bio 224 exam 4
1/76
Earn XP
Description and Tags
urinary system
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
77 Terms
About how much can you have missing from this organ system while still having it function?
You can have up to 75-80% of the organs (the kidneys) missing & it’d still function!
functions of the urinary system (4 total) (it’s all about fluid regulation!)
regulating blood…
volume
contents
concentration
blood pressure
Make EPO (hormone)
Make renin (enzyme)
Excretion of waste (in urine)
Kidney location
It’s retroperitoneal (behind the peritoneum)
Anchored to the dorsal body wall T12-L3 by some adipose
Ptosis
When a kidney slumps. This can kink up the hoses & lead to death.
Often caused by severe loss of conn. tissue
Kidney anatomy (9 structures/parts to list) (list the length & weight as well!)
5” tall & 130g
Renal Cortex- the outer part
Renal Medulla- the inner part.
Renal pyramid- the triangle shaped part of the medulla.
Papilla- the tip of the pyramid. This is where urine comes out
Renal column- the structure between the renal pyramids
Minor calyx- the channel coming from just one pyramid
Major calyx- where 2 or more minor calyces meet
Renal pelvis- where all the major calyces meet
Hilum- dent in the organ that tubes go in & out of
What percentage of your body’s blood is in your kidneys?
About 25%
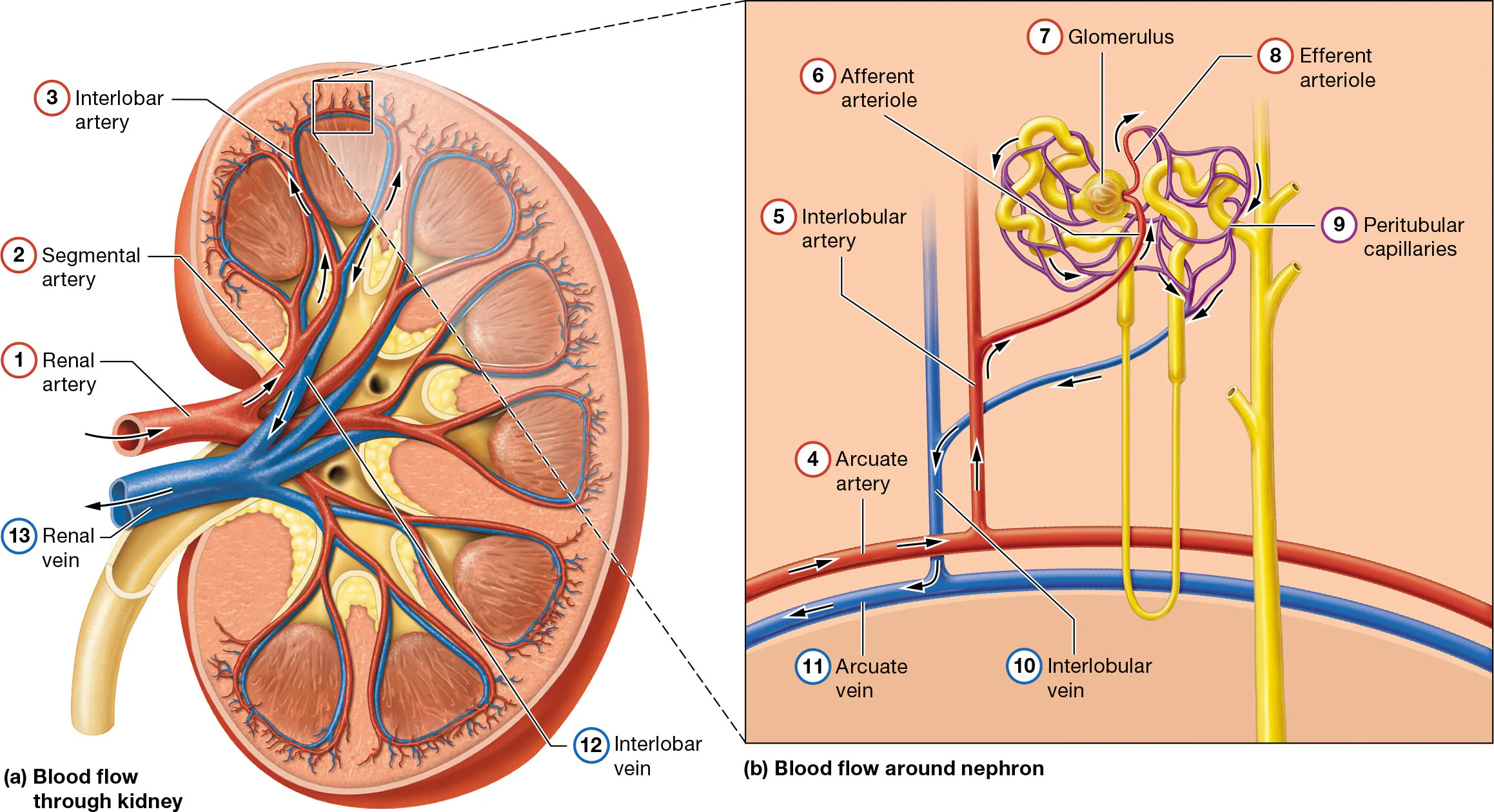
Blood flow in the kidneys (13 parts)
Renal artery
Segmental artery
Interlobar artery
Arcuate artery
Cortical radiate artery
Afferent arteriole
Glomerulus (a capillary bed where no gas exchange occurs since an arteriole goes out)
Efferent arteriole
Peritubular capillaries (perform gas exchange)
Cortical radiate vein
Arcuate vein
Interlobar vein
Renal vein
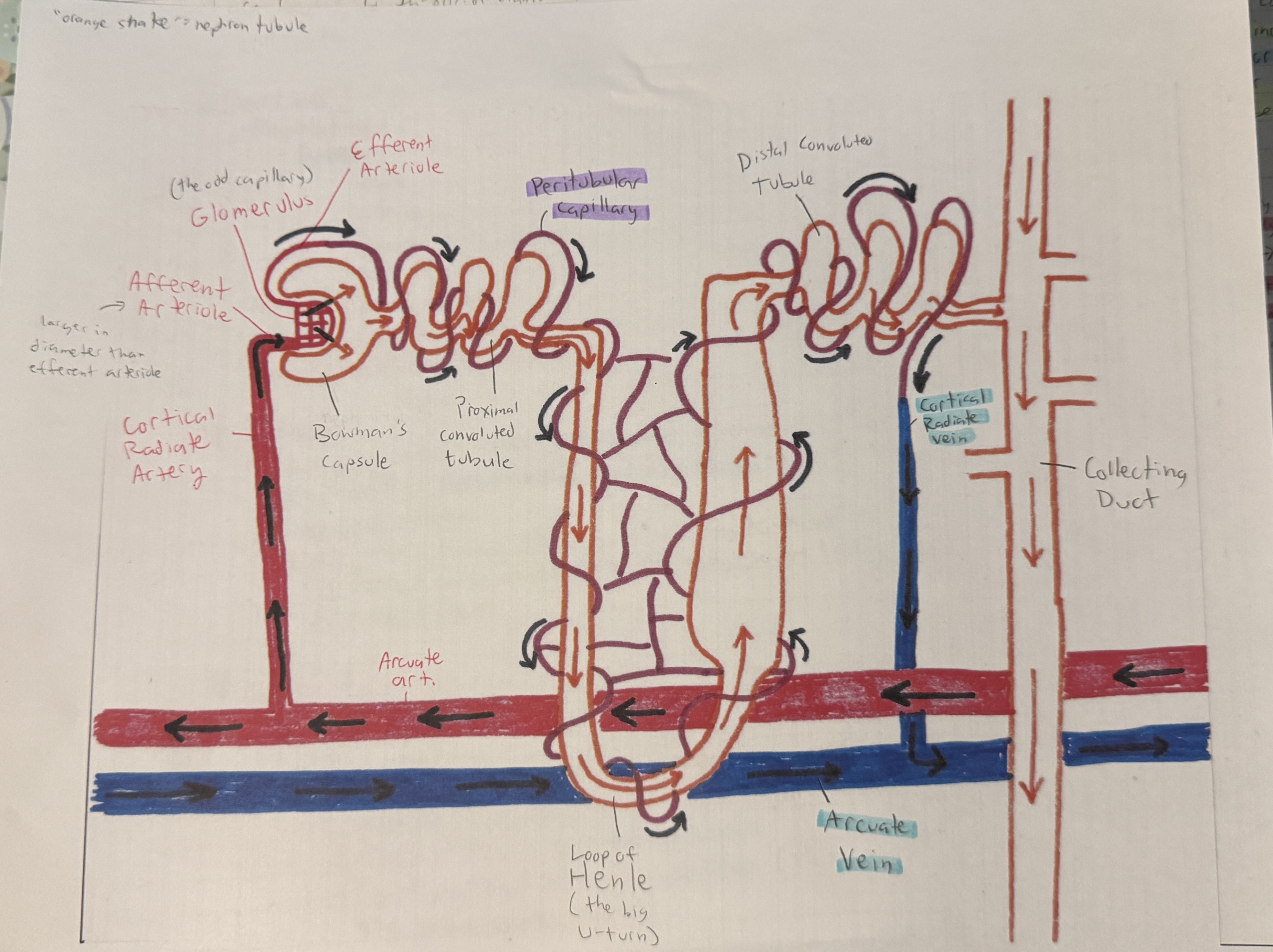
Nephron
The functional unit of the kidney
It’s the tubule & all the blood vessels associated with it from the arcuate artery to the arcuate vein)
We have about 2.6 million nephrons in our body
Anatomy of the nephron tubule (snake shaped part) (5 parts)
Bowman’s capsule- the “snake head” of the nephron tubule
Proximal convoluted tubule- the “neck” of the “snake”, connected to the head with many turns
Loop of Henle- the “large U-turn”
Distal convoluted tubule- the twisty end of the “snake” with the end connecting to the collecting duct
Collecting duct- the duct at the end of the “snake”
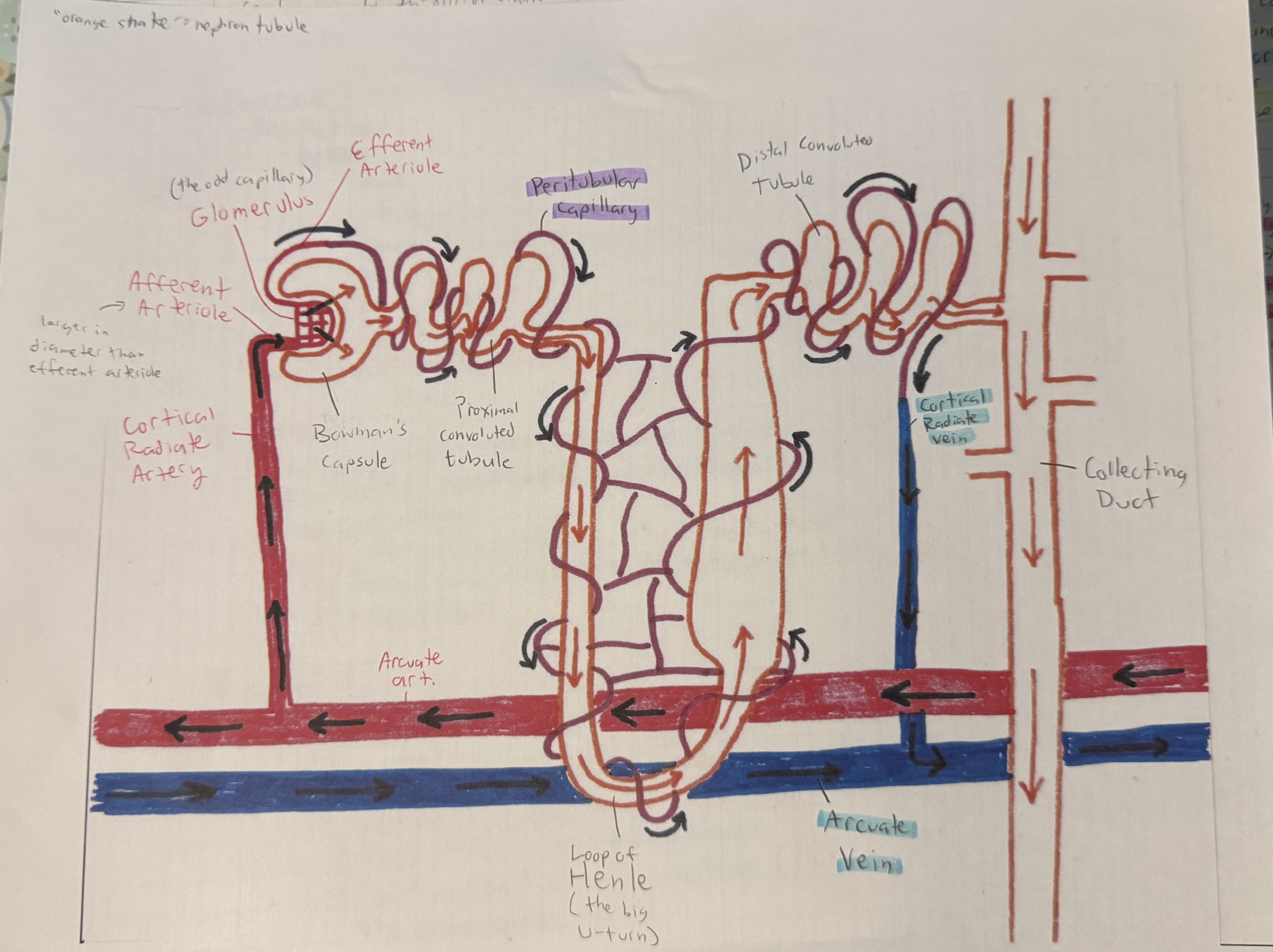
Blood vessels of the nephron (8 parts)
Arcuate artery
Cortical radiate artery
Afferent arteriole (larger in diameter than the efferent arteriole)
Glomerulus (the odd capillary in the “mouth” of the snake)
Efferent arteriole
Peritubular capillary
Cortical radiate vein
Arcuate vein
3 processes in a nephron & where they occur. What do these processes form?
Filtration= F (occurs in glomerulus & Bowman’s capsule) (the renal corpuscle)
Reabsorption= R (Proximal convoluted tubule, Loop of Henle, & Distal Convoluted Tubule/Collecting Duct) (or PCT, LH, & DCT/CD)
Secretion= S (Proximal convoluted tubule & Distal Convoluted Tubule/Collecting Duct) (or PCT & DCT/CD)
these processes form URINE
What process(es) occur(s) in Bowman’s Capsule & Glomerulus (BC & G)? (these two are part of the renal corpuscle)
filtration. F
What process(es) occur(s) in Proximal Convoluted Tubule (PCT)?
mostly reabsorption & some secretion. Rs
What process(es) occur(s) in Loop of Henle (LH)?
reabsorption. R
What process(es) occur(s) in Distal Convoluted Tubule/Collecting Duct (DCT/CD)?
Reabsorption and/or secretion, depending on our needs. R and/or S
This is where variability occurs
note: DCT & CD are anatomically different structures, but physiologically the same unit
filtrate
fluid in the nephron tubule. Formed after filtration
filtration, reabsorption & secretion
Filtration- the glomerulus leaks since it’s a capillary (all capillaries leak all the time). Plasma leaks out of blood into Bowman’s Capsule, which has holes in it. These holes in BC allow for filtration
Reabsorption-reabsorb things from filtrate (fluid in nephron tubule) into tubule (in peritubular capillary)
Absorb something that was previously lost, thus absorbing it a second time
Secretion- secrete from blood into filtrate
What enters & exits from the nephron tubule?
Blood plasma enters thru the renal corpuscle (BC & G)
Urine exits thru the collecting duct (CD)
Types of nephrons (2 types. List general location & percentages)
Cortical nephrons- makes up 80-85% of our nephrons. These are mostly in the cortex
Juxtamedullary nephrons- makes up about 15% of our nephrons. These dip way down into the medulla
Filtration (Define filtration & 4 terms/structures to know associated with it)
Filtration- blood plasma moving from bloodstream into nephron through holes
Only occurs at glomerulus & Bowman’s capsule
BC wraps around Glomerulus, like a catcher’s mitt wrapped around a ball
Podocytes- inner layer of BC. covers up glomerulus & lays against the capillary. This is where filtration occurs
Filtration slits- gaps in the BC, between podocytes
Fenestrations- little holes in blood vessel.
Filtration membrane- found where the fenestrations & filtration slits are
Filtration pressures (list the forces that favor & oppose filtration & the net filtration pressure)
blood side 50mmHg→ ←40mmHg filtrate side
Force favoring filtration (making filtrate): BP→ 50mmHg (pushing from blood to filtrate)
BP in glomerulus: 50 mmHg pushing out plasma out of the glomerulus
Forces opposing filtration (don’t want to make filtrate): 40mmHg← osmotic pressure of G & fluid pressure of BC (pushing from filtrate to blood)
Fluid pressure of BC: 30mmHg
Osmotic pressure of G: 10 mmHg
Net filtration pressure (NFP): 10mmHg → (drives fluid out of glomerulus).
Favoring filtration wins, but not by much
Glomerular filtration rate (How much do we filter per minute & per day?)
125ml/min
180L/day
This is how much filtrate we make (not urine. We make less urine than filtrate)
Caffeine’s effect on urine volume
Consuming caffeine increases BP, so the 50mmHg pushing to make filtrate (force favoring filtration) increases. This causes more filtration & more urination
What are the “big stars” of reabsorption & secretion?
Na+ & H2O
Water follows Na+, when it can when it’s allowed (when the cell membrane permeability lets it)
How is sodium reabsorbed? Water? (Includes structure for water to get through the CM)
Sodium
is reabsorbed by pumping it (active transport)
It gets pumped in, then pumped out into blood. The more the pumps work, the more sodium we get in blood.
This blood in the peritubular capillary becomes very concentrated, so it’ll pull on water thru osmosis
Water
follows sodium by diffusion/osmosis when cell membrane permeability allows
Aquaporins- Proteins that are tunnels for water in the cell membrane.
Water can only follow sodium by entering aquaporins since the CM is made of lipids
How does glucose get reabsorbed?
Glucose gets co-transported with sodium. In other words, it hitches a ride with sodium as it gets pumped
Reabsorption percentages for the PCT (4 items to list)
65% of H2O
65% of Na+
100% of glucose, amino acids, & other organic solutes (thru cotransport with Na+)
If glucose/proteins/etc. are found in urine, this can indicate an issue with the kidney (the PCT specifically) since it should reabsorb all of it
90% of HCO3- (bicarbonates)
Can you get water out of the Loop of Henle? If so, what’s the catch?
Yes, you can get H2O out of the Loop of Henle, but it’ll be more difficult
The Countercurrent system in the Loop of Henle (aka the “Double Whammy!”)
Descending Limb
Has PCT leading into it & filtrate moves down
Thinner
IS permeable to water (has aquaporins)
Reabsorbs 25% of H2O
Ascending limb
Leads out into DCT & filtrate moves up
Thicker
NOT permeable to water (has no aquaporins)
Pumps out Na+ & Cl- (chlorine)
Reabsorbs 25% of Na+ & Cl-
Sodium gets pumped out into the trough (area between each limb) & makes it more concentrated, so the water from the descending limb gets drawn out thru osmosis.
The more sodium coming out of the ascending limb, the more water comes from the descending limb. This allows it to continuously escalate.
Gets more Na+ & Cl- out of filtrate
This is a positive feedback mechanism that doesn’t stop bc filtrate constantly goes in & out
Countercurrent exchange & countercurrent multiplication
Countercurrent exchange- the 2 sides are trading substances (water for Na+ & Cl- )
Countercurrent multiplication- concentration is changing (increasing in descending limb, decreasing in ascending limb)
How much Na+ & H2O is left in the nephron by the time filtrate reaches the DCT? (after the loop of Henle)
10% each
Reabsorption at the DCT & CD
10% of Na+ & H2O is still in the filtrate, which can either get reabsorbed by the capillary or can do nothing
In the DCT, you can either:
save it (reabsorption)
Let it pass (leave it & urinate it out)
This is where we adjust the urine depending on our needs
The “fine tuners” are our hormones
Diuresis
making urine
Diuretics
Increases urine production
ADH (antidiuretic hormone)
List what it’s made by, target cells, command, & effects (2 main effects)
Made by: hypothalamus (released by posterior pituitary gland)
Target cells: DCT/CD
Command: Inc. H2O reabsorption
make more aquaporin-2 (temporary doorways) (aquaporin-1 is permanent)
Effects:
Dec. urine volume
Inc. urine concentration (keep water in blood, which will inc. blood vol.)
“SAVE THE H2O”
Aldosterone
List what it’s made by, target cells, command, & effects (1 effect)
Made by: Adrenal cortex
Target cells: DCT/CD
Command: Inc. Na+ reabsorption
more Na+ pumping
Effects:
Dec. urine concentration
H2O follows when ADH is present
by itself, aldosterone doesn’t change the volume, just the concentration
“SAVE THE Na+”
ANH/ANP (Atrial Natriuretic Hormone)
List what it’s made by, target cells, commands (2 commands), & effects (3 effects)
Made by: Right atrium when overstretched (meaning too much blood in the atrium)
think of it like a squid releasing ink in a panic. The right atrium doesn’t want to break, so it releases ANH in response to overstretching
Target cells: Posterior Pituitary Gland (where ADH is released) & DCT/CD
Command: Dec. ADH release & Dec. Na+ reabsorption
It’s saying “LOSE THEM BOTH!!” (doesn’t want water & sodium to get reabsorbed back into blood)
Effects:
Na+ & H2O stay in urine
Large volume of normal to dilute urine
Overkill to get rid of sodium, but it’s done just to be safe
Dec. blood volume
helps prevent the atrium from overstretching
“DUMP ‘EM BOTH”
Chronic diabetes insipidus
Hyposecretion of ADH. Water can’t be saved & stays in urine
Results in high urine volume (peeing all the time).
Water doesn’t get shifted back to blood at the DCT/CD
Alcohol’s effect on urine volume
Alcohol reduces the ability to produce ADH by inhibiting the hypothalamus, thus increasing urine volume
BNH or B-Type ANH
This is a version of ANH that’s made by the ventricles
This is normally less than 20% of total ANH
If/when it becomes more than 20%, this is a sign of heart failure
Renin-angiotensin-aldosterone-ADH-system
list where this fluid regulatory mechanism occurs (including what it’s composed of), what causes the release of renin, the enzymes involved, & the 5 effects
Juxtaglomerular apparatus: combo of 2 cells in the nephron:
Juxtaglomerular cells
Smooth musc. cells that surround afferent arteriole
Filled with the enzyme renin
These monitor blood pressure in afferent arteriole
Macula densa cells
Cells in the wall of DCT
monitor filtrate concentration
Release of renin: caused by Low BP (in afferent arteriole) or low filtrate concentration (in DCT)
angiotensinogen (inactive form in blood made by liver —renin→ angiotensin I (occurs in blood)
angiotensin I —ACE (angiotensin converting enzyme)→ angiotensin II (occurs in lungs)
Angiotensin II is a powerful vasoconstrictor
Effects:
Inc. ADH release
Inc. Aldosterone release (save them both!)
Dec. Urine volume
Inc. Blood volume
Vessels constricted (inc. BP)
Secretions
This is what we add to filtrate before we urinate
Substances are secreted by countertransport with sodium (pumped in different directions)
Secretions at PCT & DCT/CD
PCT
H+
Nitrogenous wastes
Some drugs
DCT/CD
H+
Nitrogenous wastes found in urine & how they’re made (4)
urea- from deamination (remove aminos) of prots. by liver (protein metabolism)
NH4+ (ammonium) - from the same as above
uric acid- from decomposition of nucleic acids (DNA/RNA)
creatinine- from CP (creatine phosphate) breakdown
can be dangerous when there’s too much due to muscle injuries (large rips of muscle tissue). Can result in kidney failure
abnormal urine contents & possible reasons for abnormalities (just 1 abnormality to list that can be found in urine) (2 reasons for abnormality)
Glucose- the glucose should be fully absorbed in the PCT, along with proteins & amino acids.
Either caused by…
too much glucose in blood that it can’t be reabsorbed fast enough
broken PCT
Urinary bladder
list the location, how much it can hold, what epithelium lines the urinary bladder, the 4 structures, & the openings
Located behind pubic symphysis
Volume can expand up to 1L thanks to rugae
Lined with transitional epithelium
Has 3 openings
2 ureteral openings & 1 urethral opening to form the trigone
Urethra- urine tube at the bottom of urinary bladder
Detrusor muscle- specialized smooth musc. that lines the bladder
2 layers of longitudinal smooth musc fibers with 1 layer of circular in between
Internal urethral sphincter- smooth musc.
External urethral sphincter- skeletal musc. (we can control this)
Male vs. Female (in regards to the urethra & sphincters). Who is more prone to UTIs & why?
Sphincters are easy to identify in males due to the prostate gland. Female have both sphincters, but it’s more difficult to identify
Urethra in male is longer (20cm) while it’s shorter in females (3-5cm)
Causes women to be more prone to UTI (urinary tract infection)
This is bc there’s less of an opportunity to catch bacteria throughout the urethra
Micturition
list the definition, what triggers it, & what will contract & relax in response to the trigger.
Micturition- voiding your bladder (peeing)
Triggered when 200-300ml of urine shows up in bladder
Pushes against walls (distention)
We have a short loop (causes reflex) & long loop (up to brain) (similar to defecation)
Detrusor musc. contracts while internal & external urethral sphincters relax
Detrusor contracts to let urine out
Sphincters relax to open
We learn to contract the external urethral sphincter to control urination
Events like childbirth, injuries or aging can cause us to lose the ability to control urination
hemodialysis
temporarily removes a person’s blood & passes it thru a filter that removes metabolic wastes & extra fluid. This normalizes electrolyte & acid-base balance
Must be performed 3 times per week at a dialysis clinic
peritoneal dialysis
dialysis fluid is placed into the peritoneal cavity, allowed to circulate for several hours, then drained
Can be performed nightly at home, so this is the preferred treatment for long-term dialysis
renal calculi (kidney stones)
Crystalline structures composed most commonly of calcium oxalate salts. Formed due to high concentrations of ions in filtrate
These can adhere to the tubules
causes severe pain, blood in urine, sweating, nausea, & vomiting
glomerulonephritis
damage to & destruction of glomeruli, causing inflammation of glomerular capillaries & filtration membrane. Can lead to renal failure
incontinence
loss of voluntary control over the bladder. Can be caused by childbirth, injuries, or age
What percentage of a person is water for a female & a male? What causes these different percentages?
Women: 50% water
Caused by more estrogen, meaning more subcutaneous adipose (our least hydrated tissue)
Men: 60% water
Caused by more testosterone, meaning more skeletal musc (our most hydrated tissue)
Where is water located in the human body? (includes the definition for fluid compartment)
Fluid compartment- where the fluid is. Extracellular fluid is the largest fluid compartment.
Either one of the two fluid compartments…
Extracellular fluid- outside cells. 40%
There are multiple kinds (ex. lymph, interstitial fluid, blood plasma, etc). These just get lumped together. Constantly moved around & similar.
Intracellular fluid- inside cells. 60%
How we get water in & water out (~3 methods each)
Gain water
Drinking
Eating
Making it (ex. from electron transport system)
Lose water
Urinating (peeing)
Defecating (pooping)
Evaporation (ex. thru skin by sweating or thru lungs by exhaling water vapor)
We want these to be equal for homeostasis. If not, we need to use fluid regulatory mechanisms
Blood plasma vs. interstitial fluid vs. intracellular fluid
Blood plasma & interstitial fluid are both extracellular fluids (outside the cell)
However, plasma has a higher protein count
Extracellular fluid has more Na+
Intracellular fluid is found inside the cell.
Has more K+ than extracellular fluid
Different from extracellular fluid due to the cell membrane.
Ion
a particle with a charge
cation vs. anion
Cation- an ion with a positive charge
Anion- an ion with a negative charge
Extracellular fluid (ECF) & Intracellular fluid (ICF)
what do they have in them (3 each) & what causes them to be different?
We expect the extracellular & intracellular fluid to be different due to the cell membrane!! That’s the cell membrane’s purpose (otherwise, we wouldn’t need one)
Ex. We have the sodium potassium pump to pump 3 sodium into ECF & 2 potassium into ICF
ECF has more sodium, chlorine, & bicarbonates
ICF has more potassium, proteins, & phosphates
electrolyte vs. nonelectrolyte
electrolyte- A substance that will dissociate (come apart) when dissolved to form charged particles (ions)
Water containing ions will carry an electrical current
Mostly inorganic molecules (don’t contain carbon) (often called salts)
Acids & bases are electrolytes
nonelectrolyte- A substance that will not come apart when dissolved, thus not breaking into ions
Tend to be organic molecules (ex. glucose)
Won’t carry a current
What are the most important ions related to acids & bases? Determine if something becomes more acidic or basic when more of each of these ions are present.
The important ions are H+ & OH-
The more H+ = more acidic
The more OH- (or fewer H+) = more basic
pH scale
Measures the strength of an acid or base based on how much H+ there is
The scale is opposite. Lower pH = more H+, & vice versa
The further you are from pH 7 (neutral), the stronger & more dangerous the acid/base is
Ex. pH of 2 is very acidic & dangerous while a pH of 13 is very basic & dangerous
Based in powers of 10
Acids vs. Bases(alkaline)
What do they do with H+? What would the pH of each be? What substances tend to fall under each category?
Acid- electrolytes that dissolve & give off H+. “H+ donors”
Almost always start with a hydrogen
pH is less than 7
Base (alkaline)- electrolytes that bind up H+. “H+ acceptors”
Often hydroxides
Takes the H+ out of the solution, combine with OH- to form water
pH is greater than 7
Why is it important to not have large shifts in pH in our bodies?
If we have large shifts in pH in our bodies, then enzymes won’t work & metabolism ends, which can lead to death
Human acidity vs. Human alkalinity (basicness).
List the definitions & sources for each (sources for H+ & OH-)
Human acidity- pH goes down (becomes more acidic). Comes from metabolism
carbonic acid, lactic acid, sulfuric acid, phosphoric acid, fatty acids & ketones are made from metabolism
Human alkalinity- pH goes up (becomes more basic).
Comes from eating K+, Mg++, Ca++, & Na+
What’s the normal pH range of human blood?
7.35-7.45
Buffers (list the 2 types)
Chemicals or actions that resist changes in pH
Chemical buffers are limited since they can essentially get overwhelmed holding onto H+. These will eventually run out
If it’s an action, it’s a physiological buffer, which is better since we can’t run out of these
Physiological buffer (list the 2 locations & functions for the human body’s buffer systems)
An action buffer, which can’t run out.
We have 2 types of physiological buffers:
Urinary system- can pee out H+ so they don’t build up in blood
Urine has a large pH range (pH of 4-8) to help make sure the blood pH doesn’t change
Respiratory system- can remove H+ by breathing out CO2. Holding in your breath can make blood more acidic
Remember, respiratory rate affects blood CO2 levels
acidosis vs. alkalosis
acidosis= too acidic (pH too low)
blood pH is less than 7.35
alkalosis= too basic (pH too high)
blood pH is greater than 7.45
Respiratory acidosis/alkalosis vs. Metabolic acidosis/alkalosis
Respiratory- caused by respiratory system
The only cause of respiratory acidosis is hypoventilation.
pH too low, low resp. rate & high blood CO2
Respiratory alkalosis is caused by hyperventilation
pH too high, high resp. rate & low blood CO2
Can determine if it’s respiratory based on the respiratory rate.
Metabolic- caused by anything that’s not the respiratory system
can have a variety of different causes, it’s just not caused by the res. sys
How fluid volume is controlled by each of the following:
renin, aldosterone, ADH, ANH, & hypothalamus (hint! only one of these will decrease fluid volume)
renin- inc. fluid volume since it wants to save sodium & water to inc. BP
aldosterone- inc. fluid volume since it wants to save sodium, & water wants to follow sodium when it can & when it’s allowed.
ADH- inc. fluid volume since it wants to keep H2O in blood
ANH- dec. fluid volume since it’s triggered by a high blood volume
hypothalamus- inc. fluid volume by releasing ADH
hypernatremia vs. hyponatremia (include what it’s commonly caused by for each)
hypernatremia- abnormal increase in plasma sodium ion concentration. Commonly caused by dehydration
hyponatremia- abnormal decrease in the plasma sodium ion concentration. Commonly caused by overhydration
hyperkalemia vs. hypokalemia
hyperkalemia- abnormally high potassium ion concentration, above 4.5 mEq/l
hypokalemia- abnormally low potassium ion concentration, below 3.9 mEq/l
hypercalcemia vs. hypocalcemia
hypercalcemia- abnormally high calcium ion concentration, above 10.5 mg/dl
hypocalcemia- abnormally low calcium ion concentration, below 8.7 mg/dl
edema
swelling caused by excess water/fluid in interstitial fluid
Source & action of parathyroid hormone & calcitonin
Parathyroid hormone (PTH)- source is the parathyroid gland
Increases blood calcium level by triggering calcium ion reabsorption in kidneys & osteoclast activity
Calcitonin- source is the thyroid gland
Decreases blood calcium level by stimulating osteoblasts