Furr and Reed Chapter 2: Cerebrospinal Fluid and the Blood-Brain Barrier
1/55
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
56 Terms
What is the blood CSF barrier made up of?
Choroid plexus and other tiny regions of the ventricles
What determines the composition of brain interstitial fluid?
Active transport of substance through the BBB
What determines the composition of the CSF?
Secretory processes through choroid plexus epithelia
What composes the BBB?
Capillary endothelial cells, basal lamina, pericytes, astroglia, and perivascular macrophages
What composes the blood CSF barrier?
Capillary endothelium, loose connective tissue, basal lamina, and ependymal cells
What portions of the CNS don’t have a BBB?
Portions of the hypothalamus, area postrema, and subfornical and subcommissural regions
How is glucose transported across the BBB?
By facilitated diffusion through the glucose transporter-1 (GLUT-1)
How can the integrity of the BBB be evaluated clinically?
Using the albumin quotient
Iatrogenic blood contamination of the CSF samples, intrathecal hemorrhage, or inflammation/traumatic disruption of the BBB will result in an elevated AQ
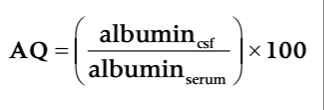
Normal Albumin Quotient
<2.1 for mature horses
1.8 ± 0.2 for foals
Immunologic Function of the Blood Brain Barrier
Inflammatory cytokines and endotoxin have been demonstrated to influence BBB endothelial cells by upregulating their expression of adhesion and MHC molecules
Leads to increased BBB permeability, formation of vasogenic edema, leukocyte extravasation, and vascular thrombosis
Pericytes contribute to microvascular reactivity, as well as being phagocytic, and express various adhesion molecules and MHC II receptors
Astrocytes interact with the endothelial cells and enhance their barrier function
Formation of CSF
Actively secreted by ependymal cells and choroid plexus
Majority is produced by the choroid plexus in the lateral ventricles
30-40% may be produced by the ependymal lining of the ventricles, the leptomeninges, and brain and spinal cord blood vessels
What is CSF production proportional to?
Production is directly proportional to the transport of sodium via a Na-K ATPase in the brush border of the choroidal epithelium and is independent of vascular hydrostatic pressure
What can alter the rate of CSF production?
Rate of CSF production can be altered by a variety of compounds
Carbonic anhydrate and Na-K ATPase inhibitors and hyperosmolality decrease production rate
Cholera toxin and adrenergic stimulation increase CSF production rate
Osmotic agents and hypertonic solutions such as mannitol and DMSO decrease CSF production in other species, effects unknown in horses
Where does CSF go after formation?
Following formation, CSF flows into the third and fourth ventricles and exits caudally through foramina in the fourth ventricle to enter the subarachnoid space
Pulsation of blood in the choroid plexus forces the CSF in a cranial to caudal flow
CSF is absorbed by collections of arachnoid villi in the dural sinuses or cerebral veins
When CSF pressure exceeds venous pressure, these villi act as a one-way ball valve forcing CSF flow to the venous sinus
What are the three physical components of the CNS that interact to generate intracranial pressure (ICP)?
Brain
Blood vascular component
CSF
What are the two major factors that determine ICP?
Arterial pressure
Intracranial venous pressure
Monro-Kellie Doctrine
Monro-Kellie doctrine - given that the total cranial volume is fixed, an increase in the volume of one component must be compensated for by a decrease in the volume of at least one of the other components, or an increase in pressure must result

Queckenstedt’s Test for Spinal Occlusion
Jugular occlusion should lead to an increase in the CSF pressure measured at the lumbar space, if this does not occur then spinal subarachonid blockage must exist
Queckenstedt's maneuver can be used as an aid during spinal fluid collection
What is ICP in awake standing horses?
2 ± 4 mmHg
What are lumbosacral CSF pressures highly correlated to?
Lumbosacral CSF pressures are highly correlated to lateral ventricle CSF pressure but specific values not reported
Does xylazine cause a change in CSF pressure?
No
Does hypercapnia increase CSF pressure?
Yes, markedly when the PaCO2 increased to 80 mmHg
ICP in Foals over the First 3 Days of Life
Ranged from 5.8-9.5 mmHg
What can cerebral edema be characterized as?
Cellular (cytotoxic)
Vasogenic
Interstitial
What characterizes cellular edema?
Cellular edema is characterized by swelling of all the cellular elements of the brain (neurons, glia, and endothelial cells) with an associated reduction on the volume of the brain extracellular fluid space
What causes cellular edema?
Results from a failure of the energy-dependent transmembrane sodium-potassium pumps which allows the accumulation of sodium, chloride, and water in the cell
Energy failure that causes Na-K pump failure also promotes excessive neuronal depolarization, reduced neurotransmitter reuptake, and increased intracellular calcium concentrations
End result is neuronal cell death
Associated with the clinical conditions of hypoxia and ischemia
E.g. hypoxic-ischemic encephalopathy of foals
Water intoxication can lead to cellular edema
What is vasogenic edema characterized by?
Vasogenic edema is characterized by increased permeability of brain capillary endothelial cells, with extravasation of macromolecules from the vasculature
What causes vasogenic edema?
Most commonly associated with tumor, trauma, abscess, infarction, lead intoxication, or severe ischemia
Features of vasogenic and cellular edema often coexist in a particular patient
Interstitial Edema
Interstitial edema is best observed in obstructive hydrocephalus
Results in transependymal movement of CSF with a subsequent accumulation of brain interstitial fluid
Pathogenesis of Vasogenic Cerebral Edema
Increased capillary permeability
ECF Composition in Vasogenic Cerebral Edema
Plasma filtrate with protein
Capillary Permeability with Vasogenic Cerebral Edema
Increased
Clinical Conditions Associated with Vasogenic Cerebral Edema
Trauma, infarct, abscess, hemorrhage
Pathogenesis of Cellular Cerebral Edema
Energy failure and cellular swelling
ECF Composition in Cellular Swelling
Water and sodium
Capillary Permeability in Cellular Cerebral Edema
Normal
Clinical Conditions Associated with Cellular Cerebral Edema
Ischemia, hypoxia hypoosmolarity
Pathogenesis of Hydrocephalic Cerebral Edema
CSF outflow obstruction and increased total brain fluid
ECF Composition in Hydrocephalic Cerebral Edema
Cerebrospinal fluid
Capillary Permeability in Hydrocephalic Cerebral Edema
Normal
When will slight turbidity of CSF be noted?
At a cell count above 400 cells/mm3
Tyndall’s Effect
Snowy or sparkling appearance when the fluid is observed and mildly agitated in direct sunlight
Observed at cell counts below 400 cells/mm3
Turbidity of CSF
Turbidity scored on a scale from 0-4+
0 normal
4+ so turbid that newsprint cannot be read through the tube
Xanthochromia
Yellowish or yellow-orange discoloration
Arises due to the presence of bilirubin
Most commonly occurs following rupture of red blood cells into the CSF but may occur due to hyperbilirubinemia
Takes 1-4h to develop after a hemorrhagic event
High total protein (over 150 mg/dL) may cause mild xanthochromia
In neonatal foals, CSF is slightly xanthochromic in foals up to 10 days of age
Cell Count in CSF
In normalcy CSF cell count is very low
WBC 0-6 cells/uL for adults and foals
Leukocytes are almost totally mononuclear cells
Neutrophils and eosinophils are almost never seen in normal horses
Due to low concentration of protein, cells within CSF deteriorate rapidly, analysis should occur within 1 hour of collection
If analysis will be delayed, the sample should be split and one portion mixed with an equal volume of 40% ethanol until analysis
Differential cell counts should be performed and require concentration methods due to the low number of cells in CSF normally
What can you see neutrophilic pleocytosis with?
Neutrophilic pleocytosis occurs in horses with infectious (bacterial or mycotic meningitis, Eastern equine encephalitis, Western equine encephalitis, and Venezuelan equine encephalitis) or inflammatory conditions (trauma or chemical meningitis from hemorrhage or injection of ionic or nonionic contrast agents)
What can you see lymphocytic pleocytosis with?
Lymphocytic pleocytosis is relatively uncommon in horses with nervous system disease
May be seen in horses with CNS lymphoma and viral meningitis, specifically West Nile Virus encephalitis
What can you see eosinophilic pleocytosis with?
Eosinophilic pleocytosis is rare but has been reported in horses with verminous encepahlitis due to Halicephalobus sp.
RBCs in CSF
"Acceptable" number of RBCs in CSF has decreased and is considered to be a value of 50 RBC/uL
Has been demonstrated that blood contamination only minimally increases the CSF WBC count and total protein if the RBC count is less than 2000 RBC/uL
Plasma Proteins in the CSF
Plasma proteins gain access to the CSF primarily by diffusion across the blood-CSF barrier
Diffusion determined by the radius of the protein molecule which is directly related to the molecular weight
Normal CSF total protein concentration is roughly 1/100th that of blood plasma
Commonly reported reference range for CSF protein is 50-100 mg/dL for CSF taken from the lumbosacral space
Total protein concentration differs depending on the site of collection with samples collected from the LS site having slightly higher concentration than that from the AO site
Also reported that ponies have higher CSF total protein than horse breeds
CSF total protein concentration of foals is higher than that of normal adult horses
Newborn foals (<2 days of age) had a mean CSF total protein of 109.0 mg/dL and decreasing to adult values by 21 days of age
Methods to Assay Total CSF Protein
Turbidometric
Spectrophotometric
Lowry
Biuret
Dye binding
Immunologic methods
What causes increased CSF total protein?
Increased CSF total protein occur due to increased permeability of the blood-CSF of BBB, increased protein synthesis within the CNS obstruction of CSF flow, or tissue degeneration/necrosis
Obstructive diseases result in high protein concentrations due to enhanced resorption of water, as well as protein leakage
Complete spinal fluid block is associated with very high CSF protein concentrations - Froin's syndrome
What causes low CSF protein?
Low CSF total protein rare, can occur due to CSF leakage, removal of excessive quantities of CSF, increased ICP, or in cases of water intoxication
AO CSF Collection
18 gauge, 3.5 in spinal needle inserted at the point at which a line drawn between the cranial borders of the atlas intersect midline
Needle directed toward the lower jaw and advanced until dura is penetrated
Fluid flows without need for aspiration
Only withdraw 1-2 mL in neonates to minimize the risk of tentorial herniation
Putting head down to graze appears to increase the degree of neck soreness following an AO puncture
Described in standing horses
LS CSF Collection
Can use ultrasound guidance which may be useful in obese horses where the landmarks are difficult to palpate
Insertion site is on midline 0.5-1 cm cranial to the point at which the tuber sacrale are most superficial
Site clipped, prepped, and locally blocked
Can make a stab incision with #15 blade to minimize dulling of spinal needle
6-8 inch, 18 gauge spinal needle inserted and stabilized at the skin surface with one hand and advanced with the other
Advance straight down with no lateral or cranial-caudal deviation
Increasing resistance as the needle approaches the space and then decrease as the needle penetrates the ligamentum flavum, felt as a pop
Penetration of the membranes often accompanied by reaction from the horse
CSF collected by gentle aspiration

Complications of CSF Collection
Introduction of infectious agents into the CNS (septic meningitis), aseptic meningitis from hemorrhage, pain and swelling at the site of needle entry, trauma associated with recovery from anesthesia
Flipping over backwards or falling during LS tap
Spinal cord penetration (pithing) during AO tap, herniation of the cerebellum, and fractures or worsening of neurologic signs after anesthetic recovery