antigen
What is natural passive immunity? (1)
Immunity a baby receives via antibodies from the mother through the placenta and breast milk
What is artificial passive immunity? (2)
- Immunity acquired after being injected with antibodies from someone else
- E.g., being given antibodies against the tetanus toxin collected from blood donors
What is an autoimmune disease? (1)
A disease caused by an abnormal immune response where the immune system attacks the body's own cells
How do autoimmune diseases arise? (2)
- Happens because the immune system cannot recognise self-antigens (antigens on the organism's own cells)
- Autoimmune diseases tend to be chronic and can be treated, but not cured
What is lupus? (1)
An autoimmune disease where the immune system attacks cells in connective tissue
How does lupus affect the body? (2)
- It causes tissue damage and painful inflammation
- Can affect the skin, joints, heart, lungs, and other organs
What is rheumatoid arthritis, and how does it affect the body? (2)
- Rheumatoid arthritis is caused by the immune system attacking cells in the joints
- It leads to pain and inflammation in the joints
How do vaccines work? (3)
- Contain antigens (free or attached to a dead or attenuated pathogen)
- That stimulate the body to produce memory cells against a specific pathogen
- Without causing disease
What is herd immunity? (2)
- When most people in a community are vaccinated, the disease becomes rare
- Unvaccinated people are less likely to get the disease because there are fewer people to catch it from
What is the difference between vaccination and immunisation? (2)
- Vaccination: Administration of an antigen in a vaccine into the body.
- Immunisation: The process of developing immunity through vaccination
What are some routine vaccinations? (2)
- MMR vaccine: Given to children at around 1 year old and again before school; contains attenuated measles, mumps, and rubella viruses
- Meningitis C vaccine: Protects against Meningitis C bacteria; given at 3 months old with boosters at 1 year old and during teenage years
Why is the influenza vaccine changed every year? (3)
- The antigens on the surface of the influenza virus change regularly, forming new strains
- Memory cells from one strain will not recognise other strains with different antigens
- WHO and CDC decide the strains included in the vaccine based on circulating strains
How do vaccination programs help prevent epidemics? (2)
- hey prevent mass outbreaks of diseases by achieving herd immunity.
- They help stop the global spread of disease strains causing epidemics in other countries
What are some natural sources of medicines? (3)
- Penicillin: Obtained from a fungus
- Cancer drugs: Made using soil bacteria
- Alzheimer's drug: Daffodils are grown to produce this drug
Why is biodiversity important in medicine development? (2)
- Maintaining biodiversity ensures that potential sources of new drugs are not lost
- Species may become extinct before they are studied for possible medical benefits
What is personalised medicine? (3)
- Medicine tailored to a person's DNA.
- Genetic information is used to predict how a patient will respond to different drugs
- Allowing for more effective prescriptions
What is synthetic biology? (2)
- The use of technology to design and make artificial proteins, cells, and microorganisms
- An example is engineering bacteria to destroy cancer cells while leaving healthy body cells intact
What are the benefits of using antibiotics to manage bacterial infections? (3)
- Kill or inhibit the growth of bacteria
- Death rates from bacterial diseases have dramatically fallen since widespread use of antibiotics
- Antibiotics can target bacterial cells without damaging human cells
What are the risks of using antibiotics? (3)
- Potential side effects
- Possible allergic reactions
- Risk of antibiotic resistance
What are superbugs? (2)
- Bacteria that are resistant to most known antibiotics
- Making bacterial infections harder to treat
What are examples of antibiotic-resistant bacteria? (2)
- MRSA
- Clostridium difficile (C. difficile)
How can the likelihood of antibiotic resistance be reduced? (3)
- Doctors are advised to prescribe fewer antibiotics
- Patients are encouraged to complete their entire course of antibiotics to ensure all bacteria are killed
- Reducing the risk of developing antibiotic-resistant bacteria