17. Renal Pathophysiology
1/95
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
96 Terms
What are the functions of the kidney?
Major excretory organ: filters blood 30x a day
Endocrine organ for renin, erythropoietin, and vit D
What are the major parts of the kidney?
Hilum
Cortex
Medulla
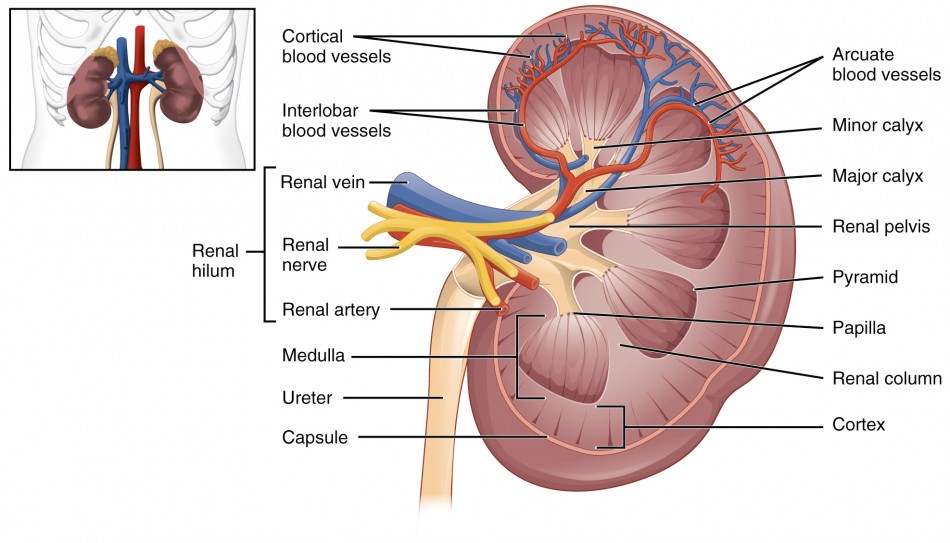
What is the major pathway of urine?
Calyx → Renal pelvis → Ureter → Bladder → Urethra
What is a nephron?
The smallest functional unit of the kidney. They are responsible for filtration, reabsorption, and secretion.
What are the differences between a nephron vs tubule?
Tubules is part of the nephron, where the filtrate from the glomerululs is processed to form urine. The nephron includes renal corpuscles and tubules.
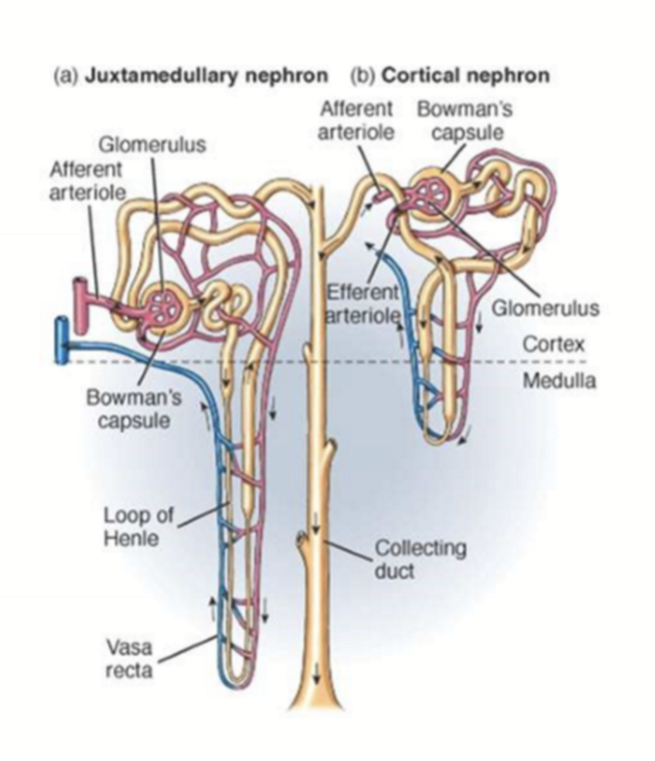
What are the types of nephrons?
Cortical nephrons: Mostly in the renal cortex; only has a bit of the loop of henle enter the medulla; and has peritubular capillaries. Mainly used for general filtration and reabsorption. Is the majority of nephrons.
Juxtamedullary Nephrons: Near the cortex-medulla junction; has long loop of henle that extends deep into the inner medulla. Mainly used for concentrating urine.
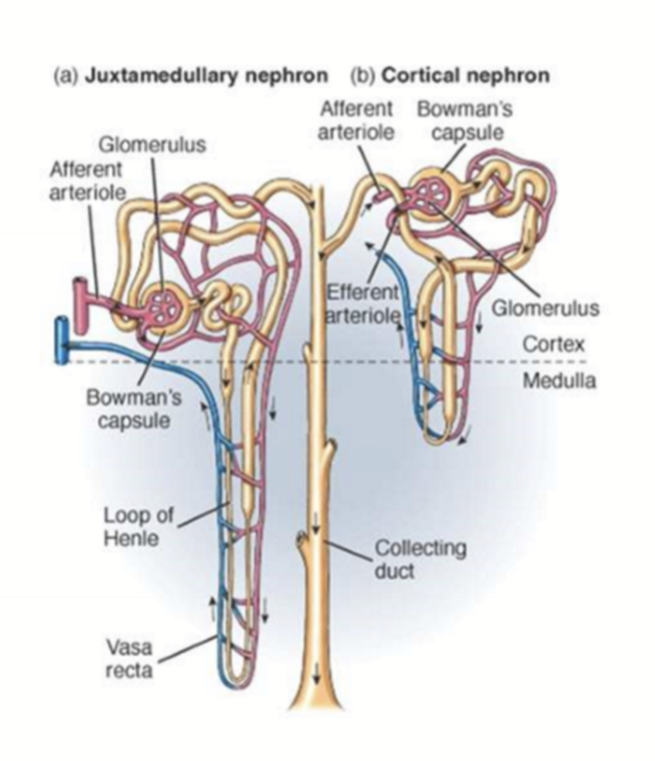
What are some commonalities between the coritcal and juxtamedullary nephrons?
Renal corpuscle in cortex
Share collecting ducts
What occurs in the renal corpuscle?
Filtration, with starling forces in the glomerular capillaries pushing particular substances into Bowman’s space to for ultrafiltrate.
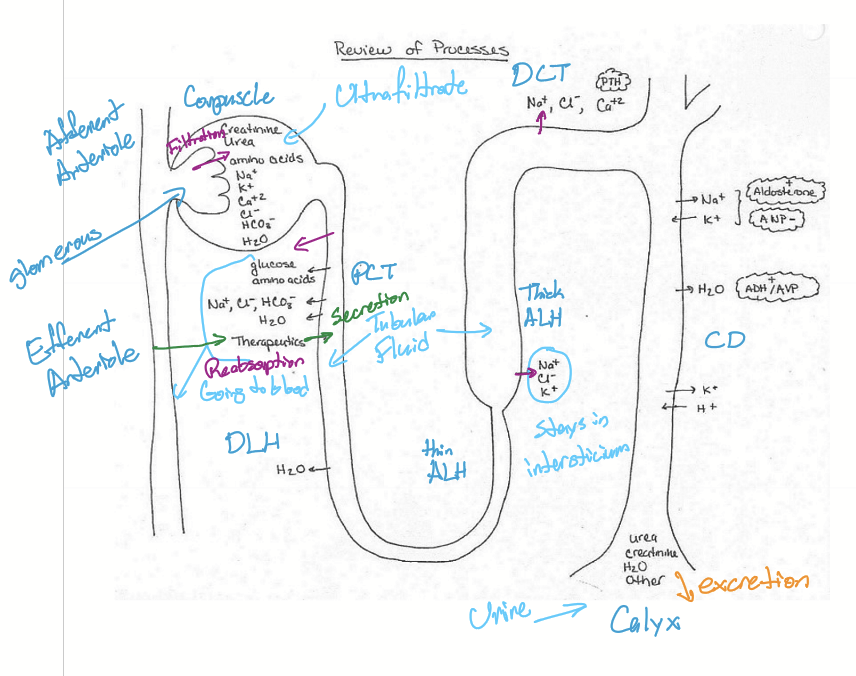
What occurs throughout the tubule?
Reabsorption of essential substances back into the blood. Secretion of certain substances from blood into tubule fluid via active transportation.
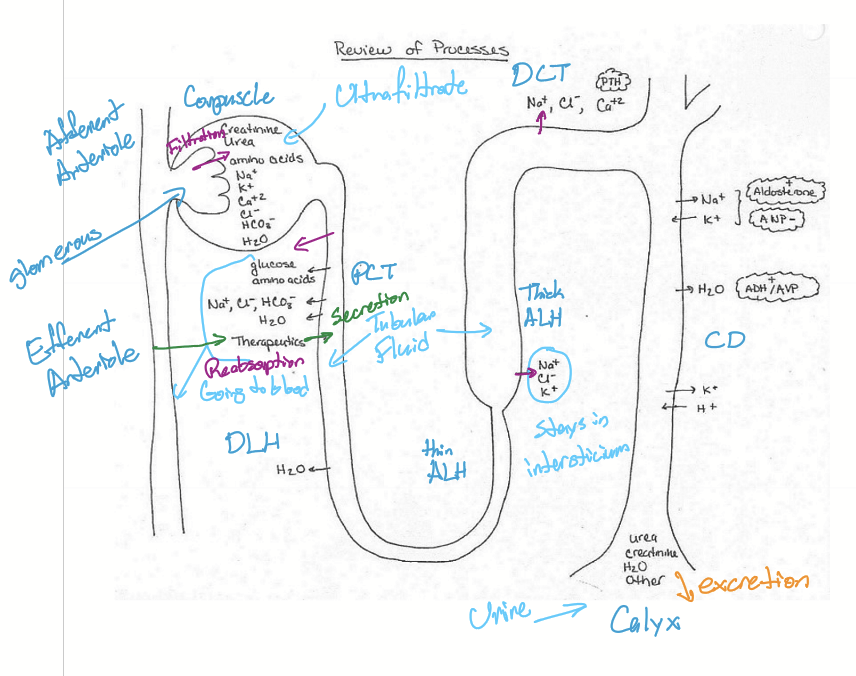
What is excretion made up of?
Filtration + secretion - reabsorption
What is renal filtration?
The process of filtering wastes and ions out of the blood.
What is Glomerular filtration rate?
The rate of plasma filtration by glomeruli
Why can substances filter through the glomeruli?
Fenestrated capillary endothelium
Basement membrane is negatively charged
Slits between podocyte foot process
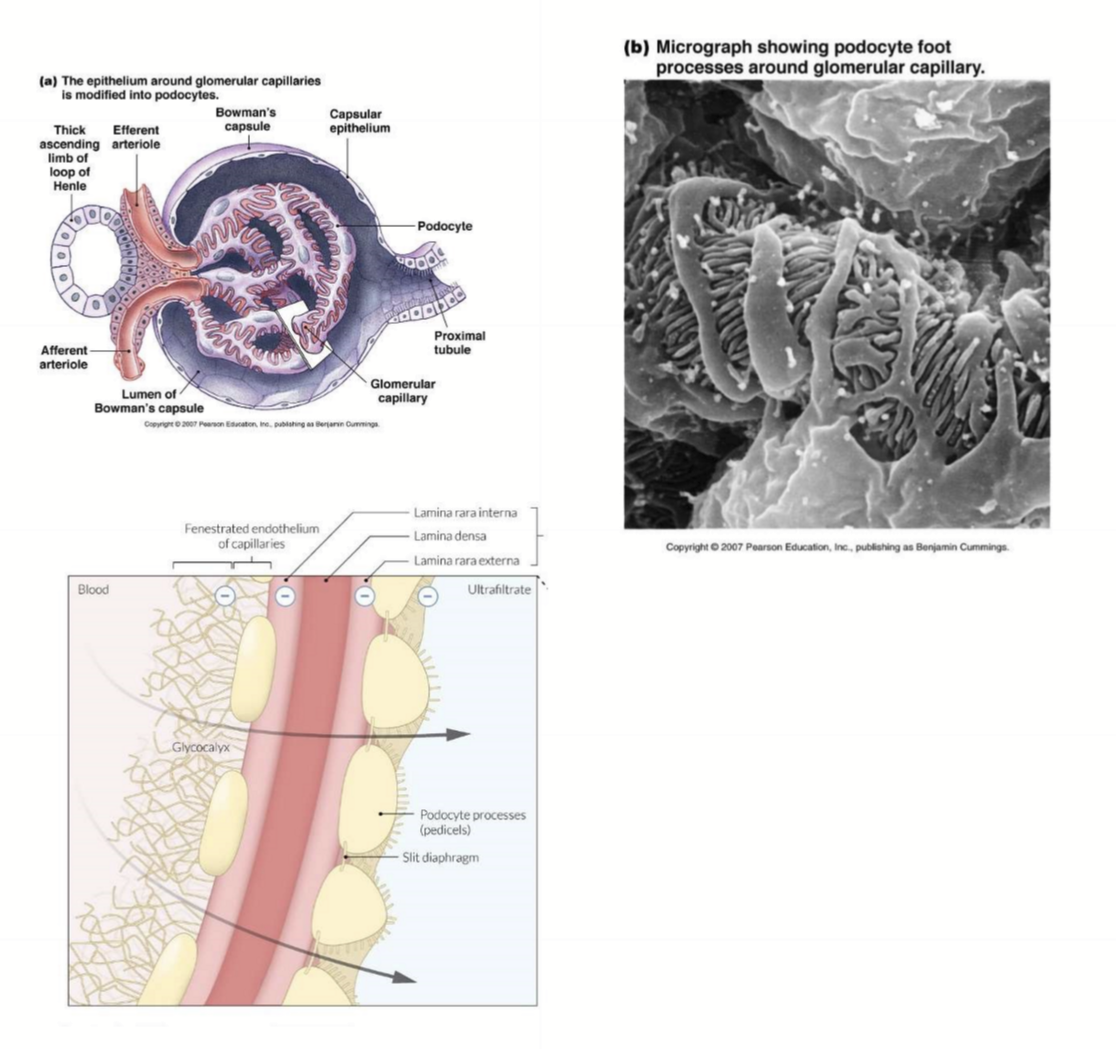
What is the ultrafiltrate composed of?
Small cations
Few small anions
Small substances: glucose and amino acids
Water
What regulates glomerular filtration rate?
Autoregulatory process: increase in pressure causes vasoconstriction and vice versa
Tubuloglomerular feedback: nephron tubule self-regulates blood flow to distribute blood flow among nephrons to maintain GFR
What is damaged in the kidneys with patients with DM?
Damaged TGF/tubuloglomerular feedback
What is the mechanism of GFR is too high?
Increased GFR
Increase Cl in DCT
Macula Densa senses Cl
Macula densa secretes adenosine
Adenosine causes vasoconstriction of afferent arteriole
Decrease GFR
What is the mechanism of GFR is too low?
Decreased GFR
Decrease Cl in DCT
Macula Densa senses Cl
Macula Densa secretes PGE2
Vasodilation of afferent arteriole
Increase GFR
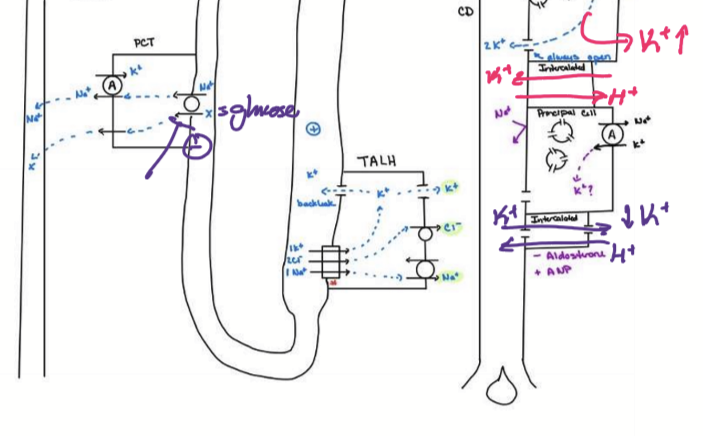
How is glucose reabsorbed into the blood in the kidneys?
NA/K ATPase active on basolateral membrane pumps NA from cell into plasma
Na decreases in cell
Low cellular Na drives Na/Glucose linked transporter
SGLT2: early in PCT (most)
SGLT1: late in PCT
Na and Glucose is reabsorbed from tubular fluid into vessel
Increased oncotic pressure in vasa recta
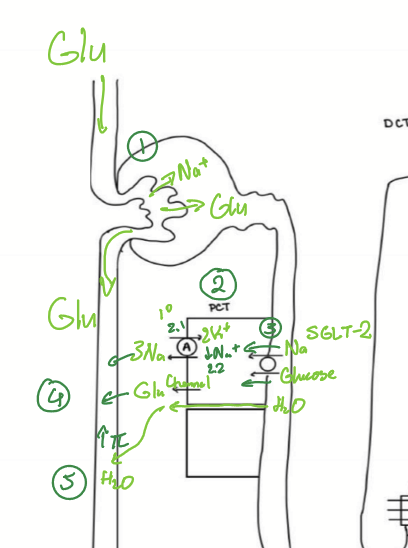
What drugs inhibit SGLT2?
dapagliflozin
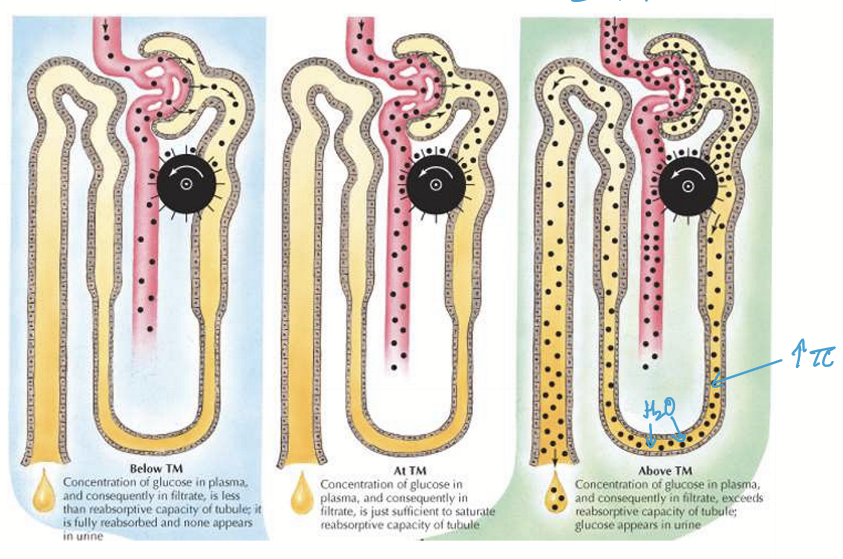
What is the relationship between the transport maximum (Tm) for glucose vs different levels of blood glucose?
Normal blood glucose < Tm : complete reabsorption
Elevated blood glucose = Tm : complete reabsorption
High blood glucose > Tm : pateint will have glucose in urine (glucosuria) and osmotic effect of excess glucose will cause osmotic diuresis, causing polyuria
What does every epithelial cell has?
NKA on the basolateral surface
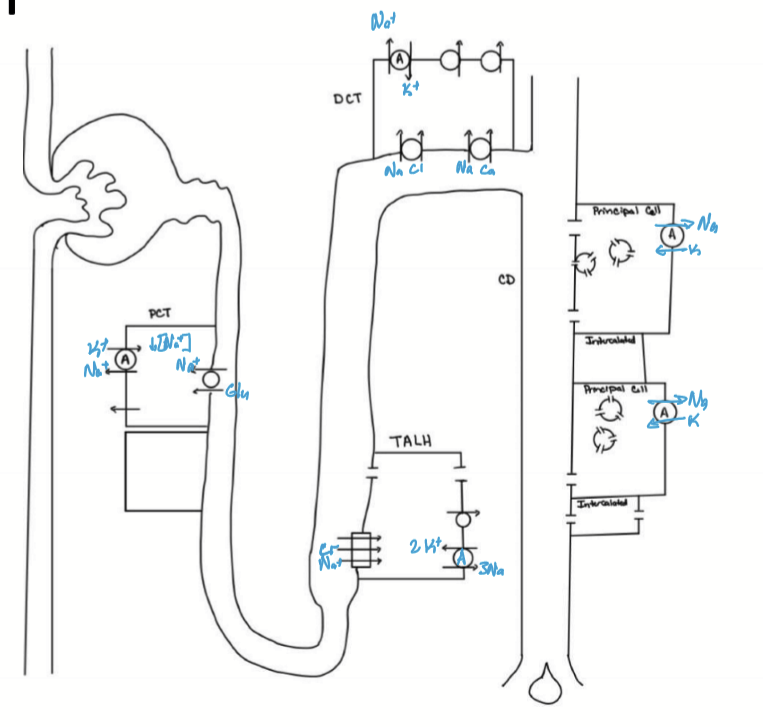
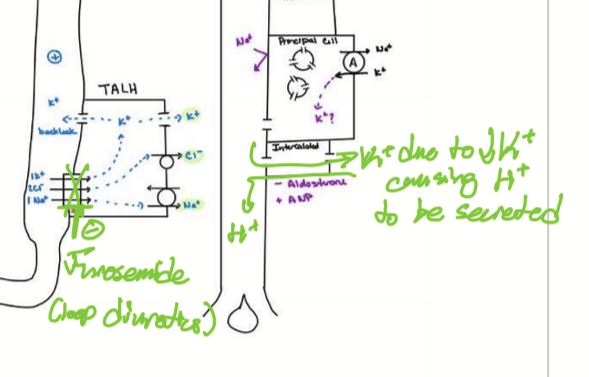
What happens in the thin ascending loop of henle?
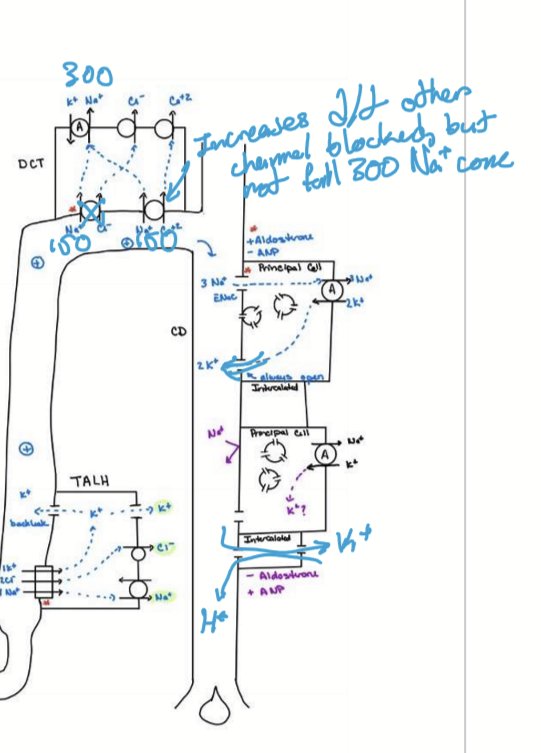
NKA on basolateral membrane pumps NA from cell into plasma
Na decreases in cell
Drives NKCC, bringing 1 Na, 2 Cl, and 1 K into the ISF (half of K is leaked back out)
Potassium back leak is responsible for “lumen positive”
Inner medullary interstitum increases to 600mOsm/L
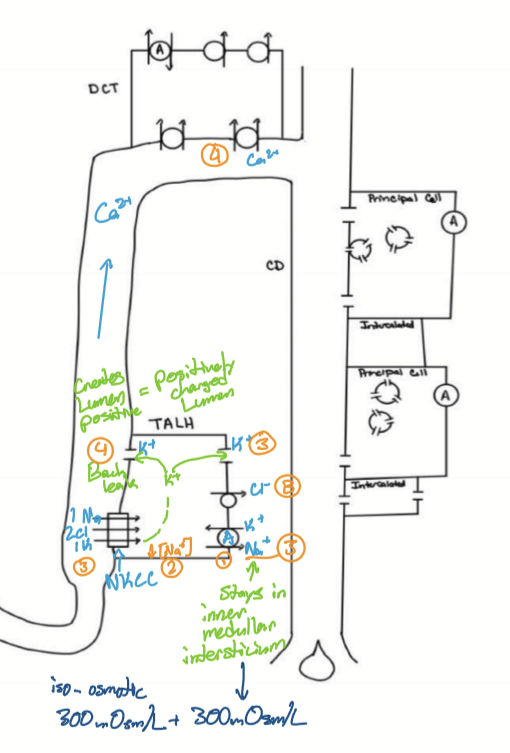
What is lumen positive used for?
Repelling Calcium in DCT to drive Ca reabsorption
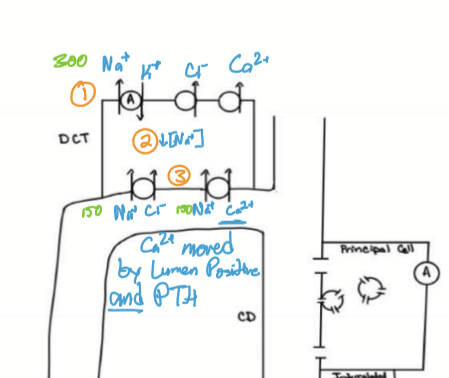
What happens in the DCT?
NKATPase decreases Na in cell to drive Na/Cl echanger and Na/Ca cotransporter
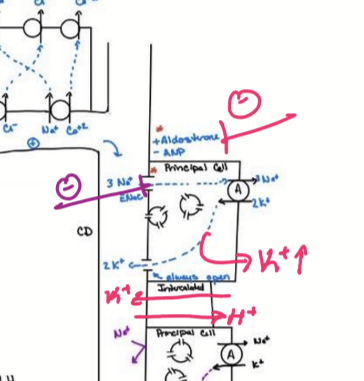
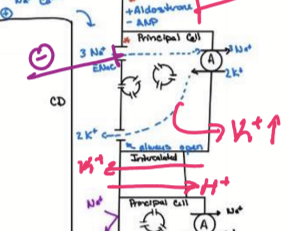
What happens in the CD with aldosterone?
With aldosterone, ENaC is inserted into apical membrane. NKATPase active on basolateral membrane pumps Na from cell into plasma, deriving 3 Na reabsorbed and 2K secreted. It causes an increase in BP, plasma osmolarity, and decrease in plasma K.
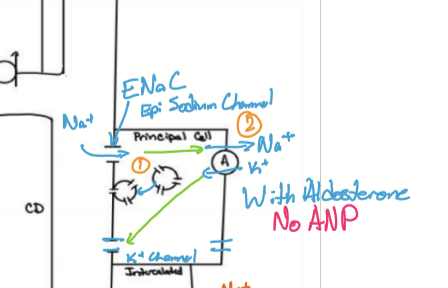
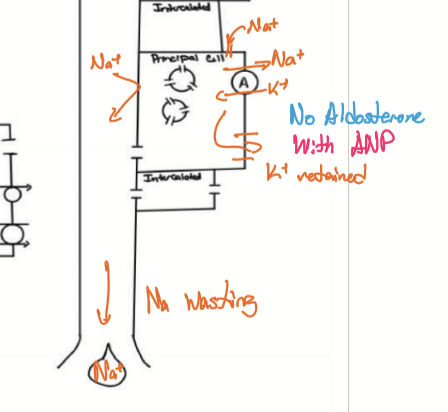
What happens in the CD without aldosterone?
Na wasted and K remains in plasma. Decreases BP, plasma osmolarity, and increases plasma K
Why is K important?
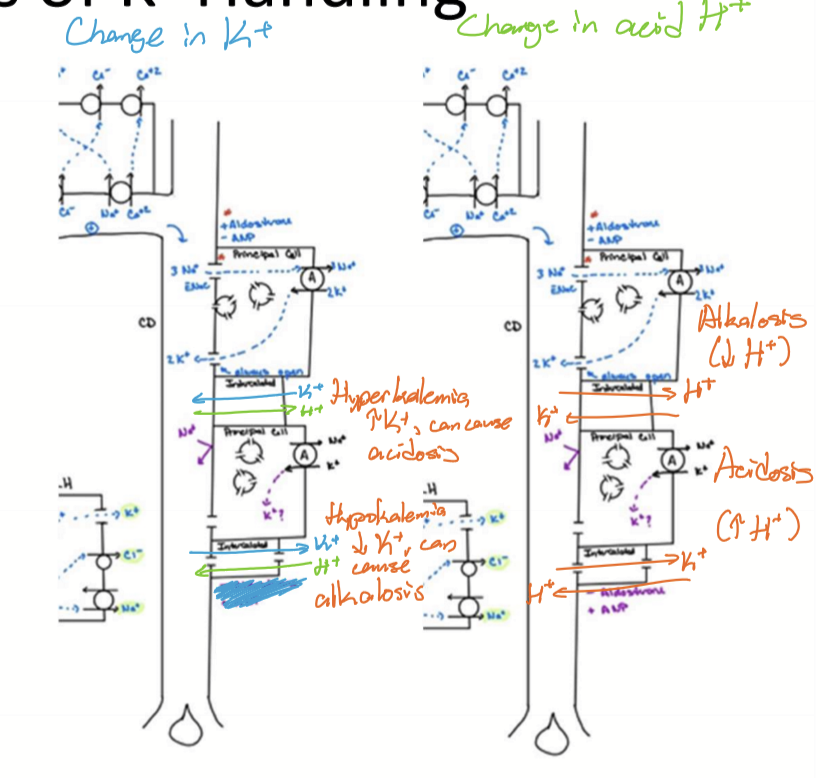
K is used in excitable cells: Nerve function, skeletal muscle fibers, pacemakers, and cardiac myocytes AND pH.
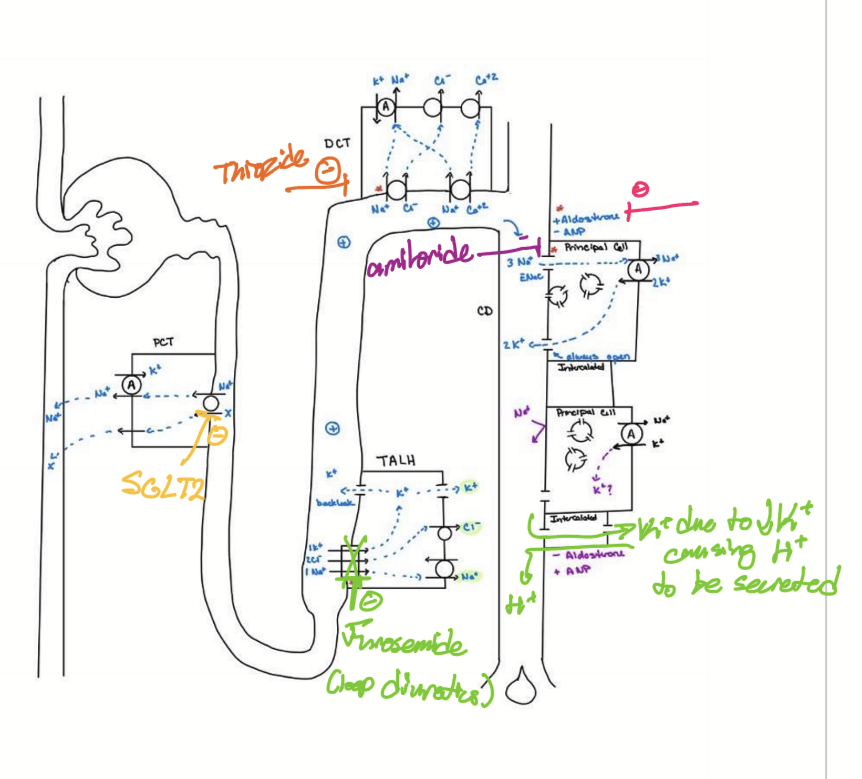
How do principal cells handle K?
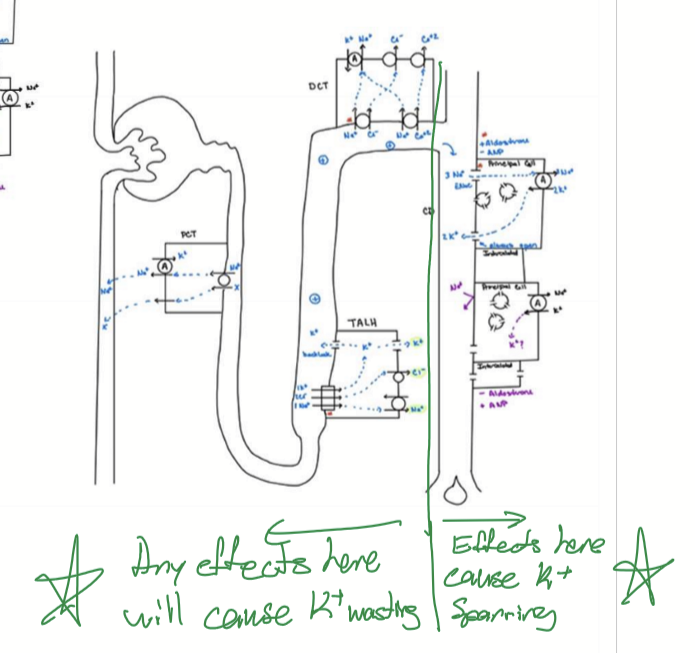
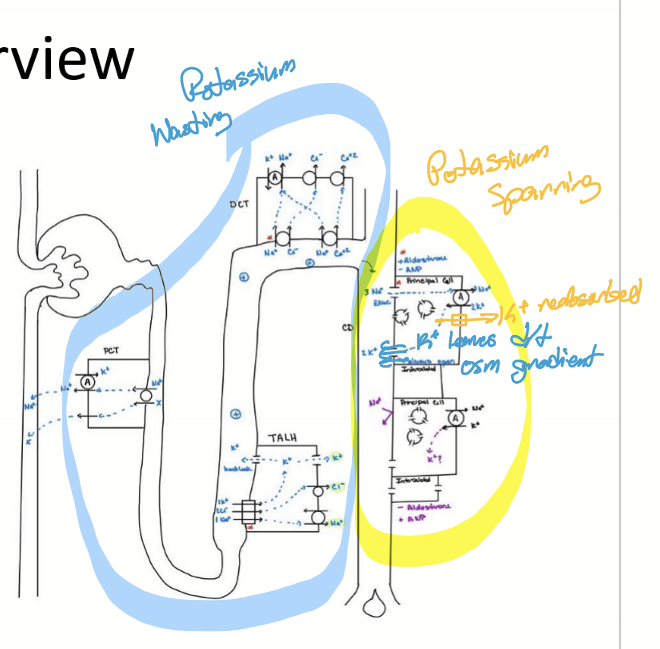
Aldosterone stimualtes K wasting. Diuretics targeting in CD causes K sparing. Diuretics targeting any other segment increases K wasting.
How does intercalated cells handle K?
In the CD, intercalated cells have bidirectional exchange of K and H. If hyperkalemia, K secretion and H reabsorption, can cause acidosis. If hypokalemia, K reabsorption and H secretion, can cause alkalosis. If acidosis, hyperkaemia. If alkalosis, hypokalemia.
What are some etiologies responsible for hyperkalemia?
Excessive K supplementation
Addison’s (low aldosterone)
Acidosis (acidemia) via activity of intercalated cells: like Diabetic keto acidosis
Type I DM: lack of insulin = less glucose in cell = less ATP = less K into cell via NKATPase
What is the importance of Calcium?
Bone
Synaptic transmission (neurons)
Muscle contraction (cardiac and smooth)
Pacemakers
Coagulation
How is Calcium handled in the kidneys?
In the DCT, TALH created lumen positive, and fine tuning done by parathyroid hormone.
What percentage of total body weight is water?
60%
How is water handled in the nephron?
Water is filtered freely and reabsorbed in PCT. In the DLH, it is freely exchanged. No water is moved in thin ascending loop of henle, Thick asending loop of henle, and distal convoluted tubule. ADH/AVP regulates water handling in CD.
What odes the counter current multiple from the DLH and TALH do to the medullary ISF?
Slight hyperosmotic, with a 300mOsm/L gradient.
What osmolarity will the vasa recta have compared to loop of henle?
The same. It mirrors the ISF.
How does Low ADH/AVP do for HTN?
Vascular effects:
Systemic vasodilation to decrease BP
Vasodilation of afferent arteriole causes increased filtration making more urine
Decreases water reabsorption in CD
CD is less permeable to water
Weak hyperosmotic gradient 300mOsm/L to 600 mOsm/L
Results in volume contraction and increased urine output
What do patients with low BP need to do?
Compensate by volume expansion via sparing/reabsorbing water.
How does high ADH/AVP work?
Vascular effects:
Systemic vasoconstriction to increase BP
Vasoconstriction of afferent arteriole: decreases filtration making less urine
Increases water reabsorption in CD
CD more permeable to water
Strong hyperosmotic gradient 300mOsm/L to 1200mOsm/L
Drives water reabsorption
Result: volume expansion (increases BP) and decreases urine output (hyperosmotic/concentration)
ADH/AVP increases water permeability how?
Causes aquaporin-2/Aqp-2 to be presented, allowing more water to be reabsorbed by increasing ISF osmolarity to 1200mOsm/L via Urea recycling through UT-1 transporters in CD.
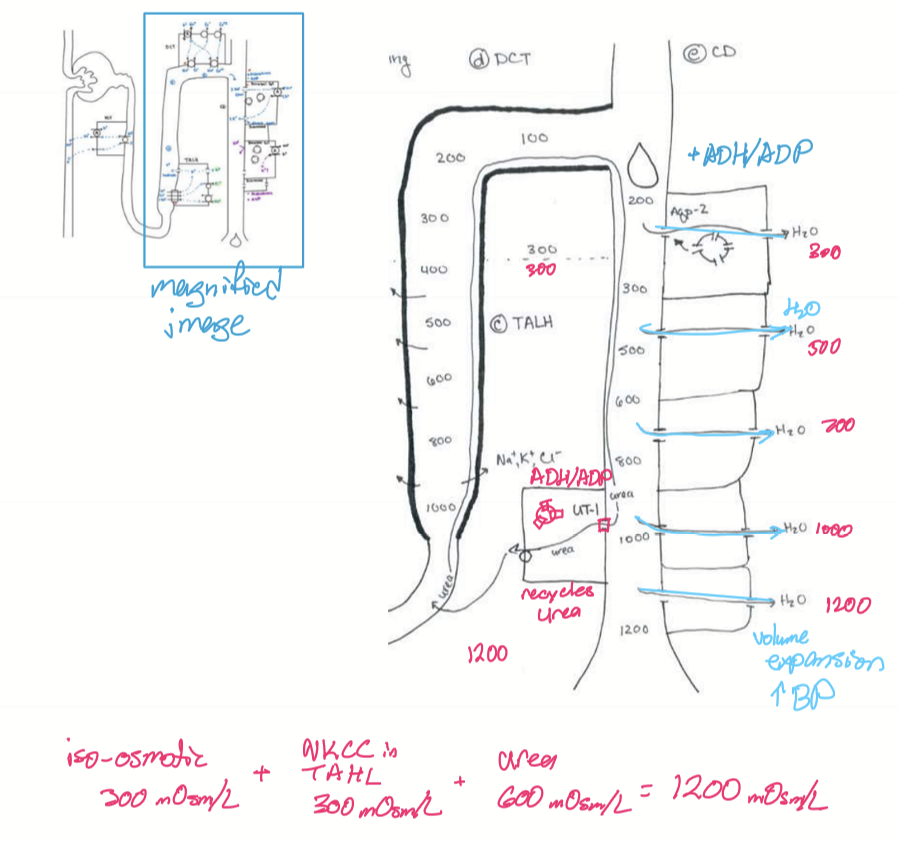
What is volume expansion associated with?
High ADH/AVP and risk of hypertensive retinopathy.
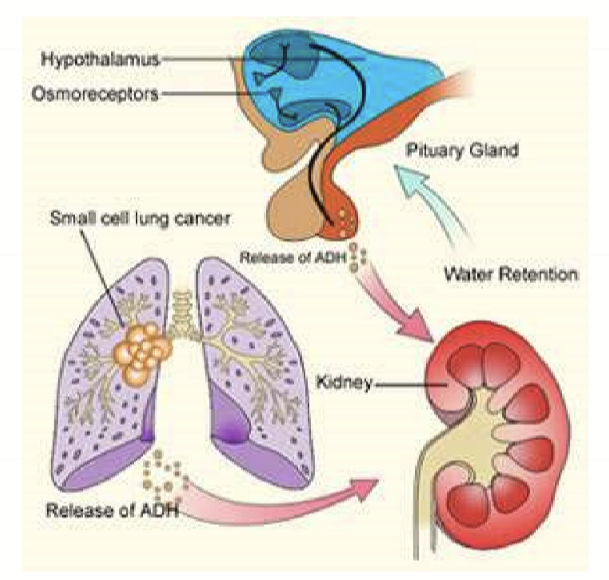
What is the etiology of high ADH/AVP?
Sydrome of inappropriate ADH/SIADH caused by complications of pituitary tumor or sign of small cell lung cancer.
What is associated with low ADH/AVP?
Volume contraction and dehyrdation
What can promote low ADH/AVP?
Alcohol and caffeine
Immature pituitary = low ADH/AVp released at night (why pee themselves when younger)
Diabetes insipidus: central diabetes insipidus (a pituitary issue) and nephrogenic diabetes insipidus (receptor issue)
Where are osmoreceptors located and what to they secrete?
Hypothalamus: ADH/AVP release
Adrenal cortex: aldosterone secretion
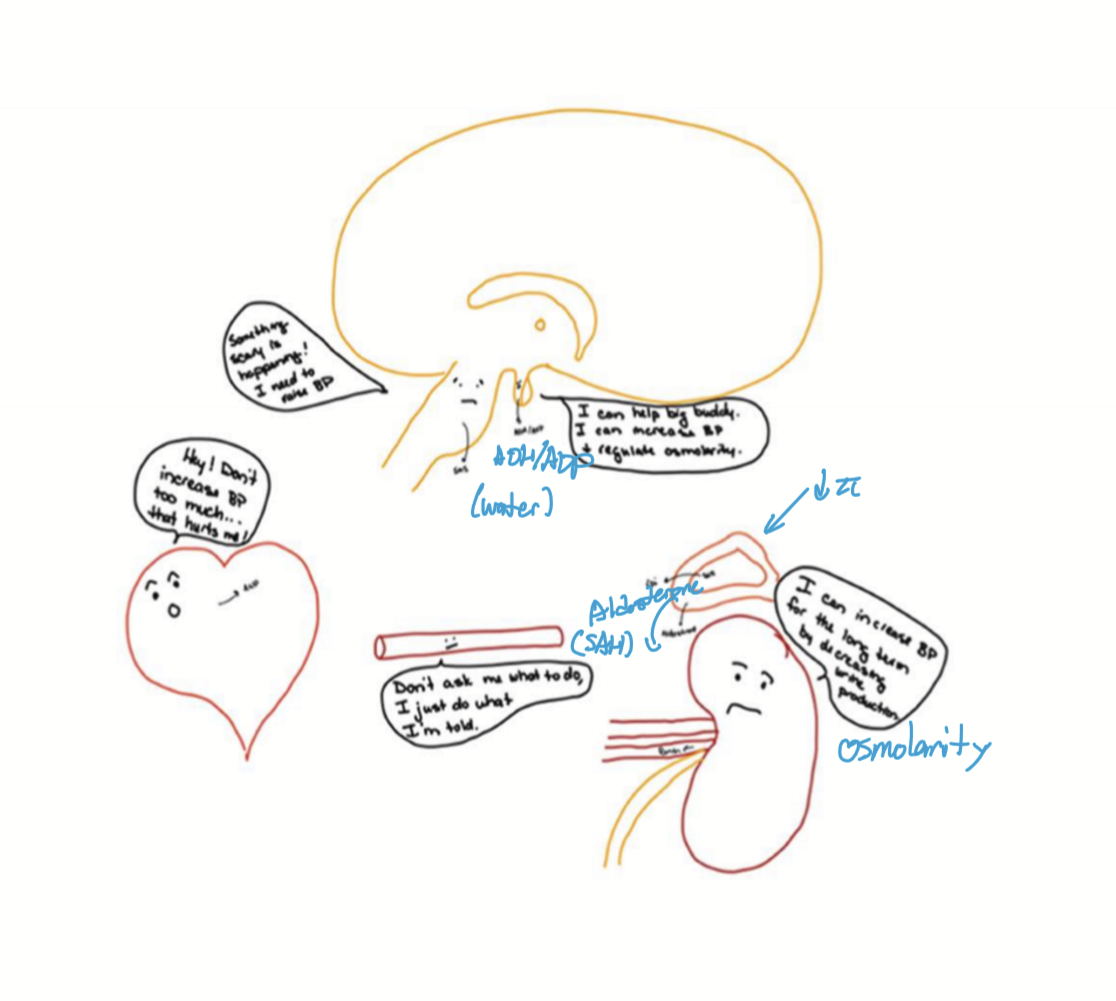
How is osmolarity balanced?
If hyperosmolarity: Decrease Na by decreasing aldosterone and increase water reabsorption via increased ADH/AVP
If hypo-osmolarity, Increase Na via increased aldosterone and decrease water via decreased ADH/AVP
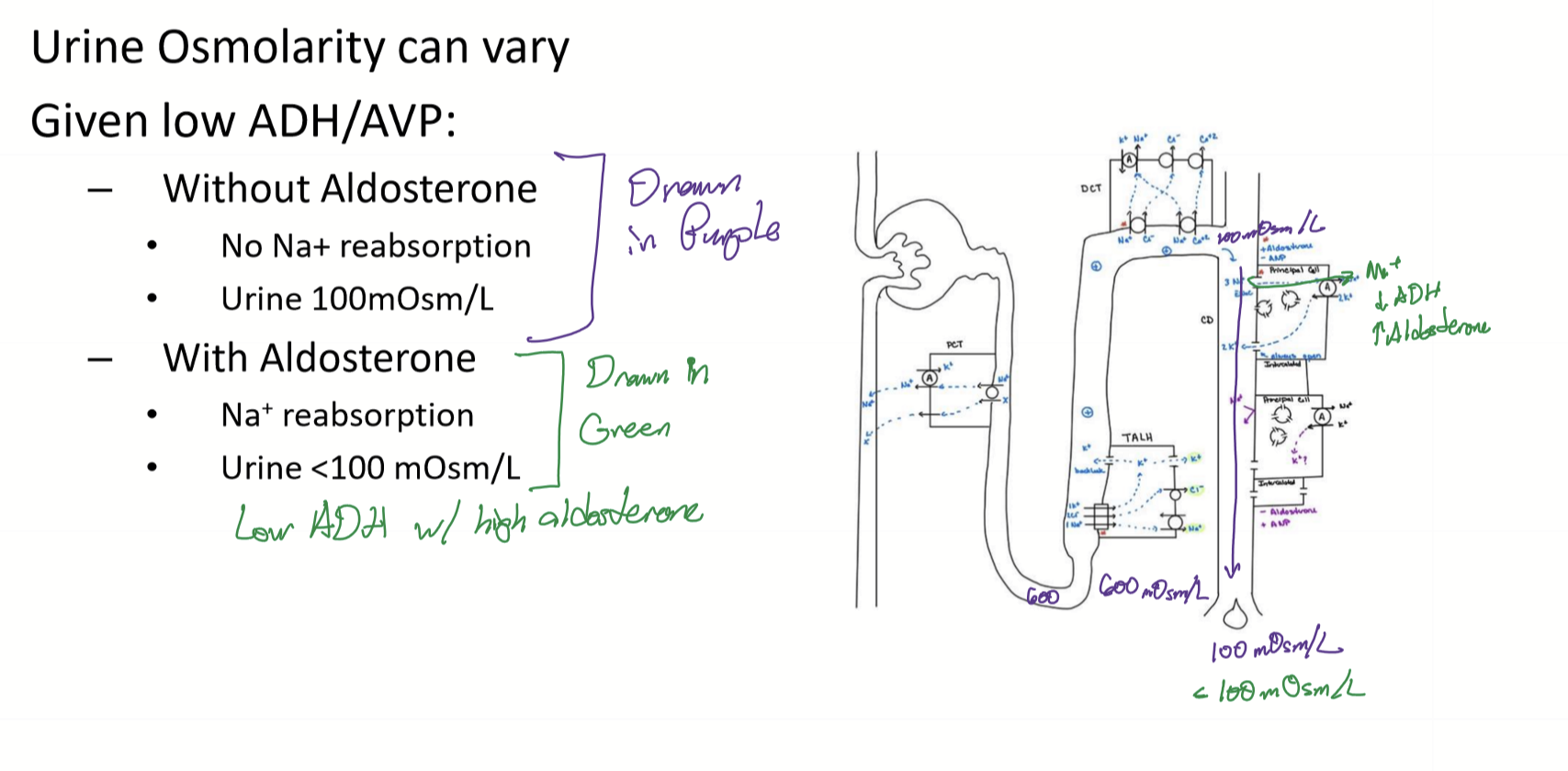
What is the osmolarity of urine with and without aldosterone?
Without aldosterone, no Na reabsorption and urine is 100mOsm/L
With aldosterone, Na reabsorption and urine <100 mOsm/L
(from 17c last slide)
What happens to renin secretion if BP is low?
Increased renin release to increase BP
How does Renin increase BP?
Activates ACE to convert Angiotensin I to angiotensin II. Ang II then cuases vasoconstriction, aldosterone release from adrenal cortex to reabsorb Na and water, and stimulates ADH to increase aquaporin-2 in CD.
What happens to renin if BP is high?
Macula densa senses chornically high salt in tubule and secretes messengers to inhibit the release of renin.
Does tubuloglomerular feedback regulate BP?
No, it regulates GFR.
How can GFR be increased?
Decreased Cl in DCT is sensed by macula densa, causing PGE2 to be secreted to vasodialte the afferent arteriole to increase GFR.
What are diuretics used to treat?
HTN
Edema
Heart failure
What do diuretics do?
Target nephrons to decrease BP by shifting fluids into urine to coause volume contraction and increase urination
What do most diuretics target?
Apical transporters to cause an increase in salt in tubule and therefore osmotic diuresis
What diuretics are K wasting?
Diuretics that target cells in the PCT, TALH, and DCT.
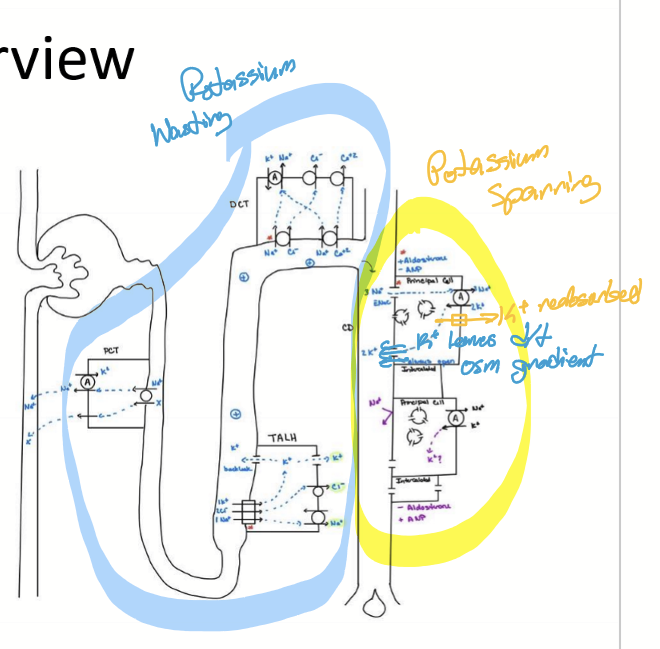
What diuretics are K sparing?
Diuretics that target cells in the CD.
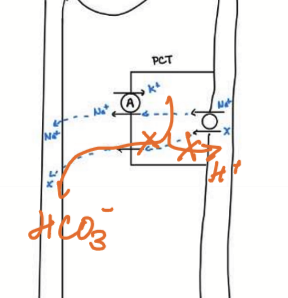
Where do Carbonic Anhydrase Inhibitors work?
Carbonic anhydrase in PCT/proximal convoluted tubules
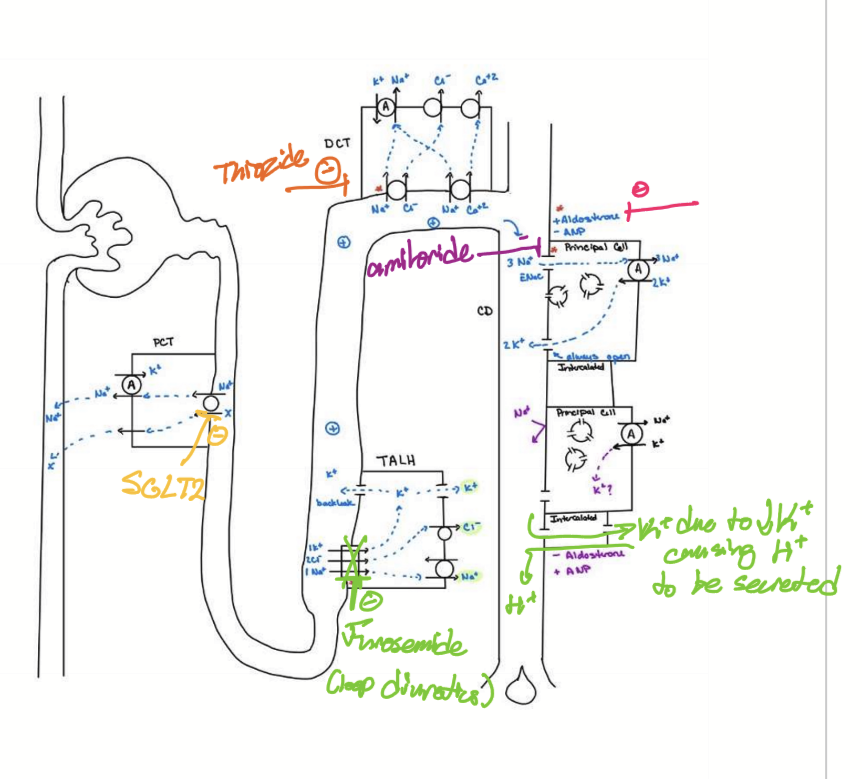
Where do Loop diuretics work/target?
NKCC in TALH/thick ascending loop of henle
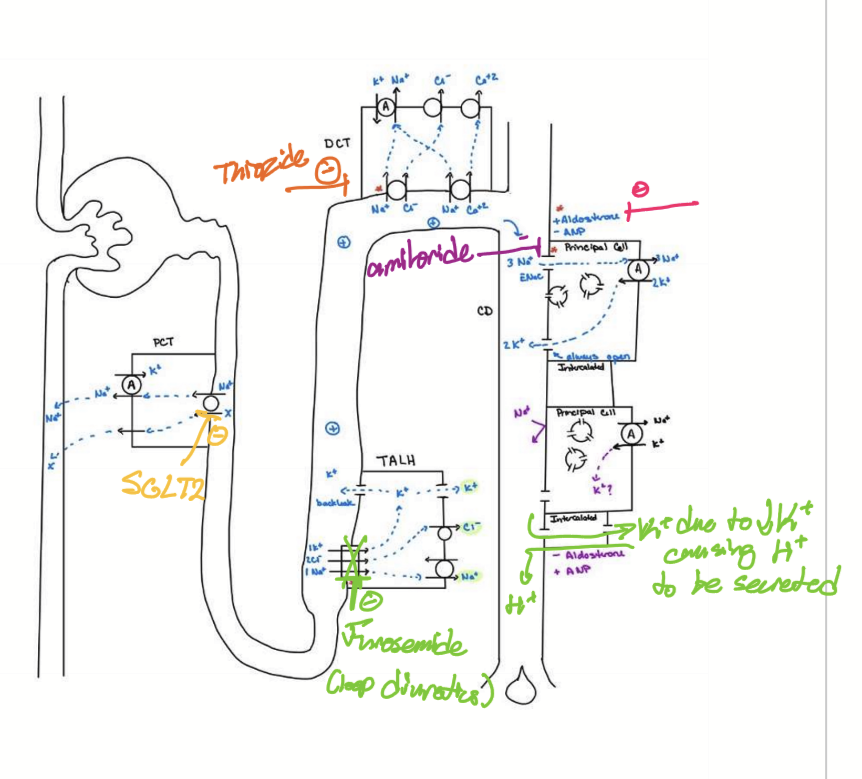
Where do thiazides work/target?
Na/Cl co-transporters in DCT
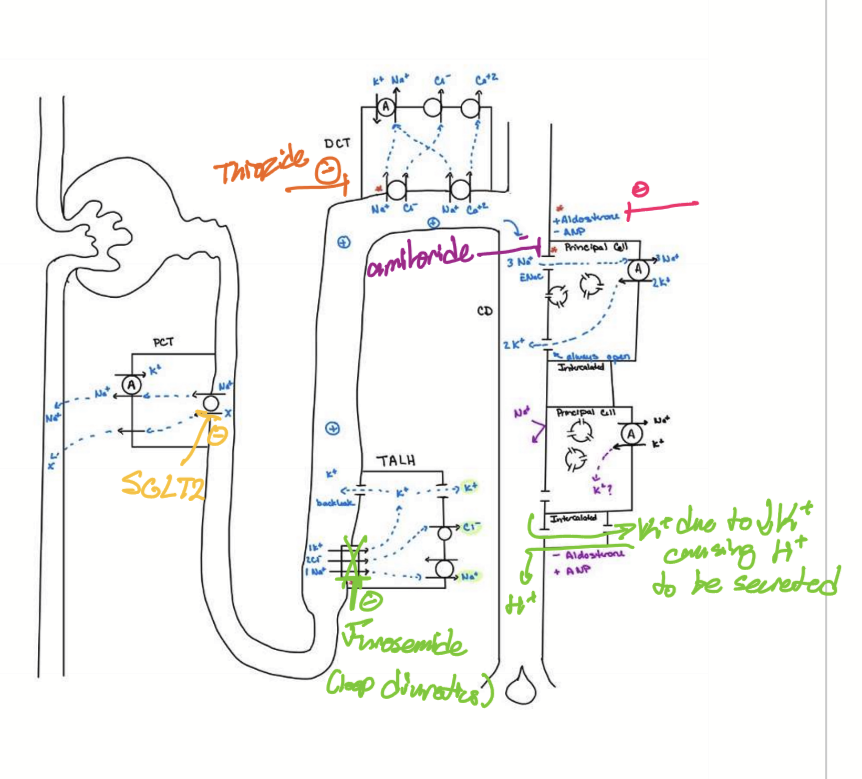
Where do potassium-sparing diuretics work/target?
Aldosterone receptor in CD (reduces number of ENaC/epithelial sodium channel) or ENaC itself in CD
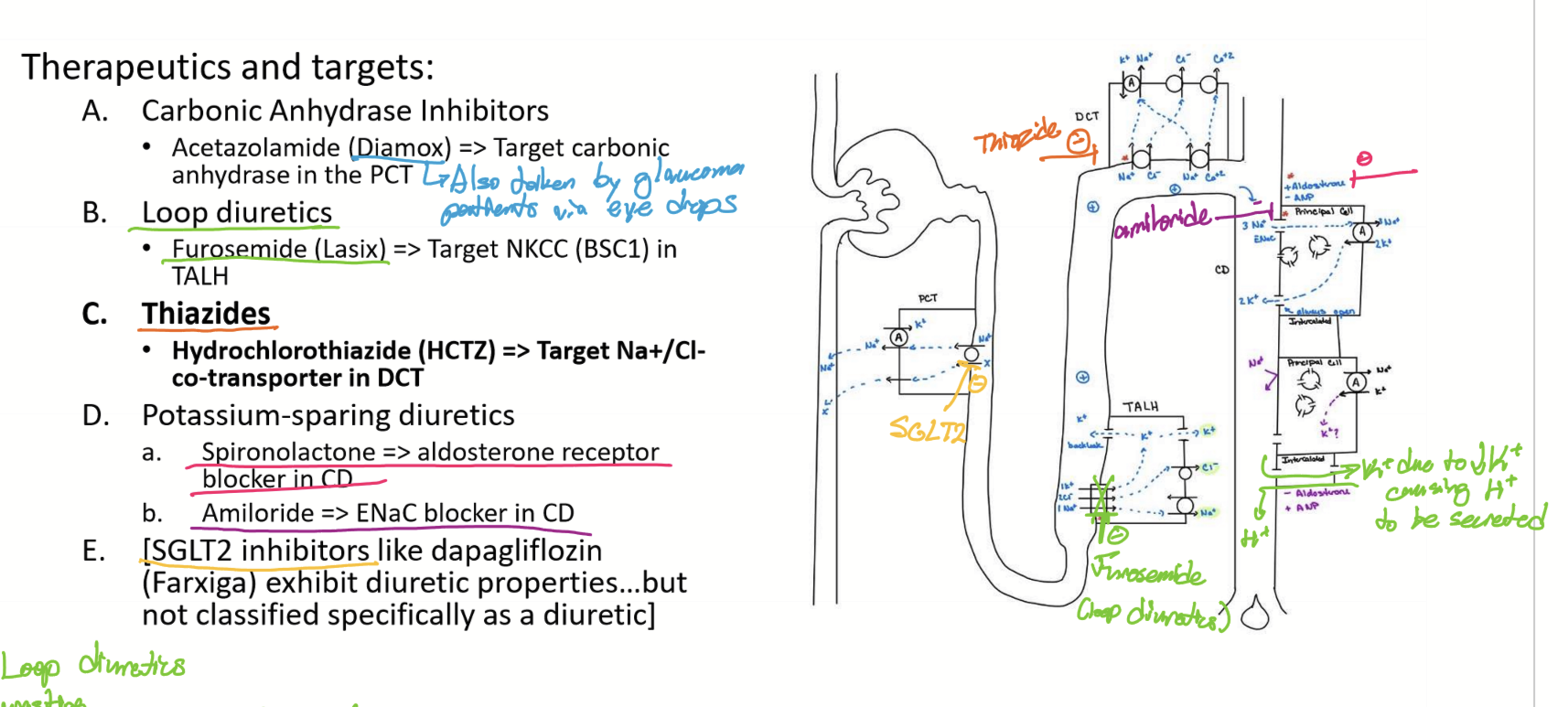
Where do SGLT2 inhibitors work/target?
In PCT on Na cotransporters.
What is the effects of Acetazolamide (Diamox)?
Since target Anhydrase in PCT, no H secreted, Na wasting, K wasting, no change on Ca, acidosis, water wasting, and decrease BP
What are the effects of Furosemide (Lasix)?
Targets NKCC (BSC1) in TALH, causing Na wasting, K wasting, Ca wasting, alkalosis, water wasting, and decrease BP
When is Furosemide/Laxis given?
To people with high CSF to reduce CSF production (uses NKCC also)
What are the effects of Hydrochlorothiazide (HCTZ)?
Target Na/Cl cotransporter in DCT, causing Na wasting, K wasting, Ca sparing, alkalosis, water wasting, and decrease BP
What are the effects of Spironolactone?
Blocks Aldosterone receptor in CD, causing Na wasting, K sparing, no change to Ca, acidosis, water wasting, and decrease BP
What are the effects of Amiloride?
Blocks ENaC in CD, causing Na wasting, K sparing, no change to Ca, acidosis, water wasting, and decrease BP
What are the effects of Dapagliflozin (Farxiga)?
Inhibits SGLT2, causing Na wasting, K wasting d/t high fluid, no change to Ca, alkalosis, water wasting, and decrease BP
What is the normal pH range of the body?
7.37 to 7.43
What is considered acidosis?
pH < 7.37
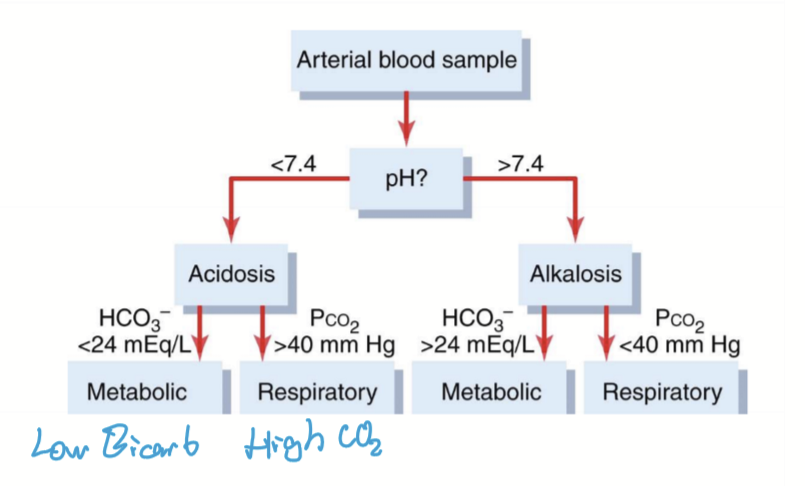
What is considered alkalosis?
pH > 7.43
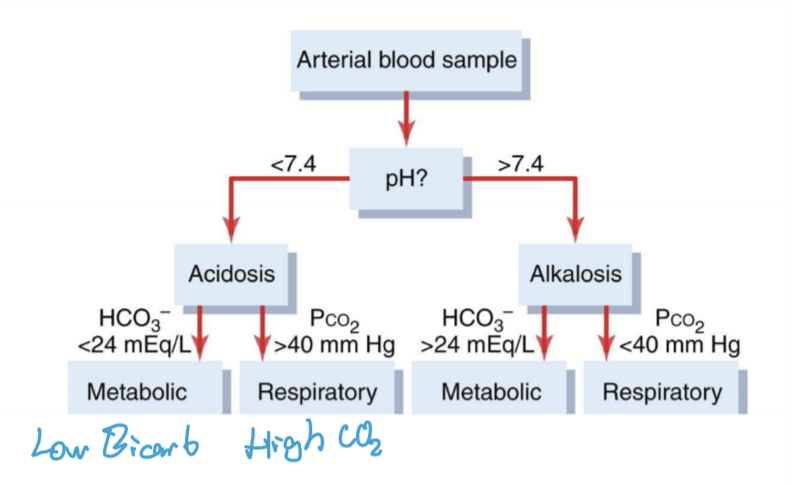
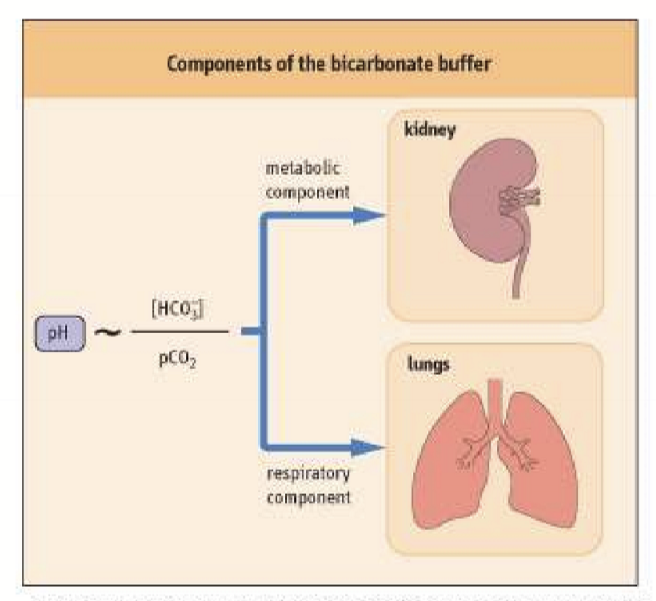
How does the body compensate for acid-base imbalances?
Bicarbonate buffer
Lungs
Kidneys
Can compensation of pH imbalances cause new acid/base imbalances?
yes
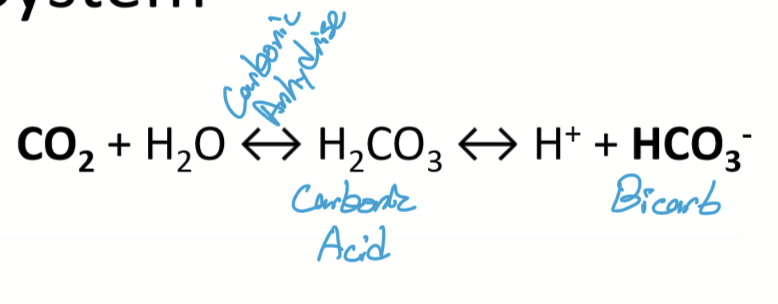
What system instantaneously responds to a pH imbalance?
Carbonic acid buffer system. CO2 is acid and Bicarbonate is base.
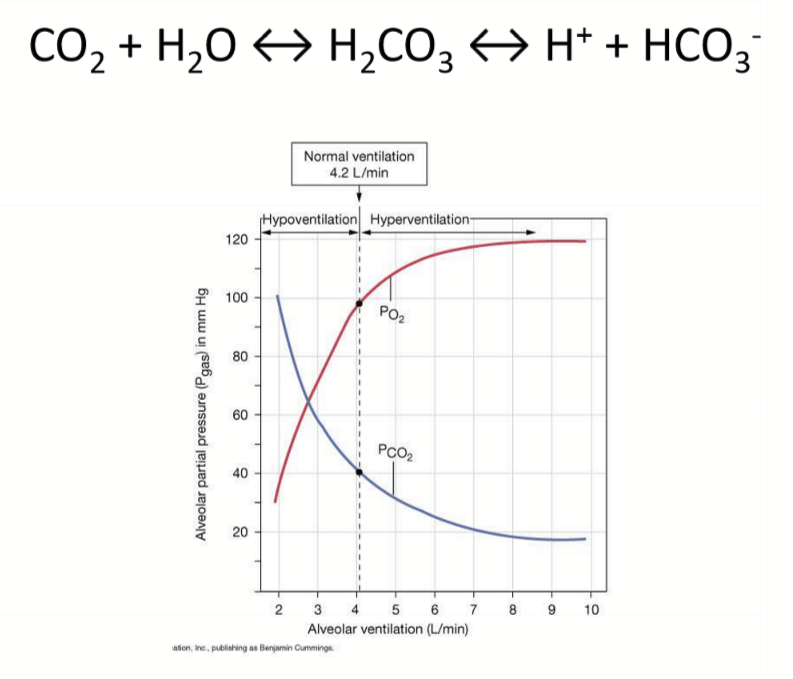
How does the respiratory system respond to acidosis?
Since acidosis/high CO2/low HCO3-, increase ventilation to decrease CO2
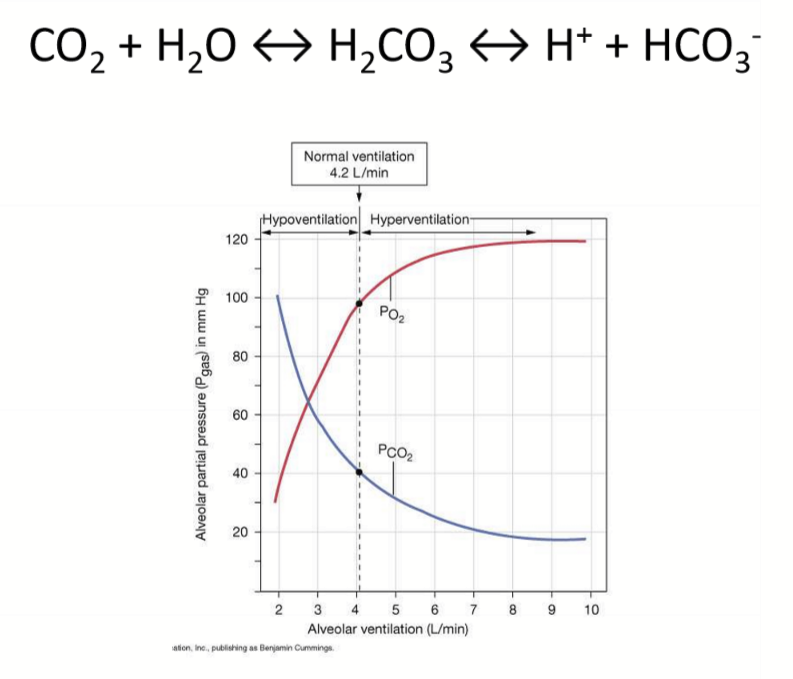
How does the respiratory system respond to alkalosis?
Since alkalosis/low CO2/high HCO3-, decrease ventilation to increase CO2
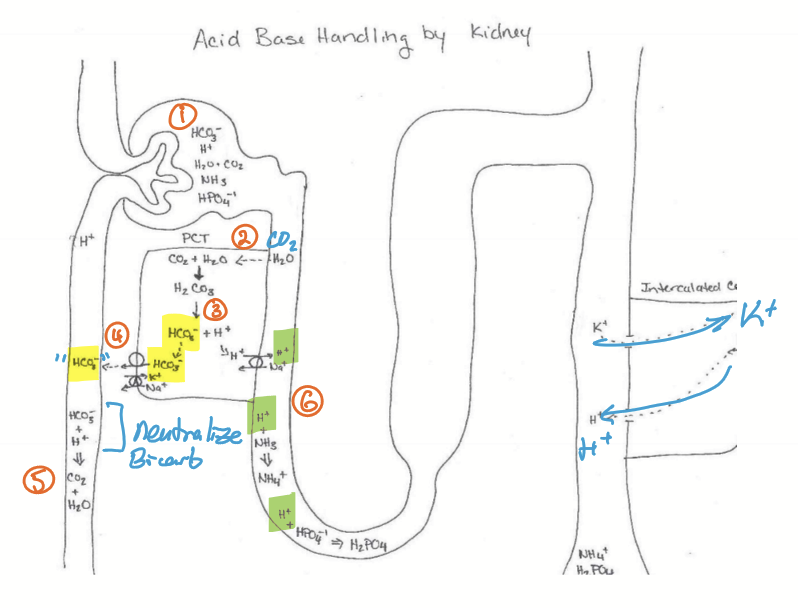
How do the kidneys regulate to maintain blood pH?
H+ and HCO3-. Regulation occurs hours to days and is more long lasting
Where is the acid/base imbalance handled in the kidneys?
Intercalated cells in the PCT by absorbing or secreting H+, will cause K imbalances. Some HCO3- handling in the PCT also.
How does the kidneys handle alkalosis?
In PCT, cells do not reabsorb HCO3 and secrete H+. Intercalated cells reabsorb H+ and secrete K+.
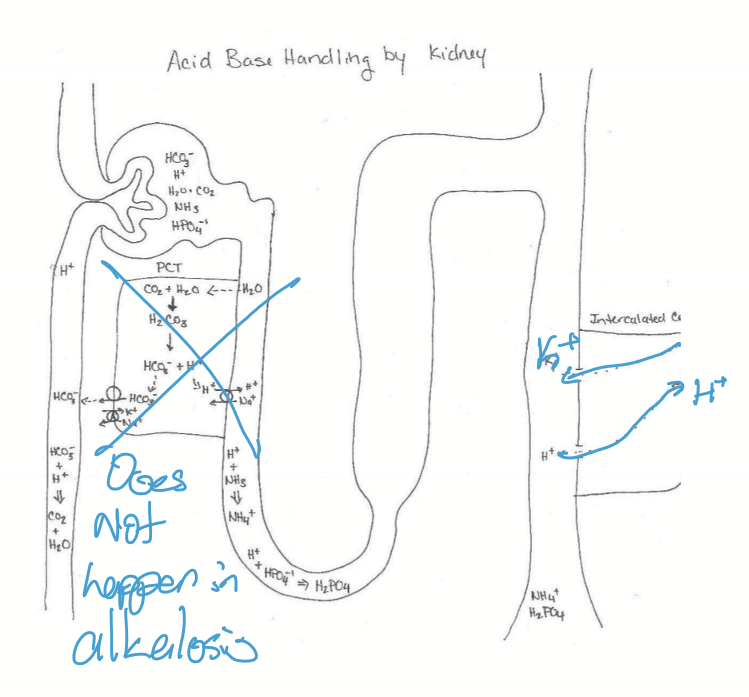
How does the kidneys handle acidosis?
In PCT:
HCO3- is reabsorbed and reacts with H+ in blood to form CO2 and H2O
H+ is secreted into lumen and is buffered
NH3 + H+ < - > NH4+
HPO4 + H+ < - > H2PO4+
Intercalated cells:
Secrete H+
Reabsorb K+
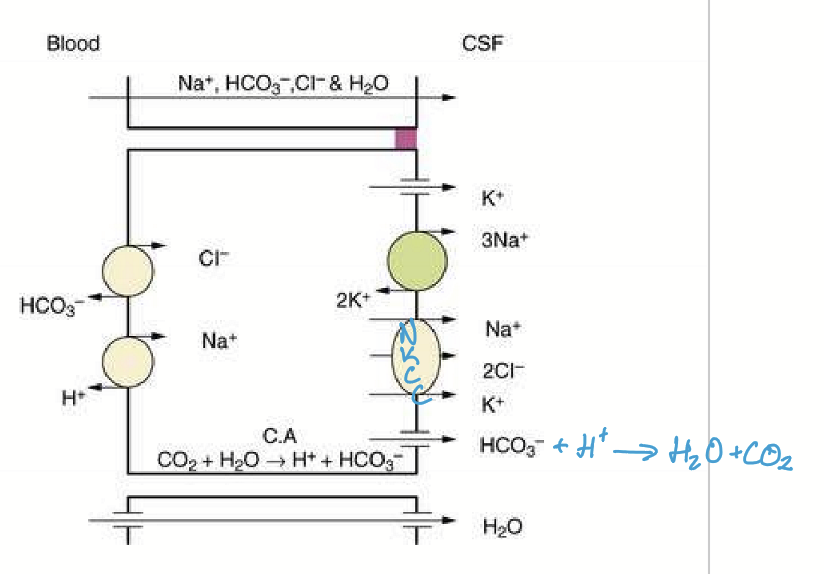
What other system uses NKCC to move water using bicarbonate?
Production of CSF and Aqueous Humor.
How is NKCC stimulated in the eye for AH production?
Beta 2 by Epi and NorE.
How is AH produced in the posterior chamber?
HCO3-, made from CO2 + H2O, is secreted into the chamber and combines with H+ to make water.
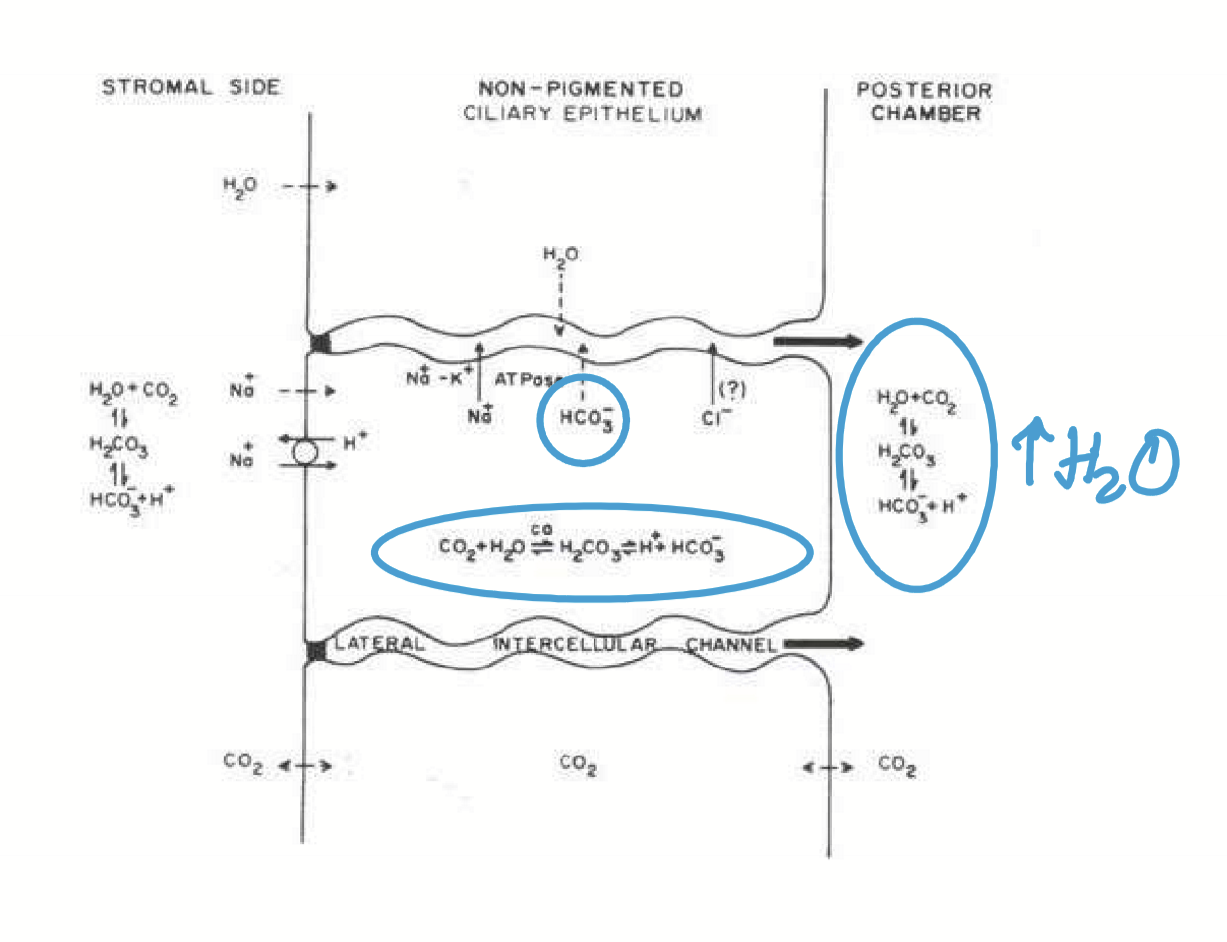
What treatments can be used to decrease IOP?
Carbonic anhydrase inhibitor (Acetazolamide or Diamox) or beta blockers can be used to treat glaucoma.
What is respiratory acidosis?
When the lungs fail to eliminate sufficient CO2, leading to a buildup of acid in the blood and a drop in blood pH.
What is respiratory alkalosis??
When the lungs removes too much CO2, causing a decrease in CO2 levels and an increase in blood pH.
What is lactic acidosis?
A condition in which the body produces too much lactic acid, leading to a decrease in the blood’s pH level.
How does the body respond to respiratory acidosis?
High CO2, so:
Lungs increase ventilation rate
In PCT, reabsorb HCO3- and secrete H+
In CD, secrete and excrete H+ and reabsorb K+
What is the etiology for respiratory acidosis?
Respiratory Disease
How does the body respond to respiratory alkalosis?
Low CO2, so:
Lungs decrease ventilation rate
In PCT, decrease reabsorption of HCO3-
In CD, reabsorb H+ and secrete K+
What is the etiology of respiratory alkalosis?
Hyperventilation
How does the body respond to metabolic acidosis?
Low HCO3-, so:
Increase ventilation rate
PCT reabsorb HCO3- and secrete H+
CT secrete H+ and reabsorb K+
What is the etiology of metabolic acidosis?
Loss of HCO3- = carbonic anhydrase inhibitors, diarrhea
Increase in H+ = aspirin, lactic acid, ketoacidosis
How does the body respond to metabolic alkalosis?
High HCO3-, so:
Increase ventilation rate
PCT: decrease HCO3- reabsorption and H+ secretion
CT: Reabsorb H+ and secrete K+