32. immune mediated disease part 2 (type III & IV hypersensitivities)
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
24 Terms
mechanism of type III hypersensitivity
formation of small, soluble immune complexes that are not cleared by phagocytes → antigen-antibody complexes deposit in tissue
→ local activation of complement (attract neutrophils)
→ inflammation & tissue damage
what are the two examples of type III hypersensitivities discussed in lecture?
target → blood vessels → purpura hemorrhagica
target → joint synovium → immune-mediated polyarthritis (IMPA)
what is the major infectious agent associated with purpura hemorrhagica in horses? what is the underlying pathology?
streptococcus equi equi
large amount of antigenic material (antigen excess; ex. draining abscesses)
with strangles, usually involves binding of both IgA & IgG complexes to M-like protein from Strep. equi
purpura hemorrhagica clinical signs
marked edema of head, ventral abdomen, and limbs
petechial hemorrhages of mucous membranes
may have signs of colic with GI infarction
diagnosing purpura hemorrhagica
history of infection, vaccination, or drug administration (although, may be idiopathic)
clinical signs
rule out other causes of vasculitis:
anaplasma
ehrlichia equi
babesiosis
equine viral arteritis
equine herpesvirus
immune-mediated thrombocytopenia
purpura hemorrhagica treatment
address underlying cause & remove it
antibiotics if bacterial infection suspected/present
stop using drugs if suspect trigger
suppress immune system → glucocorticoids (dexmethasone & prednisolone)
supportive care: hydrotherapy, leg wraps, nasogastric tube if dysphagic
pathophysiology of immune-mediated polyarthritis (IMPA)
antigen-antibody complexes become trapped in synovium
→ activates complement
→ complement attracts & activates neutrophils
→ tissue damage, edema, and joint swelling
most commonly noted in smaller joints (carpus or tarsus)
what is the typical cytologic finding in synovial fluid of a patient with IMPA?
increased number of neutrophils without evidence of infection
categories of non-erosive IMPA
idiopathic: most common in dogs
reactive: 25% of cases have underlying infection (viral, bacterial, fungal)
can be caused by vaccine or drug
enteropathic (rare): leaky gut → exposure of antigens to immune system
neoplasia-associated (rare)
what are examples/causes of reactive IMPA?
example: lyme arthritis
history of current or previous use of inciting drugs
ex. sulfonamide treatment in Doberman dogs
vaccine-induced usually occurs within 30 days of vaccination
signs usually resolve within 2-7 days of:
antimicrobial treatment
discontinuing the drug (if inciting cause)
spontaneously (vaccine-induced)
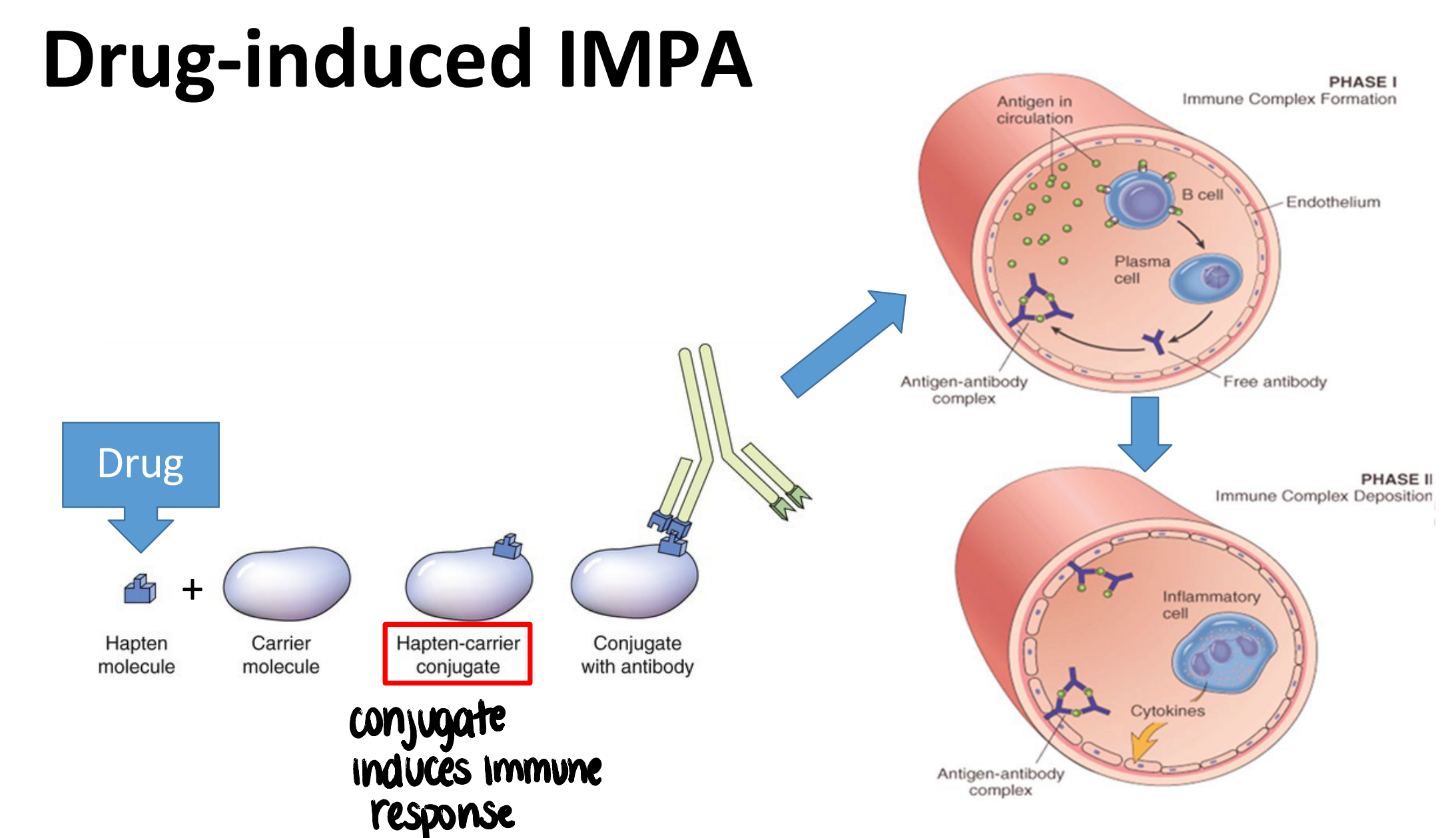
pathology of drug-induced IMPA
hapten molecule (drug) + carrier molecule → conjugate induces immune response → antibodies against conjugate produced
IMPA treatment
treat underlying factors if present (infection)
immune-suppressive doses of corticosteroids
refractive cases may need additional immune suppression (azathioprine)
mechanism of type IV hypersensitivity
antigen presented to antigen-specific T cells (usually TH1) → T cells become activated & produce cytokines → trigger leukocyte activation & infiltration (lymphocytes, macrophages) of target tissue → inflammation & tissue injury
organ-specific autoimmune disease caused by T cells are characterized by what?
chronic, progressive inflammation / tissue injury and fibrosis
what are the two examples of type IV hypersensitivities discussed in lecture?
hypothyroidism (lymphocytic thyroiditis)
keratoconjunctivitis sicca
canine hypothyroidism clinical signs
associated with inadequate thyroid function:
lethargy/inactivity
generalized weakness
unexplained weight gain
mental dullness
alopecia/excessive hair shedding
secondary skin infections (parasitic, bacterial, fungal)
histologic findings of lymphocytic thyroiditis
thyroid tissue infiltrated with lymphocytes & macrophages → destruction of thyroid gland by cell-mediated immune processes
canine hypothyroidism diagnostic findings
↑ thyroid stimulating hormone (TSH) with ↓ free thyroxine (fT4)
canine hypothyroidism treatment
lifelong supplementation with thyroid hormone → levothyroxine
correct any secondary problems (skin infections)
immune suppression NOT used to treat (damage to thyroid already done)
keratoconjunctivitis sicca (KCS) pathology/cause
most common cause is cell-mediated destruction of lacrimal gland with secondary tissue atrophy
→ decreased production of aqueous portion of tear film → dry eye
what is the most consistent clinical sign of KCS?
mucoid to mucopurulent ocular discharge
what dog breeds are at risk for immune-mediated KCS?
american cocker spaniel
cavalier king charles
english bulldog
lhasa apso
west highland white terrier
KCS diagnosis
schirmer tear test <10 mm/min
(normal > 15 mm/min)
history
clinical signs
keratoconjunctivitis sicca treatment
lifelong treatment
stimulate natural tear production
topical cyclosporine A → blocks IL-2 production & inhibits T-helper + CTL function in the lacrimal gland
topical tacrolimus (similar mechanism as cyclosporine, more potent)
provide tear replacements → artificial tears
control secondary infections → topical antibiotics
reduce inflammation → topical corticosteroids (ensure absence of corneal ulcers)