Unit 5 - Vestibular Examination
1/132
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
133 Terms
Vestibular System Function
Subjective sensation of motion: linear and angular accelerometer
Maintains body posture and balance
allowing us to stand, walk, and move with stability
Spatial orientation of the head in space
Senses linear and rotational movements of the head
Stabilizes eyes with head movements: Gaze stability
Spatial orientation of the body in space
Vestibular System Components
Peripheral Sensory Apparatus: located in the labyrinth
Central processor
Motor output
Vestibular System Components
Peripheral Sensory Apparatus: located in the labyrinth
Vestibule (sensory organ) and semi-circular canals
detect head movement and position
Cranial nerve VIII (Vestibulo-cochlear nerve)
send sensory information
Vestibular System Components
Central processor
Brainstem vestibular nuclei
Cerebellar pathways
interpret the incoming sensory input and coordinate appropriate motor responses
Vestibular System Components
Motor output
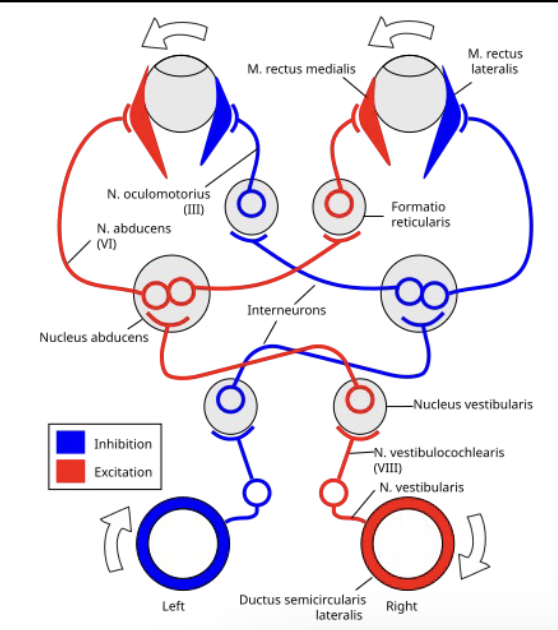
Vestibulo-ocular reflexes (VOR)
Vestibulo-collic reflexes (VCR)
Vestibulo-spinal reflexes (VSR)
highly integrated system essential for equilibrium, spatial orientation, and movement coordination
Vestibular System Components
Motor output —> Vestibulo-Ocular Reflex (VOR)
stabilizes vision during head movements
Vestibular System Components
Motor output —> Vestibulo-Collic Reflex (VCR)
stabilizes the head by activating the neck muscles
Vestibular System Components
Motor output —> Vestibulo-Spinal Reflex (VSR)
maintains the balance and upright posture by maintaining muscle tone in response to head movement
Vestibular System Components
Labyrinth
Bony labyrinth and membranous labyrinth
Perilymph circulates between the bony and membranous labyrinths (similar in composition to CSF)
Endolymph circulates within the membranous labyrinth (similar in composition to intracellular fluid)
Semi-circular canals: bony and membranous components
Three in each ear: Anterior (Superior), Posterior, and Horizontal
Canal are orthogonal (rt. angles) to each other
Vestibular System Components
Sensory organs: Contained within the membranous labyrinth
Three semicircular canals: Three in each ear
Two otolith organs: Utricle and Saccule
Vestibular System Components
Horizontal SCC
approximately 30º from horizontal
Vestibular System Components
Anterior and Posterior SCCs
in vertical planes
Vestibular System Components
two horizontal SCCs
lie in the same plane
Vestibular System Components
Left Anterior SCC and Right SCL
lie in the same plane
Vestibular System Components
SCC: Contain ampulla
dilated space at the end of each canal before it connects to the Utricle
Vestibular System Components
Cupula
a gel like bud within the ampulla that is embedded with sensory hair cells
Vestibular System Components
Utricle and Saccule
So called because they contain crystals of calcium carbonate
These organs make up the medial portion of the vestibule
Vestibular System Components
Utricle
horizontal translation of the head and head tilt
Vestibular System Components
Saccule
vertical translation of the head
Vestibular System Components
Labyrinth
part of the peripheral vestibular
consists of two main parts-- the bony labyrinth and the membranous labyrinth, and the perilymph, which is similar in composition to the cerebrospinal fluid, which circulates between the bony and membranous labyrinth
Inside the membranous labyrinth is the endolymph, a fluid that is more like intracellular fluid in composition
this unique ionic makeup is essential for generating electrical signals that travel to the brain
Vestibular System Components
Semicircular canals
both the part of bony and membranous labyrinth, and each ear consists of three canals-- the anterior superior, the posterior, and the horizontal canals
positioned approximately at right angles to each other, or orthogonal, allowing the detection of head movements in all three spatial planes
ensures that the vestibular system can accurately sense and respond to complex rotational movements of the head
Hair Cells
Endolymph within the SCC and otolith organs contain specialized hair cells: Type I and Type II
These hair cells have 50-100 stereocilia and a single taller kinocilium
highly sensitive to movement of the surrounding endolymph
During head movements, deflection of the hair bundle toward the kinocilium causes increase in firing rate and deflection away from kinocilium causes decrease in firing rate
This informs the brain about the direction of head movement
SCCs respond to angular acceleration and the otoliths to linear acceleration
Co-planar Pairing
When angular head motion occurs, the endolymph of the two sets of SCC is displaced in opposite directions resulting in increase in firing rate of one vestibular nerve and decrease in firing rate of the opposite vestibular nerve
The SCCs are linked in functional pairs
Left and Right horizontal SCC
Right Anterior SCC and Left Posterior SCC
Left Anterior SCC and Right Posterior SCC
Assist in compensation for sensory overload
The push-pull mechanism ensures redundancy of sensory input
The SCCs are linked in functional pairs
the horizontal canals
responsible for rotational movements, like shaking your head no
the vertical canal pairs
the right anterior and the left posterior, and the left anterior and right posterior semicircular canals
work together to detect head movements in the pitch and roll planes, like nodding yes or tilting your head side to side
Push-pull mechanism
helps to compensate for sensory overload
By having an excitatory and inhibitory signal, the brain receives a clear, unambiguous signal even during rapid head movements
ensures redundancy of sensory input
If one side signal is slightly compromised, the opposing signal is still providing valuable information, contributing to the remarkable resilience and accuracy of our balanced systems
Vestibulocochlear nerve (CN VIII)
carries the sensory information from the inner ear to the brain stem, helping you hear and maintain a sense of balance
two parts: The superior portion innervates the anterior and horizontal SCC and the utricle; and the inferior portion innervates the posterior SCC and the saccule
Nerve and Blood Supply
Labyrinthine artery is the main blood supply to the vestibular organs
It arises from the anterior inferior cerebellar artery (AICA) which arises from the Basilar artery
The labyrinthine artery splits into
anterior vestibular artery
supplies the anterior SCC, horizontal SCC, and the utricle
posterior vestibular artery
supplies the posterior SCC and the saccule
Central Processor
Input
Brainstem Vestibular nuclei
4 pairs —> act as a central hub, integrating signals not just from the vestibular organs but also from the visual and proprioceptive systems
crucial for a complete picture of a body's position in space
Cerebellum
fine-tunes movements, adapts responses, and learns from our experiences, ensuring that the balance reflexes are precise and appropriate for the task at hand
Central Processor
Output
VOR
VSR
VCR
Vestibular Nuclei
Lateral/Deiter’s Nucleus
Helps maintain posture through the vesitbulospinal reflexes
sends signals down to the spinal cord to control the muscles of the trunk and limbs
This is how our body automatically adjusts to keep you from falling when you encounter uneven ground or experience unexpected movements
Vestibular Nuclei
Medial and Superior Nucleus
Coordinates eye, head and neck movements through the vestibulo-ocular reflex
the midline of the vermis of the cerebellum
maintain equilibrium during both static postures and dynamic movements
cerebellar flocculus is a central key player in adaptive control of VOR
Vestibular Nuclei
Inferior Nucleus
Integrates information from the cerebellum and other sensory systems (no primary outflow of its own)
Cerebellum
Midline (Vermis)
regulate balance and eye movements
Cerebellum
Cerebellar flocculus
adjust and maintains the vestibulo-ocular reflex (VOR)
Cerebellum
Lateral regions control muscles of the extremities
fine tunes movements and plays a central role in modulating various reflexes
Vestibulo-Ocular Reflex (VOR)
Function
Generate equal and opposite eye movements in response to head movements in order to stabilize gaze during head movements
Vestibulo-Ocular Reflex (VOR)
Extraocular muscles driven by the ocular motor nuclei
Single pair of SCCs connected predominantly to single pair of extraocular muscles
Types of movement: abduction/adduction, elevation/depression, torsion
Vestibulo-Ocular Reflex (VOR)
Abduction and adduction
for horizontal head turns
Vestibulo-Ocular Reflex (VOR)
Elevation and depression
for vertical head nods
Vestibulo-Ocular Reflex (VOR)
Torsion
for head tilt
Vestibulo-Ocular Reflex (VOR)
Connections
Labyrinth to Medial longitudinal fasciculus (MLF) and paramedian Pontine reticular formation connect to the Abducens nucleus (CN VI), Trochlear nucleus (CN IV) and Oculomotor nucleus (CN III)
Vestibulo-Spinal Reflex (VSR)
Connections to the anterior horn cells of the spinal cord
Vestibular input used to stabilize head and body in space for movement and stabilization
Maintains vertical alignment of the trunk
When head side flexes on one side, there is an extensor response on that side and flexor response on the opposite side
Vestibulo-Collic Reflex (VCR)
Activates neck muscles to stabilize head in space
Compensated for displacements of the head with gait
Medical Screening
Dizziness
During history ask questions that help differentiate between vestibular and non-vestibular related dizziness
Ask them to describe their dizziness
Does the room spin around? VERTIGO
Do you feel unsteady? DISEQUILIBRIUM
Do you feel LIGHTHEADED?
Do you feel faint? PRE-SYNCOPE
Alteration in thought? CONFUSION
Medical Screening
Categories of Dizziness
Vertigo (45-54%)
Disequilibrium (Up to 16%)
Pre-syncope (Up to 14%)
Light-headedness (10%)
Medical Screening
Categories of Dizziness —> Vertigo
False sense of motion, possibly spinning sensation
Medical Screening
Categories of Dizziness —> Disequilibrium
Off-balance or wobbly when walking or standing
Medical Screening
Categories of Dizziness —> Pre-syncope
Feeling of losing consciousness or blacking out
Medical Screening
Categories of Dizziness —> Light-headedness
Vague symptoms, possible feeling disconnected with the environment
Medical Screening
Dizziness: Peripheral
Sudden (Onset): Yes
Positional: Yes
Intensity: Severe
Nausea/Diaphoresis: Frequent
Nystagmus: Torsional/horizontal
Ear (hearing loss): Can be present
Duration: Paroxysmal
CNS signs: Absent
Medical Screening
Dizziness: Central
Sudden (Onset): Slow, gradual
Positional: No
Intensity: Ill defined
Nausea/Diaphoresis: Infrequent
Nystagmus: Vertical
Ear (hearing loss: Absent
Duration: Constant
CNS signs: Usually present
Medical Screening
Red Flags – Vestibular Screening
Symptom presentation: dizziness, vertigo, imbalance and visual disturbances (oscillopsia)
Differentiate between peripheral vs central vestibular pathologies
Rule out non-vestibular causes of dizziness/imbalance
Help plan out rehabilitation or medical intervention
Screening:
History and intake
Physical examination
Assessment – vascular, cervical and CNS
Medical Screening
Red Flags – Vestibular Screening
5 Ds
Diplopia: double vision
Dysarthria: slurred or difficult speech
Dysphagia: difficulty swallowing
Dysmetria: Incoordination or difficulty with accuracy of movements
Dizziness: severe, sudden onset or atypical presentation
Others: numbness, weakness, severe headaches, loss of consciousness, new hearing loss/tinnitus
Medical Screening
Cervical Integrity Testing
To rule out cervical spine instability, injury, or arterial dissection that could mimic vestibular symptoms
Essential when there is a history of head/neck trauma
Key testing:
Cervical ROM assessment
Palpation for tenderness and muscle spasm
Ligament stability tests
Neurologic screening: dermatomes, myotomes and reflexes
Signs of cervical instability: nystagmus, pupillary changes or ataxia with neck movements
Medical Screening
Vascular Integrity: Seated Vertebral Artery Testing
To screen for potential compromise of the vertebral basilar artery system which supplies the brainstem and cerebellum
Performed when patients have dizziness associated with neck movements
Assessment:
Patient is seated and examiner stabilizes trunk. Patient actively rotates the head to one side and then extends neck maximally, holding for 10 seconds in each position
Positive sign is reproduction of dizziness, nystagmus, diplopia, blurred vision, dysarthria or loss of consciousness
Caution: this test has low sensitivity to rule out the disorder
Medical Screening
CNS Integrity: Ocular Motor Exam- Nystagmus
Peripheral Origin
Nystagmus Direction
Primarily horizontal with a slight torsional component
Gaze-evoked Nystagmus
Does not change direction with gaze, nystagmus intensity increases when looking in direction of fast component
Removal of Visual Fixation
Increases
Medical Screening
CNS Integrity: Ocular Motor Exam- Nystagmus
Centrla Origin
Nystagmus Direction
Typically pure horizontal, vertical, or torsional
Gaze-evoked Nystagmus
Persistent and changes direction depending on direction of gaze
Removal of Visual Fixation
Does not change or decreases
Medical Screening
CNS Integrity: Ocular Motor Exam
Oculomotor Tests: Smooth Pursuit
Patient follows the examiner’s finger as the examiner moves the finger horizontally and vertically in a rhythmic manner
Test is performed with the target moving slowly (20 deg/sec) and at low frequency (<1 Hz)
Normal result is if the eyes track smoothly
Abnormal result when there are consistent saccadic intrusions with pursuit (saccadic or cogwheel) in either or both directions – suggestive of CNS disorder
Medical Screening
CNS Integrity: Ocular Motor Exam
Oculomotor Tests: VOR cancellation
The examiner grasps the patient’s head and oscillates the patient’s head at 1Hz. The examiner moves with the patient so that the target (examiner’s nose) moves with the patient
This is a test of the central oculomotor pathways
Individuals (regardless of vestibular loss) should be able to maintain fixation on a point moving with them as they turn side to side
Medical Screening
CNS Integrity: Ocular Motor Exam
Oculomotor Tests: Saccade testing
extremely fast and very accurate eye movements used to shift gaze from on point to the other
The patient is cued to switch their gaze between 2 targets, typically the examiner’s nose and finger. Repeat in horizontal and vertical directions
Saccades should be conjugate (both eyes moving together)
Accuracy: accurate, hypometric (short of target), hypermetric (overshooting), multiple saccades
Velocity: very fast
Lesions: cerebellum, brainstem, neuromuscular junction
Medical Screening
CNS Integrity: Ocular Motor Exam
Oculomotor Tests: Vergence
The patient is cued to focus on the examiner’s fingertip, placed 24 inches in front of the bridge of the patient’s nose
Examiner’s finger is gradually brought in towards the bridge of the patient’s nose.
Patient is instructed to inform the examiner when the image doubles
Medical Screening
CNS Integrity: Ocular Motor Exam
VOR Testing: Slow head rotations
Patient’s head is oscillated back and forth horizontally at approximately 2Hz
Normal vestibular function: no problem
Bilateral vestibular loss: Corrective saccades with head rotation in both directions
Acute unilateral vestibular loss: corrective saccades occurring with head rotation to the side of decreased function
Medical Screening
CNS Integrity: Ocular Motor Exam
VOR Testing: Head thrust test (HTT)
Patient’s head is suddenly and rapidly rotated through a small range (15 – 30 degrees) then stopped
Patient is asked to maintain fixation on a visual target
Repeat on both sides: unpredictable in terms of timing and direction
Normal: no problem with visual fixation
BVL: corrective saccades with both sides head thrust
UVL: corrective saccades with head rotation to the side of decreased function
Medical Screening
CNS Integrity: Ocular Motor Exam
VOR Testing: Dynamic Visual Acuity
Patient reads the lowest line possible with the head stationary, and then they read the lowest line possible with head rotations side to side at 2Hz
Normal: 2 line or less difference between static and dynamic visual acuity
Abnormal: 3 line or greater difference suggests vestibular deficit
DVA will improve with central compensation
Medical Screening
CNS Integrity: Ocular Motor Exam
Head Shaking Nystagmus
Performed with eyes closed. The patient’s head is oscillated horizontally for 20 cycles. Eyes are opened just prior to stopping the head shaking
Look for post head-shaking nystagmus
Unilateral Peripheral Vestibular Loss: Horizontal nystagmus with nystagmus beating to the more active side
Central Vestibular Disorder: Vertical nystagmus
Purpose of the Subjective Examination
Establish rapport and gather detailed information
Screen for red flags and non-vestibular causes of dizziness
Identify patterns to support clinical reasoning
Guide selection of objective tests and initial interventions
Generate clinical hypotheses
Determine goals and monitor progress
Current Patient Medical History: Tempo, Symptoms, Circumstances
Onset: sudden, gradual?
Duration: seconds, minutes, hours, days, constant?
Frequency: single episode, intermittent, constant?
Current Patient Medical History: Description of Symptoms
Vertigo: spinning sensation
Dizziness: lightheadedness, unsteadiness, disequilibrium?
Oscillopsia: bouncing vision?
Current Patient Medical History: Circumstances
Provoking Factors: Specific head positions, rapid movements, environmental (busy stores)?
Alleviating Factors: Rest, specific positions, medication?
Associated Symptoms: Nausea, vomiting, headache, hearing loss, tinnitus, ear fullness, neurological symptoms (5 D's)?
Stable Symptoms
Symptoms are consistent in nature and intensity
Often associated with a fixed lesion or compensation process
Predictable triggers, predictable duration
Example: Chronic unsteadiness after initial acute phase of vestibular neuritis
Unstable Symptoms
Symptoms are fluctuating in nature, intensity, or frequency
Often suggests an active disease process or episodic disorder
Unpredictable onset, variable duration
Example: Meniere's disease, Vestibular Migraine
Management Categories Overview
BPPV
triggered by head position (rolling in bed, looking up); treat with repositioning maneuvers
Management Categories Overview
Adaptation
Stable unilateral vestibular hypofunction, for reduced VOR; treat with gaze stability exercises (VOR X1, VOR X2)
Management Categories Overview
Substitution
When adaptation is insufficient or with bilateral vestibular loss, rely on other sensory systems; treat with balance training, visual and head/eye strategies
Management Categories Overview
Habituation
symptom provocation by specific movements; reduce motion sensitivity
Management Categories Overview
Balance
disequilibrium and unsteadiness; address postural instability
Assessment of Dizziness
Visual Analog Scale (VAS) for Dizziness
0 (no dizziness) to 10 (worst imaginable dizziness)
Used for current dizziness intensity or during a typical episode
Provides a simple, quantifiable measure of subjective intensity
Assessment of Dizziness
Dizziness Handicap Inventory (DHI)
25-item self-report questionnaire
Quantifies the perceived handicap imposed by dizziness in three domains: Functional, Emotional, and Physical
Scoring: 0-100, where higher scores indicate greater perceived handicap
Tracks progress and identifies areas of greatest patient concern
Pharmacological History
Ask about:
Vestibular suppressants
Antiemetics
Ototoxic medications
Consider timing and dosage of medications
antihypertensives or sedatives can contribute to dizziness through effects like orthostatic hypotension or general sedatio
Watch for masking of symptoms
Developing a Clinical Hypothesis
Acute
sudden onset, constant symptoms (e.g., vestibular neuritis, stroke)
Developing a Clinical Hypothesis
Chronic Constant
gradual onset, persistent symptoms (e.g., uncompensated, unilateral vestibular hypofunction or bilateral vestibular loss)
Developing a Clinical Hypothesis
Chronic Episodic
recurrent episodes, intermittent attacks (e.g., BPPV, vestibular migraine, Meniere’s disease)
Benign Paroxysmal Positional Vertigo (BPPV)
Caused by displaced otoconia (calcium carbonate crystals) from the utricle into one of the semicircular canals
Most commonly affects the posterior canal
Triggered by changes in head position relative to gravity
Characterized by brief episodes of vertigo, usually lasting < 60 seconds
No hearing loss or tinnitus
Benign Paroxysmal Positional Vertigo (BPPV)
Core mechanism
tiny calcium carbonate crystals called otoconia, which normally reside in the utricle. For various reasons, these crystals can become dislodged and fall into one of the semicircular canals.
When you then move your head in a specific position, these rogue crystals shift, causing the fluid within the canal to move abnormally, leading to that brief, intense spinning sensation
Benign Paroxysmal Positional Vertigo (BPPV)
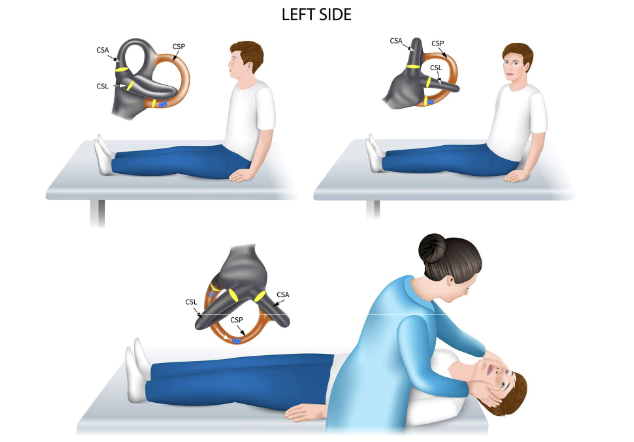
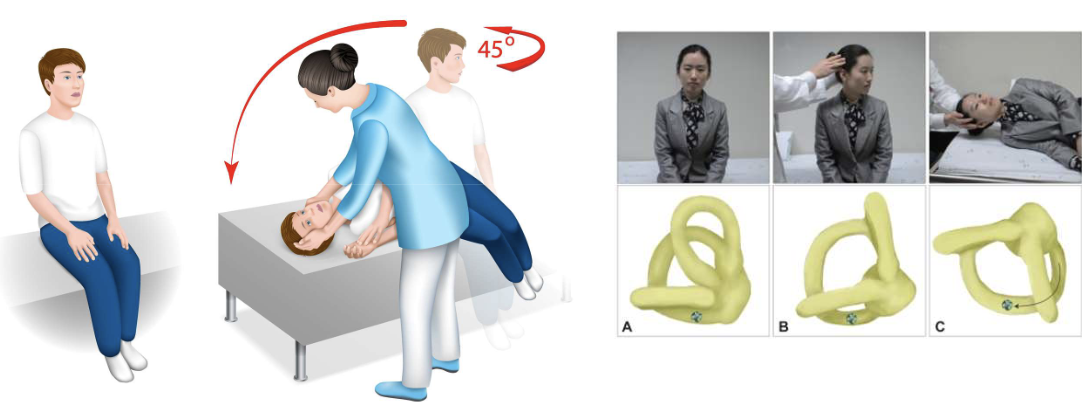
Dix-Hallpike Test: Purpose and Procedure
Patient’s head is turned 45˚ horizontally while the patient is in sitting position
The patient then quickly lies down with head hanging over the edge of the treatment table approximately 30˚ below horizontal
Observe in this position for at least 30-60 sec
The patient is brought back to sitting
Repeat the test on the other side
This places the posterior canal on the downside ear in the plane of the pull of gravity. The debris adhering to the cupula, or free floating in the canal, will shift down, resulting in vertigo and nystagmus
Benign Paroxysmal Positional Vertigo (BPPV)
Dix-Hallpike Test: Interpretation
Positive Test: Reproduction of vertigo and presence of characteristic nystagmus
Posterior Canal BPPV: Upbeating and torsional (rotary) nystagmus, beating towards the affected ear
Anterior Canal BPPV (Rare): Downbeating and torsional nystagmus, beating away from the affected ear
Benign Paroxysmal Positional Vertigo (BPPV)
Dix-Hallpike: Canalithiasis
most common, ~90-95% of cases
Latency
Vertigo/nystagmus typically begins after a 2-10 second delay after positioning
Duration
Symptoms last less than 60 seconds (usually 10-30 seconds)
Fatigability
Vertigo/nystagmus decreases with repeated positioning
Benign Paroxysmal Positional Vertigo (BPPV)
Dix-Hallpike: Cupulolithiasis
5-10% of cases
Latency
Vertigo/nystagmus begins immediately upon positioning
Duration
Symptoms last longer than 60 seconds (can be very prolonged)
Fatigability
Vertigo/nystagmus does not decrease with repeated positioning
Benign Paroxysmal Positional Vertigo (BPPV)
Dix-Hallpike Test
Nystagmus Features by Canal Affected: Posterior canal
Upbeating + torsional top pole beating toward downward ear
Benign Paroxysmal Positional Vertigo (BPPV)
Dix-Hallpike Test
Nystagmus Features by Canal Affected: Horizontal canal
Horizontal geotropic direction changing (right beating in head right position, left beating in head left position) or Horizontal apogeotropic direction changing (left beating in head right position, right beating in head left position)
Benign Paroxysmal Positional Vertigo (BPPV)
Dix-Hallpike Test
Nystagmus Features by Canal Affected: Anterior canal
Downbeating possibly with a slight torsional component
Benign Paroxysmal Positional Vertigo (BPPV)
Side Lying Test
This test can be a substitute for the Dix-Hallpike test if the patient cannot extend the head or cannot lie on their back
The patient sits on the side of the treatment table
The head is turned 45˚ to one side and the patient quickly lies down on the opposite side
This puts the posterior canal of the downside ear in the plane of the pull of gravity
The debris adhering to the cupula or free-floating in the canal will shift down
This results in vertigo and nystagmus
Sit the patient up and test the opposite side
Benign Paroxysmal Positional Vertigo (BPPV)
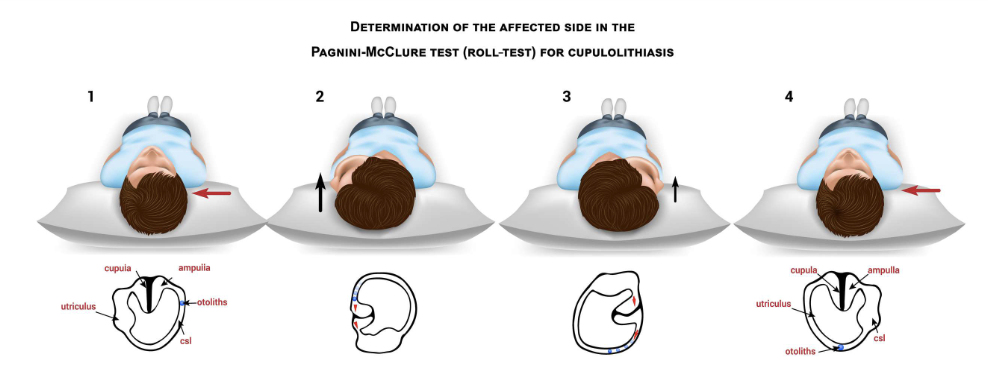
Roll Test: Purpose and Procedure
Patient lies supine with head elevated 20-30 degrees (Head elevation helps align the horizontal canal in the horizontal plane for optimal testing)
Rapidly rotate head 90 degrees to one side, observing eyes for nystagmus and asking about vertigo. Hold for 30-60 seconds.
Return head to center
Rapidly rotate head 90 degrees to the opposite side, observing eyes for nystagmus and asking about vertigo. Hold for 30-60 seconds
Benign Paroxysmal Positional Vertigo (BPPV)
Roll Test: Interpretation
Positive Test: Reproduction of vertigo and presence of characteristic nystagmus
Horizontal Canal BPPV: Purely horizontal nystagmus (no vertical or torsional component)
Geotropic Nystagmus: Beats towards the ground (Indicates canalithiasis on that side)
Apogeotropic Nystagmus: Beats away from the ground (Indicates cupulolithiasis on that side)
Benign Paroxysmal Positional Vertigo (BPPV)
Roll Test: Canalithiasis
most common
Latency
Vertigo/nystagmus typically begins after a 2-10 second delay after positioning
Duration
Symptoms last less than 60 seconds
Side
Nystagmus is stronger and lasts longer when turning to the affected side
Nystagmus
Geotropic (toward the ground)
Benign Paroxysmal Positional Vertigo (BPPV)
Roll Test: Cupulolithiasis
least common
Latency
No Latency, Vertigo/nystagmus begins immediately upon positioning
Duration
Symptoms last longer than 60 seconds
Side
Nystagmus is stronger and lasts longer when turning to the unaffected side
Nystagmus
Apogeotropic (away from the ground)
ICF Framework Applied to BPPV
Health condition: Benign Paroxysmal Positional Vertigo (BPPV)
Body Functions & Structures:
Dizziness/vertigo
Nystagmus
Altered gaze stability, balance, and postural control
Activity Limitations:
Difficulty with bending over, lying down, rolling in bed
Problems with walking in low light or crowded environments
Participation Restrictions:
Fear of falling
Avoidance of daily activities, work, or social events
Environmental/Personal Factors:
Age, co-existing anxiety, home setup, caregiver availability
Lighting, uneven surfaces, crowded spaces
Unilateral Vestibular Hypofunction (UVH): Clinical Presentation
Dysfunction in one labyrinth or vestibular nerve
Common causes: vestibular neuritis, labyrinthitis, acoustic neuroma, stroke
Symptoms: vertigo (severe), gaze instability, imbalance, nausea, nystagmus
Binilateral Vestibular Hypofunction (BVH): Clinical Presentation
Loss of vestibular function on both sides
Common causes: ototoxicity, autoimmune disease, idiopathic
Symptoms: oscillopsia, severe balance impairment, minimal vertigo
Impact and compensation
Unilateral Vestibular Hypofunction
Over time, the central nervous system compensates for the asymmetry, leading to a reduction in static symptoms (vertigo, nausea) but persistent dynamic symptoms (imbalance, gaze instability during head movement)