Unit 5 - Lumbopelvic Spine IV including SI Joint
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
52 Terms
Sacroiliac Joints (SIJ)
Junction between caudal end of axial skeleton and lower appendicular skeleton
Designed for stability
Sacrum “wedged” between ilia
Effective transfer of large forces between vertebral column, lower extremities, and ground
Pelvic Ring
Components
Sacrum
SIJs
Hemipelvis (ilium, pubis, ischium)
Pubic Symphysis Joint
Pelvic Ring
Transfers body weight force bidirectionally between pelvic ring, trunk, and femurs
SI Joint Structure
Just anterior to palpable posterior-superior iliac spine (PSIS)
Matching auricular (little ear) surfaces of sacrum and ilium
Semicircle “boomerang” shape
Concavity facing posterior
SI Joint Structure Changes
during puberty from
Diarthrodial (synovial)
Freely movable
to modified Synarthrodial
Immovable (pg. 29)
Smooth to Rough surfaces
Enhances friction, resistance to vertical shear force
85% in 60s show degenerative changes, asymptomatic
80s, 10% of population completely ossified/fused
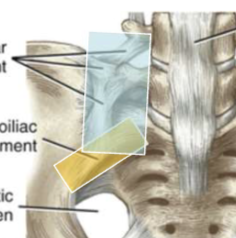
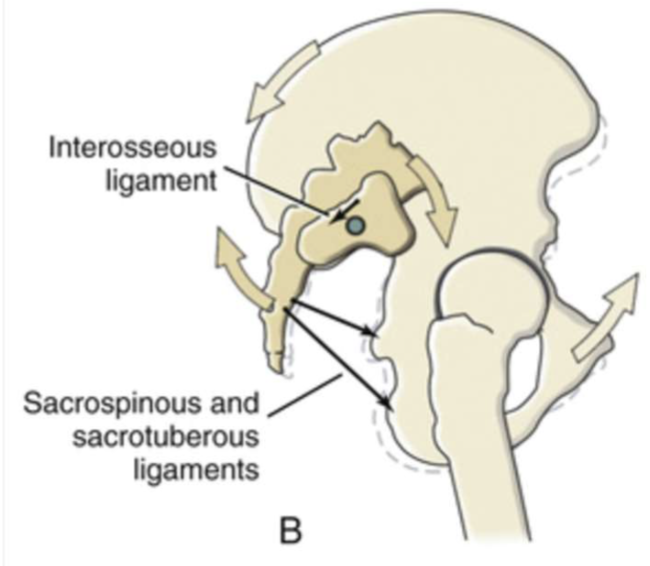
Ligaments
Anterior aspect
Anterior Sacroiliac
Thickening of anterior / inferior regions of capsule
Iliolumbar
Blends with Ant. Sacroilia
Ligaments
Within
Interosseous
Strongest of SIJ
Dense, short fibers fill gap of posterior / superior margins
Similar to syndesmosis of distal tibiofibular joint

Ligaments
Posterior aspect
Posterior Sacroiliac
Short and long
From posterolateral aspect of sacrum to iliac tuberosity and PSIS of ilium
Sacrotuberous
Large
O: PSIS, lateral aspect of sacrum, coccyx
I: Ischial tuberosity
Blends with biceps femoris (lat. Hamstring) tendon
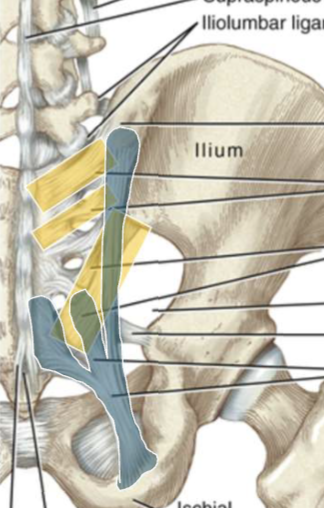
Sacrospinous
Deep to sacrotuberous
From caudal end of sacrum and coccyx to ischial spine
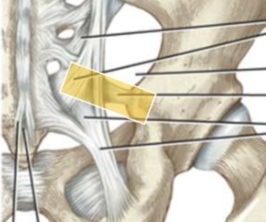
Sacrotuberous and Sacrospinous Ligaments do not directly cross the SIJ, but do provide articular stability
Innervations
Sensory nerve fibers within periarticular connective tissues of SIJ
Presence of Substance P and calcitonin-gene related polypeptides
Potential source of Nociception
Spinal Innervation
Most consistently from dorsal rami of L5-S3
Less often ventral rami of L4-S2
Thoracolumbar Fascia
Dynamic mechanical stability to lumbar spine and SIJs
Anterior and Middle Layers (surround QL)
Anchor medially to TP of lumbar spine, inferiorly to iliac crests
Posterior Layers (covers Erector Spinae, Multifidus, Latissimus Dorsi)
Anchor to all lumbar SP, sacrum, and ilium near PSIS
Lateral Raphe
Lateral fusion of posterior and middle layers
Blends with Transverse Abdominus and Obliquus Internus Abdominus
Kinematics
Rotation: 1-4 degrees
Translation: 1-2 mm
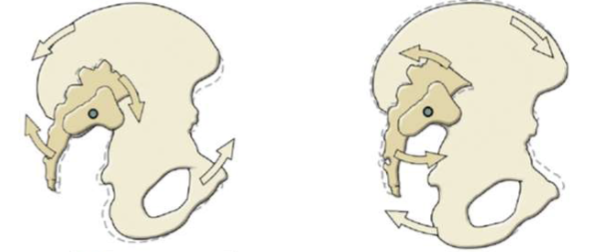
Nutation
“to nod forward”
Anterior sacral tilt relative to
Posterior iliac tilt
Counternutation
Posterior sacral tilt relative to
Anterior Iliac tilt
Defined as
Sacral-on-iliac rotation
Iliac-on-sacral rotation
Or simultaneous
Not to be confused with Anterior and Posterior Pelvic Tiltin
Kinematics
SIJ Function
Stress Relief within pelvic ring
Same for pubic symphysis
Load transfer between axial skeleton and lower extremities
Kinematics
Walking
Small, oppositely directed torsions at R and L iliac crests
Dissipates stress
Kinematics
Childbirth
Mobility / joint laxity increases during last trimester
Especially notable during 2nd pregnancy
Weight-gain + increased lordosis + hormone-induced ligamentous laxity
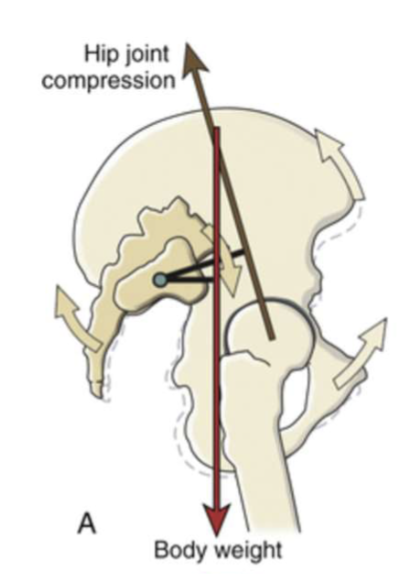
Nutation Torque
Increases stability at SIJ
Gravity
Passive tension from stretch ligaments
Muscle Activation
Increases compression and shear forces between surfaces
Full Nutation = “close-packed”
Counternutation = “loose-packed
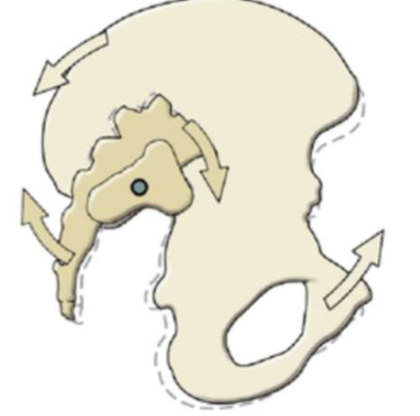
Nutation Torque: Gravity
From Body Weight passes downward
Anterior to SIJs
Posterior to femoral heads
Rotates sacrum anteriorly
Femur through Acetbula
Upward-directed counter force
Rotates ilium posteriorly
“Locks” SI
Nutation Torque: Ligaments
Tension
Interosseous Ligament
Sacrospinous Ligaments
Sacrotuberous Ligaments
Slackened
Long Posterior Sacroiliac Ligament (not pictured
Nutation Torque: Muscles
Based on attachments to
Thoracolumbar fascia
Sacrospinous & Sacrotuberous Ligaments
Stability generated by
Active compression forces against articular surfaces
Increasing nutation torque, “active locking mechanism”
Tensing connective tissues that directly or indirectly reinforce joint
Combination of above
Nutation Torque: Muscles
Directly
Rotate Sacrum anteriorly
Lumbar Multifidi
Erector Spinae
Rotate Ilium posteriorly
Rectus Abdominus
External Oblique
Biceps Femoris (hamstring)
Gluteus Maximu
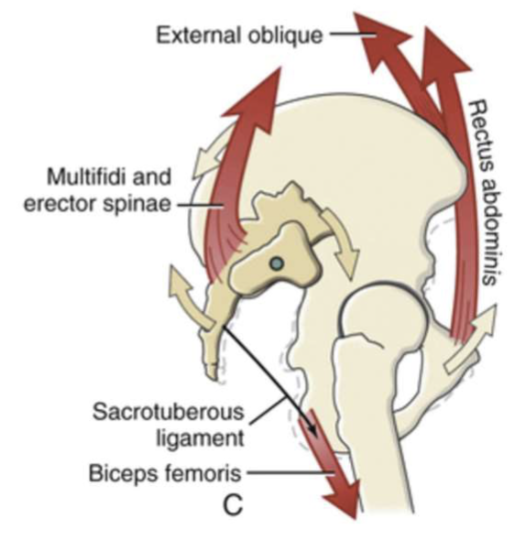
Nutation Torque: Muscles
Indirectly
Connected through Thoracolumbar Fascia
Latissimus Dorsi
Gluteus Maximus
Erector Spinae
Internal Oblique
Transverse Abdominus
Valsava Maneuver
Diaphragm
Pelvic Floor Muscles
Why Terminology Matters
Outdated terms create confusion
Consistency improves communication
Diagnostic accuracy requires precise language
Pain Classifications
Nociceptive pain
Referred pain (from adjacent structures)
Central sensitization
Pain Mechanism Revisited
Nociceptive
localized, predictable
Pain Mechanism Revisited
Referred
segmental, mimics SIJ
Pain Mechanism Revisited
Central
diffuse, unpredictable, non-mechanical
Hallmarks of SIJ Related Pain
PSIS tenderness
Pain with load transfer tasks
Negative centralization
Negative hip signs
Symptom duration >3 months
Contemporary vs. Outdated Terms
Stop saying: 'upslip', 'rotation', 'inflare'
Start saying: 'SIJ-related nociceptive pain'
Use functional and pain-based descriptors
Where SIJ Fits in Chronic LBP
SIJ accounts for ~15-30% of chronic LBP
Often coexists with myofascial or lumbar issues
Not always the primary pain source
Chronic Pain = Multidimensional
Biopsychosocial contributions
Fear, beliefs, deconditioning
Don’t ignore mood, sleep, or stress
Why Rule Out First?
Most LBP is lumbar or hip in origin
SIJ rarely acts alone
Rule-out prevents misdiagnosis and false positives
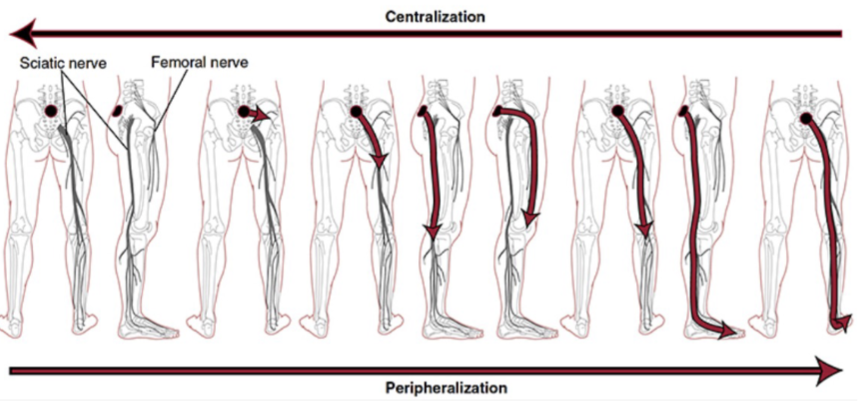
Clinical Priority: Rule Out the Lumbar Spine
Centralization with repeated motions (McKenzie)
Neurological screen: strength, sensation, reflexes
Facet loading patterns
Pain with extension, prolonged sitting, or flexio
Impairment-based Classifications Lumbar Spine
Movement Coordination Deficits
Mobility Deficits
Referred Pain
Radiating Pain (neuropathic)
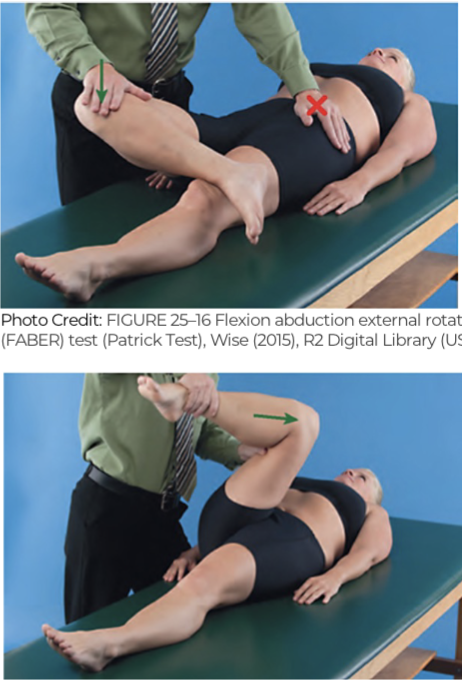
Now Rule Out the Hip
ROM testing (especially IR <15°)
FABER and FADIR provocation tests
Capsular pattern: IR > Flexion > Abduction
Pain with stairs, squatting, prolonged sitting
Hip Pathology Patterns
Hip OA: age >50, stiffness, IR loss
FAI: sharp anterior pain with flexion and rotation
Labral pathology: clicking, catching, instability
Rule-Out Summary
Step 1: Centralization or neuro signs = treat spine
Step 2: IR <15°, FABER/FADIR = treat hip
Step 3: No spine/hip findings? Consider SIJ
Laslett’s Cluster Overview
ASIS Distraction Test
ASIS Compression Test
Thigh Thrust
Sacral Thrust
Gaenslen’s Test
3 out of 5 = SIJ likely
ASIS Compression Test
applies medial force to the ASIS, which compresses the anterior SI joint and gaps the posterior surface

ASIS Distraction Test
lateral force is applied to the anterior-superior iliac spines, which distracts or opens the anterior aspect of the SI joint and simultaneously compresses the posterior aspect

Thigh Thrust
patient is laying supine
position the hip at 90 degrees and apply an axial load through the femur

Sacral Thrust
the patient is laying prone and you apply a vertical force from P to A over the sacrum

Gaenslen’s Test
should be performed on both sides
The setup creates opposing rotational forces across the pelvis
One leg is flexed, promoting posterior rotation of the ilium
The opposite leg is extended off the table, encouraging anterior rotation of the contralateral ilium
Since each side of the pelvis is stressed differently, testing both sides is essential to assess for SI joint related pain in either direction

Clinical Application Tips
Confirm symptom location and type
Apply pressure gradually
Use consistent technique
Be cautious with highly irritable patients
Why Not Just One Test?
Single test sensitivity/specificity is too low
Multiple tests increase diagnostic accuracy
Evidence supports 3/5 positive as threshold
Limitations of the Cluster (Laslett’s)
Not validated in acute LBP
Can’t rule in central sensitization
False positives if spine or hip not ruled out
CPG Informed Treatment Priorities
Stabilization training
Lumbopelvic motor control
Manual therapy for symptom modulation
Patient education and reassurance
Motor Control: Core Activation
Start with deep stabilizers: TA, multifidus
Train in neutral spine positions
Incorporate breath and pelvic floor control
Stabilization Progression: Early to Advanced
Phase 1: Isometric bracing, supine activation
Phase 2: Bridges, side planks, bird-dogs
Phase 3: Anti-rotation, single-leg stability
Phase 4: Load-bearing and dynamic movement
Manual Therapy: When and Why
Use to modulate pain, not 'realign joints'
Mobilization: SIJ, lumbar, thoracic, hip as needed
Soft tissue: glutes, piriformis, QL
Pain Science and Patient Beliefs
Pain ≠ damage
Reframe beliefs about alignment and instability
Build self-efficacy through graded exposure
When to Refer or Reassess
No progress after 6–8 weeks
Increasing disability or fear
Imaging or medical referral if red flags
The Treatment Mindset
SIJ is a regional contributor, not always primary
Treat movement, not just tissue
Progress gradually, educate constantly
Help patients reclaim confidence and control