Chapter 19: Regulation of Metabolism
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
34 Terms
Control & Integration of Carbohydrate, Protein, & Fat Metabolism
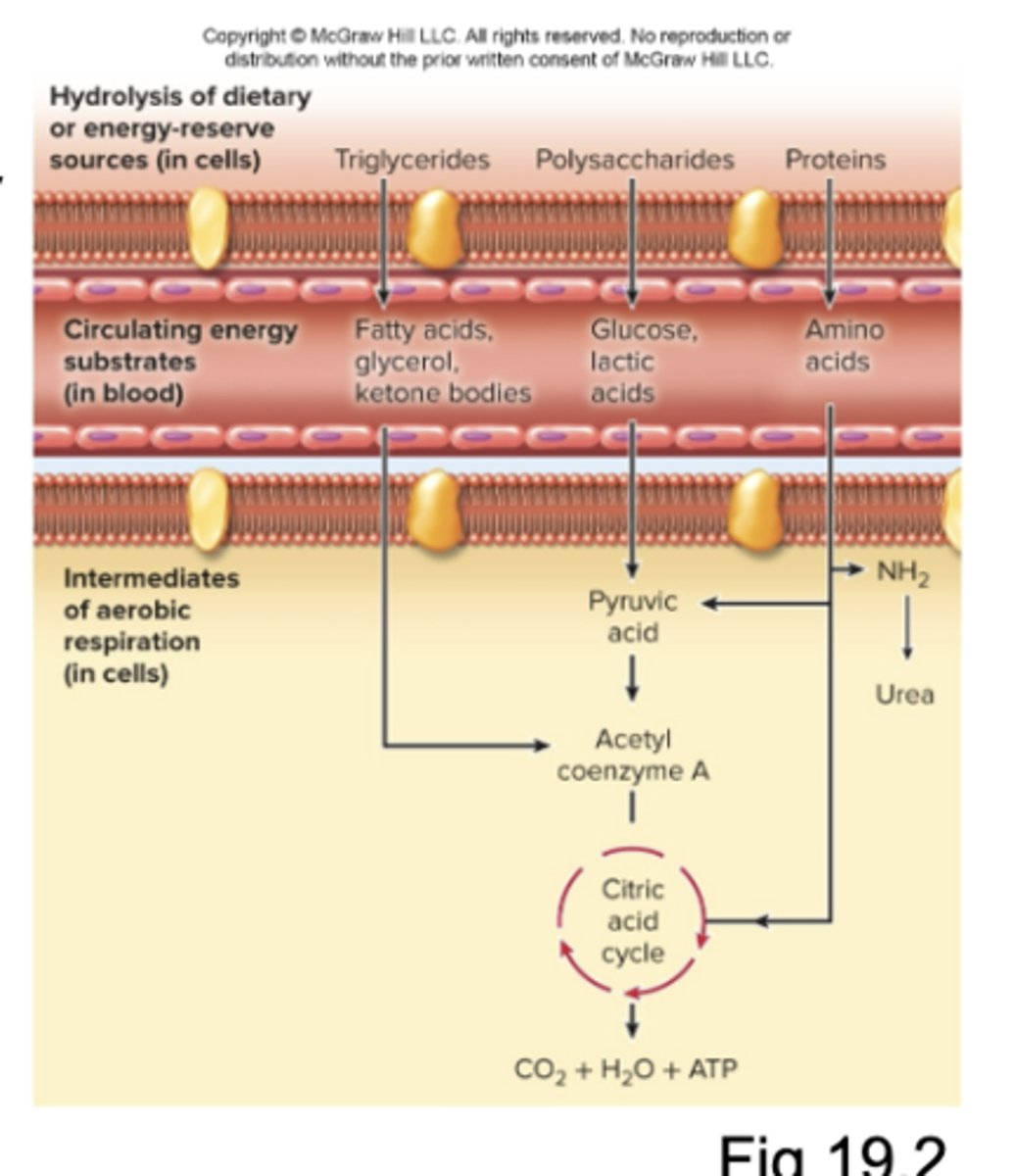
☆ Here, metabolism is defined as all of the chemical reactions in the body
- Plasma contains circulating glucose, fatty acids, and AAs used by the body's cells for the production of energy via cell respiration
- Energy reserves in cells: triglycerides, carbohydrates, and proteins (broken down via catabolism)
- Glucose concentration in blood must be maintained in a normal, healthy range for the production of energy
- Complete absorption of an average meal takes around 4 hours
- There are energy reserves (stores, storage) that are synthesized after a meal, via anabolism
Absorptive and Postabsorbtive States
☆ There are two functional states for providing energy for cellular activities and maintaining blood glucose concentration:
1. Absorptive State
2. Postaborbtive State
Absorptive State
☆ "Feasting/fed," when nutrients are absorbed into the bloodstream from the GI tract during the 4 h period following a meal
Postabsorptive State (Defintion)
☆ "Fasting," after the absorptive state, when the GI tract is empty of nutrients and the body's reserves supply energy
Regulation of States (Next 2)
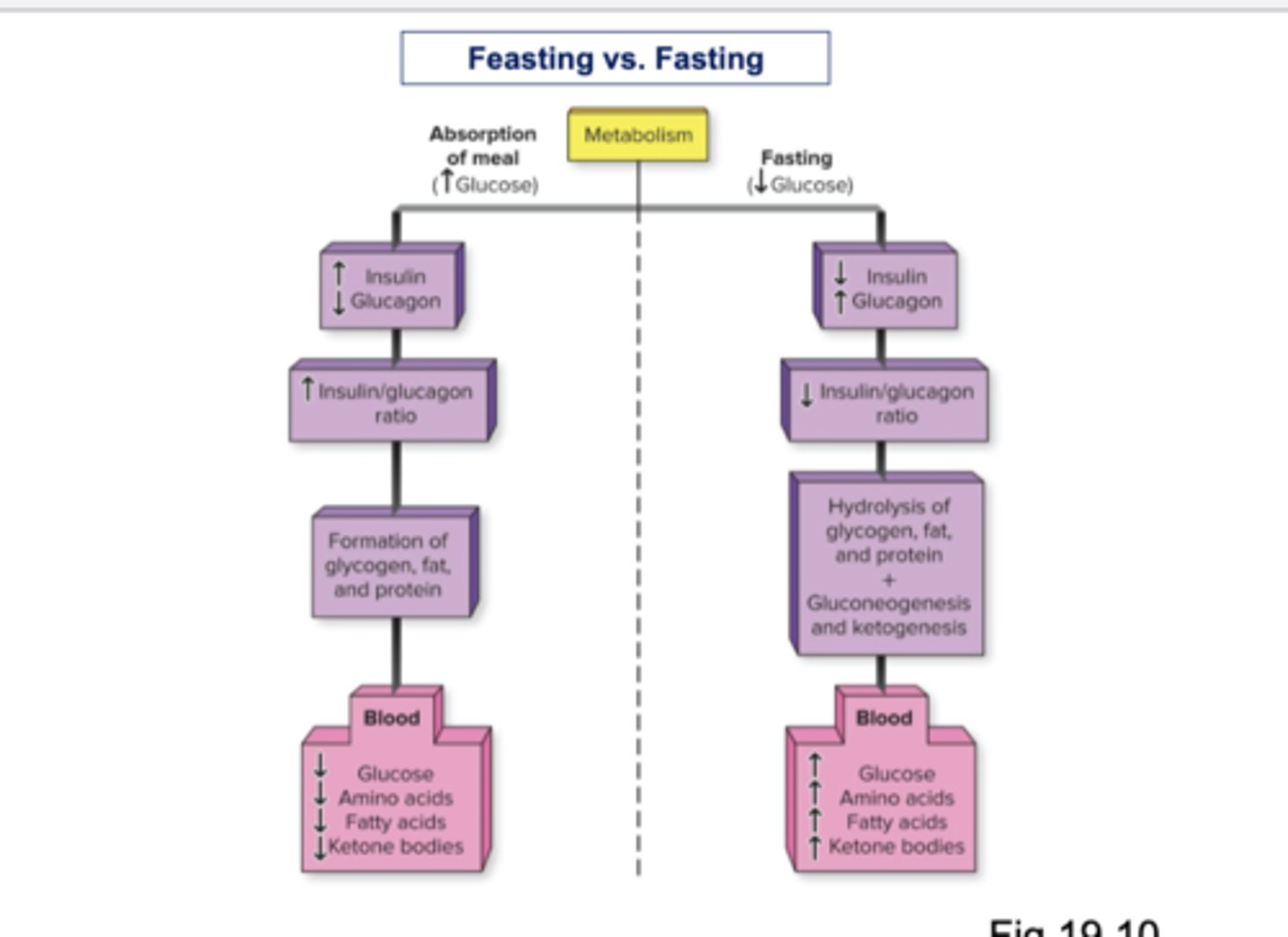
☆ Glucagon and insulin are hormones that regulate the transition between fasting and feasting and maintain homeostasis of glucose
1. Alpha Cells
2. Beta Cells
Alpha Cells
☆ Of pancreatic islets (islets of Langerhans) secrete glucagon
Beta Cells
☆ Of pancreatic islets secrete insulin
Absorptive State (Carbohydrates) (Next 2)
☆ Carbohydrates are absorbed into the bloodstream from the GI tract as monosaccharides , increasing blood glucose concentration
☆ Insulin
☆ Glucose
Insulin
☆ Increased secretion during absorptive state, when blood glucose is high (140-150 mg/dl)
Glucose
☆ Body's major energy source during absorptive state
- Insulin promotes cellular uptake of glucose
- Insulin promotes storage of glucose as glycogen in liver and muscles = Glycogenesis (anabolism)
- In cells, glucose is catabolized to Carbon Dioxide, Water, and ATP during cell respiration
- Adipose-tissue cells (adipocytes) transform glucose to fat (triglycerides) which is stored in adipose tissue = lipogenesis (anabolism)
- In the liver, glucose is also transformed into triglycerides, to be stored in adipocytes = lipogenesis
Absorptive State (Proteins)
☆ Are absorbed into the blood from the Gi tract as AAs
- Insulin promotes cellular uptake of AAs and their incorporation into proteins = protein synthesis (anabolism)
- Protein synthesis occurs in liver and many other tissues
Absorptive State (Lipids)
☆ Are absorbed into lymph as chylomicrons
- Insulin promotes conversion of lipids + glucose into lipogenesis (anabolism)...
- Cholesterol from chylomicrons is a component for bile salts and steroid hormones
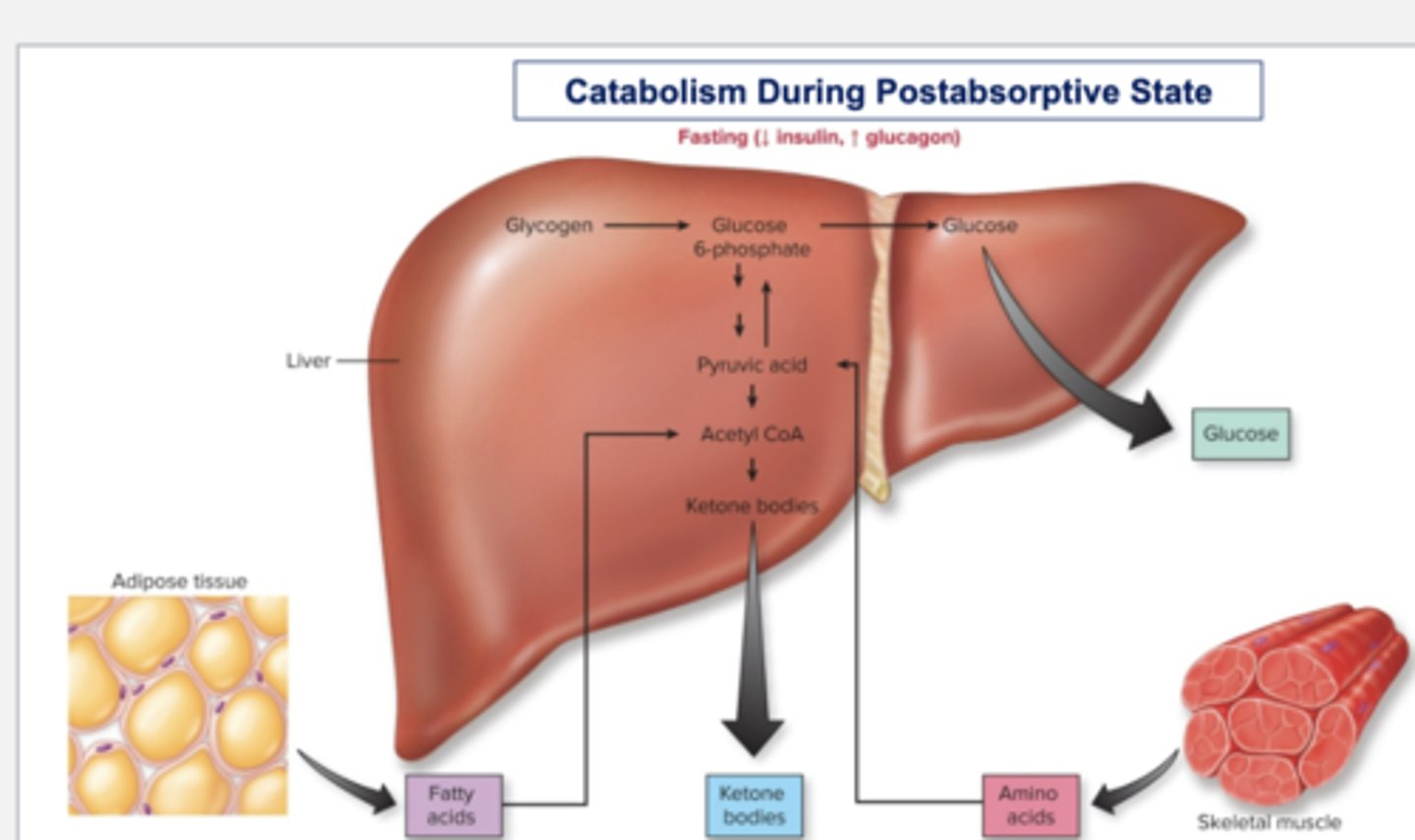
Postabsorptive State Pt. 1
☆ Synthesis of glycogen, triglycerides, and proteins ends
☆ Catabolism of reserves begins due to secretion of glucagon
☆ Glucagon
Glucagon + Stimulants (Next 3)
☆ Increased secretion during postabsorptive state, when blood glucose is low (fasting blood glucose of 65-105 mg/dl)
- Stimulates:
1. Glycogenolysis
2. Gluconeogensis
3. Glucose Sparing
Glycogenolysis
☆ Hydrolysis of glycogen in liver to increase blood glucose (glucose from glycogenolysis in skeletal muscle is used locally)
Gluconeogenesis
☆ Synthesis of glucose from AAs, glycerol, pyruvate, and lactate, in liver and kidneys
Glucose Sparing
Most tissues (except nervous) can use free fatty acids from (lipolysis) for energy instead of glucose
Postabsorptive State Pt. 2
☆ Ketogenesis in liver during prolonged fasting
- Synthesis of keton bodies from fatty acids
- Used as an alternative energy source during prolonged fasting (esp. nervous tissue)
Protein Catabolism
☆ In all tissue = breakdown of proteins into AAs
Lipolysis
☆ The breakdown of stored fat
Catabolism During Postabsorptive State
☆ During fasting, insulin secretion decreases and glucagon secretion increases
☆ There is release of glucose, fatty acids, ketone bodies, and AAs into the blood, the liver also releases glucose synthesized by glucoeneogenesis
Feasting vs Fasting Image
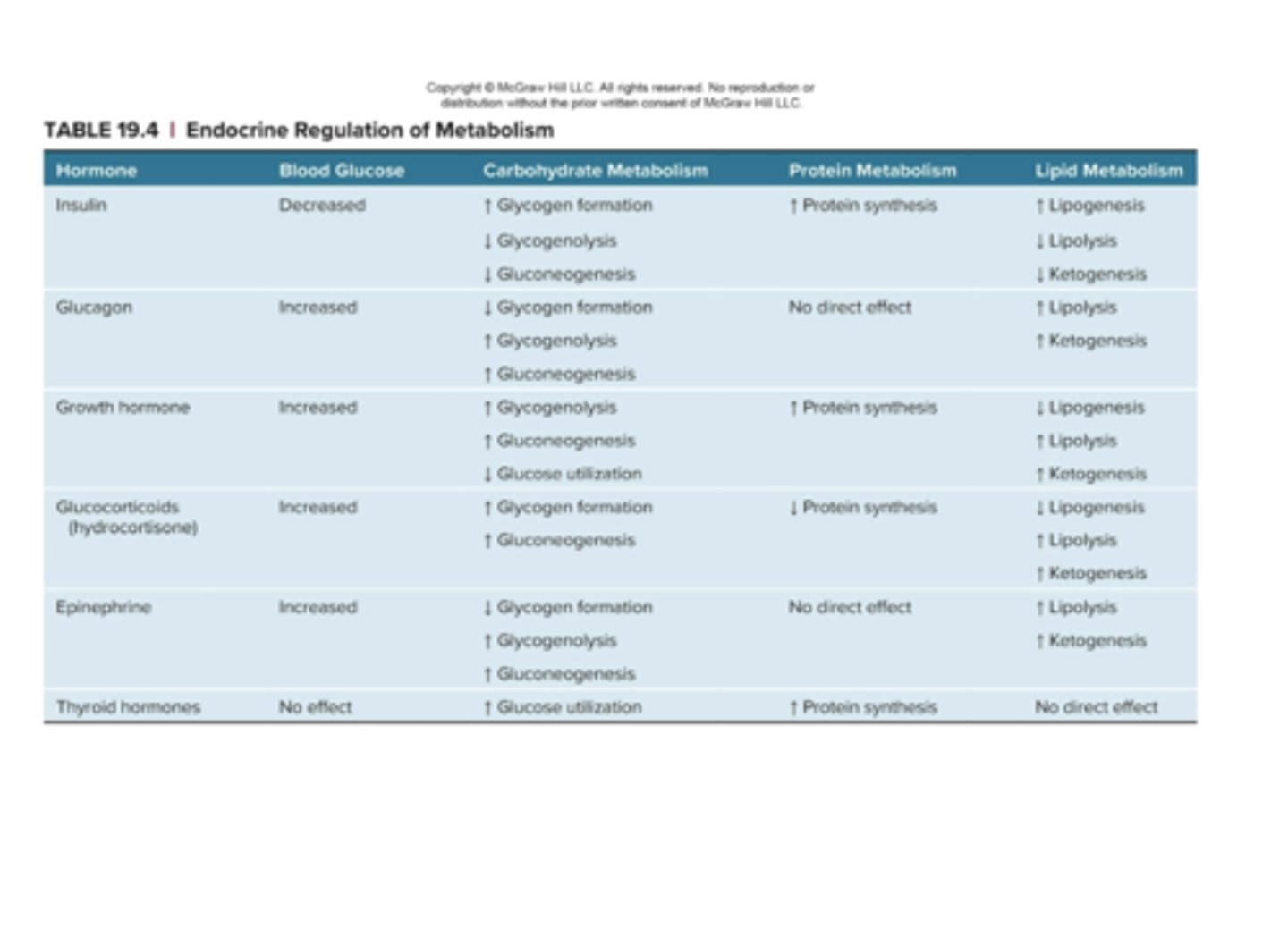
Endocrine Regulation of Metabolism Table
Diabetes Mellitus
☆ Chronic high blood glucose, hyperglycemia
☆ Two Types:
1. Type 1 diabetes mellitus (T1DM, insulin-dependent)
2. Type 2 diabetes (T2DM, non-insulin-dependent)
☆ 3 Ps: Polyuria, Polyphagia, Polydipsia
Type 1 Diabetes
☆ Insulin deficiency due to autoimmune destruction of beta cells, so insulin must be injected, pumped, or inhaled
- Genetic & environmental causes
- Hyperglycemia occurs because cellular uptake of glucose is impaired with lack of insulin
- Glucosuria occurs because amount of glucose filtered into urine exceeds maximum for reabsorption in kidneys
☆ Ketosis
- Excessive excretion of water in urine bacause excessive glucose and ketone bodies in urine cause osmotic diuresis
Ketosis (T1D)
☆ Ketone body concentration is elevated because increased lipolysis (due to lack of insulin) releases fatty acids, which are converted to ketone bodies (acidic)
- Ketoacidosis (and ketone breath) can occur if there is not enough bicarbonate to neutralize acid from ketone bodies
Type 2 Diabetes
☆ Insulin is present but target cells are resistant to insulin, so blood glucose concentration remains high
- Most common form of diabetes (around 90% of diabetics)
- Usually begins in adulthood (although often occurs in childhood nowadays)
- Common in obese individuals because insulin sensitivity is reduced by the presence of excess adipocytes
- The best treatment is weight reduction and exercise to increase insulin sensitivity in target cells
- Drug treatments also improve insulin sensitivity
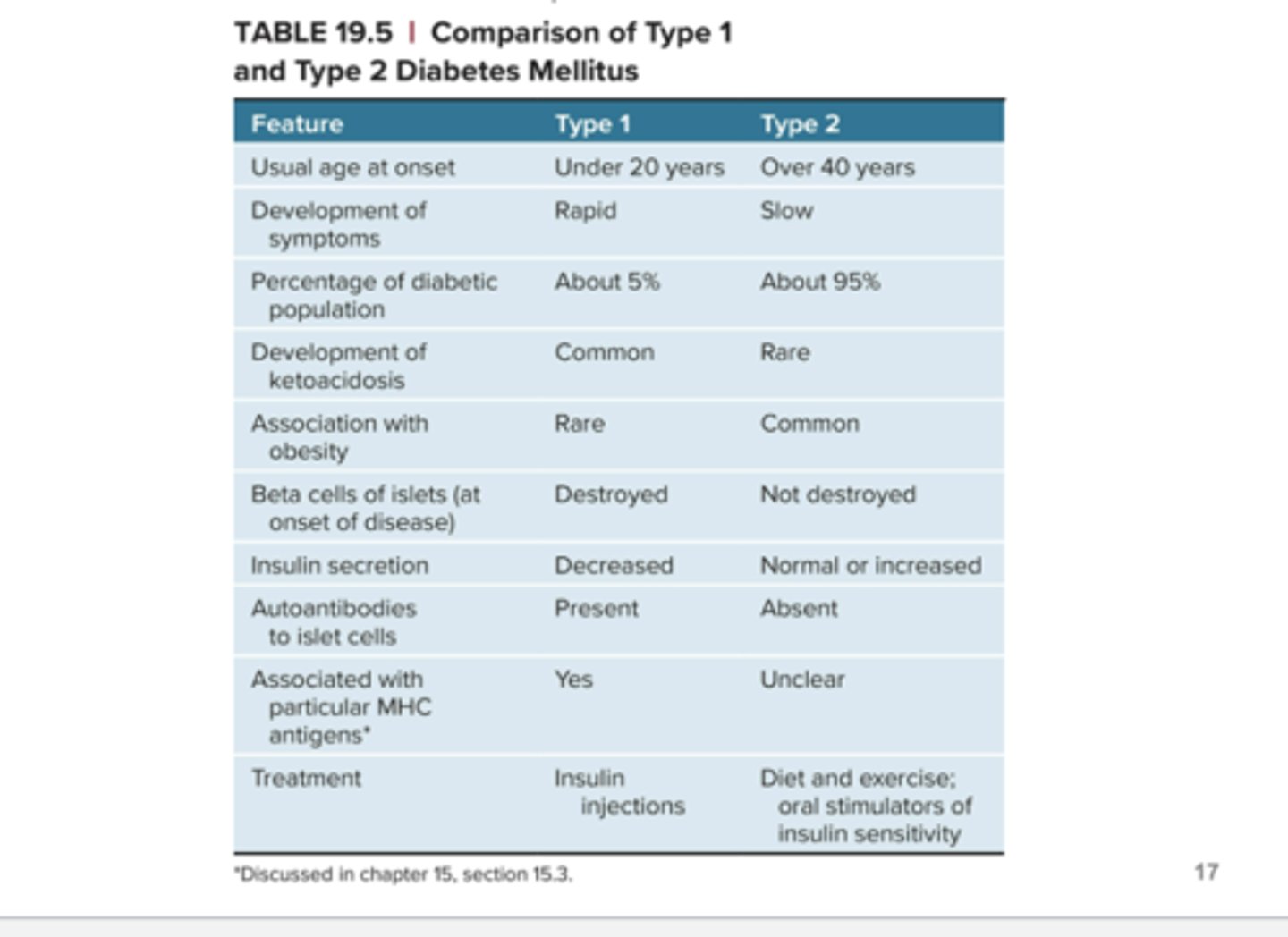
Comparison of Type 1 and Type 2 Diabetes Mellitus
Effects of Diabetes
☆ Tissue damage
☆ Peripheral nerve damage leads to decreasing sensation in the extremities
☆ Damage to capillaries in eyes and kidneys leads to blindness and kidney failure
☆ Circulatory deficiencies may result in damage to the feet, infection, gangrene, and may require amputation
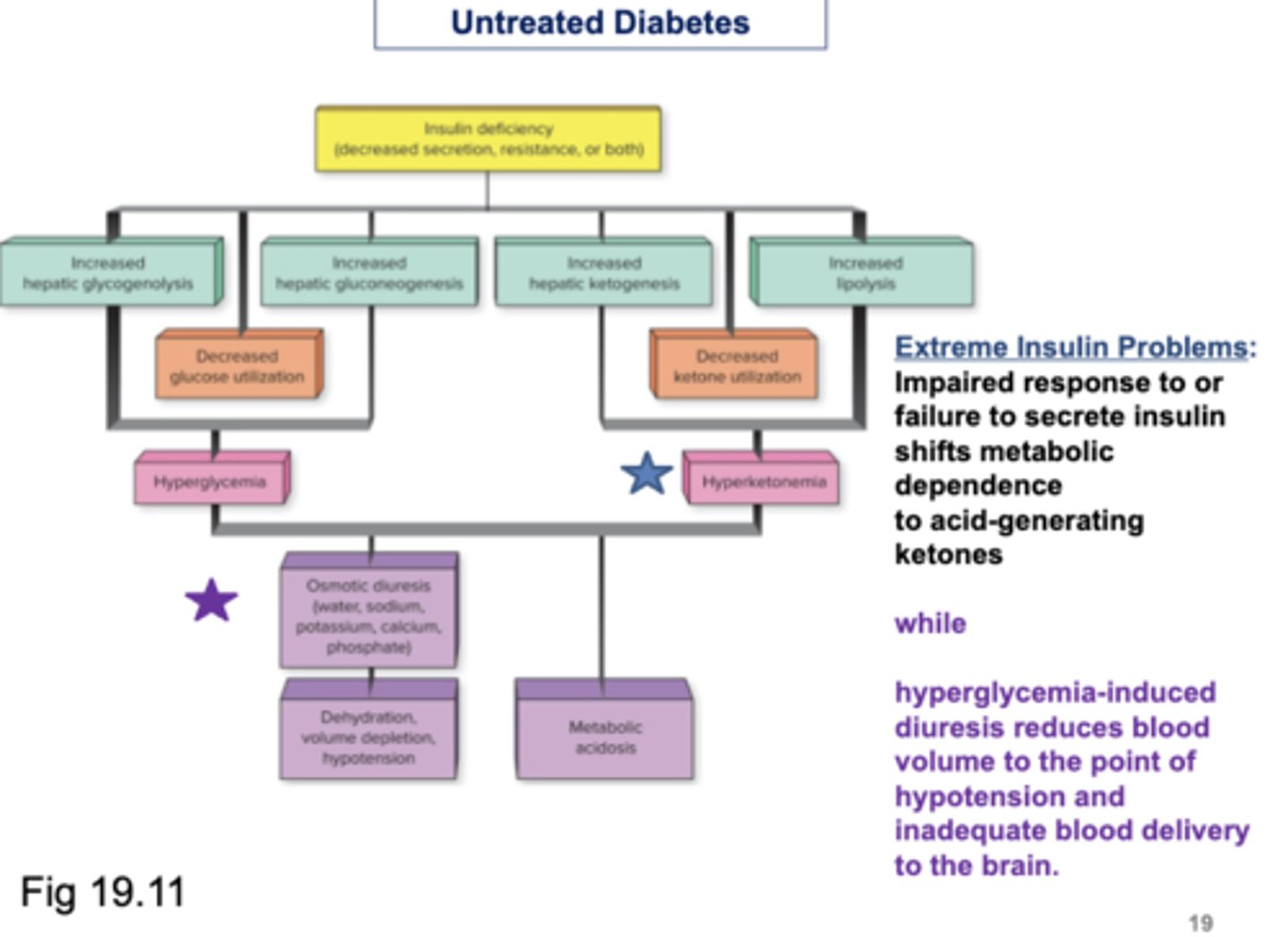
Untreated Diabetes
☆ Extreme Insulin Problems:
- Impaired response to or failure to secrete insulin shifts metabolic dependence to acid-generating ketones
WHILE
- hyperglycemia-induced diuresis reduces blood volume to the point of hypotension and inadequate blood delivery to the brain
Cholesterol
☆ Sources:
- Dietary, absorbed into bloodstream from SI
- Synthesized in liver
Functions of Cholesterol
☆ Found in plasma membrane
☆ Basis for steroids and bile salts
☆ In liver, combines with triglycerides and proteins to form VLDLs (very low density lipoproteins), which are secreted into the blood to deliver triglycerides to organs
☆ Found in LDLs (low density lipoproteins), which carry cholesterol to organs, including blood vessel walls
- LDL is the "bad cholesterol"
- Excess --> atherosclerosis
☆ Found in HDLs (high density lipoproteins), to which excess cholesterol from organs is attached to return to the liver
- HDL is the "good cholesterol"
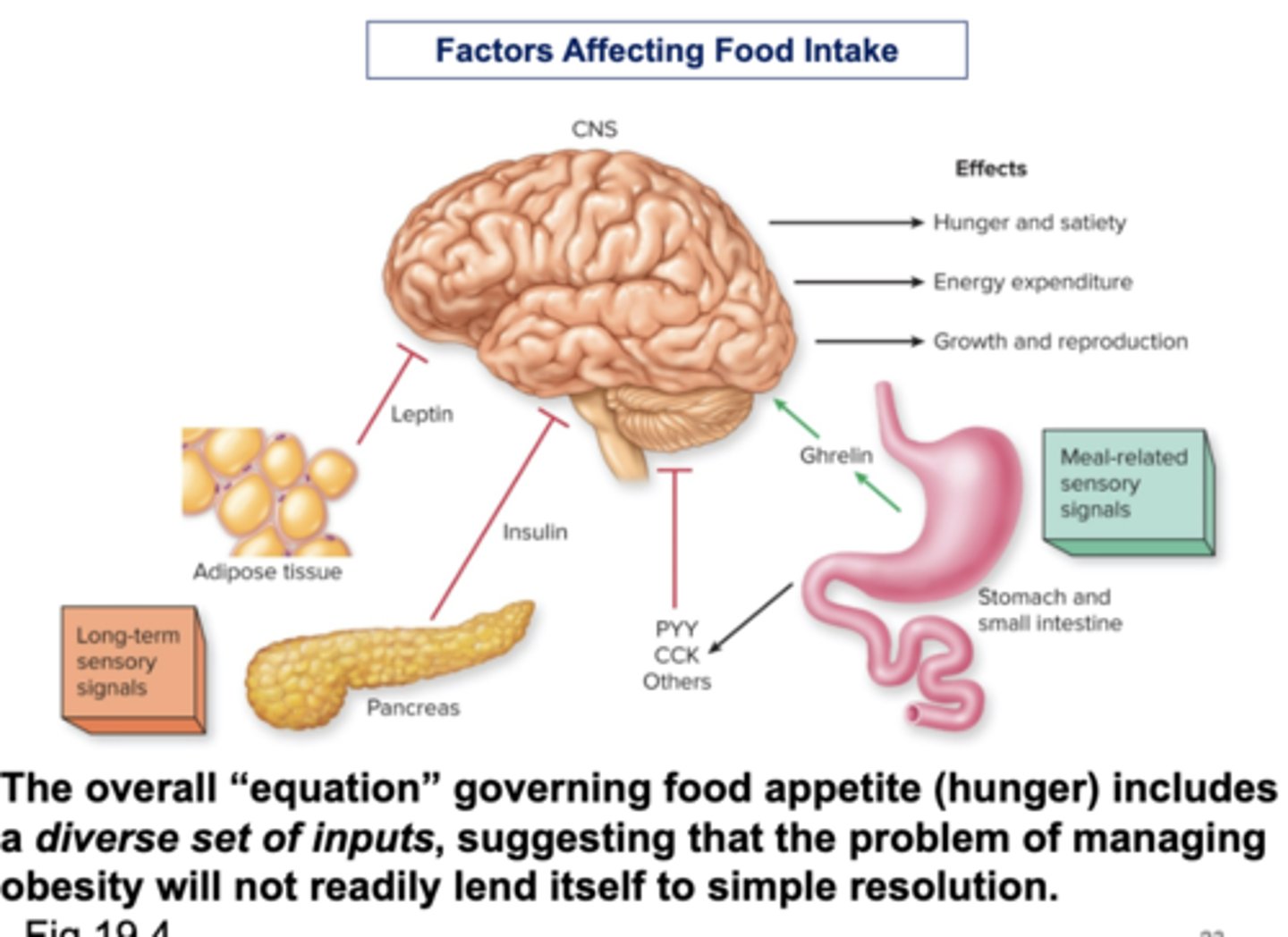
Control of Food Intake
☆ For regulation of total-body energy content and fat stores
☆ A key hormone for long-term regulation is leptin, which is synthesized in adipocytes and released in proportion to the amount of fat being stored
- Acts on hypothalamus to decrease appetite/food intake and increase metabolic rate
☆ There are several other factors that affect hunger
Factors Affecting Food Intake
☆ The overall "equation" governing food appetite (hunger) includes a diverse set of inputs, suggesting that the problem of managing obesity will not readily lend itself to simple resolution