PTE 732: electrical modalities
1/141
Earn XP
Description and Tags
basic principles of electricity, NVC, EMG, iontophoresis, HPVC, and pictures!
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
142 Terms
what are some examples of contraindications for using electricity with treatment?
patients with cardiac pacemakers, implantable defibrillator, or unstable arrhythmia
patients with venous or arterial thrombosis or thrombophlebitis in treatment area
pregnant patients
using e-stim with pregnant patients is usually frowned upon, but what is one exceptional circumstance?
can use e-stim from pain relief during labor and delivery
what is one area where e-stim/electrodes should never be placed?
over the carotid sinus
list some examples of precautions when using e-stim.
cardiac disease
impaired cognition and sensation
malignant tumors or any cancer
areas of skin irritation or open wounds
electrical current
the flow of charged particles
in the human body or electrolytic solutions, it is the flow of ions
electrical charge
matter has either no net charge (electrically neutral) or is negatively or positively charged
charge = Q
charge density= Q/cm²
T or F: a neutral body becomes charged by gaining or losing an electron (e-).
T
what are the three “rules'“ for electric charges?
like charges repel, opposite charges attract
charge can be transferred
charge cannot be created nor destroyed
ions
elements with either an excess or a deficiency of electrons
cations: pos
anions: neg
polarity
indicates relative charge
anode: pos
cathode: neg
current
rate of flow of charged particles past a specific point in a specific direction
T or F: positive ions move towards anodes and negative ions move towards cathodes.
F: positive ions → cathodes; negative ions→ anodes
voltage
the force resulting from an accumulation of electrons at one point in an electrical circuit, usually corresponds to a deficit of electrons at another point in the circuit (electrical potential difference)
ampere
unit of measurement that indicates rate of electric current flow
resistance (aka impedance)
opposition to the flow of charged particles
higher frequency of stimulation = lower resistance/impedance of tissues
what biological tissues are poor conductors of current flow?
skin
fat
bone (poorest)
what biological tissues are good conductors of current flow?
blood
muscle
nerve (best)
conductance
relative ease at which electrons or ions are allowed to move through the conductor
capacitance
property that allows the system to store charge
what are the four circuits of electrical circuits?
closed: electrons are flowing
open: current flow stops
series: only one path
parallel: two or more routes exist
direct current (DC)
continuous or uninterrupted uni-directional flow of charged particles at least 1 second long
used with iontophoresis, wound healing, and stimulation of denervated muscle
alternating current (AC)
continuous or uninterrupted bi-directional flow of charged particles that must last at least 1 second and must cross the isoelectric line at least twice in 1 second
used for stimulation of innervated muscle
pulsed current
interruption of either uni- or bi-direcitonal flow of charged particles
T or F: pulsed current is the most commonly used form of electricity in clinical applications and can be used for any stimulation treatment.
F; cannot use with iontophoresis
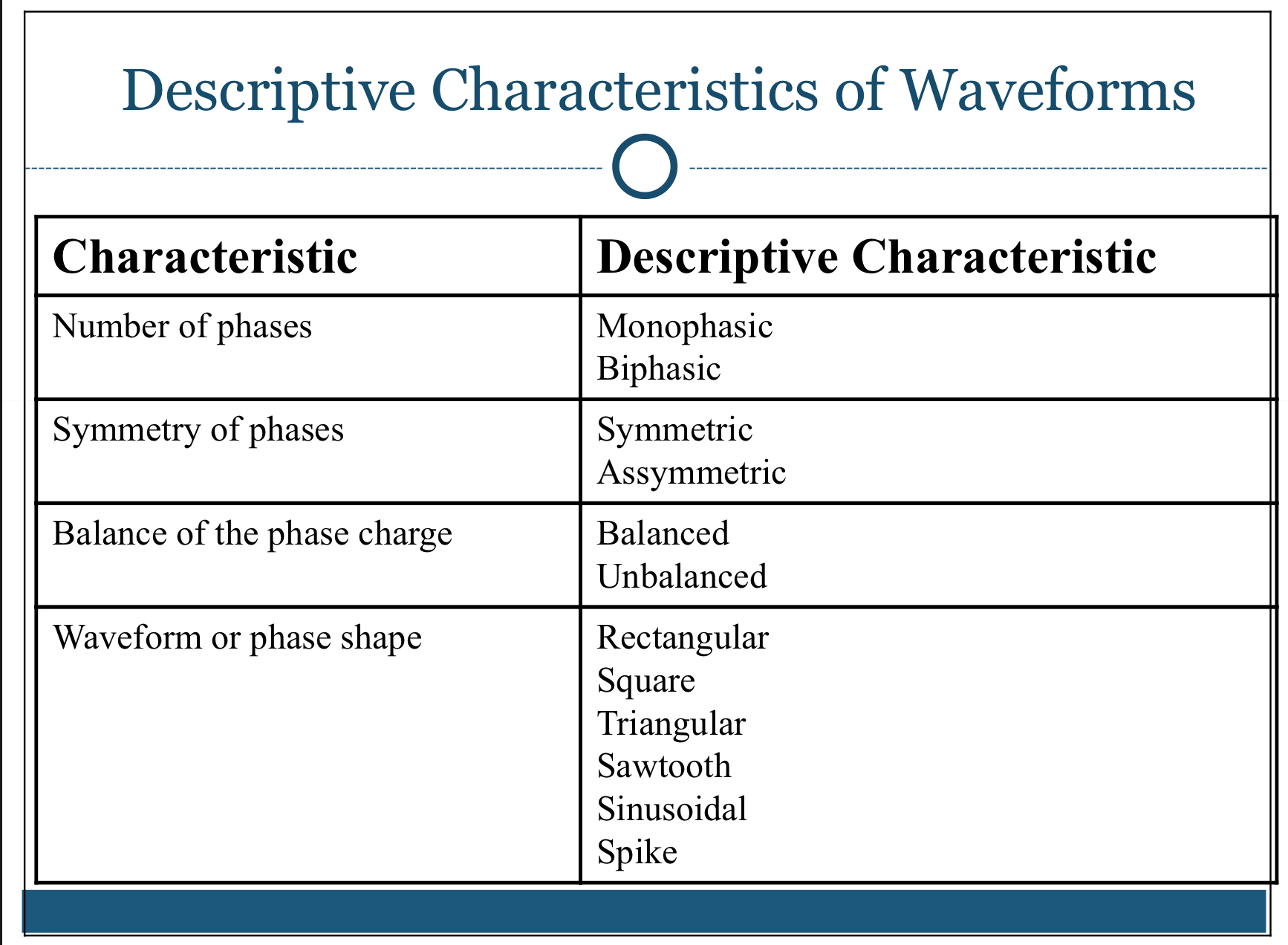
characteristics of waveforms chart
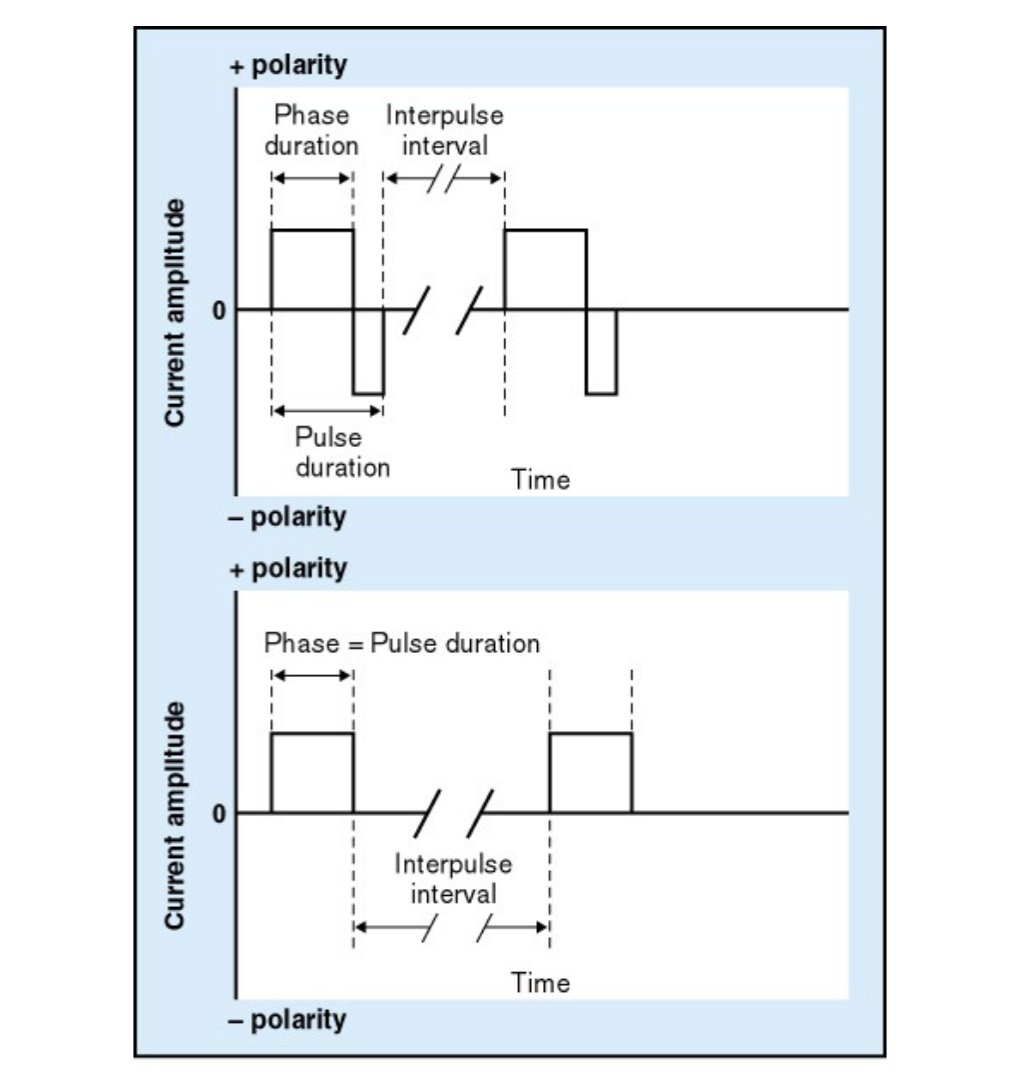
amplitude vs polarity chart
is there a thermal effect with e-stim?
no; cannot measure it
T or F: patients receiving unidirectional flow of DC may experience skin irritation in the form of white dots/blisters.
T
what’s the difference between positive and negative poles? (galvanic effect)
positive poles: the negatively charged particles cause an acidic reaction (Cl-)
negative poles: the positively charged particles cause an alkaline reaction (Na+)
which current would result in practical elimination of chemical effects at the tissue level?
pulsed current
electrical stimulation may alter the body’s physiology on four levels, what are they?
cellular
tissue
segmental
systemic
what magnitude would a patient feel a tingling sensation and muscle contraction?
1-15 mA
what magnitude would a patient feel a painful electrical shock?
15-100 mA
what magnitude would a patient experience a cardiac or respiratory arrest?
100-200 mA
T or F: it takes little intensity (small pulse duration) to stimulate sensory and motor nerves.
T
sensory is felt first, followed by motor activity
two points are needed for stimulation when testing the nerve conduction velocity. why?
to note time period of the stimulation passing over/through the neuromuslcar junction
how does electrical stimulation modulate pain?
it either activates the gate control or endogenous opiate mechanisms
“conventional” mode is also called ____ ____.
“high rate”
generally characterized by a high-rate frequency and low amplitude
some research indicates that frequencies around ___ may be optimal for pain relief.
60 Hz (pps)
describe conventional mode/high rate.
frequencies in the range of 10-100 pps
amplitude intensity that produces a comfortable cutaneous stimulation without a contraction
short pulse duration, usually 50-100 microseconds
describe low rate mode.
pulse rates (frequencies) below 10, usually 1-4 pps
pulse duration of 100-300 microseconds
amplitude adjusted to produce visibly strong and rhythmical muscle contractions
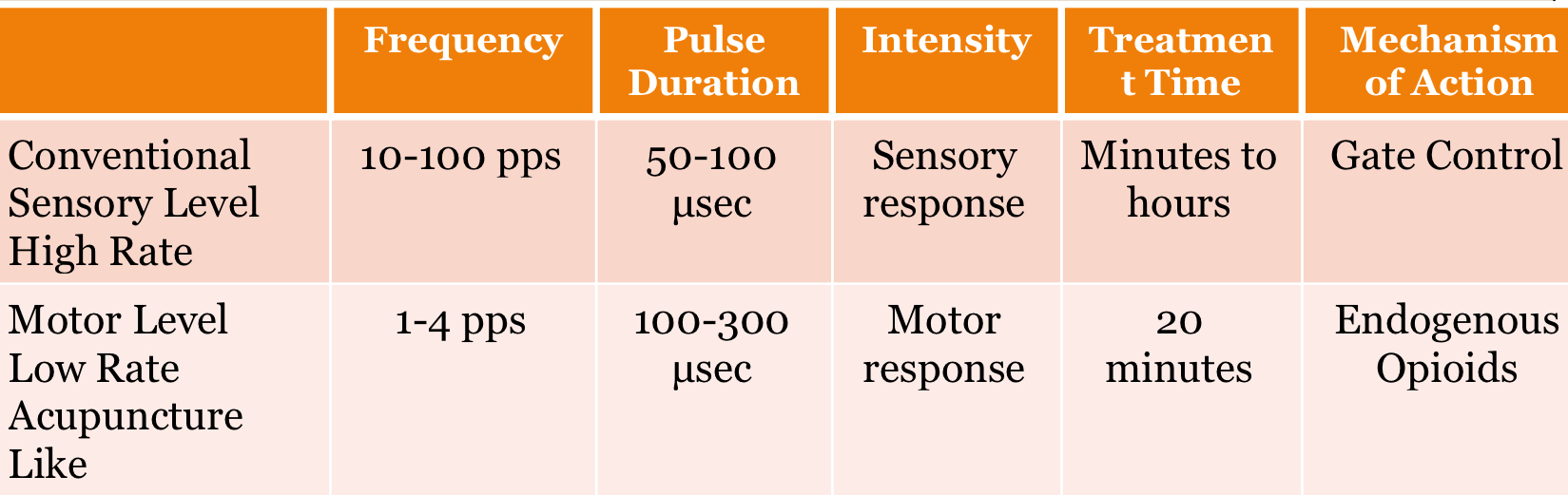
high rate vs low rate chart
when using low rate mode, ____ frequencies tend to work on the gate control mechanism, while ___ frequencies tend to cause endorphin release via the central biasing theory
higher
lower
to help with neuromuscular dysfunction affecting innervated musculature, what two components must a NMES and FES machine need?
ramp up and down time frame
time on/off option
can e-stim enhance circulation?
yes!
how does e-stim enhance micro-circulation and protein synthesis thus accelerating the healing process of wounds?
aiding with circulation via motor and sensory stimulation
muscle contracts = better blood flow (like a pump)
where should a therapist place the 2 electrodes on a patient?
positioned relative to a localized site of painful trauma or inflammation so that stimulation occurs primarily via cutaneous afferents
what are the four electrode placement options (when using 2 electrodes)?
just proximal to the site of pain (good for very distal UE or LE sites)
just outside the proximal and distal margins of the painful region
one on the painful region and the other adjacent to the spine over related spinal root
just distal to the site of pain
T or F: specific peripheral nerves that innervate a painful region can be targeted for stimulation, especially where located superficially.
T
place along nerve pathway
what stimulation may be more effective as the electrodes are placed over motor points since a motor response is a desired outcome when testing peripheral nerves?
“low rate”
can electrodes by placed on trigger points?
they may be positioned relative to the trigger points or relative to its zone of referred pain
some research suggests that high amplitude stimulation that produces a contraction can aggravate the trigger points
T or F: the current density is directly proportional to the electrode surface area, meaning large impedance= large electrodes.
F; inversely proportional
larger electrodes = lower impedance (greater current flow)
what are the common uses of electrical stimulation?
pain control
muscle re-education and strengthening
funcitonal electrical stimulation
edema
wound healing
list 5 indications for electrical stimulation for pain control.
rheumatoid arthritis and osteoarthritis
musculoskeletal pain
post-surgical pain
labor and post-labor pain
post-amputation pain
TENS
transcutaneous electrical nerve stimulation
FES
functional electrical stimulation
describe the treatment parameters of Russian stimulation.
carrier frequency of 2500 Hz
burst frequency of 50 pps
intensity to tetanic (sustained) contraction
what are the two qualifications for e-stim to be considered high voltage stimulation (HPVC)?
must have twin peak monophasic currents
must have 100-150 volts
describe the parameters for high voltage stim (HPVC).
twin spikes with high amplitude (up to 500V)
short pulse duration at 50-200 microseconds
1-120 pps
does high volt have galvanic effects?
no only iontophoresis!
what are the varied uses for HVPC?
muscle re-education (requires 150V) to reduce muscle spasm
nerve stimulation (requires 150V)
edema reduction and tissue healing
pain control
T or F: high-voltage stimulation has a high peak, but a low average current provides deep penetration of a comfortable current.
T
HPVC has a physiological response that can be excitatory or non-excitatory. what’s the difference?
excitatory: peripheral nerve stimulation for pain modulation; promotes circulation, inhibits sympathetic nervous system, and endogenous vasodilation
non-excitatory: occurs at a cellular level: protein synthesis, mobilization of blood proteins
what are the precautions for HPVC?
may cause unwanted tension on muscle fibers
muscle fatigue if insufficient duty cycle
improper electrodes can cause burns
intense stim may result in spasm or soreness
what are the contraindications for HPVC?
cardiac disability
pacemakers and metal implants
pregnancy
menstruation
cancerous lesion
infection
nerve sensitivity
what is iontophoresis?
a modality that involves the administration of ionic therapeutic agents through the skin by the application of low level electrical current
what kind of current does iontophoresis utilize?
direct current (DC)
iontophoresis is known as an anesthetic (lidocaine), but it is most commonly used to _____ _______, especially when used as a physical therapy modality.
decrease inflammation (dexamethasone)
what are the three methods that iontophoresis works through?
heightened transport of charged solutes by electrical repulsion from the electrode
enhanced skin permeability due to flow of electrical current
altered transport of un-ionized molecules and large polar peptides via electro-osmosis
list a few examples of factors that influence transdermal delivery of iontophoresis.
pH of medication, current density, ionic strength of drug, drug concentration, molecular size, and method of current application (continuous or pulsed)
before starting any electrical stimulation treatment, we should warn the patient that he or she might experience _____ ______.
skin changes!
like red marks and tiny white bumps
what is the effective dosage for iontophoresis?
40-80 mA x minutes
1 mA = 40 mins
2 mA = 20 mins
4 mA = 10 mins
T or F: transport of drugs across skin is inversely proportional to molecular size, causing smaller peptides to be safer than larger peptides.
T
list some indications for using iontophoresis.
hyperhidrosis
plantar fasciitis
musculoskeletal inflammatory disorders
rheumatoid disorders
carpal tunnel syndrome
scar tissue
what are the contraindications for iontophoresis?
demand cardiac pacemaker or arrhythmias
placement of electrodes over carotid sinus
over venous or arterial thrombosis or thrombophlebitis
pregnancy
what are the precautions for iontophoresis?
cardiac disease
impaired mentation or impaired sensation
malignant tumor
skin irritation or open wounds
after using other physical agents
what are the three main side effects of iontophoresis?
erythema
itching/burning/tingling
minimal blistering
describe the galvanic effects of iontophoresis.
negative electrode = sodium hydroxide = alkaline reaction
positive electrode = hydrochloric acid = acidic reaction
what patient diagnoses can iontophoresis be used for?
inflammation
lateral epicondylitis
hyperhidrosis
anesthetic
glucose monitoring
what is biofeedback?
the use of electronic instrumentation to provide objective info (or feedback) to an individual about a physiologic function or response so that the individual becomes aware of his or her response
biofeedback monitors and measures 6 different responses. what are they?
EMG
EEG
blood pressure
heart rate
temperature
any visceral and vasomotor responses
T or F: biofeedback is a tool that clinicians can use to help patients learn new tasks or modify existing motor patterns by providing useful info to the clinician and patient.
T
what three questions are required for the patient to answer before applying and using biofeedback?
does the patient have a motor impairment that would suggest that the info provided by biofeedback would be of benefit?
do they have the ability for voluntary control?
are they motivated and cognitively aware?
why would a therapist use biofeedback?
muscle re-education
relaxation of muscle guarding
pain reduction
treatment of neurological conditions
what e-stim factors can we manipulate to make a patient’s experience more comfortable?
intensity
duration
frequency
your patient complains she is not feeling anything during e-stim. what are the possibilities for error?
didn’t properly clean the skin
cord is frayed or not plugged in
pulse duration is not long enough
intensity may not be “high” enough
frequency is not correctly set
stimulating at the wrong area
NVC or NCS
nerve conduction velocity
what information is obtained during NVC?
excitability and fatigability of PNS
nerve conduction time and velocity
amplitude and duration of action potential
what are the recording techniques and general considerations when using NCV?
securely fasten electrodes to subject with tape or straps
clearly mark points of stimulation
use metal measuring tape
cathode positioned toward active (recording) electrode
apply adequate stimulus to evoke a motor or sensory response
what must we subtract when using NVC?
the time it takes for the stimulus to cross the neuromuscular junction
what are the considerations for patient positioning?
consider patient’s comfort
easy accessibility of the extremity for examiner
positioning of nerve segment
T or F: for all techniques in the NIOSH manual, the cathode (negative pole) of the stimulating electrode is positioned toward the active electrode.
T
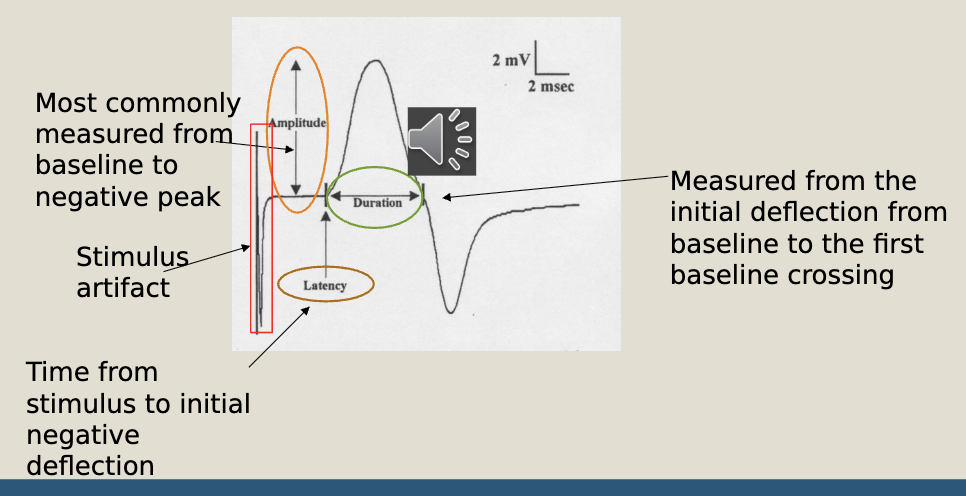
compound muscle action potential diagram
motor nerve conduction tests table
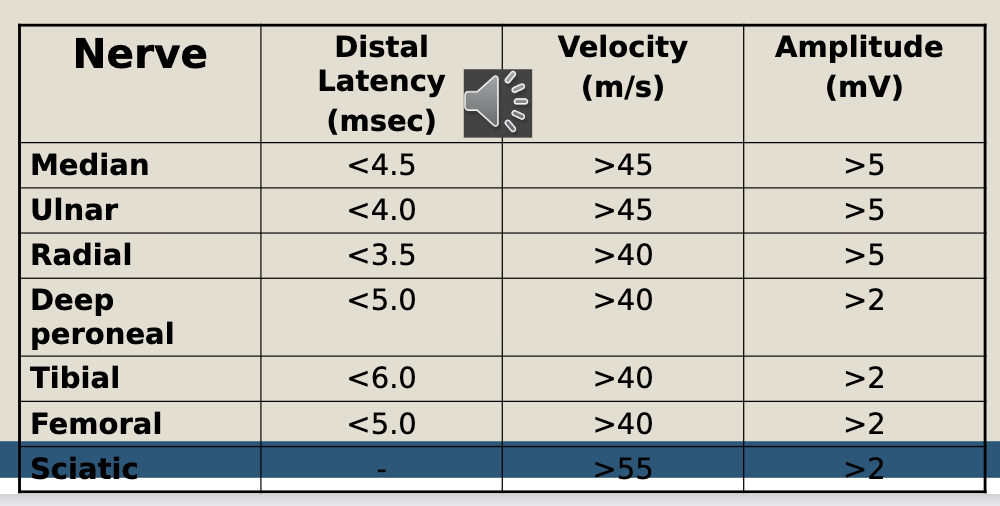
motor nerve conduction study results
T or F: when conducting sensory nerve tests, repeated testing of the same nerve gives no new info.
T
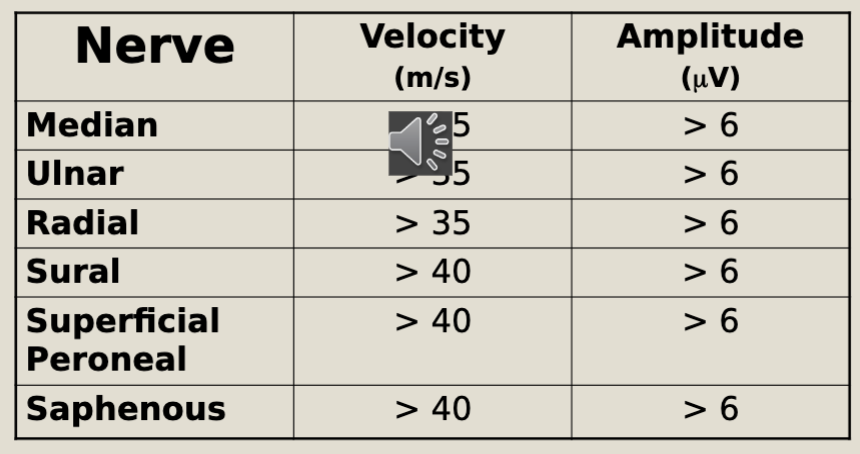
sensory nerve conduction tests table
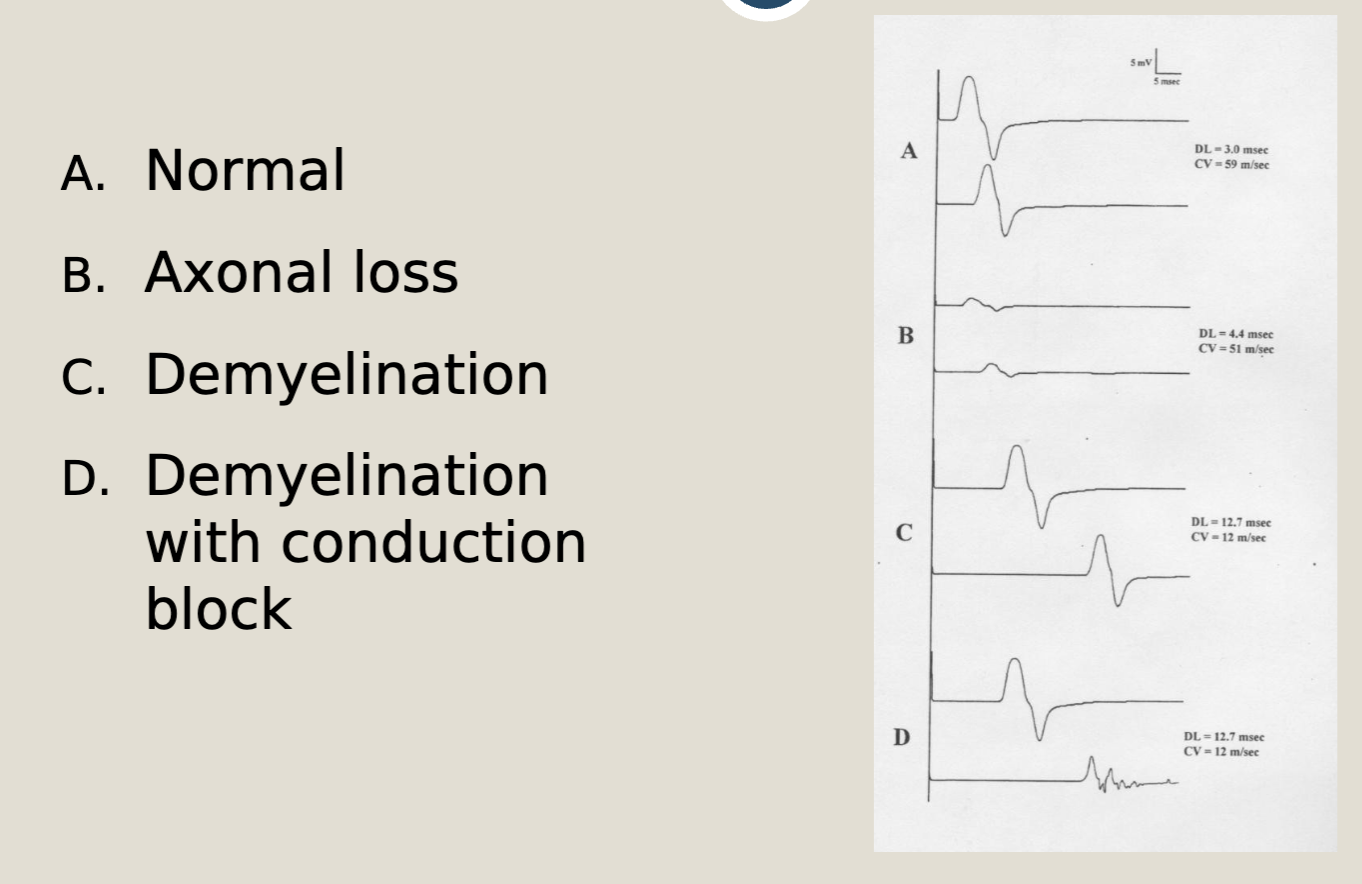
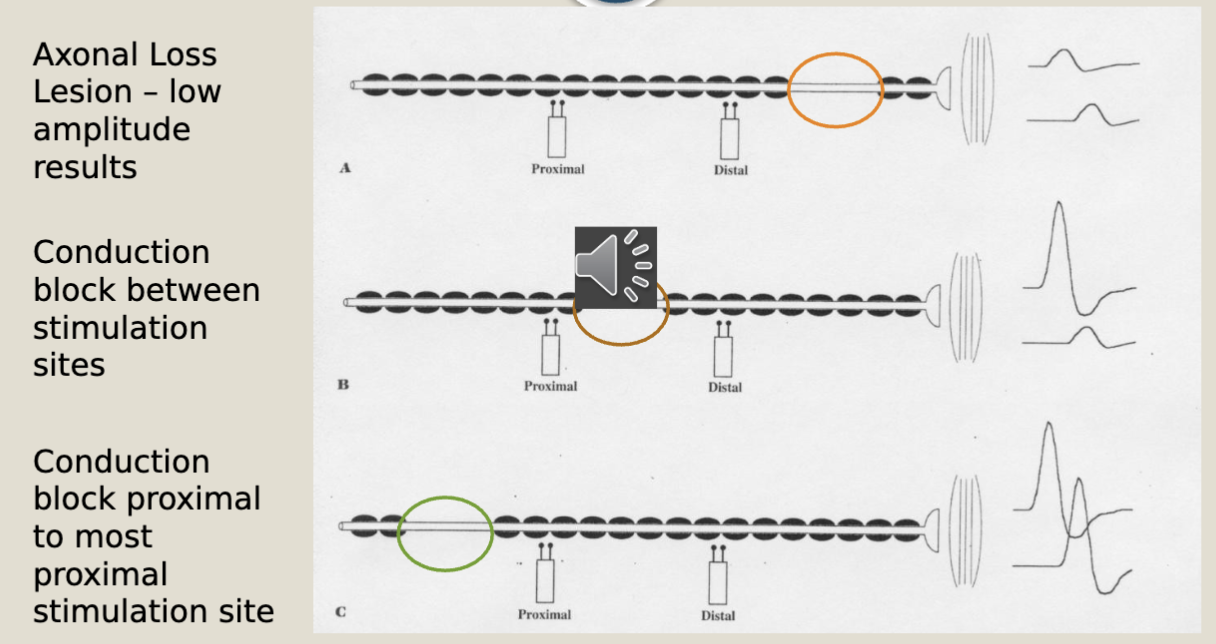
nerve conduction block possibilites (chart)
an antidromic study results in a _____ amplitude sensory nerve action potential (SNAP) whereas an orthodromic study results in a _____ amplitude SNAP.
higher
smaller
F-Wave
elicited by a supra-maximal stimulus of a peripheral nerve at a distal site; both orthodromic (to distal muscle) and antidromic (to anterior horn cell) responses
impulse is thought to reverberate