Lung Pathogens Causing Pneumonia
1/70
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
71 Terms
•Infection of the lower respiratory tract symptoms and signs
Symptoms include cough, chest pain, fever, and difficulty in breathing
Sputum is often rust-colored from blood coughed up from lungs (thick and yellow with streaks of blood)
•Radiological lung opacity
•Seen as different types
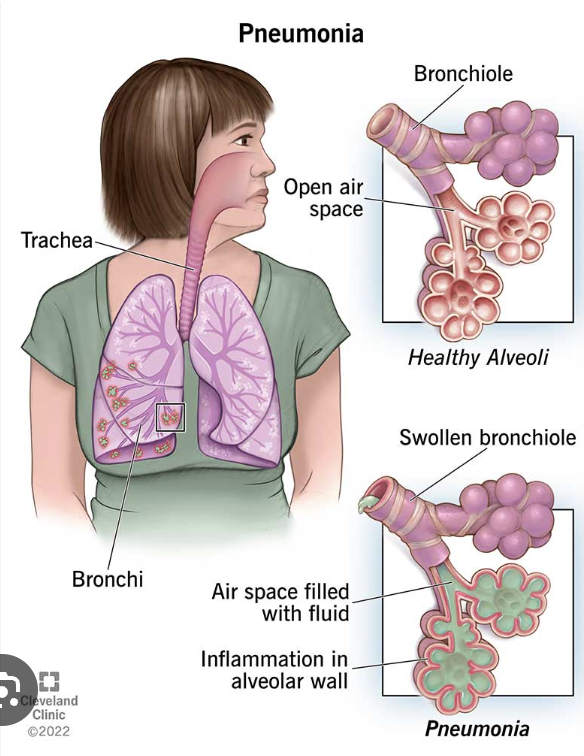
Pneumonia
inflammation of lung parenchyma
inflammation leads alveoli to be filled with exudate instead of air —> pneumonia
Pneumonia is inflammation and fluid in your lungs caused by a bacterial, viral or fungal infection
Classification of Pneumonia according to
-location: nosocomial/community
-etiology: cause
-anatomical: area of lung affected
Location acquired
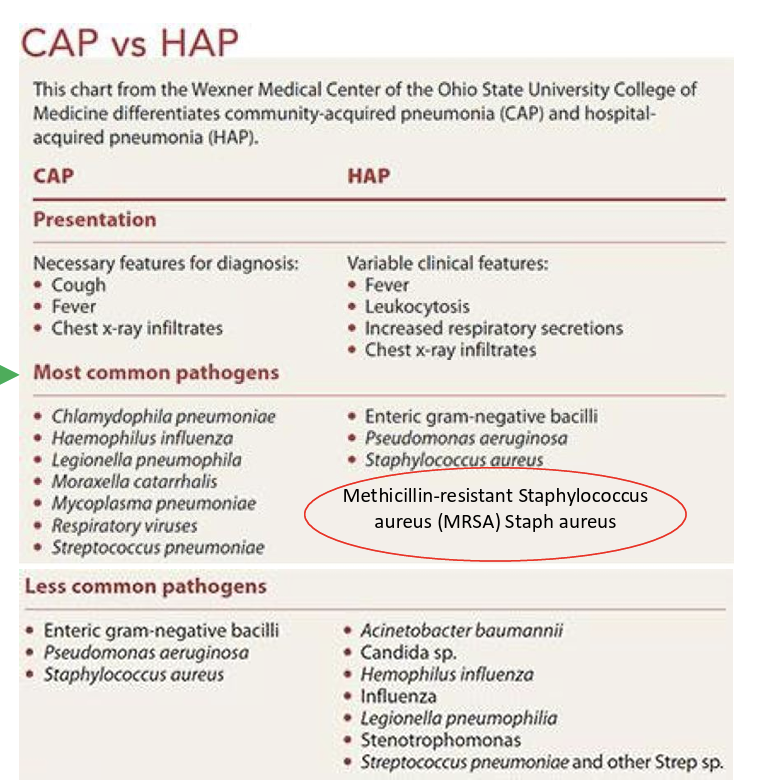
Community Acquired Pneumonia (CAP)
Nosocomial Pneumonia
Community Acquired Pneumonia (CAP)
Pneumonia acquired outside of hospitals or extended-care facilities
Nosocomial Pneumonia (HAP)
Hospital Acquired Pneumonia (HAP) (48 hrs after admission)
Ventilator Associated Pneumonia (VAP) (more than 48-72 hrs after endotracheal incubation)
More serious because of patients weakened immune system
Different microbes, highly virulent and antibiotic resistance
Anatomical Area of lung affected
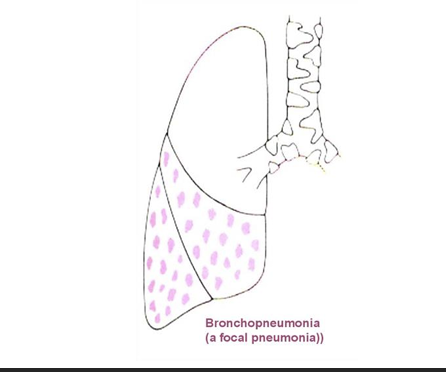
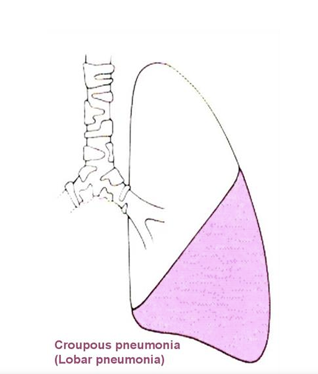
Bronchopneumonia
Lobar pneumonia
Bronchopneumonia
Infection of the terminal bronchioles that extends into the surrounding alveoli patchy consolidation of the lung.
Lobar pneumonia
Acute bacterial infection of part of a lobe, entire lobe or two lobes of both the lungs.
Etiology
Infectious causes
Non infectious causes
Non infectious causes
1. Toxins
2. Chemicals
infectious causes
1. Bacteria
2. Viruses (RSV, Parainfluenza)
3. Fungi (fungal pneumonia)
4. Parasites (parasitic pneumonia)
Bacteria that cause pneumonia
-gram positive
-gram negative
-atypical
Gram Positive:
Strep pneumoniae (pneumococcus)
Staph aureus (No vaccine)
Gam Negative:
Haemophilis influenza
Klebsiella pneumoniae (No vaccine)
E. coli
P. aeruginosa (No vaccine)
Atypical organisms
Mycoplasma pneumoniae
Legionella pneumophila (No vaccine)
Chlamydia pneumoniae
Coxiella brunetti
Streptococci Characteristics
-gram
-capsule
-motile
-spore
-catalase
-oxygen
-growth
-selective growth media
• Gram-positive bacterium
• Capsulated
• Non-motile
• Non-spore forming
• Catalase negative cocci (selective for identification)
• Facultative anaerobes
• Some are obligate (strict) anaerobes
• Grow in pairs or chains
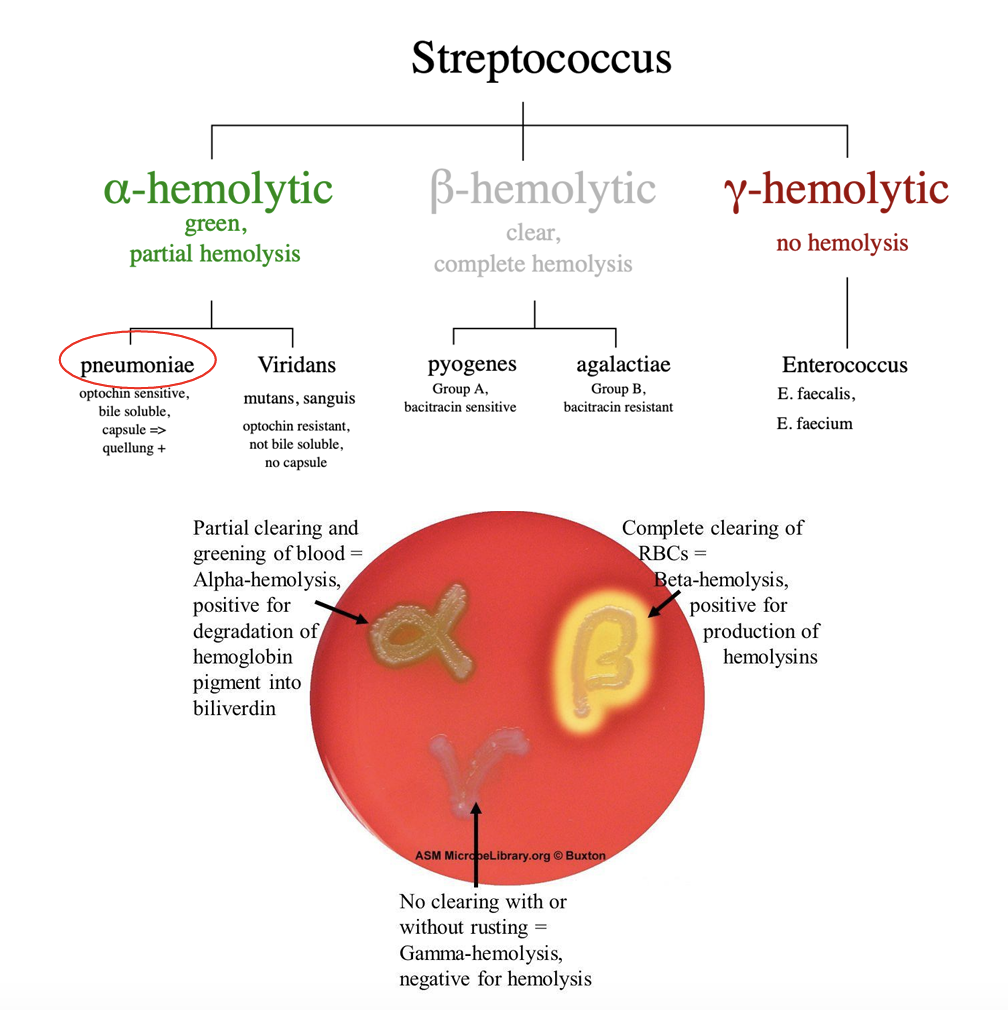
• Selective growth media (Blood agar) (Classification)
Streptococci hemolysis
alpha hemolytic = partial hemolysis
S. pneumoniae causes
Community-Acquired Pneumonia (most organism that causes it)
Otitis media
Sepsis
Meningitis
S. pneumoniae Capsular Polysaccharide (CPS)
-All virulent strains of Streptococcus pneumoniae are provided with a polysaccharide capsule.
-The physical removal of the pneumococcal capsule completely abolishes virulence. (Crucial Virulence factor)
-Resistance to phagocytosis and Antibiotics (rapid + incresing global problem)
-serological 90 types (vaccine challenge)
why are there many serological strains of S. pneumoniae Capsular Polysaccharide (CPS)
-Geographical and age differences in the distribution of the 90 different serotypes
-Ability of S pneumoniae to transfer capsular genes from one strain to another
Capsular Polysaccharide (CPS) functions
• The capsular polysaccharide is a key determinant of S. pneumoniae virulence:
1. Adhesion: promoting adhesion to epithelial surfaces
2. Protection: playing a crucial role in the escape from host defenses by complement- dependent and -independent phagocytosis
3. Resistance to Antibiotics
4. Highly immunogenic (specific antibody)
5. It is not toxic
6. Vaccine development
Pneumolysin (PLY)
- major exotoxin
-pore-forming toxins produced by more than 20 species of Gram positive bacteria, originally described as hemolysins
-Initially, the toxin binds to the cell membrane
- It then forms large pores (up to 30 nm in diameter) by the oligomerization toxin monomers
-Required for transmission
-Inhibits ciliary beating
-The main activity of PLY is its lytic activity (alpha/partial hemolysis)
what happens when s.pneumoniae number is sufficient
-any more can lead to competition —> autolysis occurs by autolysin (Lyt), partial hemolysis
types of autolysins
Autolysin A (main autolysin)
Autolysin C
Autolysin functions
autolysis
This will lead to the release of Ply, bacterial DNA and RNA
-The release of these factors directly contribute to host tissue damage.
-Also leads to stimulate host innate immune response —> inflammation
Choline-Binding Proteins (CBPs)
Repeat domains with choline in the pneumococcal cell wall (cholinec ontaining lipoteichoic acid)
• CBPs are anchored to the cell surface interaction via interaction with choline
• Several CBPs have been implicated in virulence such as:
• Pneumococcal surface protein A (PsPA)
• Pneumococcal surface protein C (PsPC)
Pneumococcal surface protein A (PsPA)
Lactoferrin plays an important part in innate immunity and inflammatory response
• PspA binds to lactoferrin
• Mutants lacking this protein have reduced bacterial virulence in an animal model
• Is an important virulence factor
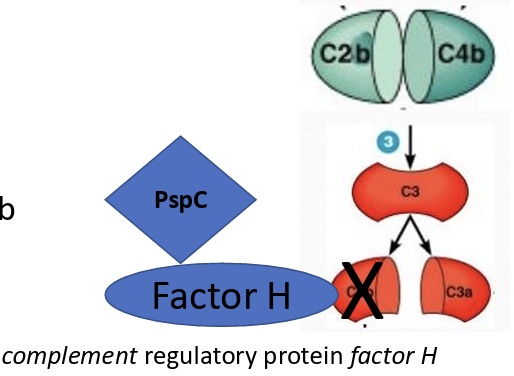
Pneumococcal surface protein C (PsPC)/ CbpA
PspC binds “factor H” → degrades C3b → evades C3b mediated phagocytosis
CBPs functions
PspA----Lactoferrin---resist innate immunity
PspC----Factor H----resist complement activation and complement-mediated phagocytosis
Other Virulence Factors
Others may contribute to the pathogenicity, but their role in virulence has not been established:
Various proteases Neuraminidase A (NanA), β-galactosidase (BgaA) (mucus degradation)
The pilus mediates binding of pneumococci to cells (first contact to cells)
It also stimulates proinflammatory cytokine production
Not all pneumococci have pili
Pili
Adhesion
Capsular Polysaccharide (CPS):
main virulence factor
vaccine development
Adhesion and protection
Ply
lytic activity, transmission, inhibit ciliary beating
Lyt:
release Ply and other factors
-initiate innate immunity
• CBPs:
Lactoferrin binding, Factor H binding, resist immunity, resist phagocytosis
Neuraminidase A (NanA), β-galactosidase (BgaA)
mucus degradation
First step Evasion of clearance
(LytA (autolysin)) facilitates release of Ply
(Ply) damages the epithelium and inhibits ciliary beating
(Neuraminidase A (NanA), β-galactosidase (BgaA)) degrade mucus and thereby inhibit mucociliary clearance and help adhesion
Second step Adherence to epithelium surface
The first contact with the epithelium and epithelial receptors (Pilus) then capsule (CPS)
Third step Endocytosis
S. pneumoniae induces its own endocytosis, which is followed by release of pneumococci at the basolateral surface
Fourth step Exocytosis and Hematogenous spread
Special host bacterial protein interaction would enable pneumococci to traverse the endothelium and enter the bloodstream.
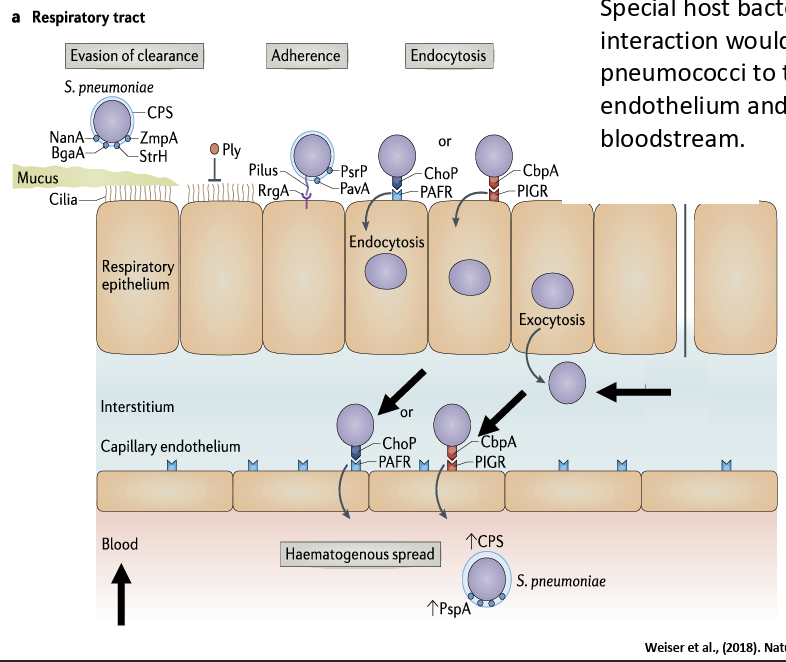
Molecular mechanisms of pneumococcal colonization of host surfaces
(LytA (autolysin)) facilitates release of Ply
(Ply) damages the epithelium and inhibits ciliary beating
(Neuraminidase A (NanA), β-galactosidase (BgaA)) degrade mucus and thereby inhibit mucociliary clearance and help adhesion
The first contact with the epithelium and epithelial receptors (Pilus) then capsule
Bind lactoferrin to acquire iron and blocks the antimicrobial effect (PspA)
PspC (CbpA) interacts with factor H interactions to facilitate adherence, block complement deposition and subsequent internalization of S. pneumoniae via cell glycosaminoglycans
?
Streptococcus pneumoniae colonizes the mucosa. Carriers can shed S. pneumoniae in nasal secretions and thereby transmit the bacterium (airborne and surface contact). Dissemination by aspiration leading to invasive diseases, such as pneumonia, meningitis and otitis media.
Antibiotic resistance (Superbug ) of s.pneumonia
S. pneumoniae is resistance to beta-lactams, macrolides, lincosamides, fluoroquinolones, tetracyclines, and trimethoprim-sulfamethoxazole (TMP-SMX).
•For example Between 20% and 40% of S. pneumoniae isolates are resistant to macrolides.
•Antibiotic resistance mechanisms include
1) alteration in target site (capsule is altered)
2) alteration in antibiotic transport (pathway blocked)
3) enzymatic inactivation of the antibiotic (degrade antibiotic)
Vaccination Pneumococcal vaccine (PCV)
-many capsule types
-pneumococcal conjugated vaccines has different types that has a different number of common serotypes of capsules
PCV7 protects against 7 types of pneumococcal bacteria
PCV10 protects against 10 types of pneumococcal bacteria
PCV13 protects against 13 types of pneumococcal bacteria
Vaccination Pneumococcal vaccine (PCV) indications
CDC recommends pneumococcal conjugate vaccine for all children younger than 2 years old, all adults 65 years or older, and people 2 through 64 years old with certain medical conditions.
Klebsiella pneumoniae location
ventilator associated pneumonia
Klebsiella pneumoniae characteristics
-gram
-oxygen
-shape
-motility
-capsule
• Gram negative.
• Facultative anaerobic.
• Rod shaped.
• Non-Motile.
• With large polysaccharide capsule
• Size: 2 µm by 0.5 µm
Klebsiella pneumoniae vs h.influenza
k. pneumonia has no vaccine and can grow on MacConkey agar
Klebsiella pneumoniae strains
Classic strains (c-KP)
hypervirulent strains (hv-KP)
Classic strains (c-KP)
Pneumonia
urinary tract infection
nosocomial infections
neonatal sepsis in immunocompromised patients
C-KP in neonates is associated mainly with
prematurity
the immaturity of the immune system
prolonged staying in the intensive care unit (ICU)
mechanical ventilation
using intravenous or urinary catheters
hypervirulent strains (hv-KP)
Liver abscesses
Meningitis
Endophthalmitis
In healthy adults
K. pneumoniae is a significant cause of respiratory (especially pneumonia) and urinary tract diseases (opportunist)
Virulence factors in classical and hypervirulent K. pneumoniae (Kp) strains.
1. Capsule
2. LPS
3. Fimbriae (types 1 & 3)
4. Siderophores.
-hypervirulent has thicker capsule —> more resistance to antibiotics and immune response
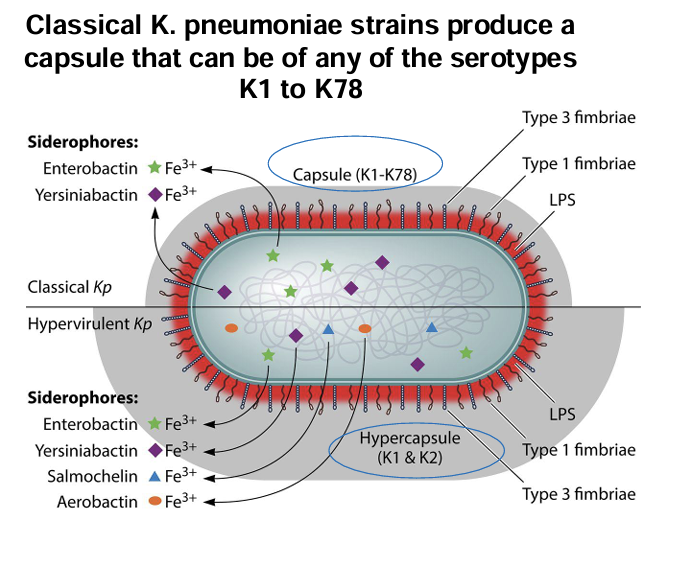
capsule types
Classical K. pneumoniae strains produce a capsule that can be of any of the serotypes K1 to K78
K1 and K2 are associated with increased pathogenicity (hypervirulent strains; hypercapsule)
capsule function
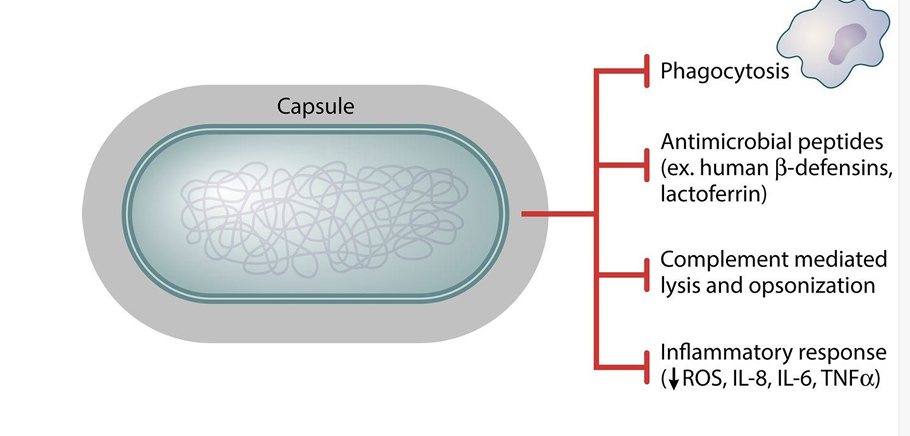
fimbriae function
Types 1 and 3 Fimbriae help in Invasion and biofilm formation
LPS function
LPS abrogates bacterial lysis by the complement
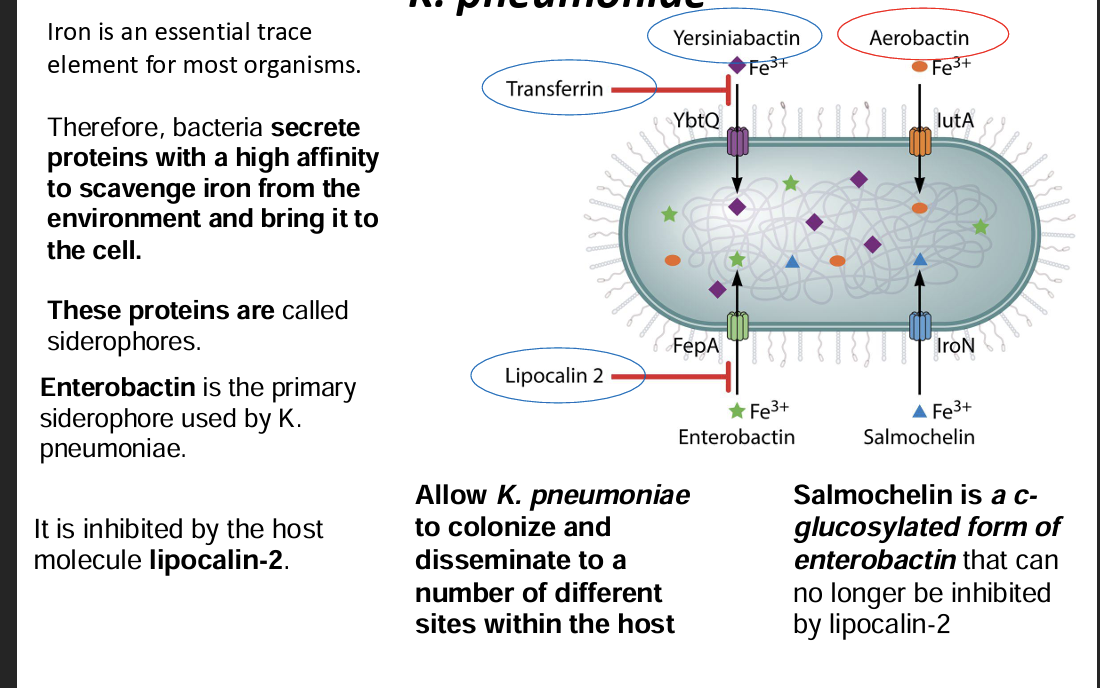
Siderophore function and MOA
bacteria secrete proteins with a high affinity to scavenge iron from the environment and bring it to the cell called siderophores. Enterobactin is the primary siderophore used by K. pneumoniae. It is inhibited by the host molecule lipocalin-2.
Treatment of klebsiella + prevention
1. First-Line Antibiotics (If Susceptible)
Beta-lactams (if susceptible)
Ceftriaxone (IV)
Cefotaxime (IV)
Piperacillin-tazobactam (IV)
2. Multidrug-Resistant (MDR) Strains
If the strain is Extended-Spectrum Beta-Lactamase (ESBL)-producing:
Carbapenems (e.g., meropenem, imipenem, ertapenem) are preferred.
If the strain is Carbapenem-Resistant Klebsiella pneumoniae (CRKP):
Colistin or polymyxin B (as a last resort due to toxicity)
Prevention: No approved vaccine
Epidemiology klebsiella
Humans are the primary reservoir for K. pneumoniae. Carrier rates of K. pneumoniae in the community range from 5 to 38 % in stool samples and 1 to 6 percent in the nasopharynx.
Legionella pneumophila mainly present in
Mainly present in drinking water (biofilms, mist at the flower sections).
• Inhalation of aerosolized water containing the bacteria
• Accidently swallow water containing Legionella into the lungs.
• Infect Amoeba.
Legionella pneumophila characteristics
gram
oxygen
shape
capsule
motility
• Gram negative.
• Strictly aerobic.
• Small size organism (0.2–0.8 μm).
• Rod shaped bacilli,
non-encapsulated
• Motile (flagella, pili, fimbriae).
Legionella pneumophilia pathogenesis
-mimicks ER, escapes macrophages and lysis cells in 14hrs
Dot/Icm type IV secretion system
Virulence factor (secrets effector proteins)
Proteins and transport vesicles (yellow spheres) are recruited to Legionella-containing vacuole (LCV), is transformed to ribosome-studded compartment that mimics host-cell rough endoplasmic reticulum (ER) and supports replication of L. pneumophila.
Eventually, the host cell is lysed, and L. pneumophila bacteria are released to infect other macrophages.
Treatment
Known to use macrolides, tetracyclines, and fluoroquinolones
no vaccine
Epidemiology
cause of sporadic and epidemic community-acquired pneumonia (CAP) in all age groups and in both healthy and immunosuppressed host
two clinical syndromes
Legionnaires disease and pontiac fever
Legionnaires disease
Legionnaires disease is an acute, serious, and sometimes lethal pneumonia,
Pontiac fever
Pontiac fever is generally a self-limited, nonpneumonic, influenza-like condition.
walking pneumonia?
Walking pneumonia is a mild case of pneumonia. When you have walking pneumonia, your symptoms may not be as severe or last as long as someone who has a more serious case of pneumonia. You probably won’t need bed rest or to stay in the hospital when you have walking pneumonia.
-mycoplasma pneumoniae
cause of walking pneumonia
It is often caused by a virus or the mycoplasma pneumoniae bacteria.
isn't severe enough to require bed rest or hospitalization.
mycoplasma pneumoniae bacteria. characteristics
-cell wall
-gram
-resistant
• Small size organism (1–2 μm long and 0.1–0.2 μm) wide.
• Gram stain (not visible ) M. pneumoniae lacks a cell wall and is fastidious; therefore, gram stain and cultures are not useful for the diagnosis of these organisms. negative.
• Non motile. Gram
• Lacks a rigid cell wall, allowing it to alter its size and shape
• Resistant to beta-lactams antimicrobial agents (penicillin) bcz no cell wall.
• It is predominantly considered a mucosal pathogen existing parasitically on the epithelial surface of its host
common causes of CAP
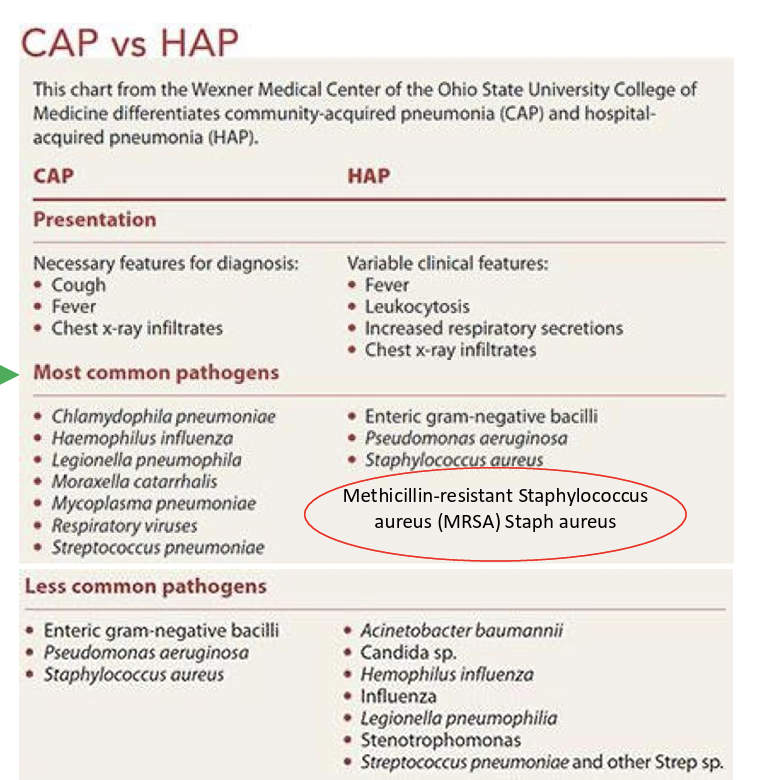
common causes of HAP