Exam 3 - GI
1/189
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
190 Terms
Primary clinical signs of gastroesophageal disease
Dysphagia
regurgitation
vomiting
Dysphagia
difficulty chewing and swallowing
issue with:
oral cavity
pharynx
upper esophagus
Secondary clinical signs of Gastroesophageal disease
anorexia
polyphagia
hypersalivation
retching
abdominal pain
bloat
weight loss
melena
coughing/gagging
Regurgitation Esophagus
Passive expulsion of undigested food or fluid from the esophagus
a passive process that occurs without warning
only neural reflex involved is the gag reflex (to protect the airway)
classic sign of esophageal disease
Dysphagia - absent
ability to drink - normal
attempts to swallow - single
pain on swallowing - possible
abdominal contractions - absent
time after eating - usually immediate; could be delayed with megaesophagus
food - undigested; tubular; foamy saliva
bile (yellow) - absent
blood - bright red
hair, plant, other - possible
complications:
aspiration pneumonia - common
fluid/electrolyte imbalance - unlikely

Regurgitation with Dysphagia pharynx/upper esophagus
Dysphagia - present
ability to drink - poor
attempts to swallow - multiple
pain on swallowing - possible
abdominal contractions - absent
time after eating - immediate
food - undigested; tubular; foamy saliva
bile (yellow) - absent
blood - bright red
hair, plant, other - possible
complications:
aspiration pneumonia - common
fluid/electrolyte imbalance - unlikely

The Act of Swallowing
3 phases
1st phase Oropharyngeal phase
oral
pharyngeal
Cricopharyngeal (UES relaxation)
2nd phase Esophageal phase
3rd phase Gastroesophageal phase
GES relaxation
Vomiting stomach
Forceful expulsion of gastric and intestinal contents through the mouth (CNS reflex)
dysphagia - absent
ability to drink - normal
attempts to swallow - single
abdominal contractions - present
time after eating - variable
food - partially digested; may be undigested
bile (yellow) - present
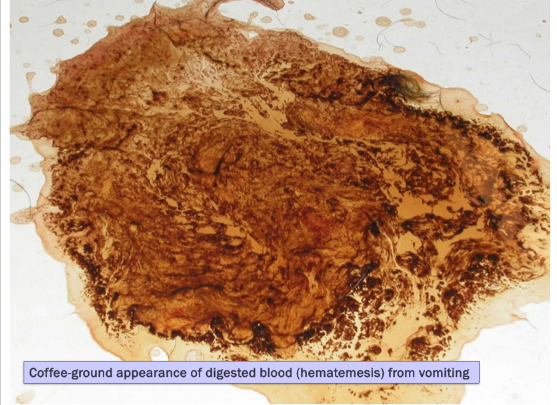
blood - dark brown “coffee grounds”
hair, plant, other - possible
complications:
aspiration pneumonia - possible
fluid/electrolyte imbalance - common
upper vs lower esophageal dz signs
upper
excessive salivation, difficulty swallowing, choking, and food/liquid coming out of the nose
lower
frequent retching, coughing, gagging, and vomiting
Aspiration pneumonia
regurgitation complications:
aspiration pneumonia (common) and fluid/electrolyte imbalance (unlikely)
vomiting complications:
fluid/electrolyte imbalance (common) and aspiration pneumonia (possible)
Clinical vomiting syndromes
Gastrointestinal bleeding:
iron deficiency/chronic blood loss/microcytic hypochromic anemia
hematemesis
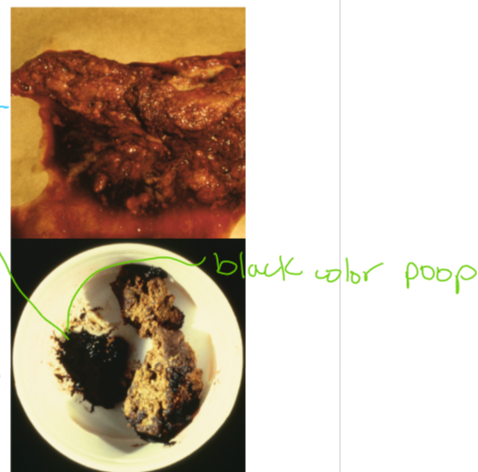
melena
pale mucous membranes and anemia
Delayed gastric emptying:
Rexongiziable food in vomitus >10 hours after eating
projectile vomiting
common with pyloric obstruction
bloating
belching
metabolic alkalosis
net loss of acid from body
Diagnostic methods for Gastroesophageal disease
Imaging
survey radiographs
contrast radiography
fluoroscopy
motiltiy disorders
ultrasonography
GI Endoscopy
upper GI examination
Esophagus, stomach, proximal duodenum
Lower GI examination
colon, cecum, distal ileum
GI Endoscopy
Non-invasive!!
an atraumatic technique thats an alternative to surgery requiring general anesthesia
take 10-15 biopsies per are of interest
Diagnosis capabilities:
gross appearance
mucosal biopsy
cytology
microbiology
parasite ID
Therapeutic indications:
foreign body retrieval
balloon dilation of strictures
placement of G-tube
polypectomy
Limitations:
submucosal and muscularis lesions
lesions beyond the reach of the scope
Exploratory Surgery
full-thickness biopsies
resection of masses
remove large foreign bodies
evaluate SI and other abdominal organs
Gastrointestinal Protectants
Antacids (aluminum hydroxide, calcium carbonate)
Histamine H2-receptor antagonists
Proton pump inhibitors
Sucralfate
Indications for use:
Gastroduodenal erosions or ulcers
Reflux esophagitis (heart burn)
Gastritis
Hypersecretory states (gastrinoma)
Histamine H2-receptor Antagonists
suppress acid production in stomach
Examples:
Famotidine/Pepcid
Cimetidine
Nizatidine (Axid) - 1st choice
Ranitidine (not available anymore)
renal excretion
product differences
Cimetidine: inhibition of p450 enzymes
Ranitidine, Nizatidine): GI promotility effects on stomach, intestine, colon
acid-suppressing effects start to diminish after several days of use
MOA: inhibits acetylcholinesterase
Proton Pump Inhibitors
The best we have for decreasing acid production
Broad spectrum anti-secretory
Examples:
Omeprazole (Prilosec)
Lansoprazole (Prevacid)
Pantoprazole
Esomeprazole
more effective than H2-blockers
to prevent rebound acid hypersecretion when stopping treatment, wean patients off PPI’s if used >3-4 weeks
Downside of PPI’s:
peptic hydrolysis of dietary proteins
Liberate vitamin B12 from dietary protein
suppress natural gastrin release
Sucralfate (Carafate)
Like putting a bandage on broken bone
aluminum salt of sucrose sulfate
mechanism
site protective
inactivate pepsin
adsorb bile acids and pancreatic enzymes
stimulates local PG
binds other oral drugs
separate administration by >1 hour
GI Promotility Drugs
Metoclopramide
Cisapride
Erythromycin
Azithromycin
H2-receptor blockers
Ranidine (Zantac)
Nizatidine (Axid)
Indications for use:
Reflux esophagitis (GES)
Megaesophagus (cats)
Functional delayed gastric emptying
Ileus
Megacolon
Metoclopramide
Promotility drug
Also an anti-emetic
no colonic motility
GI effects:
increased GES tone
increased gastric contractions
increased peristalsis proximal SI
no effect on distal GI tract including colon
Cisapride
Promotility drug
more effective pro-motility agent than metoclopramide in dogs and cats
Has NO anti-emetic properties
compounding pharmacy only
GI smooth muscle stimulated:
serotonergic (5HT4) effect on post-ganglionic cholinergic neurons
compared to metoclopramide:
not antiemetic
better for esophagus (Cats), stomach, SI, colon
Erythromycin
GI promotility drug
motilin analogue
effects on:
GES
stomach
SI
colon
works in dogs
lower dose than antimicrobial
Azithromycin
motilin analogue
used anecdotal since erythromycin price increased
effects probably similar to erythromycin
Diagnosis of swallowing disorders
Young animals:
congenital disease
cleft palate
cricopharyngeal achalasia
congenital megaesophagus
vascular ring anomaly
hiatal hernia
esophageal foreign body
infectious (rare)
older animals:
degenerative disease
acquired neuromuscular disorder
Idiopathic megaesophagus
Neoplasia
Selected breeds at risk
congenital Idiopathic megaesophagus
German Shepherd*
Shar Pei
Acquired Myasthenia gravis
German Shepherd*
Golden Retriever
Cricopharyngeal achalasia / dysphagia
Golden Retriever
Hiatal hernia / Reflux esopahgitis
Shar Pei
Bulldog
Oropharyngeal Dysphagia
structural disorders
dental/periodontal disease
stomatitis
pharyngitis/tonsillitis
neoplasia
foreign body
cleft palate
TMJ disease
95% of the time there is an underlying structural cause
functional disorders considered once structural disorders ruled out
potential clinical findings:
abnormalities prehending food or lapping water
excess chewing, chomping
dropping food
repeated swallowing
ptyalism
gagging, retching
management
treat underlying cause
supportive care
antibiotics for pneumonia
tube feeding (by-pass pharynx)
determine conistency of food best tolerated
what is the most common complication of esophageal disorders in dogs and cats?
Aspiration pneumonia
What is the most common cause of intraluminal esophageal obstruction in dogs and cats
Foreign body
especially linear foreign body in cats
Esophageal Foreign Body
Common FB’s
bones, needles, fish hooks, string (cats common), elastic hairbands, hairballs.
Predilection sites (where esophagus narrows)
cervical esophagus
thoracic inlet
base of heart
diaphragm
Diagnosis
clinical signs
acute onset
regurgitation, dysphagia
gagging, salivation
rads
endoscopy
methods of removal
endoscopy (preferred)
remove out of mouth
push into stomach
surgery
esophagotomy (least desirable)
Gastrotomy (easier than esophagostomy)
complications:
Esophagitis
Perforation
Stricture
Pneumonia
what is the method of choice for esophageal foreign bodies in dogs and cats? why considered urgent
Endoscopy is the method of choice for removal of esophageal FB
minimally invasive procedure
remove out-of-mouth or push into stomach
EMERGENCY! esophageal FB can cause a blockage that can lead to difficulty breathing and even death (by asphyxiation)
Esophageal Perforations
Air in mediastinum or pleural space
G-tube feedings
antibiotics
IV fluids
serial radiographs
small perforations
can heal with symptomatic therapy
prognosis good
large perforations
require surgery
prognosis guarded
What are causes of esophagitis? what factor determines whether a stricture will form as a consequence of esophagitis? what drugs can cause esophageal strictures in cats?
causes:
Exogenous
foreign bodies
chemicals
drugs
Endogenous
gastroesophageal reflux (gastric acid)
strictures form when esophagitis involves deeper layers (submucosa/muscularis) which heal with fibrous tissue
oral doxycycline, clindamycin tabs (cats)
Treatment options for reflux esophagitis
Proton pump inhibitor
refluxed gastric juice less acidic
Sucralfate suspension
esophageal mucosal protection
Metoclopramide or Cisapride
increase GES tone - less gastroesophageal reflux
Corticosteroids
empirical - prevent healing by stricture
use only if severe
Nutritional support
gastrostomy tube - only if severe esophagitis
Esophagitis
Causes
Exogenous
foreign bodies
chemicals
drugs
Endogenous
Gastroesophageal reflux (gastric acid)
predisposing causes of gastroesophageal reflux
General anesthesia*
hiatal hernia
brachycephalic obstructive airway syndrome
gastric outflow obstruction
profuse vomiting
clinical findings:
history
recent esophageal FB
recent medications
general anesthesia
signs of acute or chronic esophageal disease
caustic injury - oral ulcers
Endoscopic findings
more sensitive than radiography for detecting esophagitis b/c can see subtle reddening
lesions
muscal erythema, friability, erosions, ulcers, pseudomembranes
reflux esophagitis
lesions worse in distal esophagus
general therapy:
proton pump inhibitor
sucralfate suspension
metoclopramide or cisapride
corticosteroids
nutritional support
Esophageal Stricture
Abnormal narrowing of the esophageal lumen due to fibrous tissue
forms when esophagitis invovles deeper layers (submucosa/muscularis), which heal with fibrious tissue
most common causes:
gastroesophageal reflux during anesthesia
secondary to esophageal foreign body
oral doxycycline, clindamycin tabs (cats)
other (caustic agents, esophageal surgery)
clinical signs
regurgitation
solid food»>liquids
progressive
3 to 14 days after esophageal injury
ravenous appetite
weight loss
Management:
Balloon dilation*
typically requires multiple dilations under general anesthesia every 5-7 days
surgical resection
corticosteroids (empirical)
treat esophagitis
gastrostomy tube
prognosis - guarded to poor
Give your top 3 differential diagnoses for causes of regurgitation in puppies. what diagnostic tests would be most helpful to differentiate these disorders? how to tx and prognosis
Esophageal stricture (Dx by esophagram)
Megaesophagus (Dx by thoracic rads)
Foreign body (Dx by thoracic rads)
Reflux esophagitis (Dx by ADD)
Thoracic radiographs - best single test for esophageal disorders
Vascular ring anomaly
congenital malformation of great vessels and branches that entraps the intrathoracic esophagus
Persistent right aortic arch:
congenital malformation
young (<6 months)
regurgitation (solids>liquids)
often first noted when weaned to solid food
diagnosis
Thoracic rads*
contrast esophagram* or CT angiography
treatment - surgical
prognosis
good with surgery (clinical improvement in >90%)
worse if delayed surgery or large diverticulum
Esophageal Neoplasia
Not very common
types
Sarcoma
spirocerca lupi
squamous cell carcinoma
old cats
Leiomyoma/sarcoma
distal esophagus of dogs
features
asymptomatic (early)
obstruction (advanced)
treatment
surgical resection (distal leiomyoma)
prognosis
guarded (except leiomyoma)
What is the most common cause of megaesophagus in dogs
Idiopathic acquired is the most common in dogs
symptomatic tx
supportive tx
prognosis: POOR due to repeat aspiration pneumonia events
IF myasthenia, many will have clinical remission and excellent long-term outcome with supportive therapy
myasthenia gravis MUST be tested for in patients with megaesophagus or functional neuromuscular disorders of the esophagus (Acetylcholine receptor Abs)
IV LRS
Abx
Pyridostigmine (Cholinesterase inhibitor)
why would promotility drugs like cisapride and metoclopramide be unlikely to be effective in the tx of idiopathic megaesophagus in dogs as compared to cats? what is the rational for giving sildenafil to dogs with idiopathic megaesophagus
Promotilty drugs like cisapride and metoclopramide are unlikely to be effective in the treatment of idiopathic megaesophagus in DOGS because these drugs primarily work by stimulating the GI tract muscles and increasing pressure within the GI tract
this can be beneficial in CATS with idiopathic megaesophagus as it can help to move food and liquid through the esophagus and into the stomach
however, in DOGS the esophagus is not a muscle so this type of treatment is not likely to be effective
furthermore, these drugs may actually make signs worse in DOGS as they can irritate the already weakened esophagus and cause further inflammation
Sildenafil (phosphodiesterase type 5 inhibitor) decreases GES tone, and regurgitation and facilitates emptying
what are two undelrying causes of acquired megaesophagus in cats?
Hiatal hernia
Reflux resophagitis
what common structural diseases of the oropharynx can present with dysphagia? Describe the 2-step diagnostic approach to oropharyngeal dysphagia
Oropharyngela neoplasia (tumors), FB obstruction, strictures, and trauma
first a complete physical examination of the pet should be performed in order to identify any obvious signs of oropharyngela disease, such as swelling, inflammation, or tumors
if the physical exam does not reveal any obvious signs of oropharyngeal disease, imaging such as radiographs or endscopy should be performed to further evlauate te oropharynx and look for any structural abnormalities
Drugs to induce vomiting
Dogs
Apomorphine
Dopamine (D2) agonist at CRTZ
GOLD standard emetic for dogs; IV or crushed tab in conjunctival sac
Dogs
Ropinirole (Clevor)
Dopamine (D2) agonist at CRTZ
Eyedrops recently approved for market
Cats
Xylazine
a-2 adrenergic agonist at CRTZ
Cats
Dexmedetomidine
a-2 adrenergic agonist at CRTZ
may be more effective than xylazine
apomorphine is not effective in cats because they lack dopamine receptors
Why is metoclopramide not effective as a central-acting antiemetic in cats
Acts on dopamine receptors and cats lack dopamine receptors, therefore it has no antiemetic effects in cats
when is metoclopramide contraindicated
Intestinal obstruction
What diangostic tests or procedures are useful to identify systemic (non-GI) causes of vomiting
blood tests, rads, ULS, others
pancreatitis: pancreatic lipase
kidney disease: BUN, creatinine, SDMA, UA
liver disease: ALT, ALP, SBA, T bili
Diabetes mellitus: serum and urine glucose
hypoadrenocorticism: Na+, K+, ACTH stim
Hyperthyroidism (cats): T4
FeLV/FIV (Cats)
What are indications for antiemetic therapy
symptomatic control of vomiting (short-term basis)
profuse vomiting (resulting in fluid, lyte, or acid-base imbalances)
motion sickness
what mechanism should be considered in a vomiting dog or cat with hypochloremic hypokalemic metabolic alkalosis what is the fluid of choice for treatment (including supplementation)
0.9% NaCl (plus KCl)
Causes of vomiting - clinical approach
primary GI disease
distention, inflammation, irritation of GI tract; chemo
intestinal tract
vomiting center
Non-GI disease
liver, kidney, pancreas, adrenals, endocrine → circulating metabolites or toxins (± other mechnaisms)
chemoreceptor trigger zone
vomiting center
Clinical features of vomiting
if vomiting undigested food > 10 hours after eating → delyaed gastric emptying
if projectile vomiting, forceful ejection → gastric or upper small bowel obstruction
Metabolic consequences of vomiting
Dehydration
Electrolyte imabalances
gastric juice is rich in K+, Na+, Cl-
hypokalemia
hypoanremia
hypochloremia
acid-base disturbances
metabolic acidosis
secondary to dehydration, poor tissue perfusion, lactic acidosis
metabolic alkalosis (uncommon)
in situations with a net loss of acid from the body
gastric and proximal duodenal obstruction
Primary GI disease
Dietary indiscretion/hyperensitivity
Acute gastritis or gastroenteritis (AHDS, parvo, parasitic, bacterial, protozoal)
drug associated
obstruction (FB, GDV, intussuscption)
GI ulcers (NSAIDs)
Non-GI disease
acute pancreatitis
acute liver disease/failure
acute kidney disease
hypoadrenocorticism (dog)
acute abdomen (all causes)
sepsis/endotoxemia
diabetic ketoacidosis
sick acute vomiter RED FLAGS
disturbing potential cause identified
vomiting/diarrhea frequent/severe
unstable/systemically sick
dehydrated
unwilling to eat/drink; cant hold anything down
abnormal PE
Commonly used antiemetics
Metoclopramide
Ondansetron
Maropitant (Cerenia)
chlorpromazine
others:
Mirtazapine
Antihistamines
Motion sickness meds for dogs
Maropitant (Cerenia)
Chlorpromazine
Diphenhydramine (Benadryl)
Vomiting from parvo drug options
Maropitant (Cerenia) - not under 8 weeks old
Metoclopramide (if <8 weeks of age)
CRTZ
promotility effect
vomiting from pancreattis drug options
Maropitant (Cerenia)
vomiting center
visceral analgesia
refractory vomiting - add Ondansetron
Nausea and vomiting from chemo drug options
Ondansetron
especially for nausea
Vomiting cat drug options
Maropitant (Cerenia)
Mirtazapine
also appetite stimulant
not metolcopramide
unless promitlity action needed
Mirtazapine
anti-emetic
appetite stimulant
nonselective 5-HT2-3 antagonist
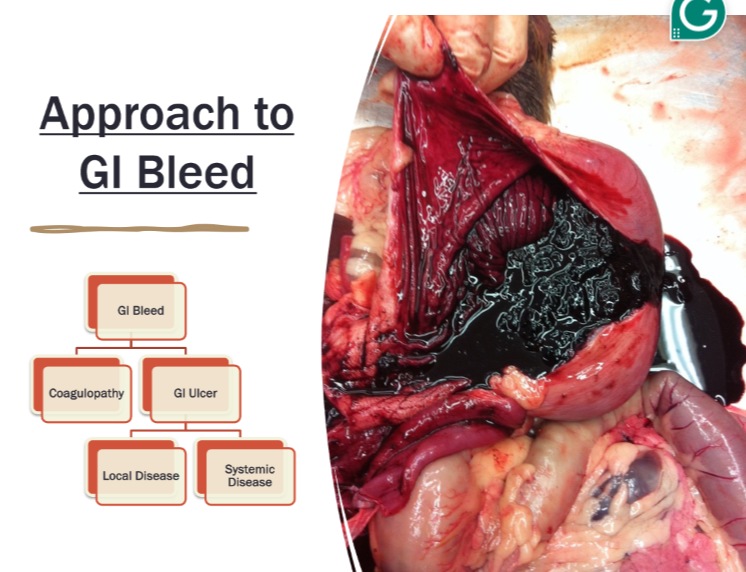
GI bleeding with vomiting
history - NSAIDs and or corticosteroids?
CBC, chemistry profile, UA
regnerative anemia, hypoproteinemia
iron-deficienciey (microcytic) anemia (chronic)
undelryiing organ disease
Imaging
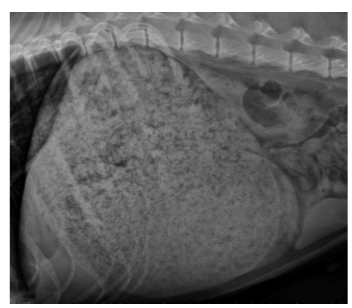
rads - unremarkable unless perforation
contrast rads - mucosal defect
AUS - muscoal thickening; organ disease
Endosocpy or surgery
Management
eliminate risk factors
maintain fluid, electrlyte, acid-base balance
gastroprotectants
PPI (omeprazole)
sucralfate
prognosis
guarded to good
depends on undelrying cause
Vomiting with Delayed gastric emptying
Rexongizable food in vomitus >10 hrs after eating
Mechanical obstruction:
luminal or mural lesion
foreign body
congenital pyloric stenosis
antral pyloric hypertrophy
gastritis or ulcer
neoplasia or polyp
GDV
secondary to intestinal obstruction
extramural compression
hepatic or pancreatic inflammation or neoplasia
enlarged lymph nodes
diaphragmatic hernia
Functional “Obstruction”
Eg. anticholinergic drugs, opiods, parvo, vagal nerve damage (surgery)
projectile vomiting
bloating
belching
Metabolic alkalosis - net loss of acid from body
History - acute or chronic, FB exposure, medications
labortatory features - hypochloremic, hypokalemic metabolic alkalosis
imaging
survey abdominal rads
contrast studies
AUS- outflow tract
management:
fluid therapy
0.9% saline plus KCI metabolic alkalosis
relieve obstruction
consider prokinetic drugs only FOR
post-op gastric atony (chronic obstruction)
functional delyaed gastric emptying
no evidence of mechanical obstruction
Cisapride preferred
Dietary recommendations
low fat, canned or liquid
small frequent meals
Describe empirical treatment for “Bilious vomiting syndrome” in dogs
meal before bedtime, metoclopramide, or gastroprotectant (PPI)
How would you differentiate a patient that had GI bleeding due to a sepsis and DIC versus a gastroduodenal ulcer
physcial exam melna systemic bleeding oral mm hemorrhage of skin, evidence of bleeding elsewhere
ulcers or erosions
Hematemesis, melena, ± anemia
Compare the sensitivity of contrast radiography versus endoscopy in the diagnosis of gastric mucosal erosions and ulcers
contrast radiography is a less invasive and less expensive imaging technique than endoscopy. it is also widely available and retatvely easy to use
however contrast radiography is limited in its ability to detect small lesions and subtle mucosal erosions
endoscopy on the other hand is a much more sensitive imaging technique that can detect small lesions and subtle mucosal erosions
it is also able to provide a more detailed examiantion and allow for biopsy sampling
therefore endoscopy is more sensitive than contrast radiography in the diagnosis of gastric mucosal erosions and ulcers
What are potential mechanisms for gastric foreign bodies to cause clinical signs? why are pennies minted after 1983 toxic? what clinical signs might they present for?
mechanisms cause clinical signs of Gastritis, obstruction, toxins
Zinc toxicity, check PCV to check for hemolytic anemia
might present for acute vomiting
Under what circumstances would inducing vomiting with apomorphine for removal of a gastric foreign body in a dog be contraindicated?
If the foreign body is a sharp or pointed object
What drugs can cause a functional delay in gastric emptying
Anticholinergic drugs like (atropine and glycopyrrolate)
Opioids
Parvo
vagal nerve damage due to surgery
How do you make the diagnosis of a functional gastric empyting disorder
Signalment
young - congenital pyloric stenosis, FB
Old - antral pyloric hypertrophy (dogs), neoplasia
history
acute or chronic, FB exposure, medications
Laboratory features:
hypochloremic, hypokalemic metabolic alkalosis
imaging
survey abdominal rads
contrast studies
AUS - outflow tract
Why does hypochloremic metabolic alkalosis occur with pyloric obstruction? what type of fluids are indicated for treatment of this acid-base disorder?
Hypochloremic metabolic alkalosis with pyloric obstruction because the vomiting associated with the obstruction causes a loss of hydrochloric acid (HCI) from the body
this reduces the concentration of chloride (Cl-) in the extracellular fluid, leading to an alkalosis due to an increase in the pH of the blood
the most appropriate treatment for this disorder is the administration of fluids containing electrolytes such as sodium chloride or potassium chloride to replace the lost HCl and Cl-
fluids with a higher sodium content are preferred 0.9% NaCl + KCl
what is the most common malignant gastric neoplasm in dogs and cats?
Dogs - Adenocarcinoma
Cats - Lymphoma
Gastritis
Acute
sudden onset of vomiting; healthy
chronic:
chronic vomiting of food or bile; otherwise healhty
inflammation of the gastric mucosa
lymphoplasmacytic most common
eosinophilic (parasites hypersensitivity)
granulomatous and atrophic are rare
requires a biopsy for diagnosis
cause is usually not identified
Idiopathic most common cause of gastritis
Diagnostic approach:
CBC, chemistry profile, UA
often unremarkable
sometimes eosinophlia
parasite evaluation
fecal flotation
vomitus (cats - olulanus)
abdominal imaging
usually unremarkable
look for other causes of vomiting
therapeutic trials first, if not response then endocospy and biopsy
therapeutic trials:
diet trial (min 2-3 wks; ideal 4-6 wks)
highly digestible / GI
novel (limited) ingredient
hydrolyzed
fenbendazole deoworming
omeperazole (PPI)
± promitlity drug
metoclopramide or cisapride
post-biopsy
continue diet therapy
Ulcers or erosions
Hematemesis, melena, ± anemia
Clinical associations:
drugs, chemicals, toxins
NSAIDs*, corticosteroids*
increased gastric acid secretion
kidney failure, mast cell tumor*, liver disease*, pyloric obstruction/GDV, gastrinoma (rare)
Diagnostic approach:
history
NSAIDs and or corticosteroids
CBC, chemistry profile, UA
regenerative anemia, hypoproteiemia
iron deficiecy (microcytic) anemia (chronic)
underlying organ disease
imaging
rads - unremarkable unless perforation
contrast rads - mucosal defect
AUS - mucosal thickening; organ disease
endoscopy or surgery
management:
eliminate risk factors
maintain fluid, electrolyte, acid-base balance
gastroprotectants
PPI (Omeprazole)
Sucralfate
prognosis
guarded to good
depneds on undelrying cause
Gastric Foreing Body
common problem
dogs > cats
acute vomiting
signs due to
gastritis
obstruction
toxins
lead, zinc
Diagnosis:
lab findiings
hypochloremic, hypokalamic metabolic alkalosis with obstruction
abdominal rads
contrast rads
cloth, radiolucent objects
endoscopy
surgery
Management:
medically induced vomiting
small objects without sharp edges or points
endoscopy
always radiograph just prior to removal
sharp objects could damage esophagus during removal
prepare owner that lapartomy will be necessary if endoscopy fails
surgery
Hairballs (cats)
common problem
higher in long haired cats
hair swallowed during grooming
consider excess hair ingestion
fleas, pruritic skin disease, overgrooming d/t anxiety
or GI disease (2nd motility problem)
dietary intolerance, IBD
complications:
Nasopharynx
vomited but doesnt come out the mouth
Esophagus
obstruction, esophagitis, stricture
stomach
intestine
obstruction (partial or ocmplete)
hairball colitis
may require surgical removal
prevention:
dietary management
contain fiber
daily brushing: lion clip
gastric lubricants
laxatone (NOT mineral oil)
promotility drugs
metoclopramide, cisapride
What parasite should always be considered in dogs with large bowel diarrhea
Whipworms
what parasite should always be considered in cats with large bowel diarrhea
Tritrichomonas
Define hematochezia, melena, and tenemus
Hematochezia - blood with normal feces (think polyp!)
Melena - dark, tarry stool ± blood (mainly caused by the upper GI tract (stomach or SI)
small bowel diarrhea
Tenesmus - straining to defecate (diseaseof large intestine)
Why would a serum thyroixin (T4) level be important to evaluate in a 10 year old cat with chornic diarrhea and weight loss?
Because it can help to diagnose or rule out certain thyroid conditions that could be causing the symptoms
Hyperthyroidism for example is a common cause of chornic diarrhea and weight loss in cats, and a low serum T4 can indicate this condition
Low serum T4 levels can also indicate hypothyroidism, which can also cause these symptoms
by evaluating the T4 serum level, the vet can determine if the cat has a thyroid disorder that is causing the chronic diarrhea and weight loss
Why would you evaluate a serum cortisol / ACTH stimulation test in a young adult dog with unexplained chronic or recurrent GI signs
A serum cortisol/ACTH simulation test is used to evaluate the function of the adrenal glands
the test invovles collecting a baseline blood sample and measuring the cortisol level, then administering a synthetic form of the hormone ACTH and collecting a second sample one hour later measure the cortisol response
an abnormally low cortisol response suggests the presence of Addison’s disease an adrenal insufficiency disorder that can cause chronic GI signs
what type of treatment is universally important in any animal with acute severe small bowel diarrhea
empirical de-worming is always reasonable
IV fluids if dehydrated (isotonic crystalloids: LRS, plasmalLyte) - monitor for hypoK
When should Lopermaide (Imodium) use be avoided or used with caution?
avoid with diarrhea with bacterial etiology or acute diarrhea with secondary invasive bacteria (parvo)
avoid or use at reduced dose in animals with MDR1/p-glycoprotein defects; increased risk of adverse CNS effects (Collies, Australian Shepherds, other)
Which antibiotics are most commonly used to treat intestinal dysbiosis?
Metraonidazole and tylosin
Corticosteroids are often indicated as the primary treatment for what chronic GI condition?
Chronic enteropathy (IBD) immunosppression Tx (Prednisolone)
Why is cobalamin replacement important when it is depleted in animals with chronic enteropathy?
cobalamin deficiency itseflt can contribute to intestinal disease
villus atrophy
mucosal inflammation
What are the 3 cellular or tissue targets for canine parvovirus
rapidly dividing cells intestines, bone marrow, lymphocytes
How would the clinical signs, physical findings, and CBC help distinguish severe paravoviral enteritis from less serious causes of sudden GI upset such as dietary indiscretion
sudden onset of vomiting or diarrhea (bloody), fever, anorexia, depression, dehydration, death (hypovovlemia; sepsis)
canine parvovirus
Etiology: CPV-type 2 (a,b,c)
affinity: for rapidly dividing cells
intestines → crypt cell necrosis; vomit/diarrhea
bone marrow → neutropenia
lymphocytes → lymphopenia; immunosuppression
transmission
fecal-oral; highly contagious
survival for months to years in environment, fomites
Incubation: onset of signs 4 to 7 days
age: puppies 6 wk to 6 months
signs: sudden onset
vomiting, diarrhea (bloody), fever, anorexia, depression, dehydration, death (hypovlemia; sepsis)
Diagnose: clinical signs:
age plus exposure, leukopenia, neutropenia, lymphopenia, rads (gas distentioin; ileus), fecal antigen immunoassay (SNAP- ELISA technology)
fecal antigen immunoassay (ELISA)
negative test does NOT rule out disease
especially if >10 days after initial infection
low viral load; intermittent shedding; antibody coated virus
vaccination unlikely to cause positiive
treatment: persistent vomiting and diarrhea - antiemetic (metoclopramide; ondansetron)
neutropenia - antibiotics (IV; ampicillin -slbactam)
dehydration hypokalemia, acidosis - IV fluid rehydration; add KCl
hypoglycemia - add dextrose to IV fluids
nutritional support - feed through vomiting; NG tube
hookworms and roundworms - anthelminitc (pyrantel)
Feline parvovrus
Etiology:
Feline parvovirus -95%
CPV-2 variants (a,b,c)-5%
at risk kittens 8-12 wks of age
pathogenesis - same as CPV except
no myocarditis
CNS signs if in utero or early neonatl infection
cerebellar hypoplasia most common
peracute form - sudden death from septic shock
acute form
fever, anorexia, lethargy, vomiting, diarrhea (bloody in <15%), dehydration
final stage - hypethermia, DIC
diagnose: consistent signalment, history, signs
neutropenia and lymphopenia (65-75%)
use canine fecal ELISA assay
false negatives occur
false positives for at least 14 days after vacciantion
treatment: principles of therapy same as for CPV
high mortality rate
50-80% in cats despite treatment
10-40% mortality rate in dogs
vaccination: vacciantion (MLV or inactivated)
6-8 wks, then every 3-4 wks until 16-20wks
booster 1 year after primary series
then every 3 years
In a dog with diarrhea what is the significance of a positive fecal culture for Clostridium perfringes? does the presence of Clostridial spores on fecal microscopy confirm the diagnosis of enterotoxigenic Clostridial diarrhea?
Disease most likely caused by C. perfringens type A producing enterotoxin (CPE)
role of CPE in canine diarrhea unclear (cats)
recently C. perfringesn type A identified which encodes gene for novel net F toxin acute hemorrhagic diarrhea syndrome (AHDS) in dogs (formely HGE)
combination testing*
PCR for toxigenic strains
ELISA detection of C. perfringens enterotoxin (CPE)
When should you consider giving antibiotics to a dog with a fecal culture positive for Salmonella?
NOT recommended for uncomplicated
YES if systemic signs (fever etc) or immunocompromised animal
ampicillin + Enrofloxacin (or based on clinical signs)
what organs systems can be involved with histoplasmosis in dogs?
GI tract (esp. colon)
respiratory tract
liver, spleen, lymph nodes, bones, eyes
7 giardia vs tri
Considering efficacy and safety what drug would be considered the overall best choice for treating giardiasis in dogs and cats?
Fenbendazole
often used in combination with metronidazole (but this one not as effective and also neutrotoxic)
What type of intestinal foreign body causes aggregation of abdominal bowel loops?
Linear foreign body
Where does a linear foreign body typically lodge proximally in a cat? How is this different in a dog?
cats → base of tongue
Dogs → Pylorus
Palpation of sausage shaped midabdominal mass in a young dog suggests what diagnosis?
Intussusception
Ileocolic junction most common location in dogs
young animals
usually idiopathic
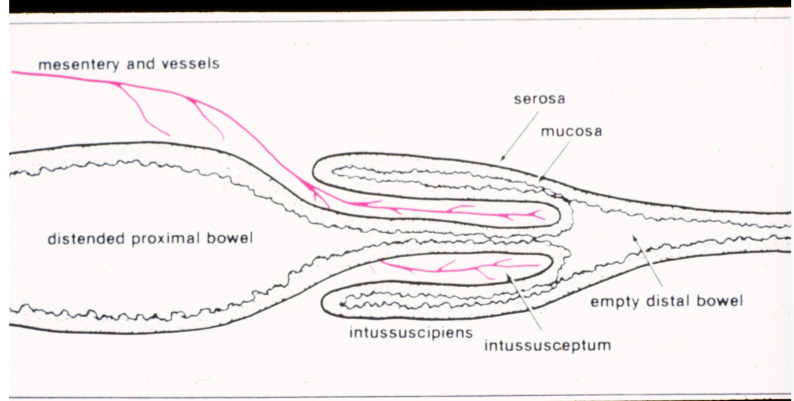
What disorders can predispose to development of an intussu
Disease associations:
parasites
parvo
lepto
FB
Prior GI surgery
What intestinal neoplasm is most likely to cause a focal circumferential stenosing stricture like lesion?
Intestinal adenocarcinoma
Which neoplasm is most likely to cause diffuse thickening of the wall of a large portion of the small intestins?
Intestinal lymphoma
What breed of dog has the highest incidence of exocrine pancreatic insufficiency? Age of onset?
German shepherfd, young adult dogs