Chapter 19: The Cardiovascular System: The Heart
- Although the term “heart” is an English word, cardiac (heart-related) terminology can be traced back to the Latin term, “kardia.”
- Cardiology is the study of the heart, and cardiologists are the physicians who deal primarily with the heart.
Heart Anatomy
Location of the Heart
- The human heart is located within the thoracic cavity, medially between the lungs in the space known as the mediastinum.
- Within the mediastinum, the heart is separated from the other mediastinal structures by a tough membrane known as the pericardium, or pericardial sac, and sits in its own space called the pericardial cavity.
- The slight deviation of the apex to the left is reflected in a depression in the medial surface of the inferior lobe of the left lung, called the cardiac notch.
Shape and Size of the Heart
- The shape of the heart is similar to a pinecone, rather broad at the superior surface and tapering to the apex.
- A typical heart is approximately the size of your fist: 12 cm (5 in) in length, 8 cm (3.5 in) wide, and 6 cm (2.5 in) in thickness.
- Enlarged hearts are not always a result of exercise; they can result from pathologies, such as hypertrophic cardiomyopathy.
Chambers and Circulation through the Heart
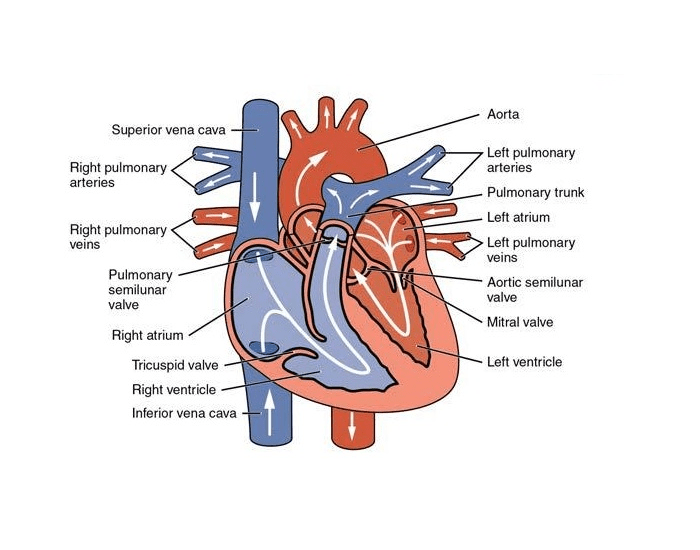
- The human heart consists of four chambers: The left side and the right side each have one atrium and one ventricle.
- Each of the upper chambers, the right atrium (plural = atria) and the left atrium, acts as a receiving chamber and contracts to push blood into the lower chambers, the right ventricle and the left ventricle.
- The pulmonary circuit transports blood to and from the lungs, where it picks up oxygen and delivers carbon dioxide for exhalation.
- The systemic circuit transports oxygenated blood to virtually all of the tissues of the body and returns relatively deoxygenated blood and carbon dioxide to the heart to be sent back to the pulmonary circulation.
- The right ventricle pumps deoxygenated blood into the pulmonary trunk, which leads toward the lungs and bifurcates into the left and right pulmonary arteries.
- The capillaries will ultimately unite to form venules, joining to form ever-larger veins, eventually flowing into the two major systemic veins, the superior vena cava and the inferior vena cava, which return blood to the right atrium.
Membranes
- The membrane that directly surrounds the heart and defines the pericardial cavity is called the pericardium or pericardial sac.
- It also surrounds the “roots” of the major vessels, or the areas of closest proximity to the heart.
- The more delicate serous pericardium consists of two layers: the parietal pericardium, which is fused to the fibrous pericardium, and an inner visceral pericardium, or epicardium, which is fused to the heart and is part of the heart wall.
- In the case of the heart, it is not a microscopic layer but rather a macroscopic layer, consisting of a simple squamous epithelium called a mesothelium, reinforced with loose, irregular, or areolar connective tissue that attaches to the pericardium.
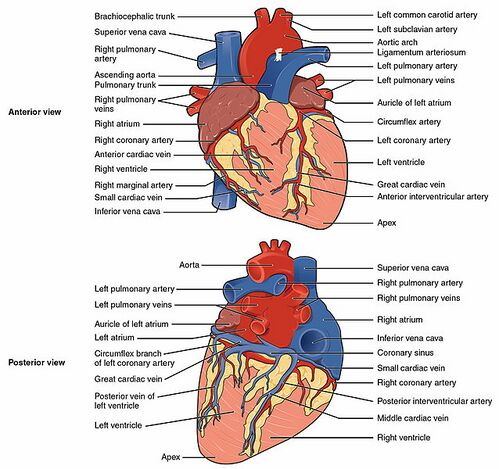
Surface Features of the Heart
- There is a superficial leaf- like extension of the atria near the superior surface of the heart, one on each side, called an auricle, a name that means “ear-like” because its shape resembles the external ear of a human.
- Also prominent is a series of fat-filled grooves, each of which is known as a sulcus (plural = sulci), along the superior surfaces of the heart.
- The deep coronary sulcus is located between the atria and ventricles.
- The anterior interventricular sulcus is visible on the anterior surface of the heart, whereas the posterior interventricular sulcus is visible on the posterior surface of the heart.
Layers
- The wall of the heart is composed of three layers of unequal thickness.
- From superficial to deep, these are the epicardium, the myocardium, and the endocardium.
- The outermost layer of the wall of the heart is also the innermost layer of the pericardium, the epicardium, or the visceral pericardium.
Septa of the Heart
- The word septum is derived from the Latin for “something that encloses;” in this case, a septum (plural = septa) refers to a wall or partition that divides the heart into chambers.
- Located between the two atria is the interatrial septum. circuit.
- Within seconds after birth, a flap of tissue known as the septum primum that previously acted as a valve closes the foramen ovale and establishes the typical cardiac circulation pattern.
- Between the two ventricles is a second septum known as the interventricular septum.
- The septum between the atria and ventricles is known as the atrioventricular septum.
- Located in each of these openings between the atria and ventricles is a valve, a specialized structure that ensures one-way flow of blood.
- The valves between the atria and ventricles are known generically as atrioventricular valves.
- The valves at the openings that lead to the pulmonary trunk and aorta are known generically as semilunar valves.
- Since these openings and valves structurally weaken the atrioventricular septum, the remaining tissue is heavily reinforced with dense connective tissue called the cardiac skeleton, or skeleton of the heart.
Right Atrium
- The right atrium serves as the receiving chamber for blood returning to the heart from the systemic circulation.
- The two major systemic veins, the superior and inferior venae cavae, and the large coronary vein called the coronary sinus that drains the heart myocardium empty into the right atrium.
- While the bulk of the internal surface of the right atrium is smooth, the depression of the fossa ovalis is medial, and the anterior surface demonstrates prominent ridges of muscle called the pectinate muscles.
Right Ventricle
- The right ventricle receives blood from the right atrium through the tricuspid valve.
- Each flap of the valve is attached to strong strands of connective tissue, the chordae tendineae, literally “tendinous cords,” or sometimes more poetically referred to as “heart strings.”
- They connect each of the flaps to a papillary muscle that extends from the inferior ventricular surface.
- The walls of the ventricle are lined with trabeculae carneae, ridges of cardiac muscle covered by endocardium.
- In addition to these muscular ridges, a band of cardiac muscle, also covered by endocardium, known as the moderator band.
Heart Valve Structure and Function
- Between the right atrium and the right ventricle is the right atrioventricular valve, or tricuspid valve.
- Emerging from the right ventricle at the base of the pulmonary trunk is the pulmonary semilunar valve, or the pulmonary valve; it is also known as the pulmonic valve or the right semilunar valve.
- Located at the opening between the left atrium and left ventricle is the mitral valve, also called the bicuspid valve or the left atrioventricular valve.
- At the base of the aorta is the aortic semilunar valve, or the aortic valve, which prevents backflow from the aorta.
Coronary Arteries
- Coronary arteries supply blood to the myocardium and other components of the heart.
- Coronary vessel branches that remain on the surface of the artery and follow the sulci are called epicardial coronary arteries.
- The circumflex artery arises from the left coronary artery and follows the coronary sulcus to the left.
- The larger anterior interventricular artery, also known as the left anterior descending artery (LAD), is the second major branch arising from the left coronary artery.
- An anastomosis is an area where vessels unite to form interconnections that normally allow blood to circulate to a region even if there may be partial blockage in another branch.
- The marginal arteries supply blood to the superficial portions of the right ventricle.
- On the posterior surface of the heart, the right coronary artery gives rise to the posterior interventricular artery, also known as the posterior descending artery.
Coronary Veins
- Coronary veins drain the heart and generally parallel the large surface arteries.
- The great cardiac vein can be seen initially on the surface of the heart following the interventricular sulcus, but it eventually flows along the coronary sulcus into the coronary sinus on the posterior surface.
- The posterior cardiac vein parallels and drains the areas supplied by the marginal artery branch of the circumflex artery.
- The middle cardiac vein parallels and drains the areas supplied by the posterior interventricular artery.
- The small cardiac vein parallels the right coronary artery and drains the blood from the posterior surfaces of the right atrium and ventricle.
- The anterior cardiac veins parallel the small cardiac arteries and drain the anterior surface of the right ventricle.
Cardiac Muscle and Electrical Activity
Structure of Cardiac Muscle
- Cardiac muscle cells branch freely.
- A junction between two adjoining cells is marked by a critical structure called an intercalated disc, which helps support the synchronized contraction of the muscle.
Sinoatrial (SA) Node
- Normal cardiac rhythm is established by the sinoatrial (SA) node, a specialized clump of myocardial conducting cells located in the superior and posterior walls of the right atrium in close proximity to the orifice of the superior vena cava.
- This impulse spreads from its initiation in the SA node throughout the atria through specialized internodal pathways, to the atrial myocardial contractile cells and the atrioventricular node.
- There is a specialized pathway called Bachmann’s bundle or the interatrial band that conducts the impulse directly from the right atrium to the left atrium.
Atrioventricular (AV) Node
- The atrioventricular (AV) node is a second clump of specialized myocardial conductive cells, located in the inferior portion of the right atrium within the atrioventricular septum.
- The Purkinje fibers are additional myocardial conductive fibers that spread the impulse to the myocardial contractile cells in the ventricles.
Electrocardiogram
- By careful placement of surface electrodes on the body, it is possible to record the complex, compound electrical signal of the heart.
- This tracing of the electrical signal is the electrocardiogram (ECG), also commonly abbreviated EKG (K coming kardiology, from the German term for cardiology).
Cardiac Muscle Metabolism
- Normally, cardiac muscle metabolism is entirely aerobic.
- Oxygen from the lungs is brought to the heart, and every other organ, attached to the hemoglobin molecules within the erythrocytes.
Cardiac Cycle
- The period of time that begins with contraction of the atria and ends with ventricular relaxation is known as the cardiac cycle.
- The period of contraction that the heart undergoes while it pumps blood into circulation is called systole.
- The period of relaxation that occurs as the chambers fill with blood is called diastole.
Cardiac Physiology
Resting Cardiac Output
- Cardiac output (CO) is a measurement of the amount of blood pumped by each ventricle in one minute.
- Since the heart is a muscle, exercising it increases its efficiency.
- The difference between maximum and resting CO is known as the cardiac reserve. It measures the residual capacity of the heart to pump blood.
- So although aerobic exercises are critical to maintain the health of the heart, individuals are cautioned to monitor their HR to ensure they stay within the target heart rate range of between 120 and 160 bpm, so CO is maintained.
- During rest, both centers provide slight stimulation to the heart, contributing to autonomic tone.
- Both sympathetic and parasympathetic stimulations flow through a paired complex network of nerve fibers known as the cardiac plexus near the base of the heart.
Input to the Cardiovascular Center
- Collectively, these inputs normally enable the cardiovascular centers to regulate heart function precisely, a process known as cardiac reflexes.
- The cardiac centers monitor baroreceptor firing to maintain cardiac homeostasis, a mechanism called the baroreceptor reflex.
- There is a similar reflex, called the atrial reflex or Bainbridge reflex, associated with varying rates of blood flow to the atria.
- Afterload: Afterload refers to the tension that the ventricles must develop to pump blood effectively against the resistance in the vascular system.
Development of the Heart
- The critical early development of the heart is reflected by the prominent heart bulge that appears on the anterior surface of the embryo.
- The heart forms from an embryonic tissue called mesoderm around 18 to 19 days after fertilization.
- The heart begins to develop near the head of the embryo in a region known as the cardiogenic area.
- The cardiogenic area begins to form two strands called the cardiogenic cords.
- The two tubes migrate together and fuse to form a single primitive heart tube.
- The truncus arteriosus will eventually divide and give rise to the ascending aorta and pulmonary trunk.
- The bulbus cordis develops into the right ventricle.
- The primitive ventricle forms the left ventricle.
- The primitive atrium becomes the anterior portions of both the right and left atria, and the two auricles.
- The sinus venosus develops into the posterior portion of the right atrium, the SA node, and the coronary sinus.