_Micro E4 Content Practice Questions
1/179
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
180 Terms
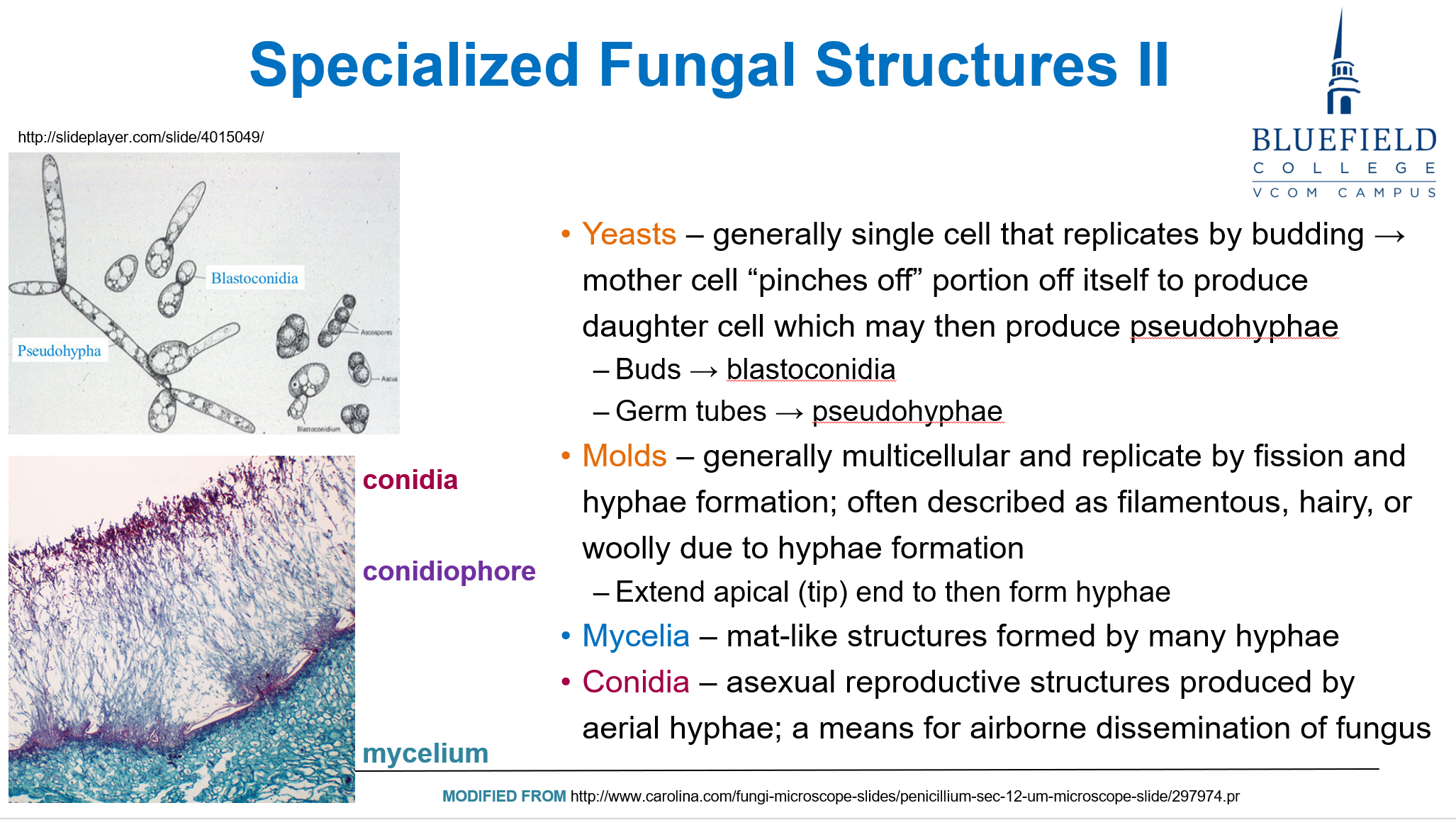
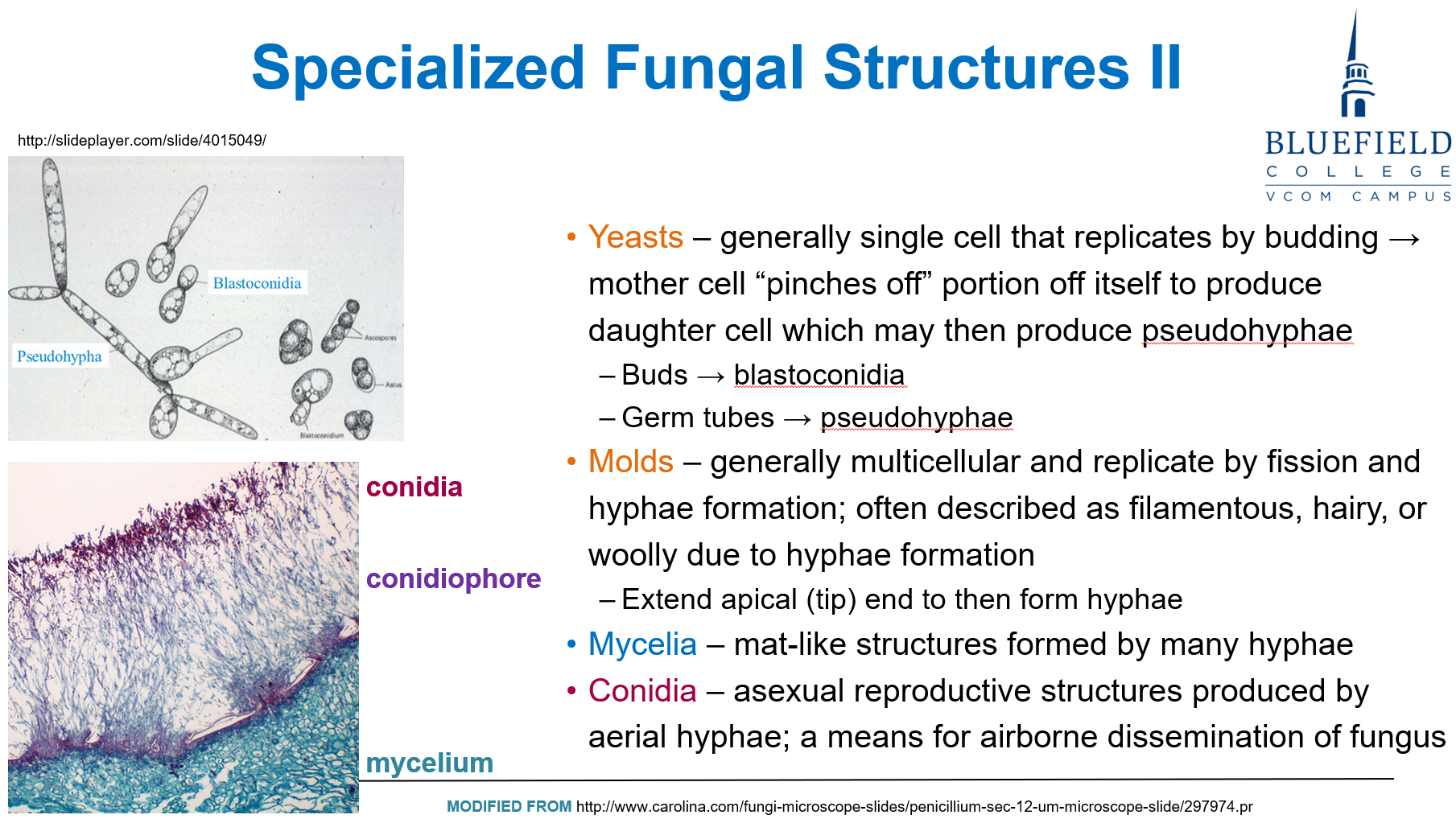
A 33-year-old immunocompromised man presents with a chronic cough and weight loss. Imaging reveals lung nodules, and biopsy shows a multicellular filamentous structure with septate hyphae and conidia. Which of the following best classifies this organism?
A. Unicellular budding yeast with pseudohyphae
B. Dimorphic fungus with a yeast form at room temperature
C. Filamentous mold with aerial and vegetative hyphae
D. Sporangiospore-producing anaerobe
E. Encapsulated yeast with polysaccharide wall
C. Filamentous mold with aerial and vegetative hyphae
Molds are multicellular fungi that reproduce via conidia and possess hyphae, which can be aerial or vegetative. This matches the biopsy findings.
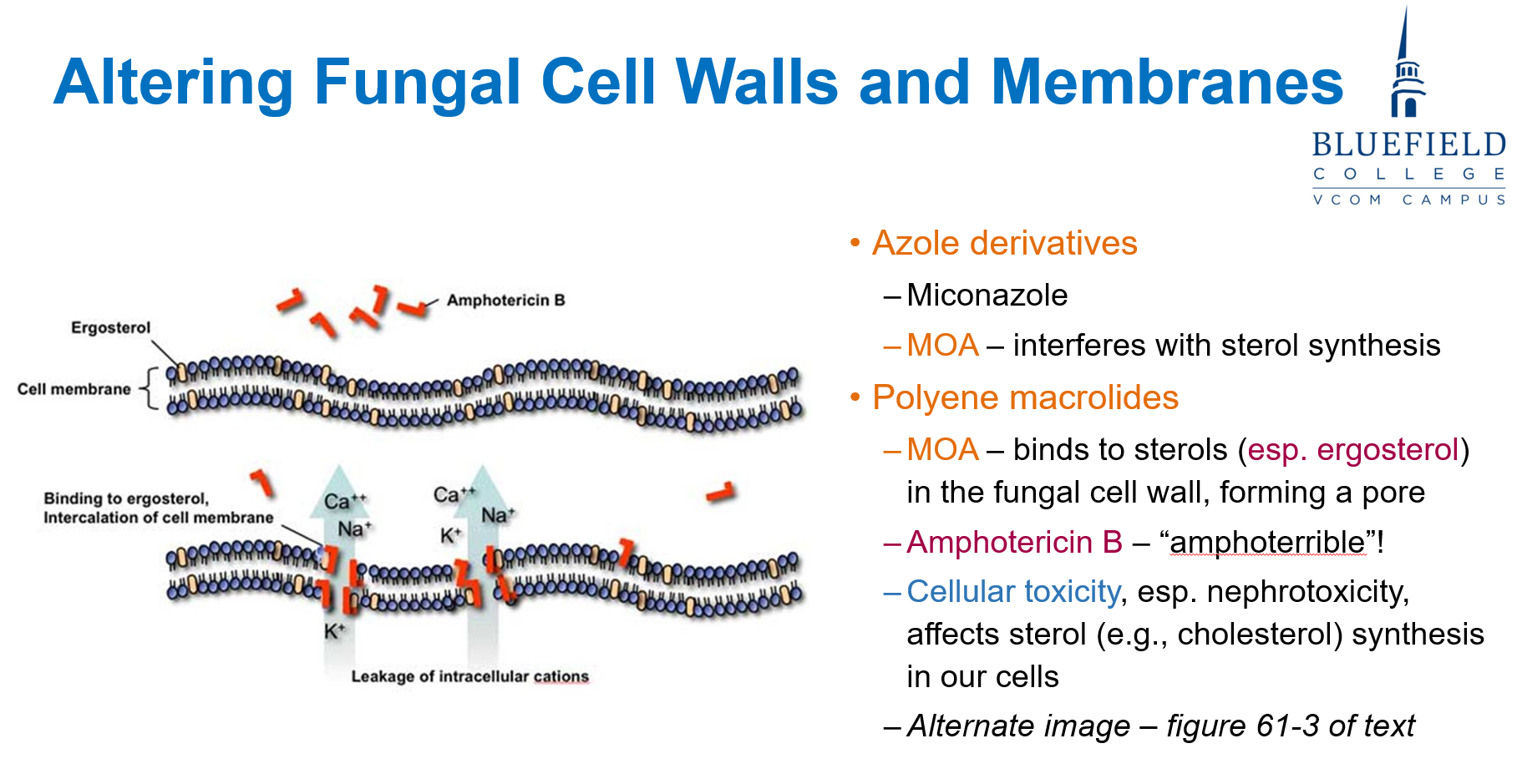
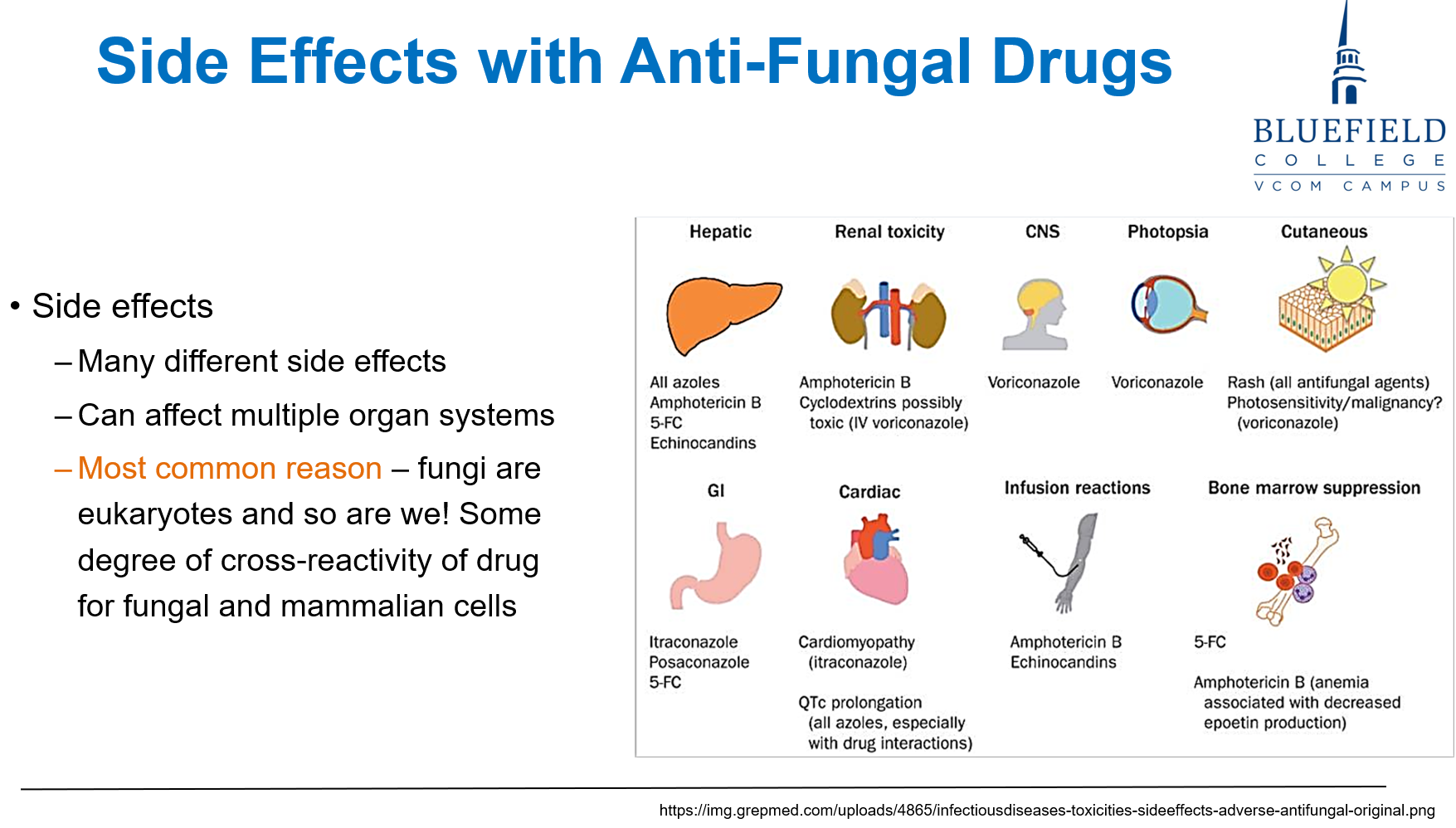
A 55-year-old man being treated for systemic candidiasis develops renal impairment after several doses of an antifungal drug. The agent most likely responsible targets which of the following?
A. β-glucan synthesis
B. DNA methylation
C. Ergosterol in fungal membranes
D. Peptidoglycan cross-linking
E. Ribosomal RNA synthesis
C. Ergosterol in fungal membranes
Polyene macrolides like amphotericin B bind to ergosterol, disrupting fungal membranes. However, due to similarities with human cholesterol, nephrotoxicity is a common side effect.
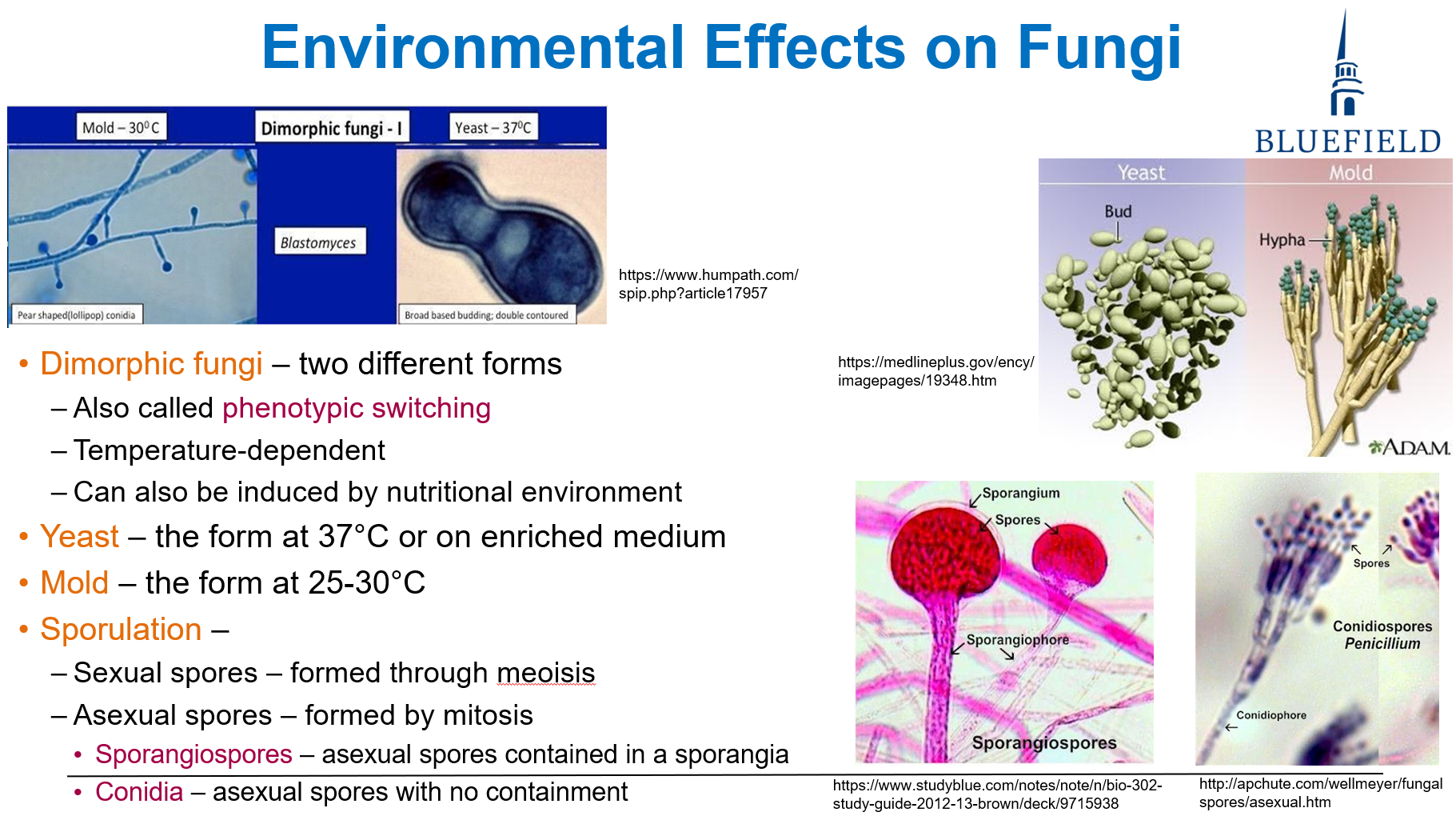
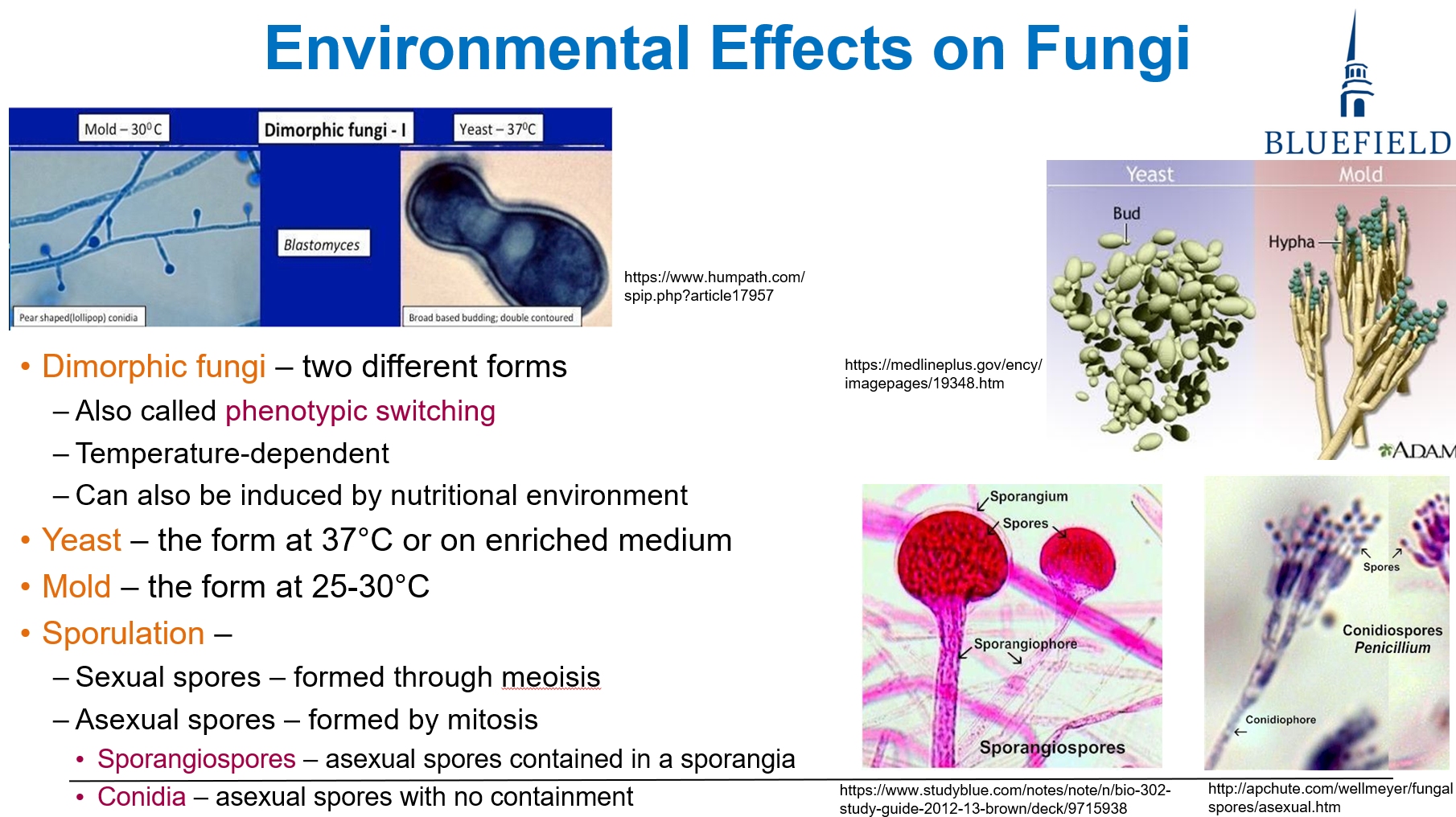
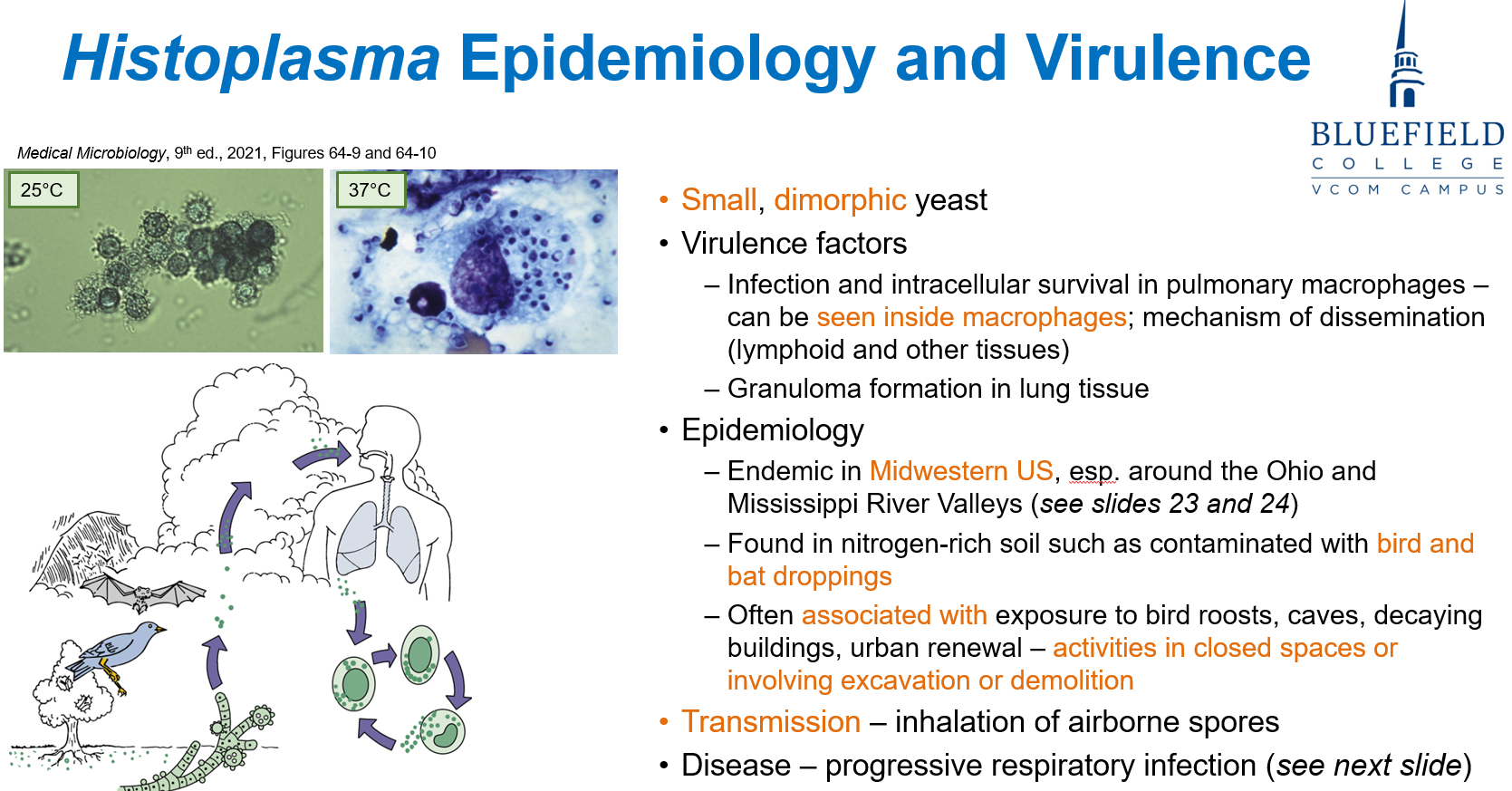
A 45-year-old man develops pneumonia after returning from a spelunking trip. Lung biopsy reveals yeast-like cells at 37°C but mold-like structures when cultured at room temperature. Which of the following best describes the organism?
A. Obligate mold that forms septate hyphae
B. Commensal yeast that replicates by budding only
C. Dimorphic fungus with temperature-dependent forms
D. Filamentous fungus forming coenocytic hyphae
E. Anaerobic mold that produces sporangiospores
C. Dimorphic fungus with temperature-dependent forms
Dimorphic fungi exist as yeast at 37°C and mold at 25–30°C, a key feature of pathogens like Histoplasma.
Which component of the fungal cell wall or membrane is the primary target of polyene antifungal agents such as amphotericin B?
A. β-glucan
B. Chitin
C. Mannoproteins
D. Ergosterol
E. Peptidoglycan
D. Ergosterol
Polyene macrolides, like amphotericin B, bind ergosterol, forming membrane pores. Ergosterol is unique to fungi, making it a critical selective drug target.
A mold seen under microscopy reveals non-septate, broad hyphae invading blood vessels. What reproductive structure is most likely associated with this organism?
A. Sporangiospore
B. Blastoconidium
C. Arthroconidium
D. Ascospore
E. Germ tube
A. Sporangiospore
Molds like Mucor have non-septate hyphae and reproduce asexually by sporangiospores, which are contained in a sporangium.
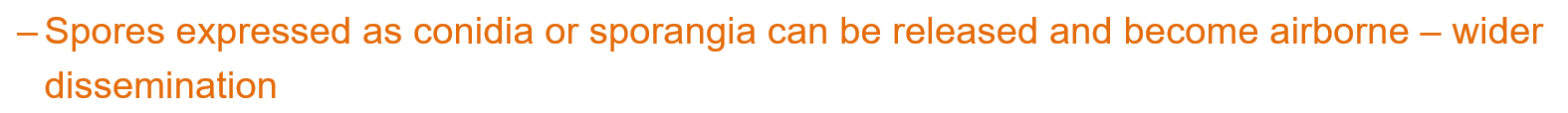
Which of the following best distinguishes asexual fungal reproduction from sexual reproduction?
A. Formation of zygospores
B. Use of meiotic division
C. Involvement of genetic exchange
D. Production of conidia via mitosis
E. Generation of ascospores in ascus
D. Production of conidia via mitosis
Asexual reproduction involves mitotic division, producing structures like conidia, whereas sexual forms involve meiosis and genetic recombination.
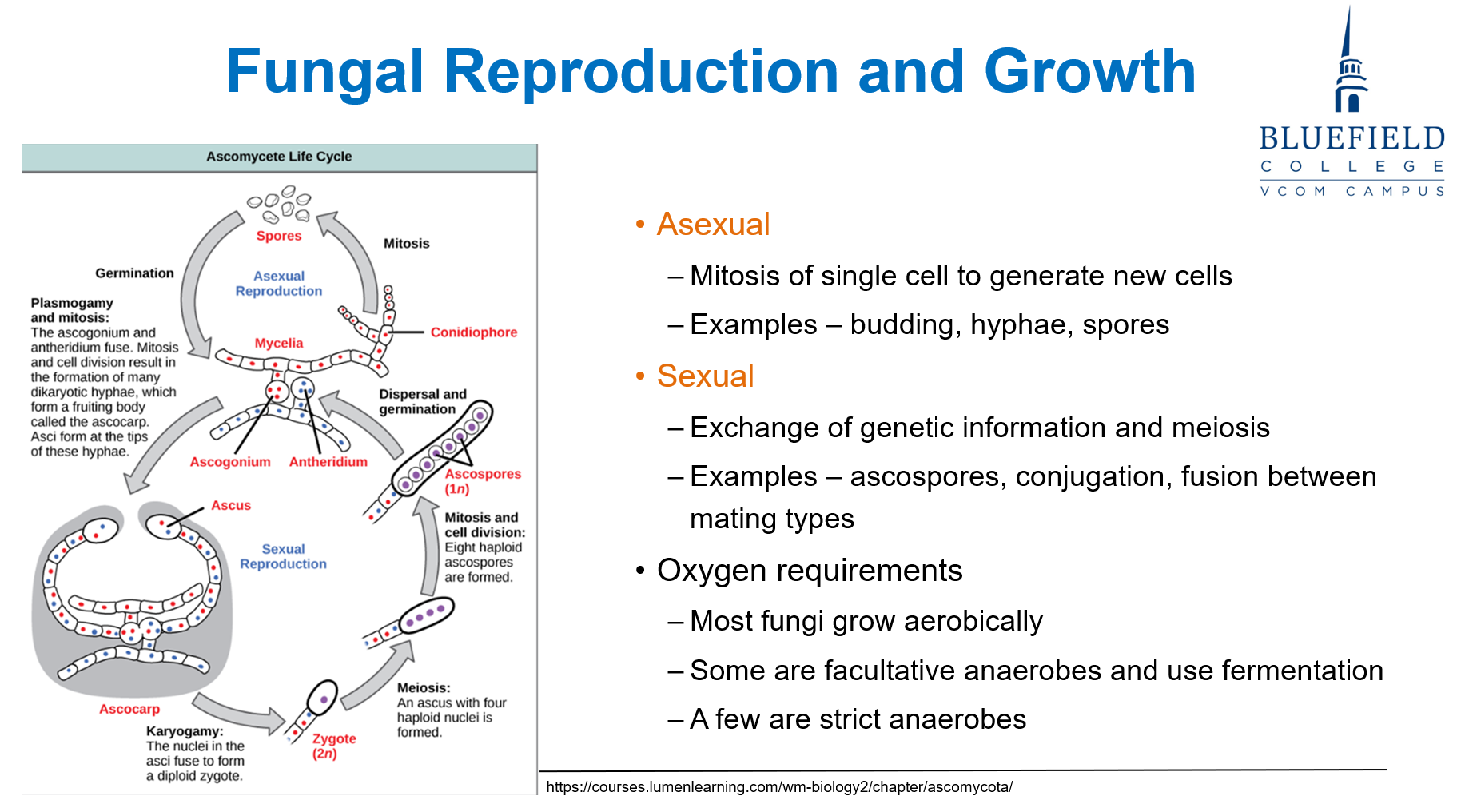
Which of the following represents the primary method of asexual reproduction in budding yeasts such as Candida albicans?
A. Sporulation through sporangium
B. Binary fission forming coenocytic hyphae
C. Apical hyphal growth and branching
D. Bud formation from mother cell
E. Production of septate vegetative hyphae
D. Bud formation from mother cell
Yeasts like Candida reproduce asexually by budding, forming blastoconidia from a mother cell.
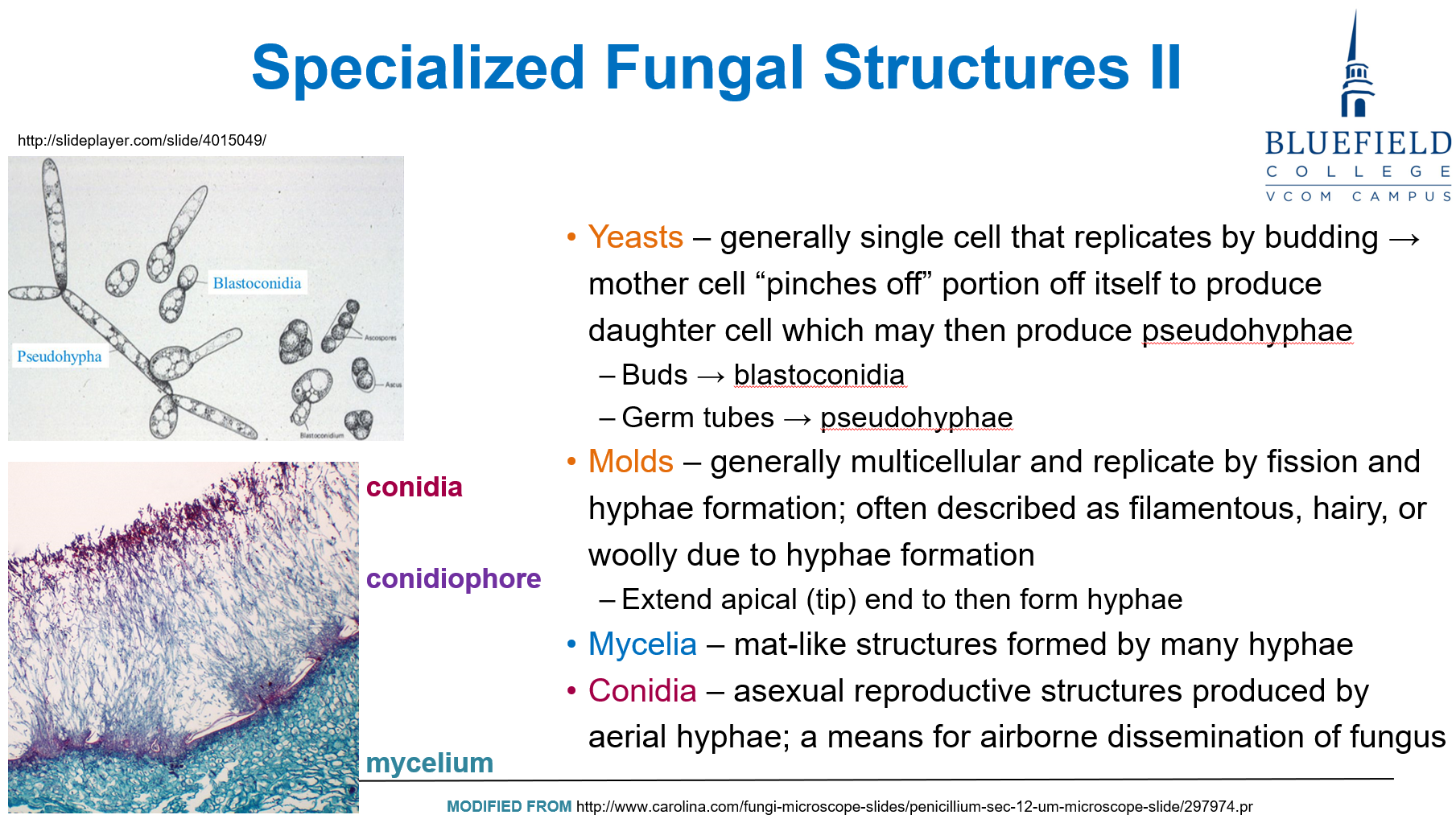
A patient inhales fungal spores while gardening and develops pulmonary symptoms. Which structure is most likely responsible for the airborne transmission?
A. Sporangium
B. Germ tube
C. Mycelium
D. Aerial conidia
E. Vegetative hyphae
D. Aerial conidia
Conidia are asexual spores produced on aerial hyphae and are the primary means of airborne fungal transmission.
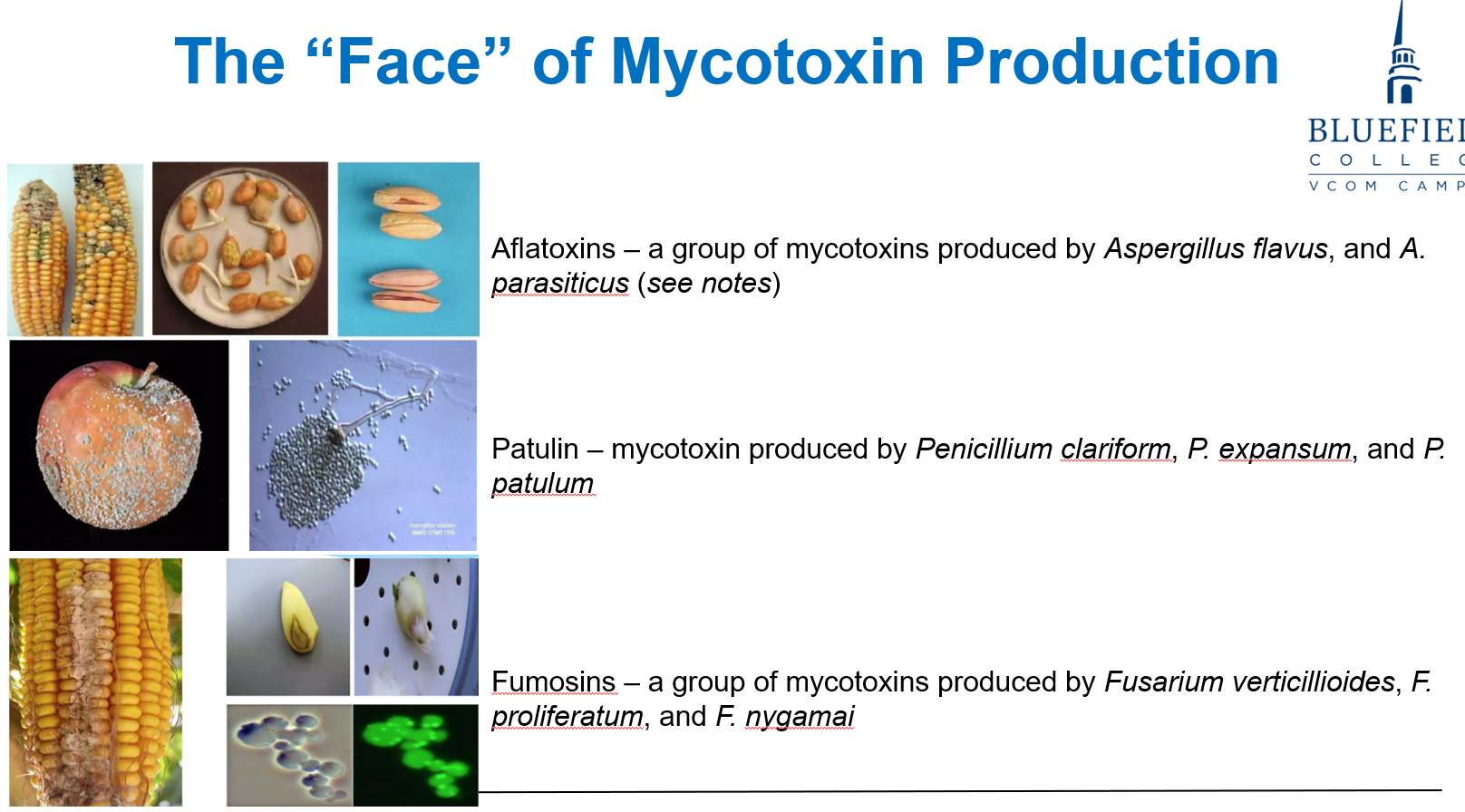
A family develops liver failure after eating contaminated corn. No fungal elements are detected in tissue. What best explains the clinical symptoms?
A. Invasive hyphal infection of hepatocytes
B. Systemic spread of fungal spores
C. Hepatotoxicity due to ingested mycotoxin
D. Immune complex deposition due to fungal antigens
E. Allergic reaction to fungal β-glucans
C. Hepatotoxicity due to ingested mycotoxin
Mycotoxins, such as aflatoxin, can cause toxicity without infection. Disease results from toxin ingestion, not organism invasion.
An elderly patient in a rehabilitation facility develops a superficial fungal infection on the skin folds. Culture reveals budding yeast. What is the most likely mode of transmission?
A. Inhalation of conidia from a distant reservoir
B. Injection through contaminated IV equipment
C. Contact with contaminated surfaces and local spread
D. Ingestion of spores in contaminated food
E. Penetration through intact skin via arthroconidia
C. Contact with contaminated surfaces and local spread
Budding yeasts like Candida are commonly transmitted by direct contact or surface contamination, leading to local dissemination in areas prone to moisture and skin breakdown.
A farmer presents with fever and cough. Chest imaging reveals lung infiltrates. Biopsy shows filamentous fungi with conidia. Which transmission route most likely caused this infection?
A. Ingestion of contaminated water
B. Inhalation of airborne spores
C. Sexual contact with an infected person
D. Traumatic inoculation during work
E. Contact with contaminated surfaces
B. Inhalation of airborne spores
Conidia and sporangiospores are airborne and can be inhaled, leading to pulmonary fungal infections—especially with mold exposure in agricultural settings.
Which of the following is not a typical route for fungal infection?
A. Inhalation of environmental spores
B. Ingestion of food contaminated with mycotoxins
C. Penetration through skin wounds
D. Inoculation through sexual intercourse
E. Dermal contact with contaminated surfaces
D. Inoculation through sexual intercourse
Sexual transmission is not a common route for fungal infection. Most infections occur via inhalation, ingestion, or dermal trauma/contact.
A 72-year-old nursing home resident with diabetes develops candidemia. Which of the following most likely contributed to the fungal infection?
A. Living in a warm climate
B. Recent international travel
C. Long-term hospitalization with catheterization
D. Consumption of contaminated fruits
E. High-fiber diet with fermented products
C. Long-term hospitalization with catheterization
Patients in long-term care settings, especially with invasive devices (e.g., catheters), are at higher risk for fungal infections due to compromised barriers and opportunistic pathogens.

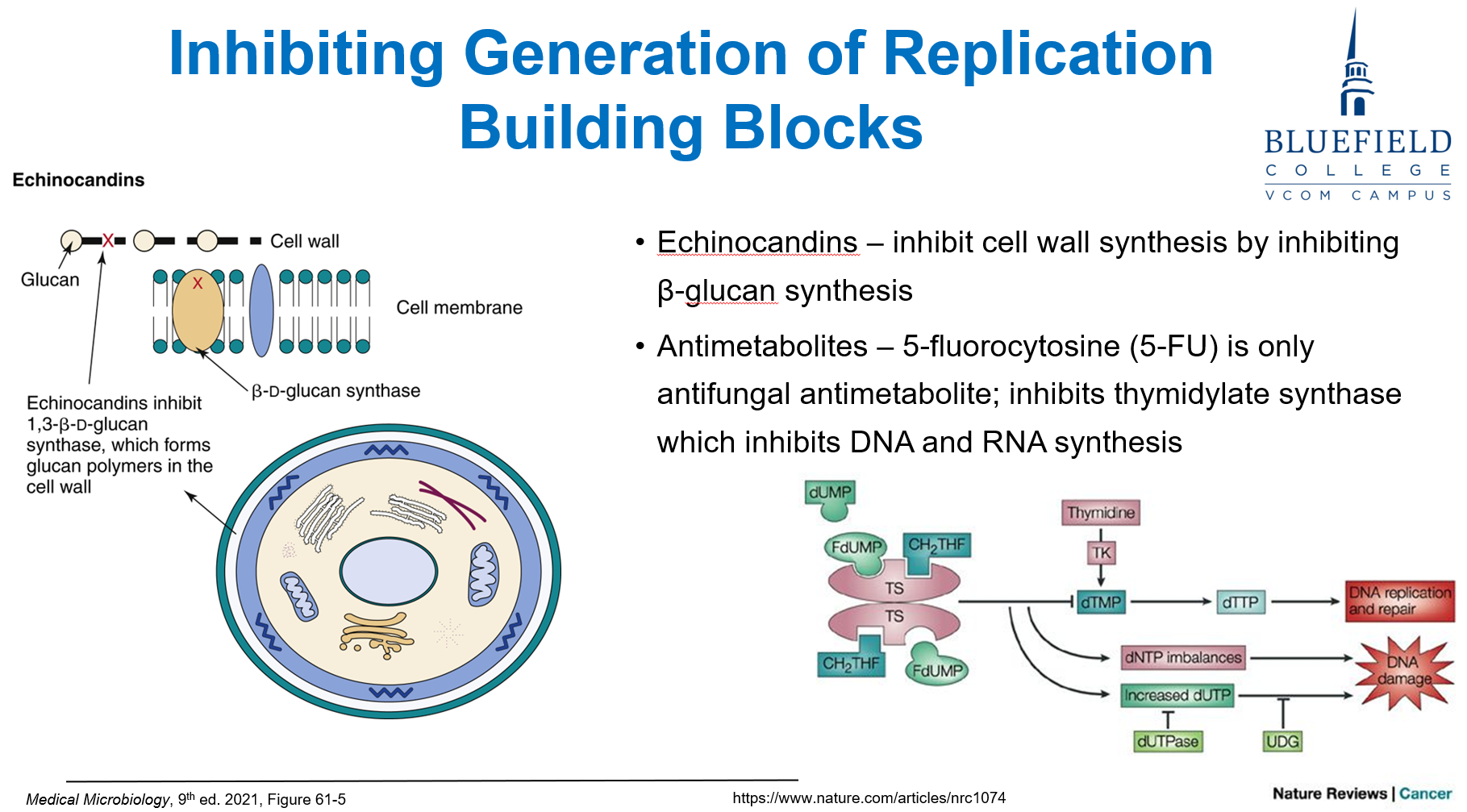
Which antifungal drug class inhibits β-glucan synthesis, weakening the fungal cell wall?
A. Azoles
B. Polyene macrolides
C. Echinocandins
D. Antimetabolites
E. Allylamines
C. Echinocandins
Echinocandins (e.g., caspofungin) inhibit β-glucan synthesis, which is critical for fungal cell wall integrity, a unique target not found in human cells.
A 63-year-old patient with systemic fungal infection develops renal failure after starting antifungal therapy. Which of the following best explains this adverse effect?
A. Inhibition of human peptidoglycan synthesis
B. High resistance rates from horizontal gene transfer
C. Toxicity due to shared eukaryotic cell structures
D. Rapid fungal mutation rates in host tissue
E. Activation of fungal endotoxin pathways
C. Toxicity due to shared eukaryotic cell structures
Fungi and humans are both eukaryotic, making it difficult to target fungi without some cross-toxicity to human cells. Nephrotoxicity is common with amphotericin B.
A 62-year-old man with acute myeloid leukemia develops fever and pulmonary infiltrates. Biopsy shows filamentous fungi invading tissue. Which host condition most predisposed him to this infection?
A. Age-related decline in immunity
B. Chronic sinusitis
C. Corticosteroid therapy
D. Exposure to contaminated water
E. Travel to a tropical environment
C. Corticosteroid therapy
Immunodeficiency, especially from chemotherapy or corticosteroids, is the major risk factor for invasive fungal disease. These drugs impair innate and adaptive immunity.
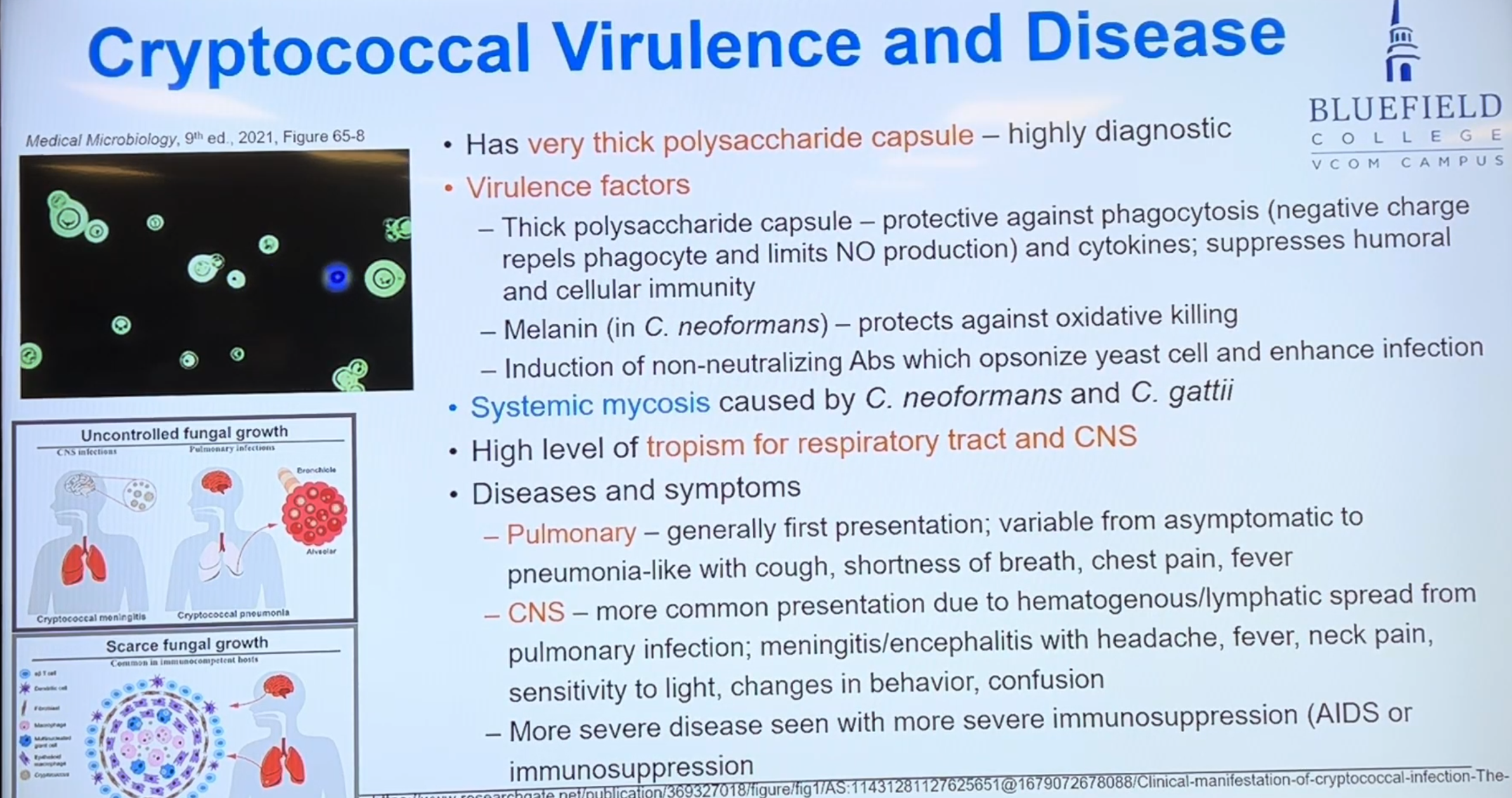
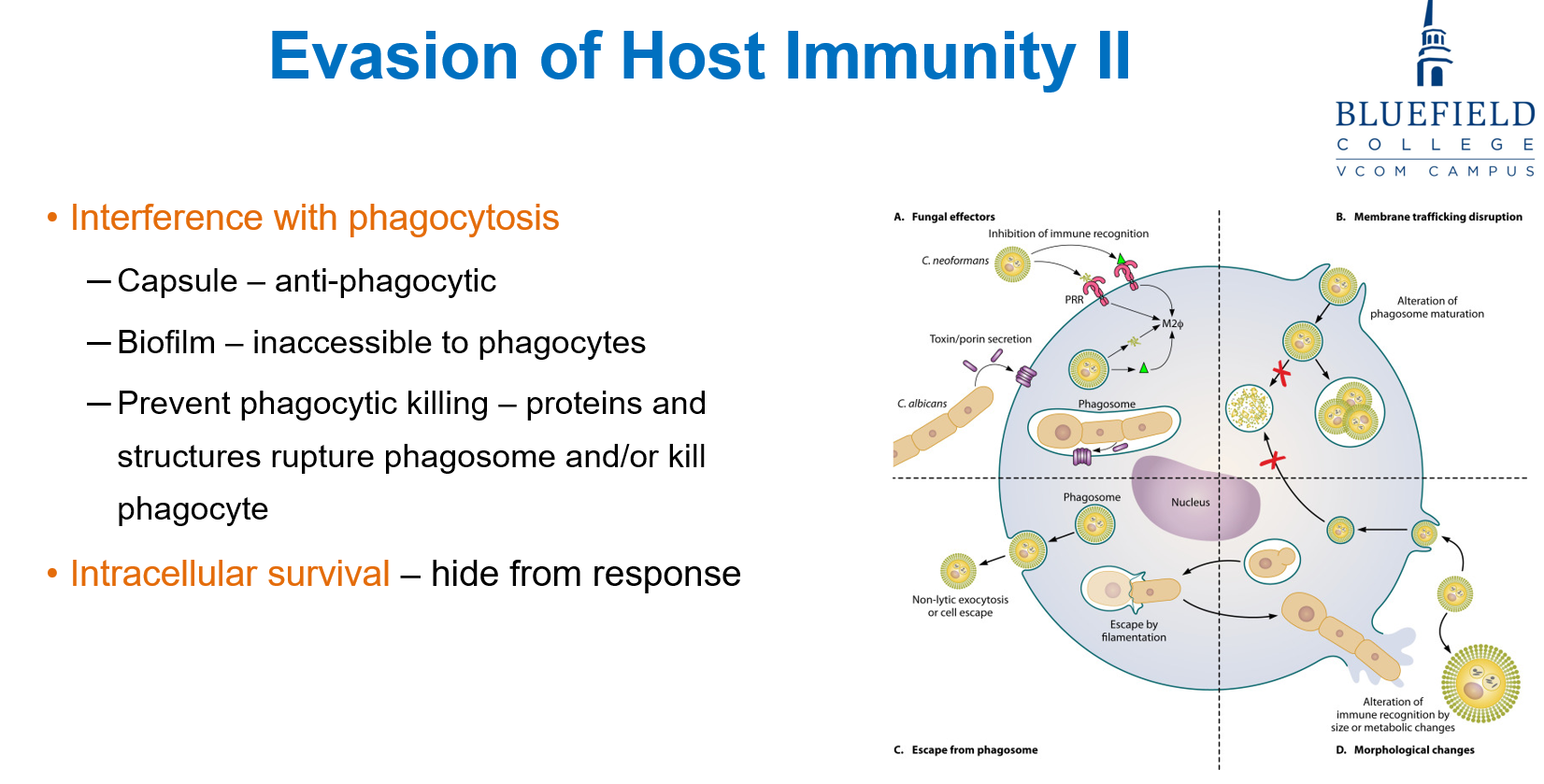
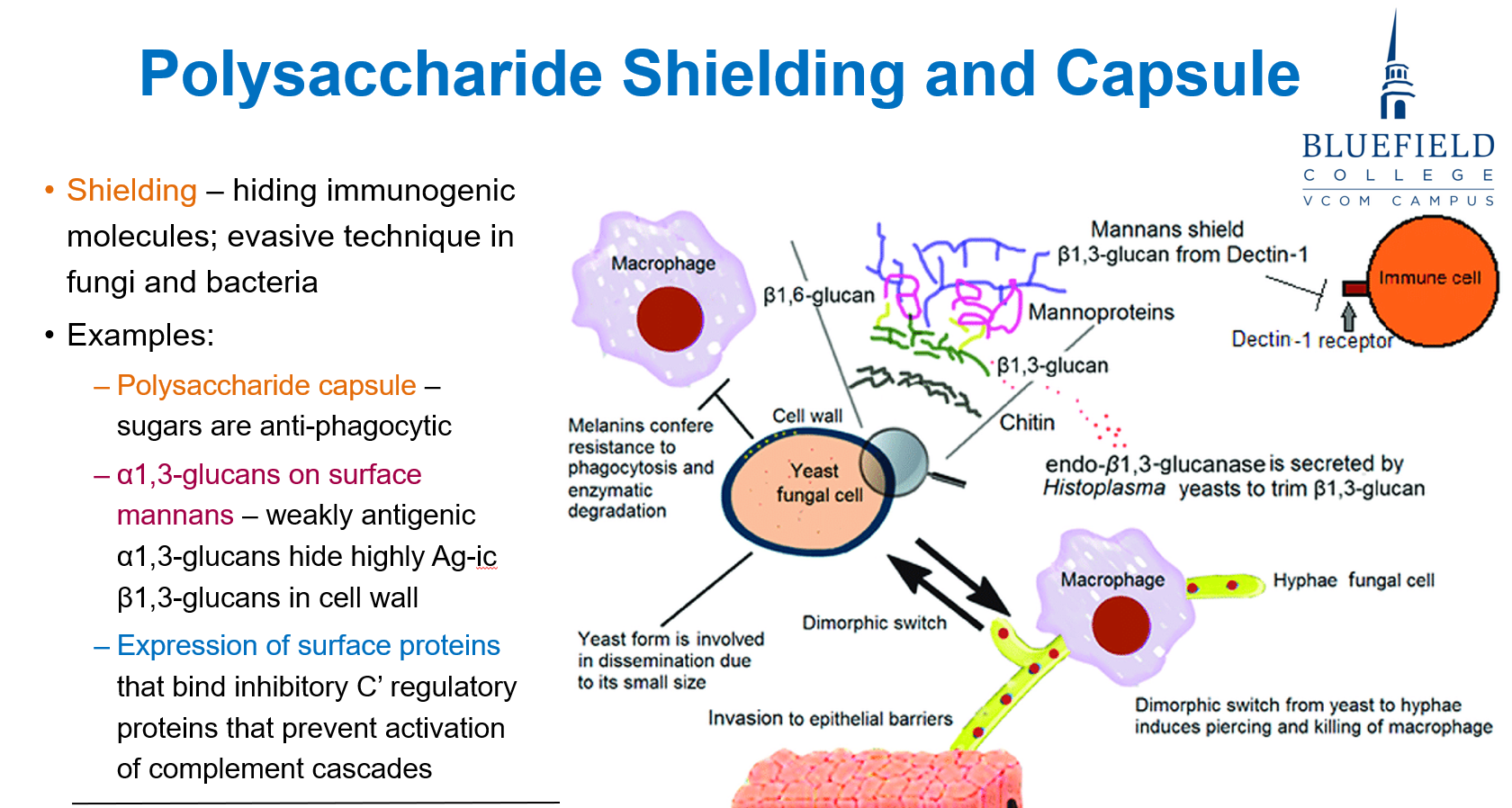
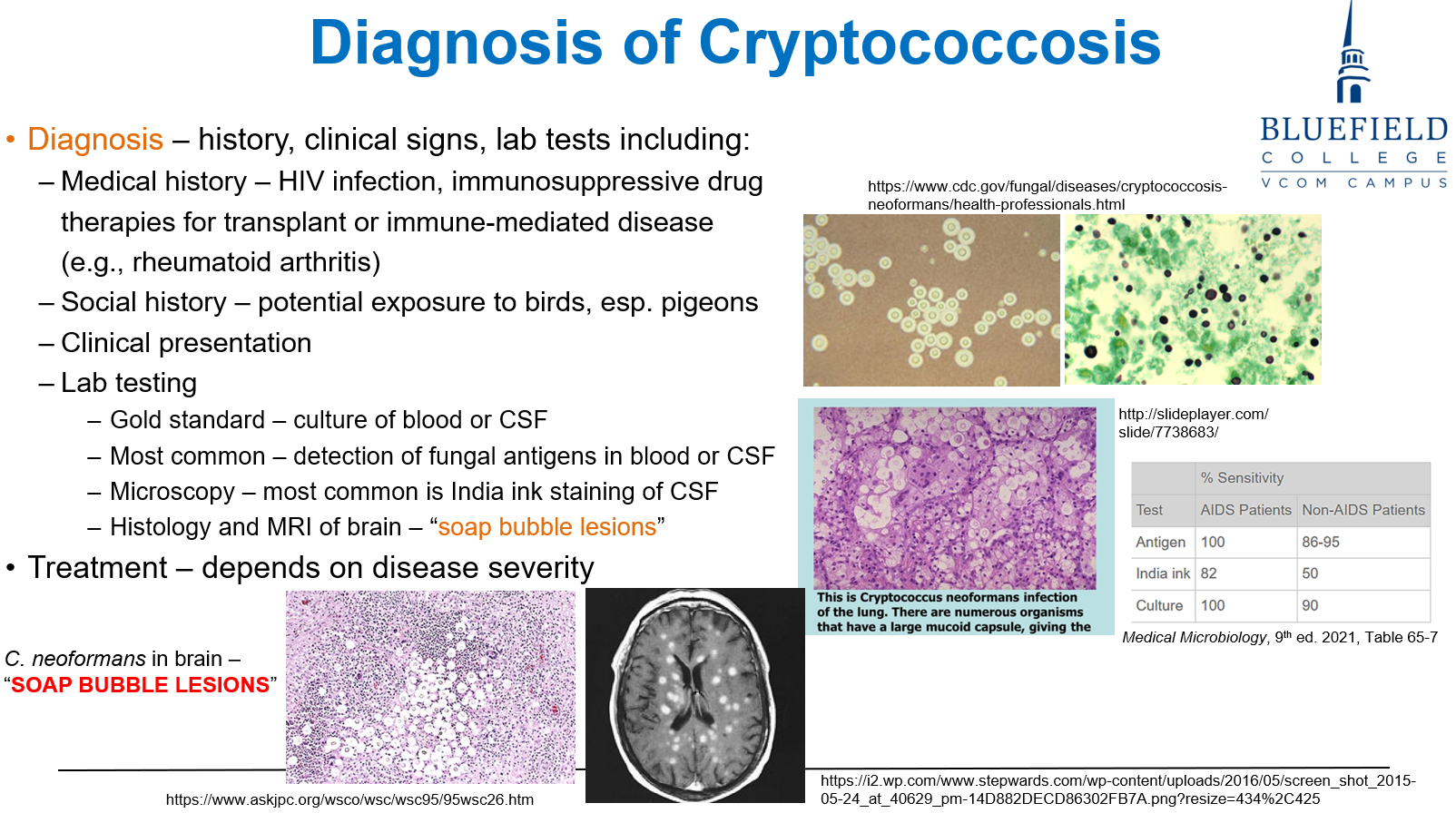
A patient with suspected fungal meningitis undergoes lumbar puncture. India ink stain reveals encapsulated yeast. Which virulence factor contributes most to immune evasion?
A. Aerial hyphae
B. Polysaccharide capsule
C. β-glucan-rich cell wall
D. Mycotoxin production
E. Sporangiospore formation
B. Polysaccharide capsule
The capsule (as seen in Cryptococcus neoformans) is anti-phagocytic and enables immune evasion, especially within the CNS.
A hospitalized patient develops a catheter-associated Candida albicans bloodstream infection. What structural adaptation allows Candida to persist on the catheter?
A. Germ tube elongation
B. Biofilm formation on surfaces
C. Sporangiospore production
D. Molecular mimicry
E. Production of hyaline hyphae
B. Biofilm formation on surfaces
Biofilms anchor fungi to surfaces like catheters and protect against host immunity and antifungal drugs.

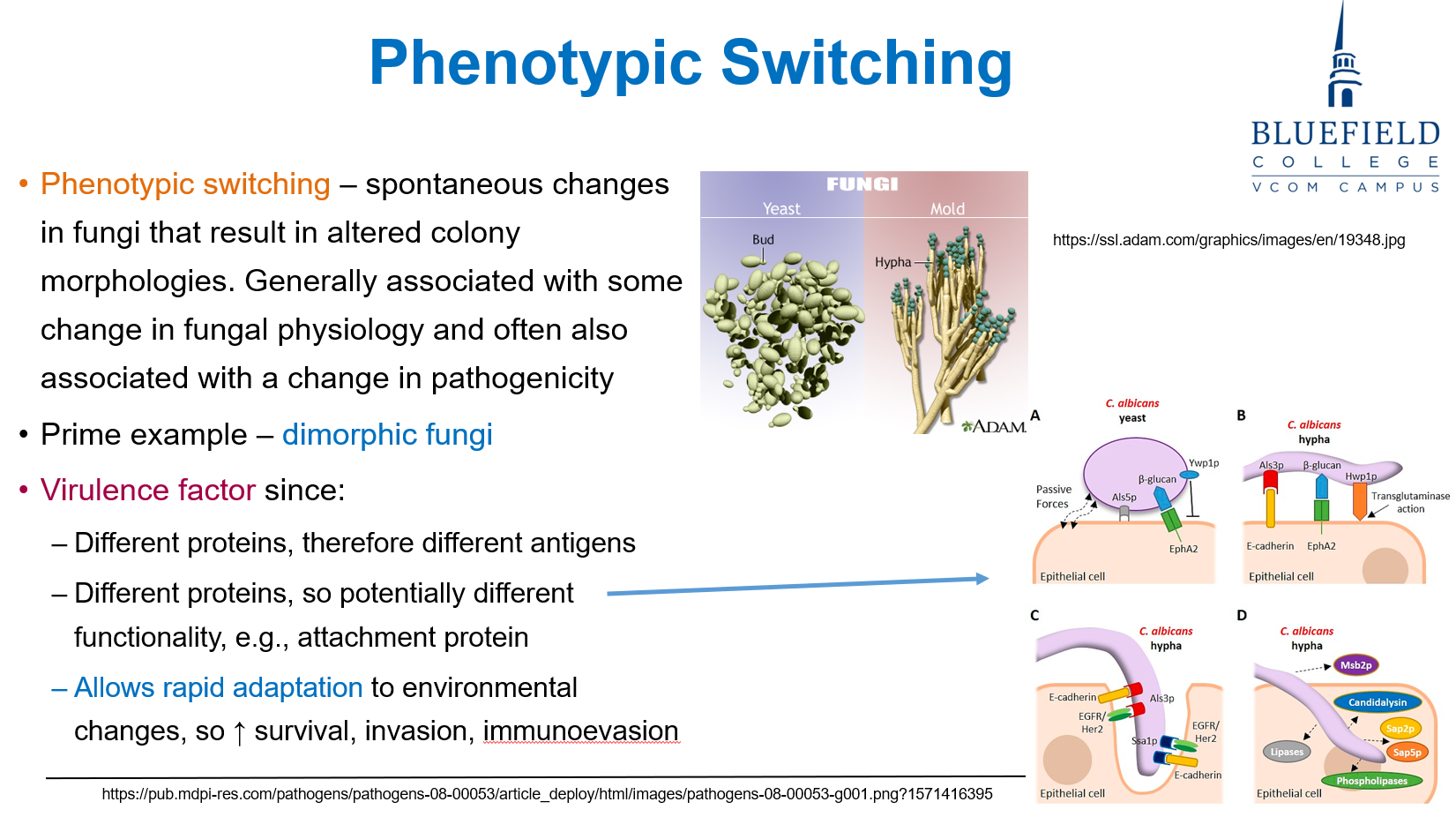
A dimorphic fungus changes morphology after entering the host. What is the likely advantage of this change?
A. Inhibition of antibody production
B. Increased tissue invasion via flagella
C. Enhanced uptake of iron and calcium
D. Activation of the host complement cascade
E. Decreased production of ergosterol
C. Enhanced uptake of iron and calcium
Phase variation, like dimorphism, aids in nutrient sequestration (e.g., iron, calcium) and adaptation to the host environment.
A 5-year-old child develops vomiting and liver dysfunction after eating moldy peanuts. No fungal growth is seen on biopsy. Which of the following best explains the disease process?
A. Disseminated fungal invasion
B. T-cell mediated hypersensitivity
C. Mycotoxin-induced organ damage
D. Overgrowth of gut commensal fungi
E. Allergic fungal rhinosinusitis
C. Mycotoxin-induced organ damage
Mycotoxicosis is intoxication, not infection. It results from ingestion of fungal toxins (e.g., aflatoxin), not fungal invasion.
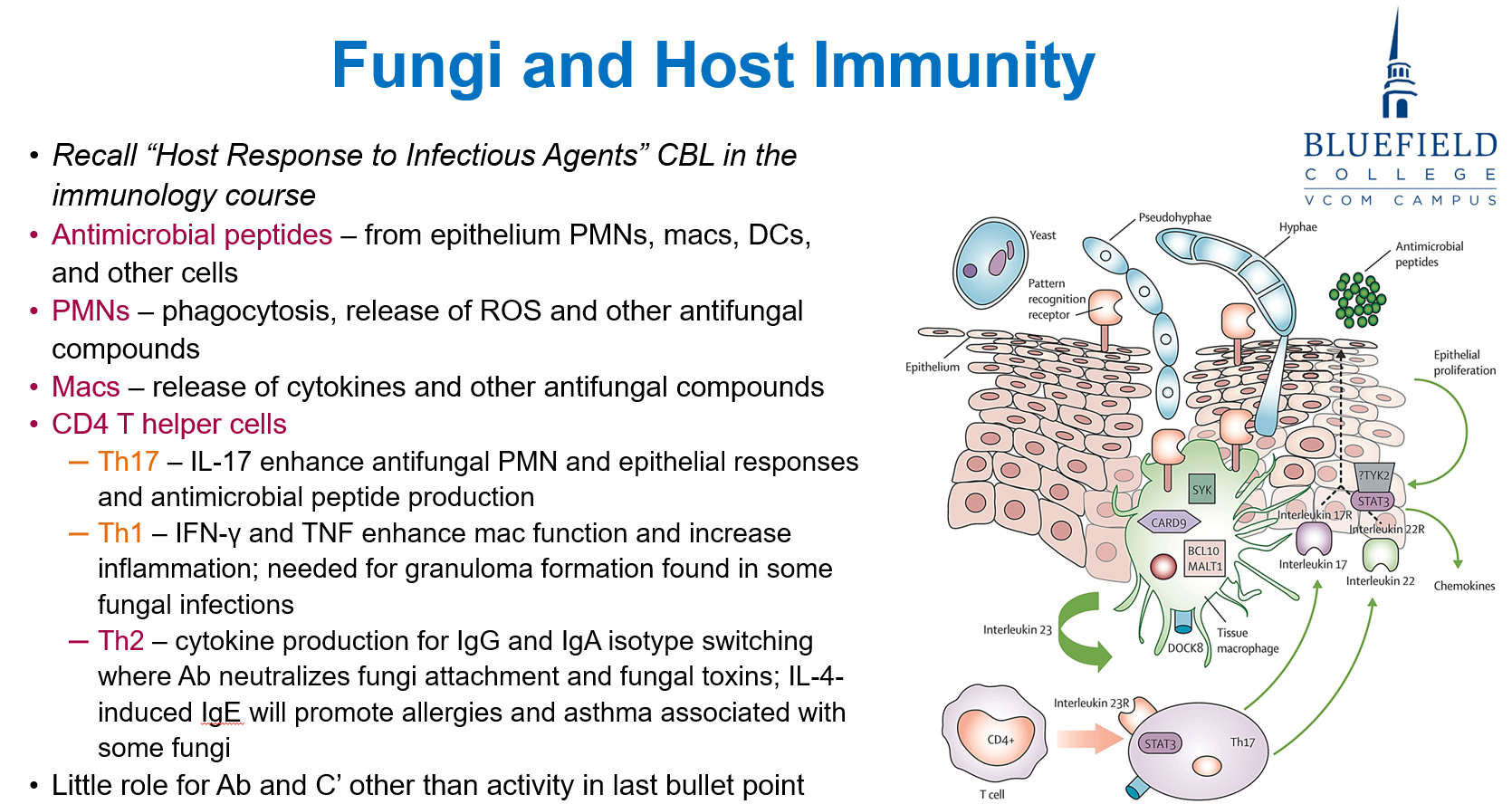
A 25-year-old patient with a genetic deficiency in IL-17 presents with recurrent fungal skin and mucosal infections. Which of the following immune processes is most likely impaired in this patient?
A. Neutrophil-mediated killing of fungi
B. Granuloma formation in response to fungi
C. IgE-mediated neutralization of fungal toxins
D. Antibody class switching to IgA
E. Eosinophil recruitment to infection sites
A. Neutrophil-mediated killing of fungi
Th17 cells produce IL-17, which promotes PMN recruitment and epithelial antimicrobial peptide production, both essential for antifungal defense at mucosal surfaces.
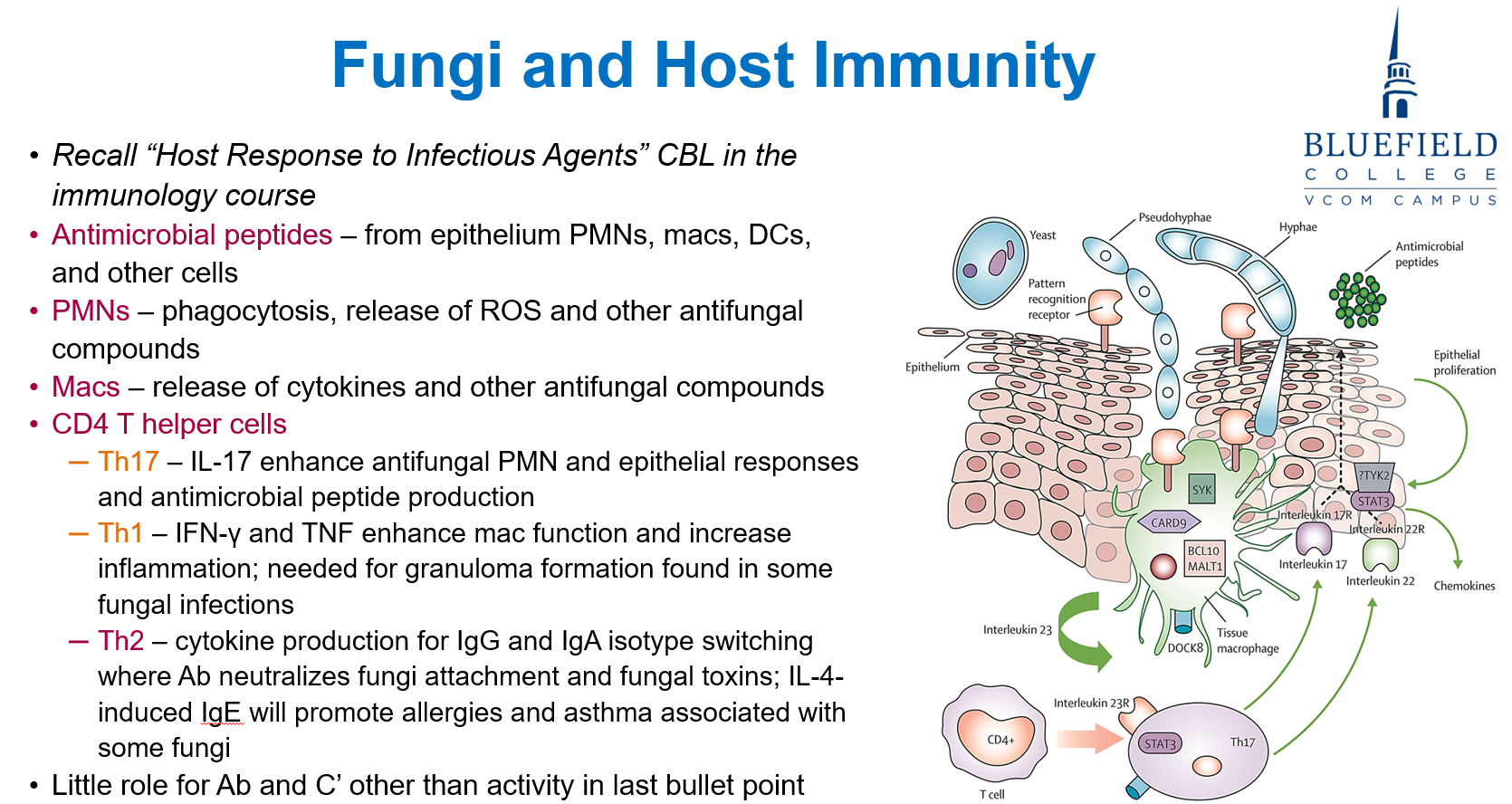
A 40-year-old woman with a history of seasonal allergies develops wheezing and shortness of breath. Bronchoalveolar lavage reveals Aspergillus fumigatus. Which T cell subset and immune product are most responsible for her allergic symptoms?
A. Th1; TNF
B. Th17; IL-17
C. Th2; IgE
D. Treg; IL-10
E. CD8+ T cells; perforin
C. Th2; IgE
Th2 cells produce IL-4, promoting IgE isotype switching, which mediates allergic responses like asthma in response to fungal antigens (e.g., Aspergillus).
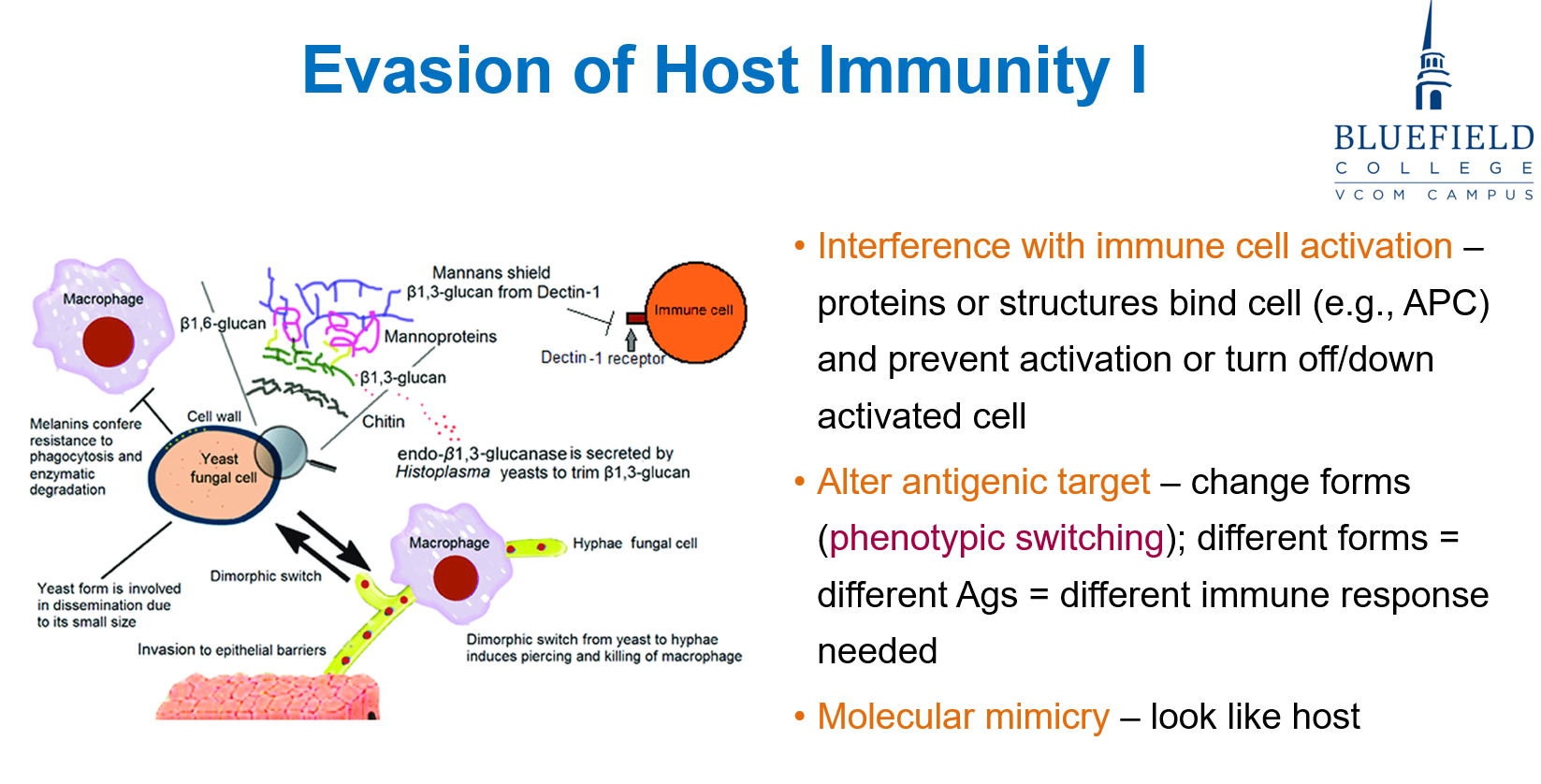
A fungus avoids host immunity by surviving within macrophages and producing antigens similar to host proteins. What are the primary immune evasion mechanisms?
A. Inhibition of IL-2 and IL-4
B. Capsule formation and spore shedding
C. Intracellular survival and molecular mimicry
D. Toxin release and complement inhibition
E. Antibody sequestration and capsule shedding
C. Intracellular survival and molecular mimicry
Fungi like Histoplasma can survive intracellularly and use molecular mimicry to resemble host proteins, avoiding detection.
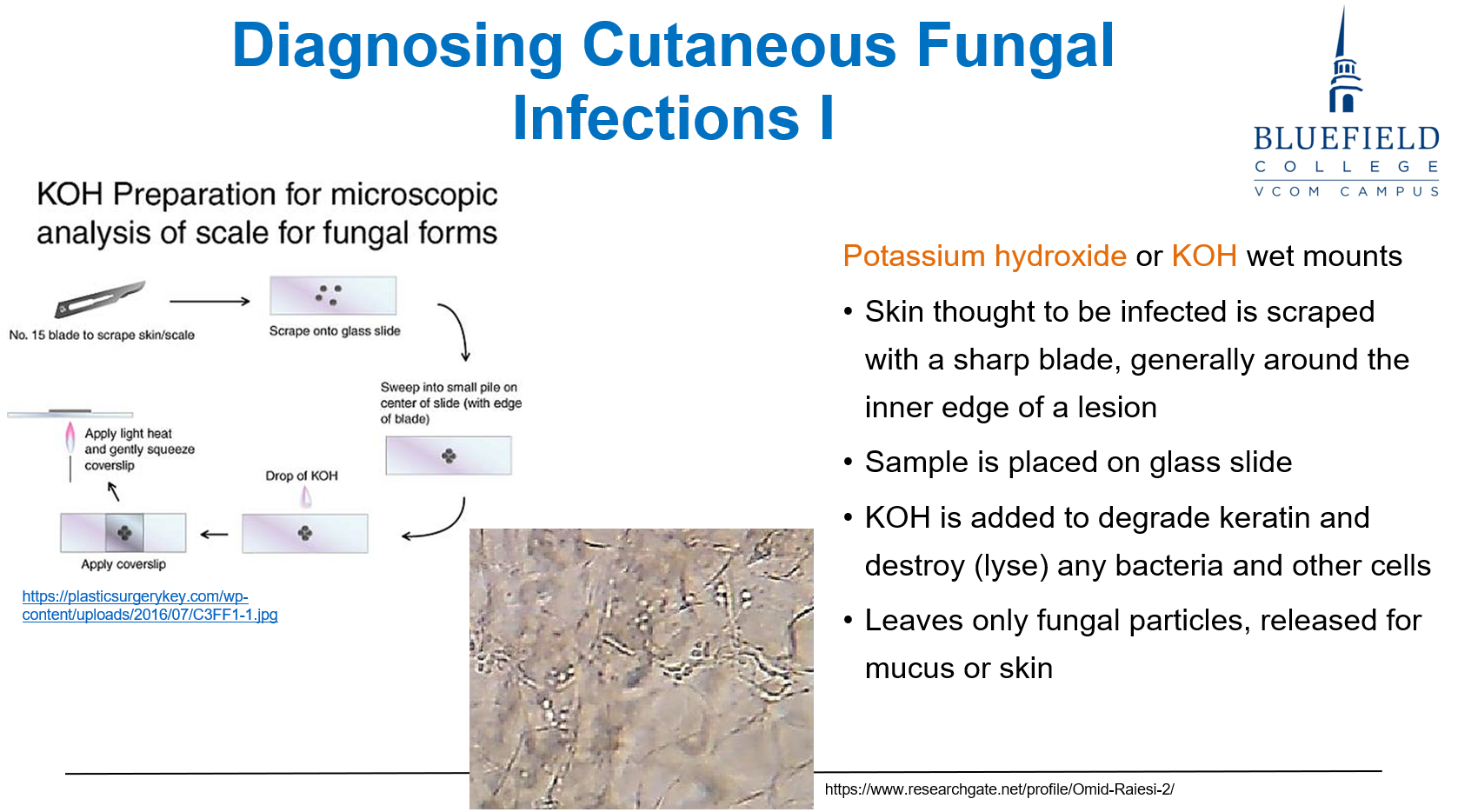
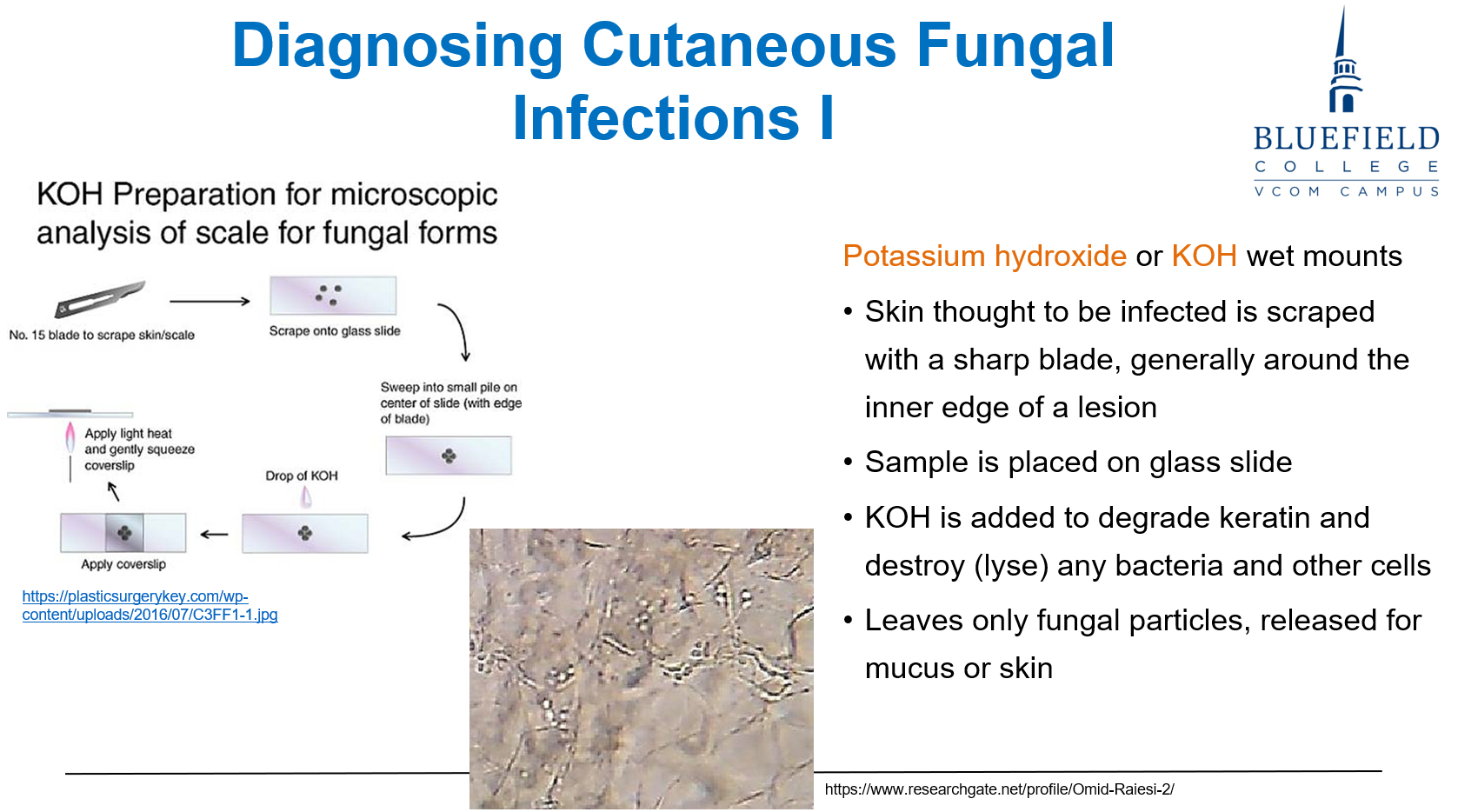
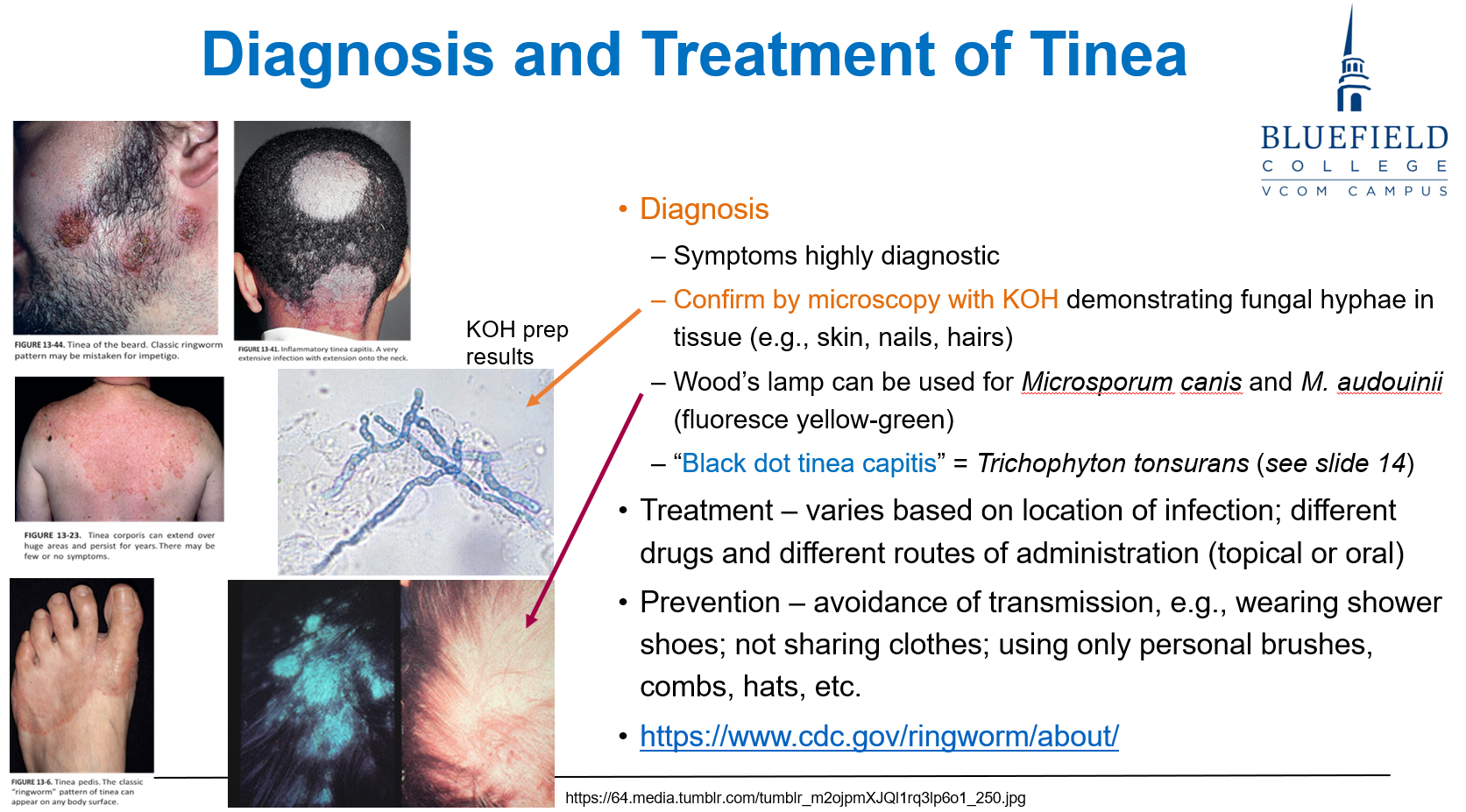
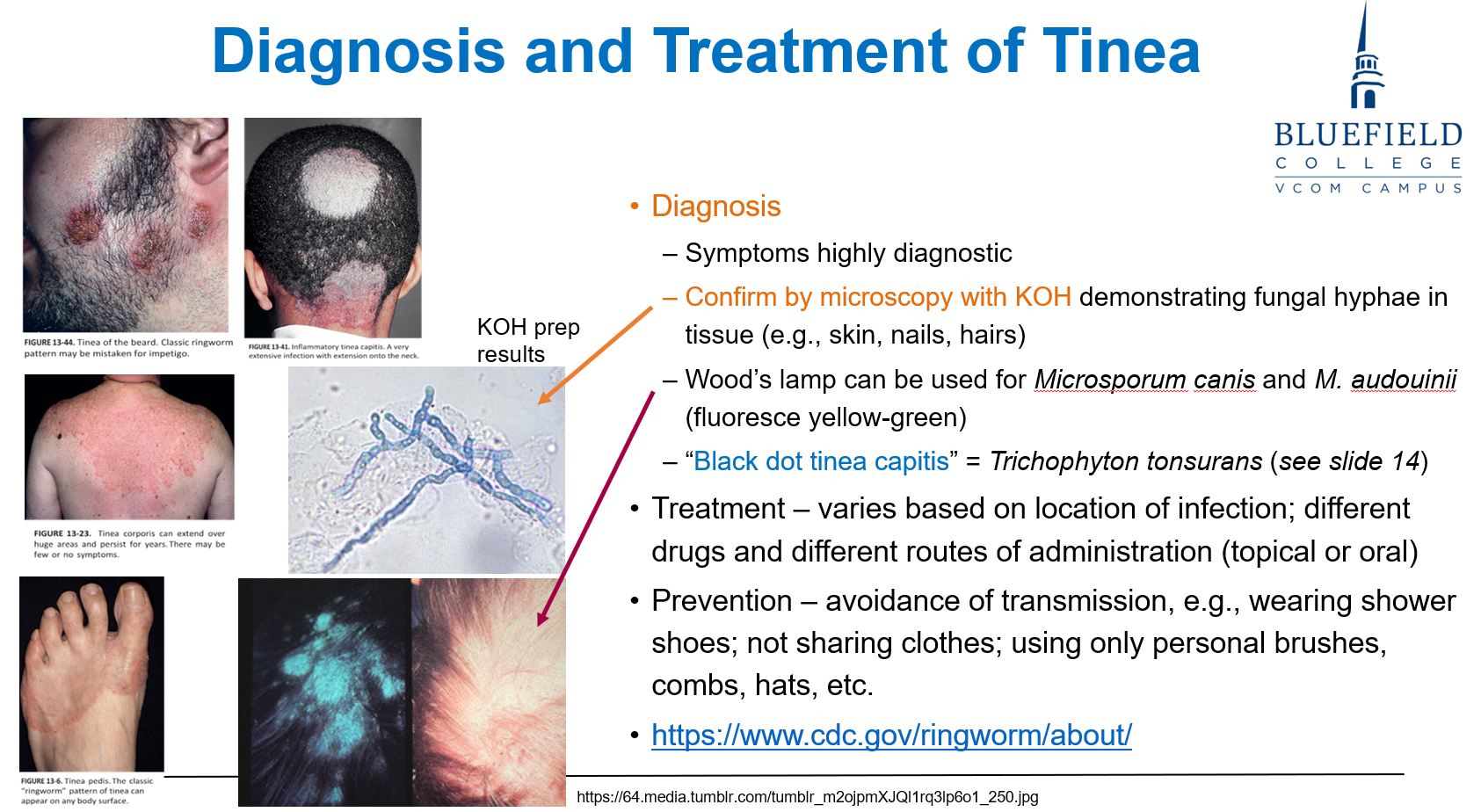
A physician suspects a superficial dermatophyte infection. Which of the following is the fastest and most cost-effective method to confirm the diagnosis?
A. GMS staining
B. Fungal culture on Sabouraud agar
C. PCR amplification of fungal genes
D. Potassium hydroxide prep
E. Serologic IgG detection
D. Potassium hydroxide prep
KOH prep is a rapid, inexpensive diagnostic tool that clears skin debris and reveals fungal elements under light microscopy.
Which of the following fungal structures directly inhibits phagocytosis and prevents immune cell activation?
A. Aerial hyphae
B. Polysaccharide capsule
C. β-glucan hydrolase
D. Ergosterol-rich membranes
E. Germ tube elongation
B. Polysaccharide capsule
The capsule, particularly in Cryptococcus neoformans, is anti-phagocytic and impairs immune activation, shielding the fungus from macrophage detection.
A fungal isolate undergoes phenotypic switching during growth in human tissue. Which of the following best describes how this aids in immune evasion?
A. Enhances spore production under stress
B. Allows the fungus to mimic host cell receptors
C. Changes surface antigens to avoid recognition
D. Inhibits T-cell receptor binding to MHC I
E. Increases polysaccharide thickness in the wall
C. Changes surface antigens to avoid recognition
Antigenic variation, such as dimorphism, allows fungi to alter their surface proteins, making it difficult for the adaptive immune system to recognize and respond.
A patient presents with a scaly rash suspected to be tinea corporis. Which of the following is the most rapid and cost-effective method to identify the presence of fungal elements?
A. Fungal culture on Sabouraud agar
B. Microscopic visualization using KOH prep
C. Giemsa staining of skin scraping
D. PCR-based fungal gene amplification
E. Immunofluorescence with pan-fungal antibodies
B. Microscopic visualization using KOH prep
KOH test rapidly dissolves keratin, revealing fungal morphologies under the microscope. It’s fast and inexpensive, making it ideal for superficial infections.
A 36-year-old HIV-positive man presents with headache and fever. CSF shows round yeast with a clear halo on India ink stain. What is the most likely organism?
A. Histoplasma capsulatum
B. Aspergillus fumigatus
C. Candida albicans
D. Cryptococcus neoformans
E. Fusarium spp.
D. Cryptococcus neoformans
India ink stain highlights the polysaccharide capsule of Cryptococcus, showing a clear halo around the organism. It is highly associated with AIDS patients and meningitis.
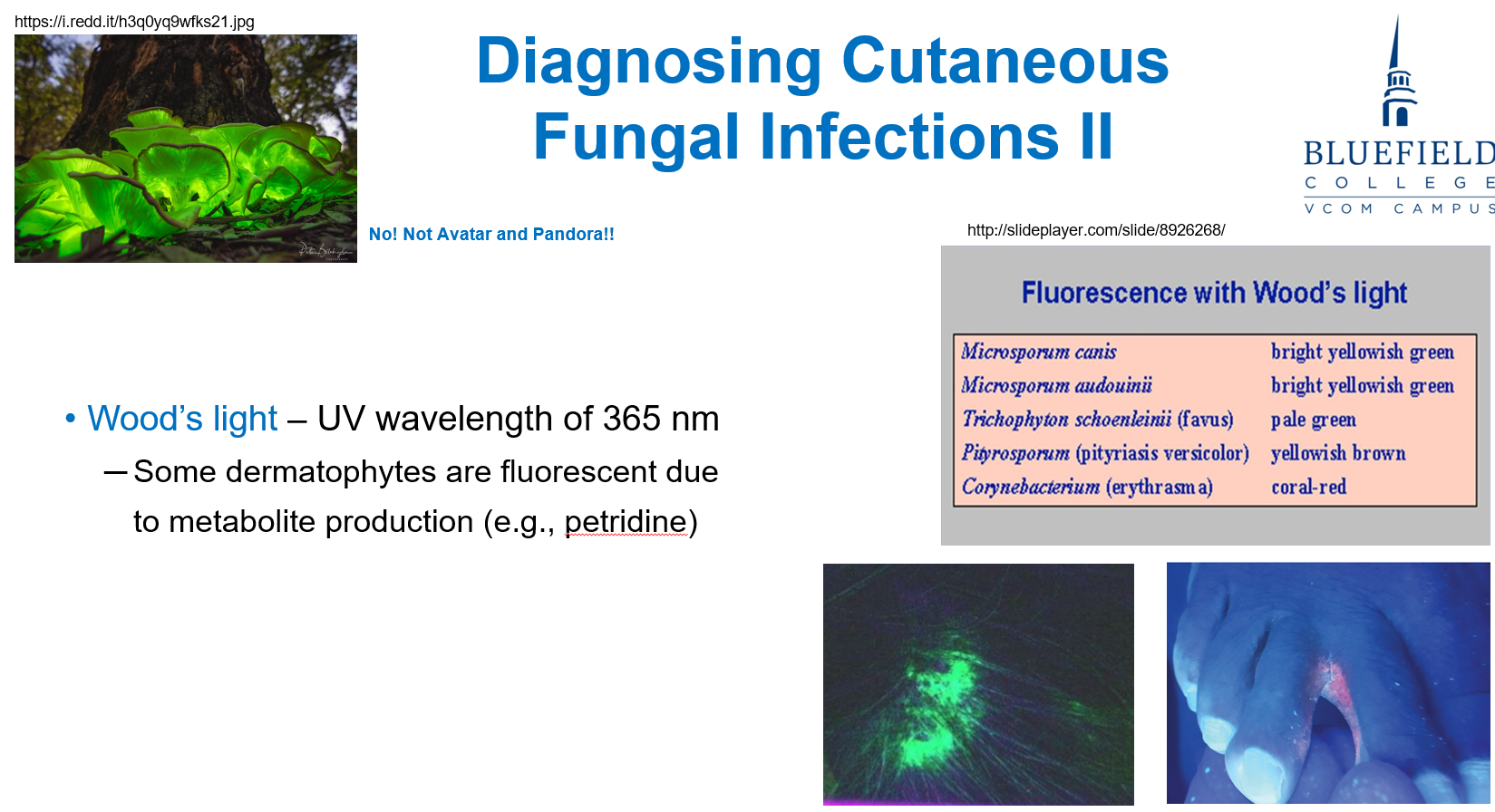
A child with hypopigmented skin patches is evaluated with a Wood’s lamp, which reveals green fluorescence. What is the clinical utility of this tool?
A. Detects deep tissue fungal infections
B. Identifies spore-producing hyphae
C. Highlights fungal pigments in certain dermatophytes
D. Visualizes capsule thickness in certain yeast
E. Measures cell wall integrity in certain fungi
C. Highlights fungal pigments in certain dermatophytes
Wood’s lamp emits UV light that causes fluorescence in some dermatophytes, especially those producing petridine. It helps confirm cutaneous fungal infections.
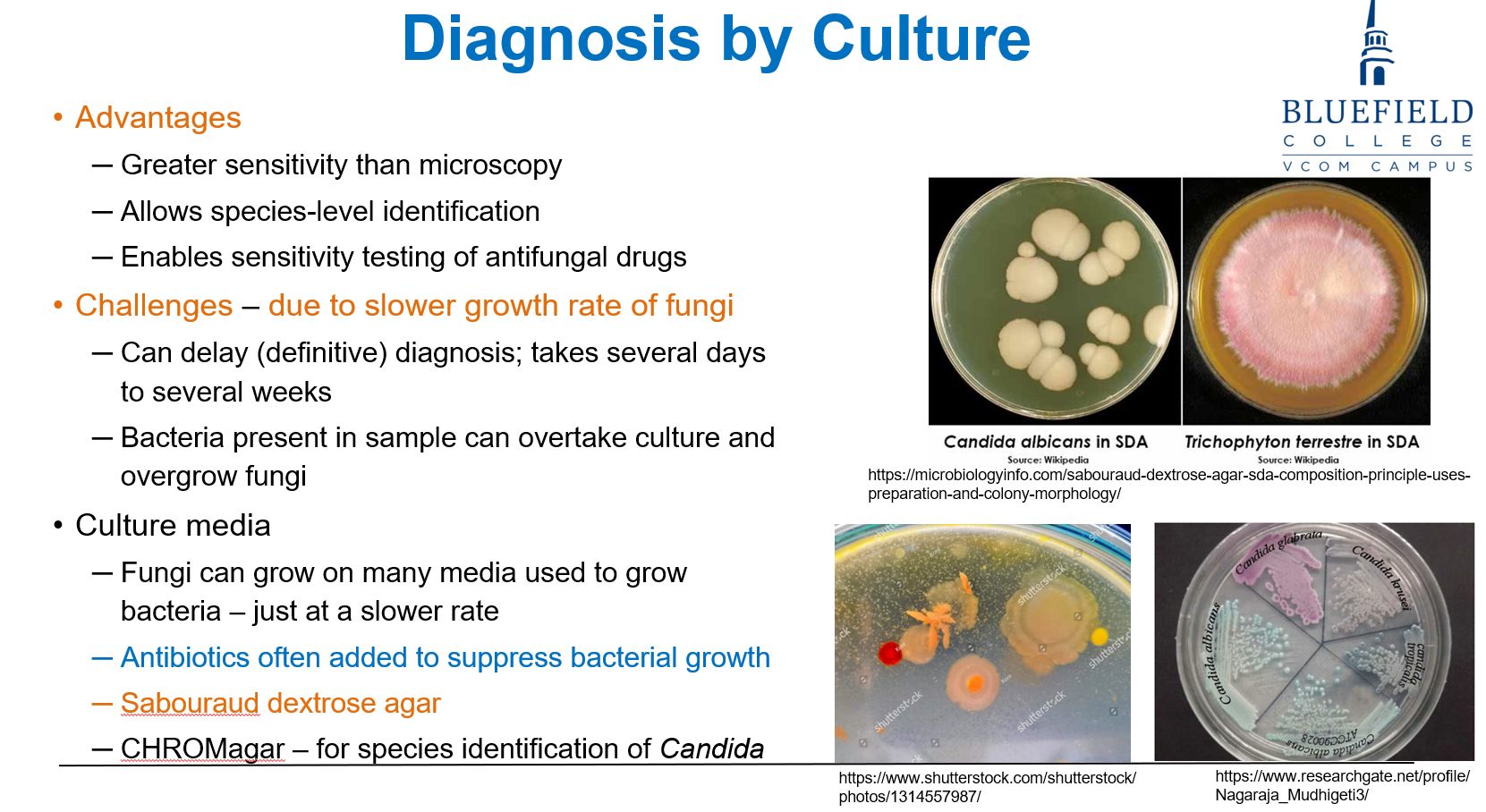
A 44-year-old woman with vaginal candidiasis has a sample plated on CHROMagar. Colonies appear in different colors. What is the primary advantage of this medium?
A. Detects antifungal resistance
B. Promotes growth of dimorphic fungi
C. Enhances visualization of capsule
D. Differentiates fungal species based on colony color
E. Shortens the incubation time to less than 24 hours
D. Differentiates fungal species based on colony color
CHROMagar is a differential medium that allows species-level identification of Candida by colony color differences. It improves diagnostic precision over standard media.
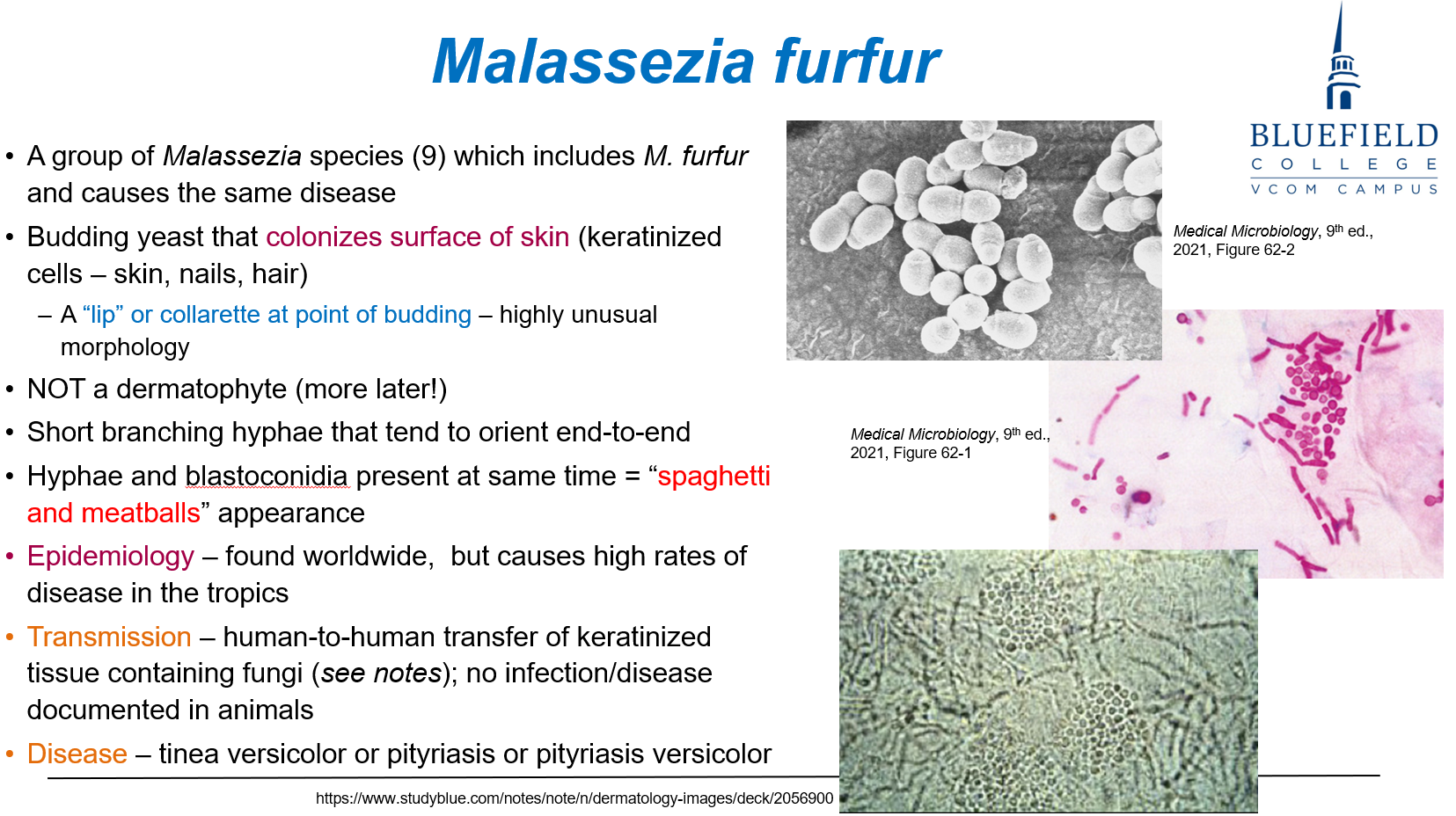
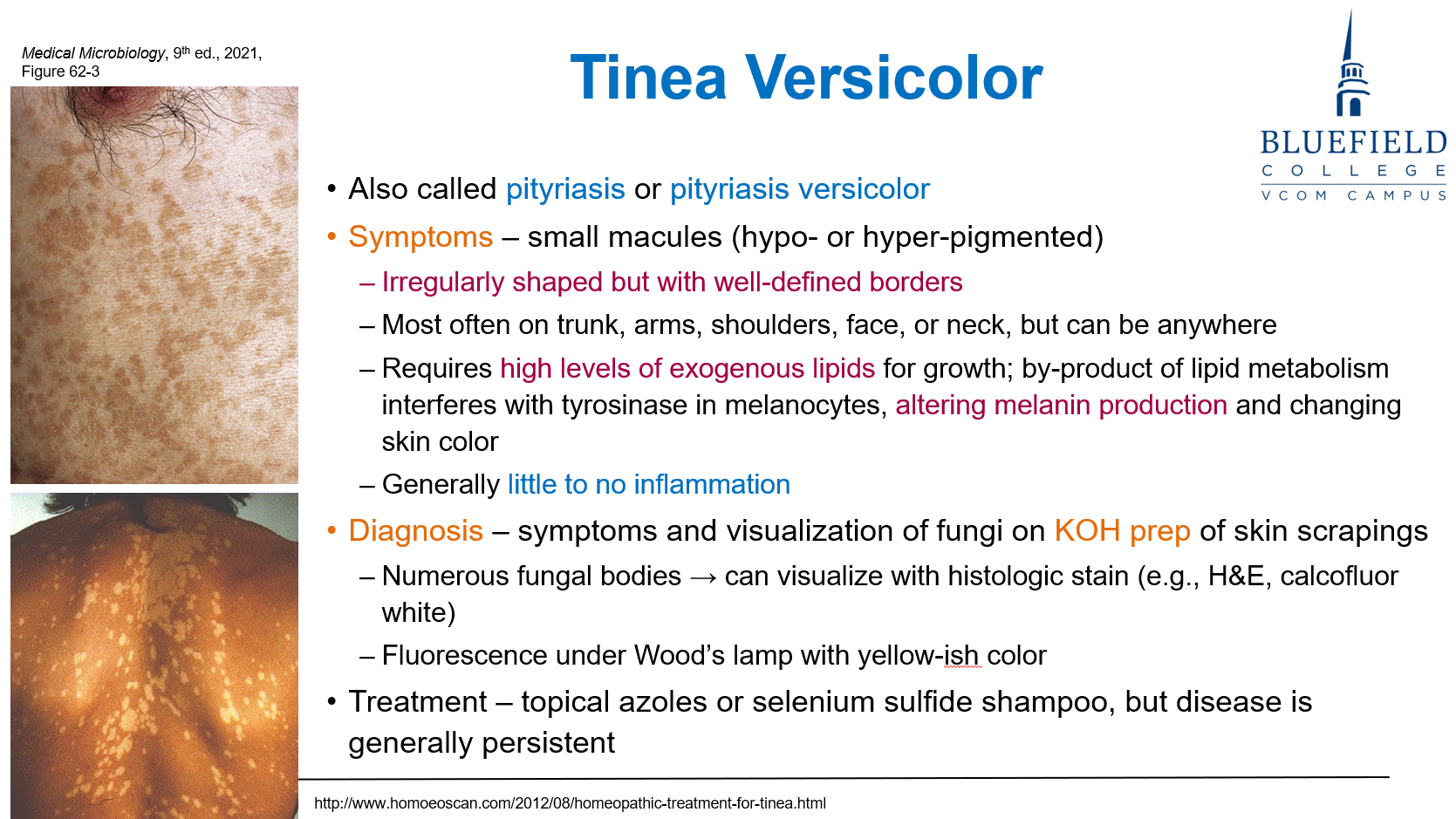
A 24-year-old woman presents with hypopigmented macules on her upper back. KOH prep reveals yeast and short hyphae. What is the most likely microscopic finding?
A. Branching septate hyphae forming mats
B. Spherical yeasts with thick capsules
C. “Spaghetti and meatballs” appearance
D. Cigar-shaped yeast cells in chains
E. Broad, non-septate hyphae with sporangia
C. “Spaghetti and meatballs” appearance
Malassezia furfur shows hyphae and yeast cells together, forming this distinctive appearance.
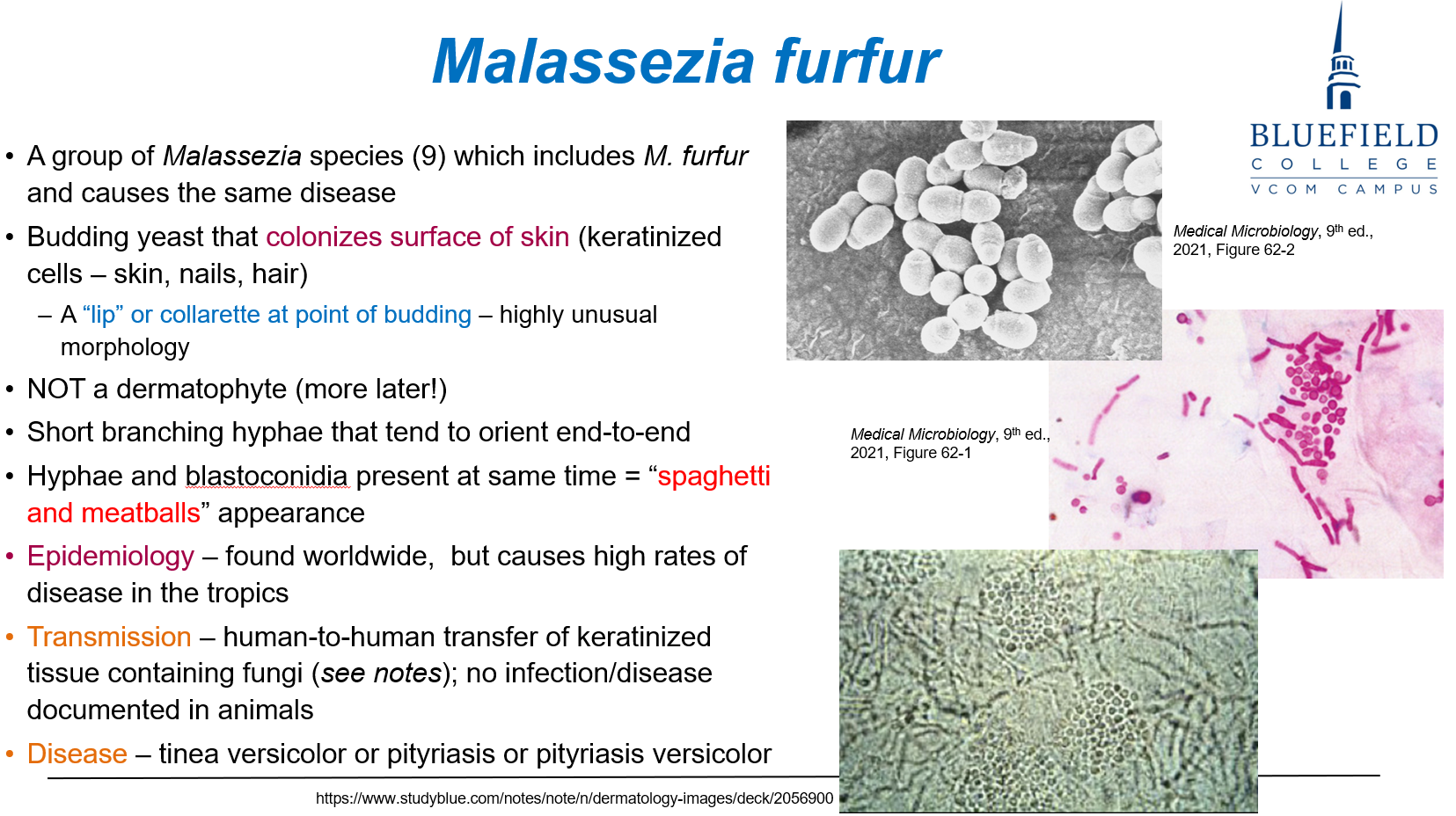
How is Malassezia furfur most commonly transmitted?
A. Inhalation of airborne spores
B. Penetrating trauma through thorns
C. Human-to-human transfer of keratinized tissue
D. Animal bites
E. Contaminated water exposure
C. Human-to-human transfer of keratinized tissue
Malassezia is spread through direct skin contact involving keratinized material.
What causes the pigment change seen in tinea versicolor?
A. Iron deposition in dermis
B. Melanin production from fungal pigments
C. Lipid metabolism byproducts disrupting melanocytes
D. Immune destruction of melanocytes
E. Dermal hemorrhage due to fungal toxins
C. Lipid metabolism byproducts disrupting melanocytes
Malassezia requires lipids, and its metabolic byproducts inhibit tyrosinase, affecting melanin synthesis.
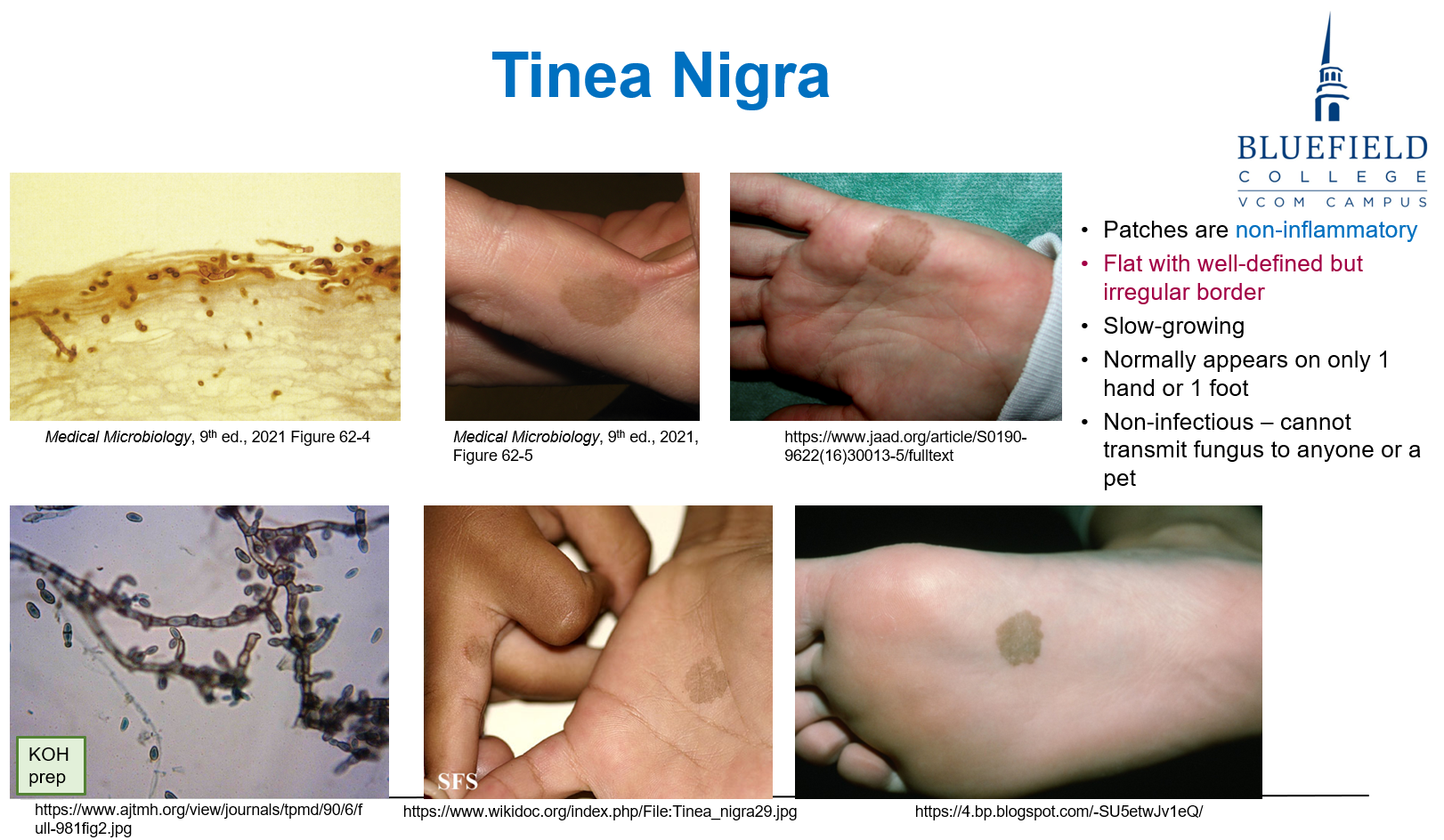
Which of the following best describes the clinical appearance of tinea nigra?
A. Itchy, scaly, red plaques on trunk
B. Painful nodules with regional lymphadenopathy
C. Gray-black patches on palms or soles, non-inflammatory
D. Hypopigmented macules with mild scaling
E. Boggy pustular scalp lesions with hair loss
C. Gray-black patches on palms or soles, non-inflammatory
Hortaea werneckii causes tinea nigra, a superficial pigmented patch with no inflammation.
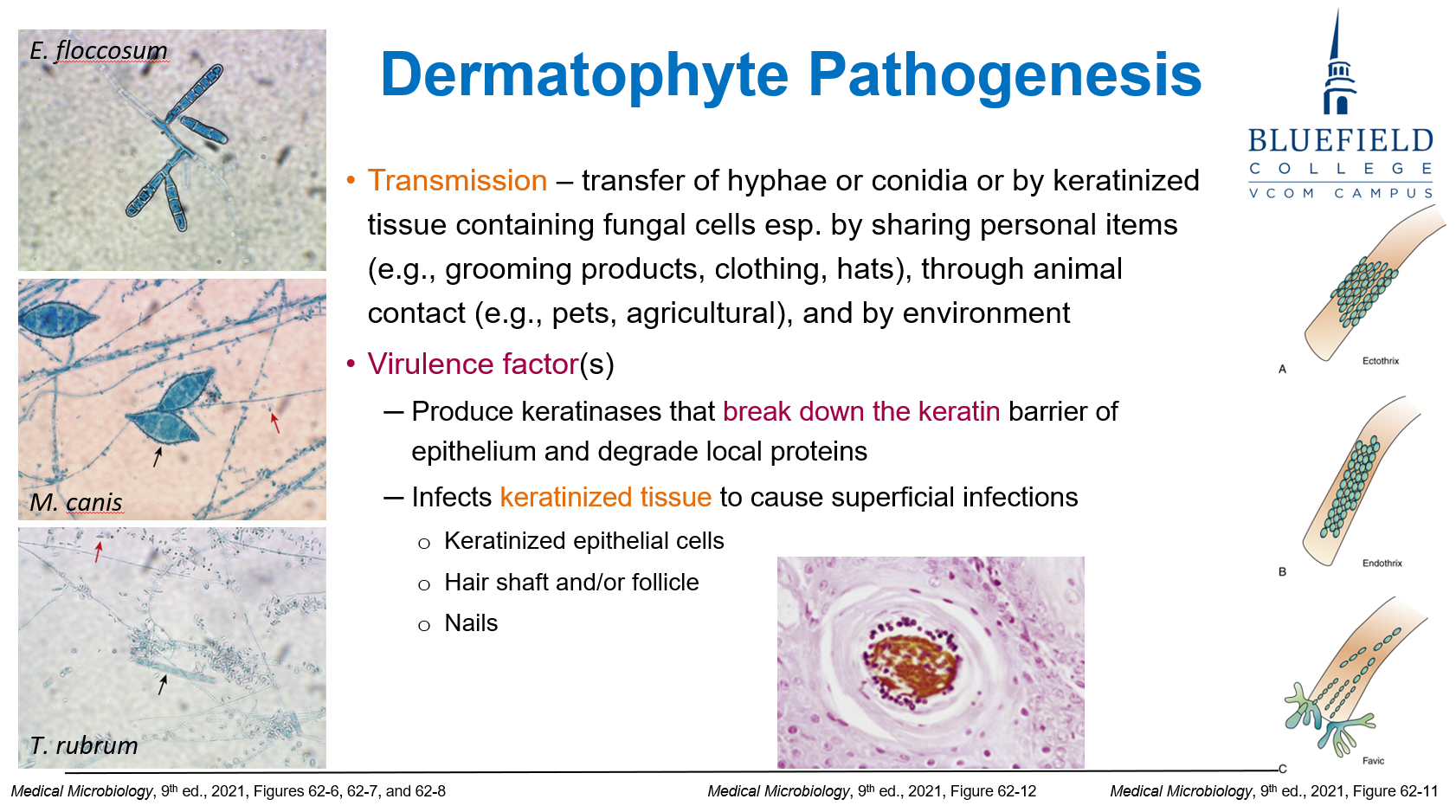
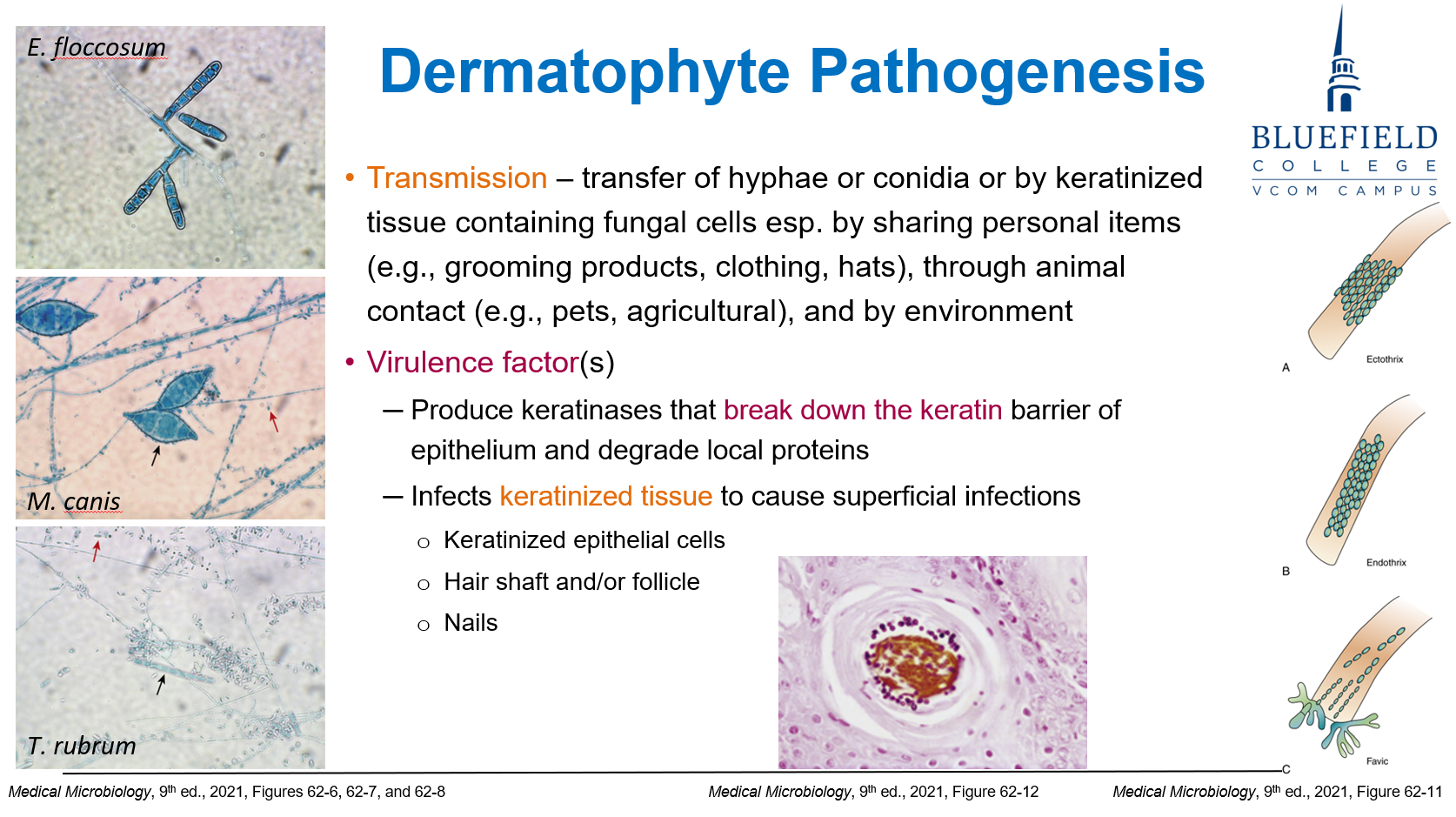
Which of the following best characterizes dermatophytes?
A. Encapsulated yeast with narrow budding
B. Filamentous fungi with septate hyphae and conidia
C. Cigar-shaped yeast with eosinophilic asteroid bodies
D. Broad, coenocytic hyphae
E. Dimorphic yeast producing melanin
B. Filamentous fungi with septate hyphae and conidia
Dermatophytes (e.g., Trichophyton, Microsporum) are filamentous fungi with septate hyphae.
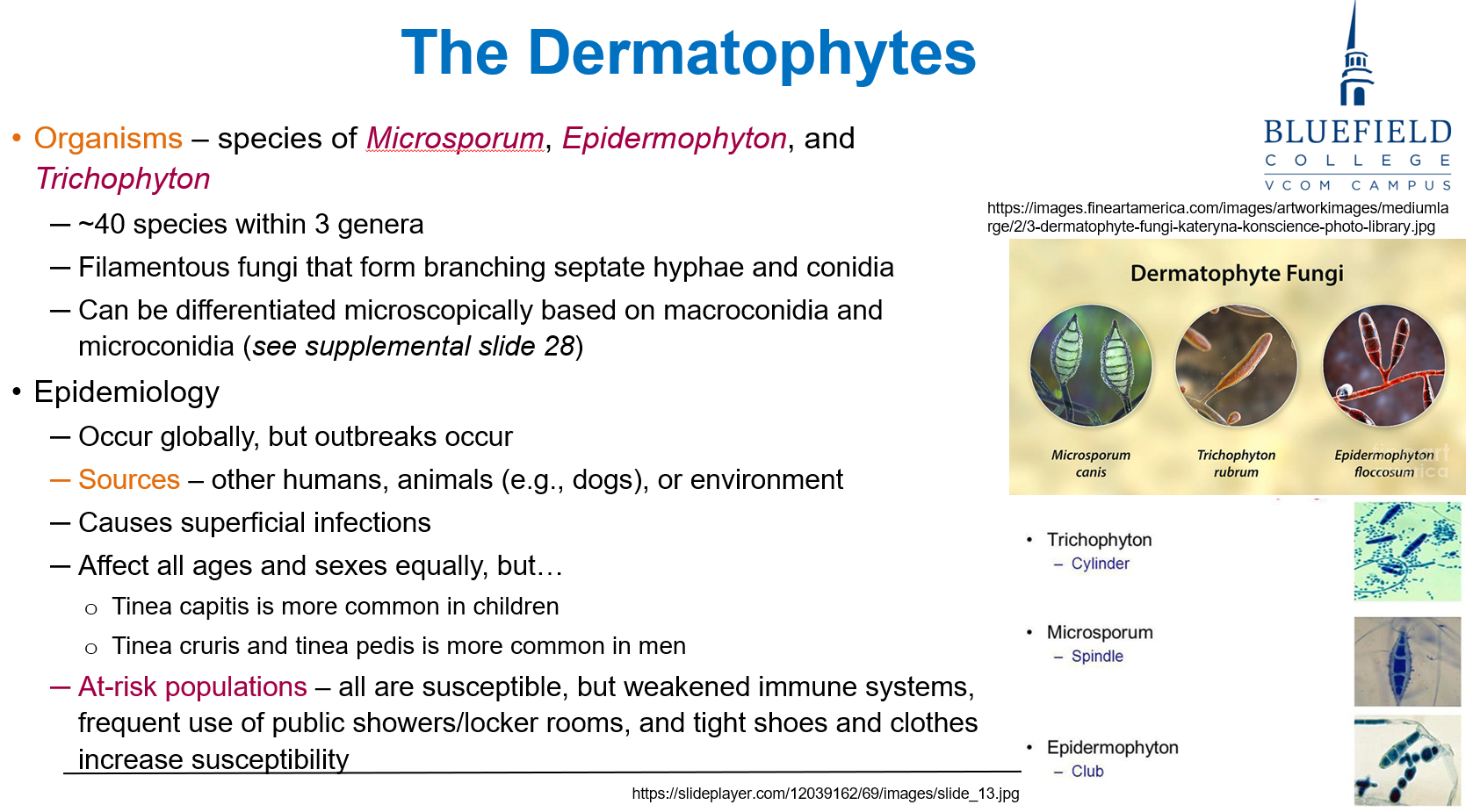
Dermatophytes are most commonly transmitted through:
A. Bloodborne exposure
B. Human and animal contact with infected keratin
C. Aerosol droplets in healthcare settings
D. Ingestion of contaminated food
E. Transplacental passage
B. Human and animal contact with infected keratin
Dermatophytes infect keratinized tissues and spread via contact with infected skin, hair, or nails.
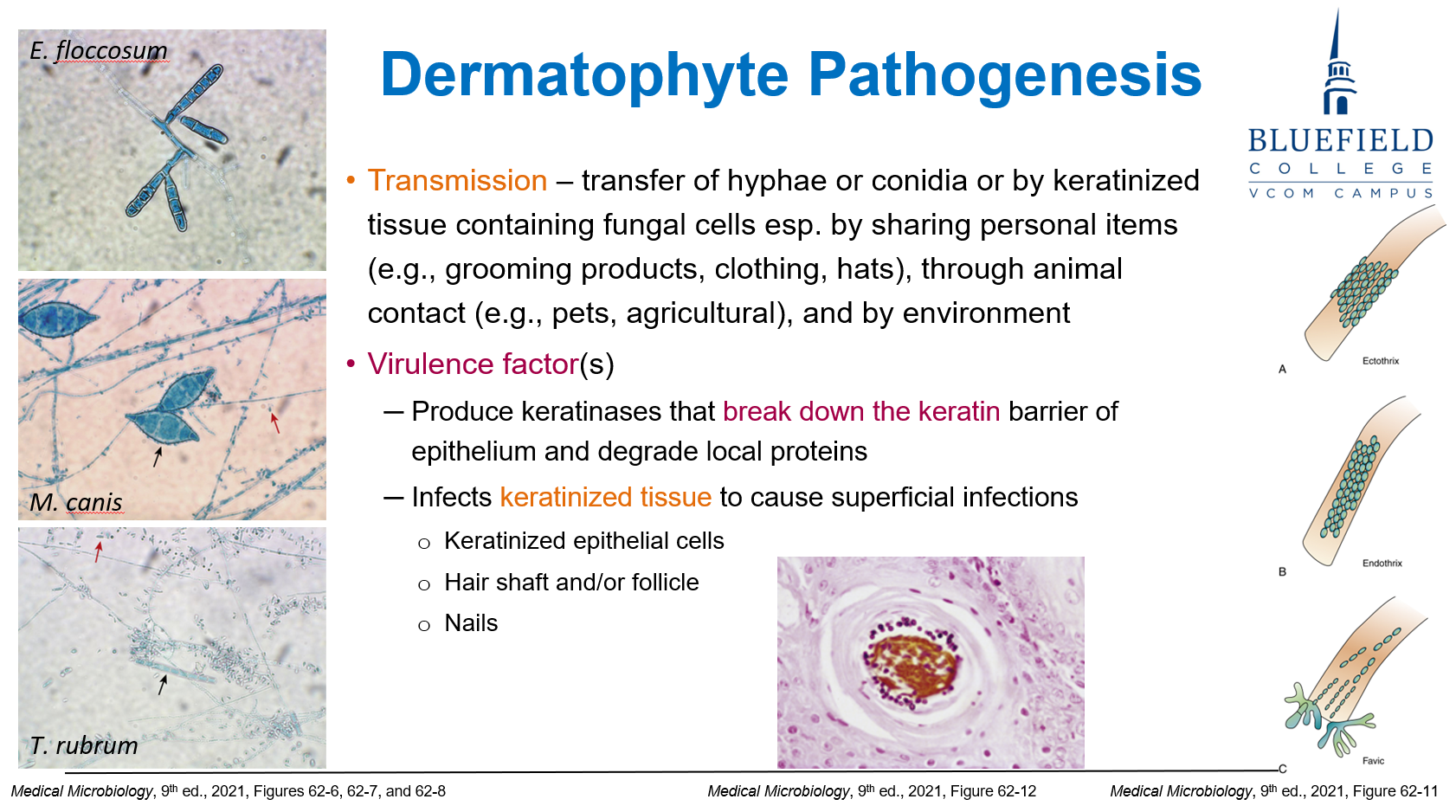
What enzyme allows dermatophytes to invade the skin?
A. Elastase
B. Protease A
C. Urease
D. Keratinase
E. Lipase
D. Keratinase
Dermatophytes produce keratinase, breaking down keratin in the epidermis, nails, and hair.
A patient presents with an annular, scaly rash with central clearing. What is the most likely diagnosis?
A. Erythema nodosum
B. Tinea corporis
C. Psoriasis
D. Tinea nigra
E. Tinea versicolor
B. Tinea corporis
Tinea corporis presents with ring-shaped lesions; scaly, pruritic, and often with central clearing.
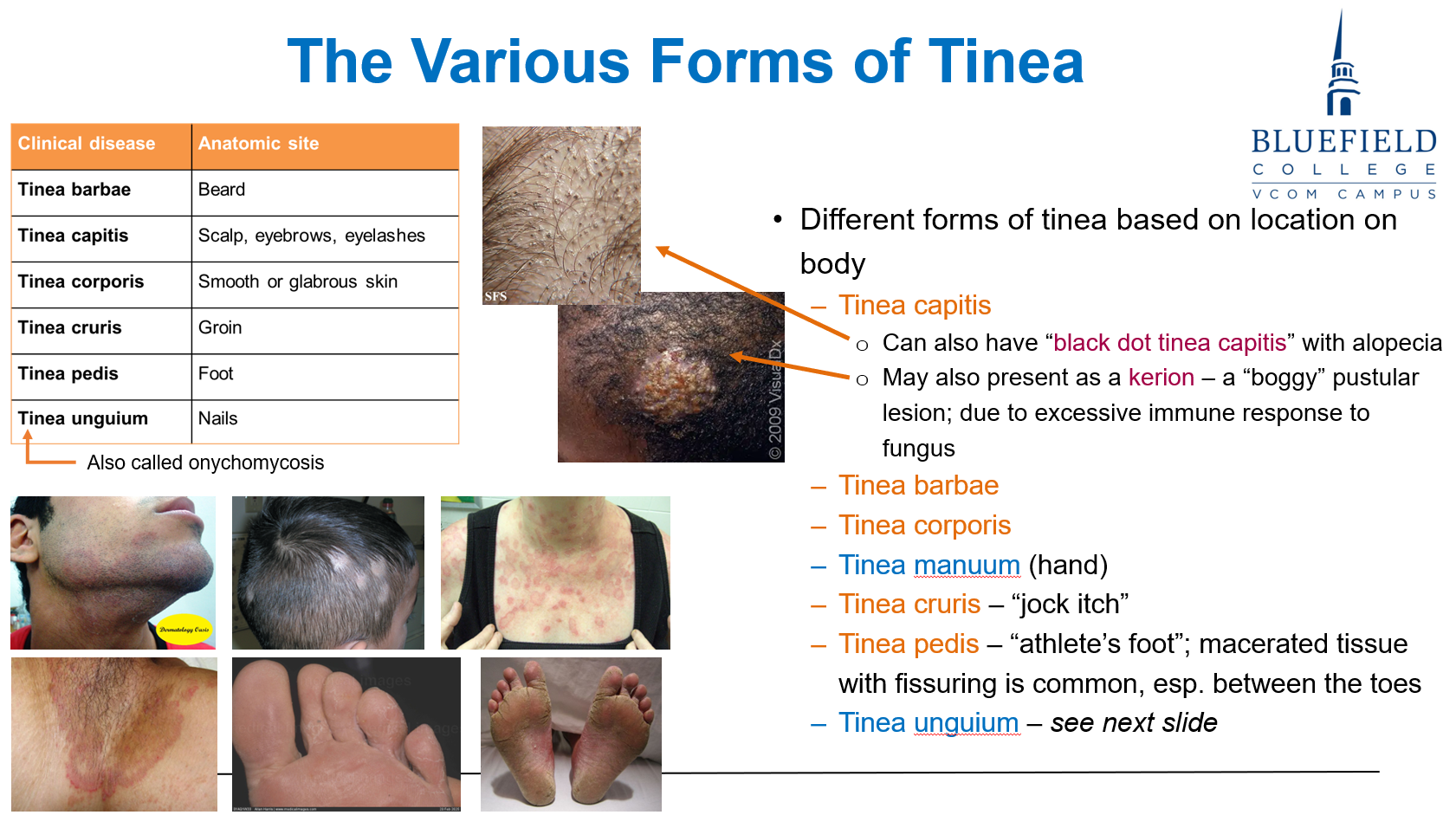
Which form of tinea capitis shows black dots due to broken hairs?
A. Kerion
B. Favus
C. Black dot type
D. Seborrheic variant
E. Pustular impetigo
C. Black dot type
Black dot tinea capitis shows broken hair shafts, appearing as black dots on scalp.
Which of the following is not a risk factor for onychomycosis?
A. Tinea pedis
B. Immunosuppression
C. Peripheral vascular disease
D. Nail trauma
E. Antibiotic overuse
E. Antibiotic overuse
Antibiotics are not direct risk factors. Nail trauma, tinea, and PVD are.
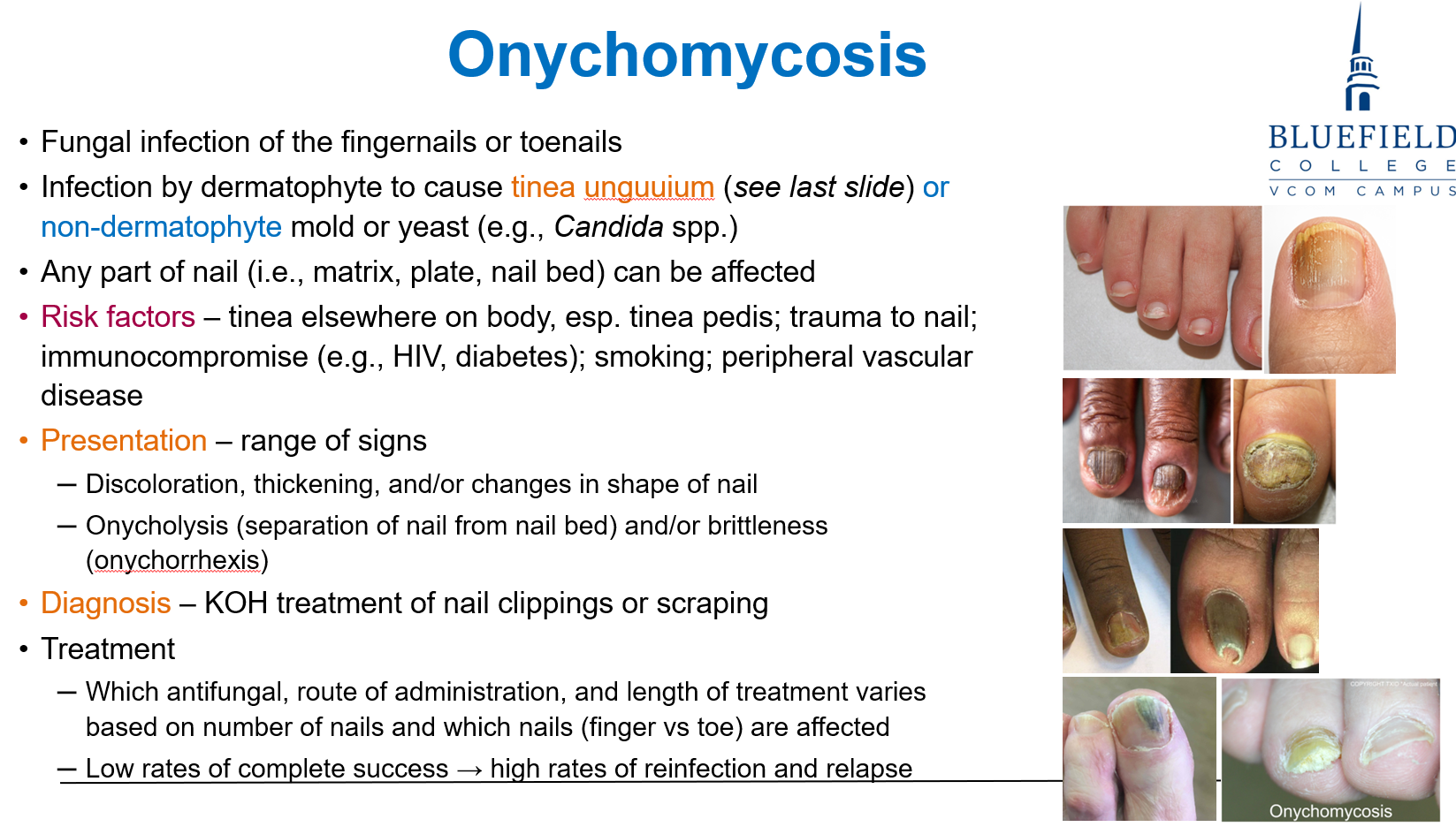
What is the first-line diagnostic test for suspected fungal nail infection?
A. Gram stain
B. Blood culture
C. PCR of nail sample
D. KOH prep of nail clippings
E. Wood’s lamp
D. KOH prep of nail clippings
KOH prep is fast, dissolves keratin, and shows fungal hyphae in nails.
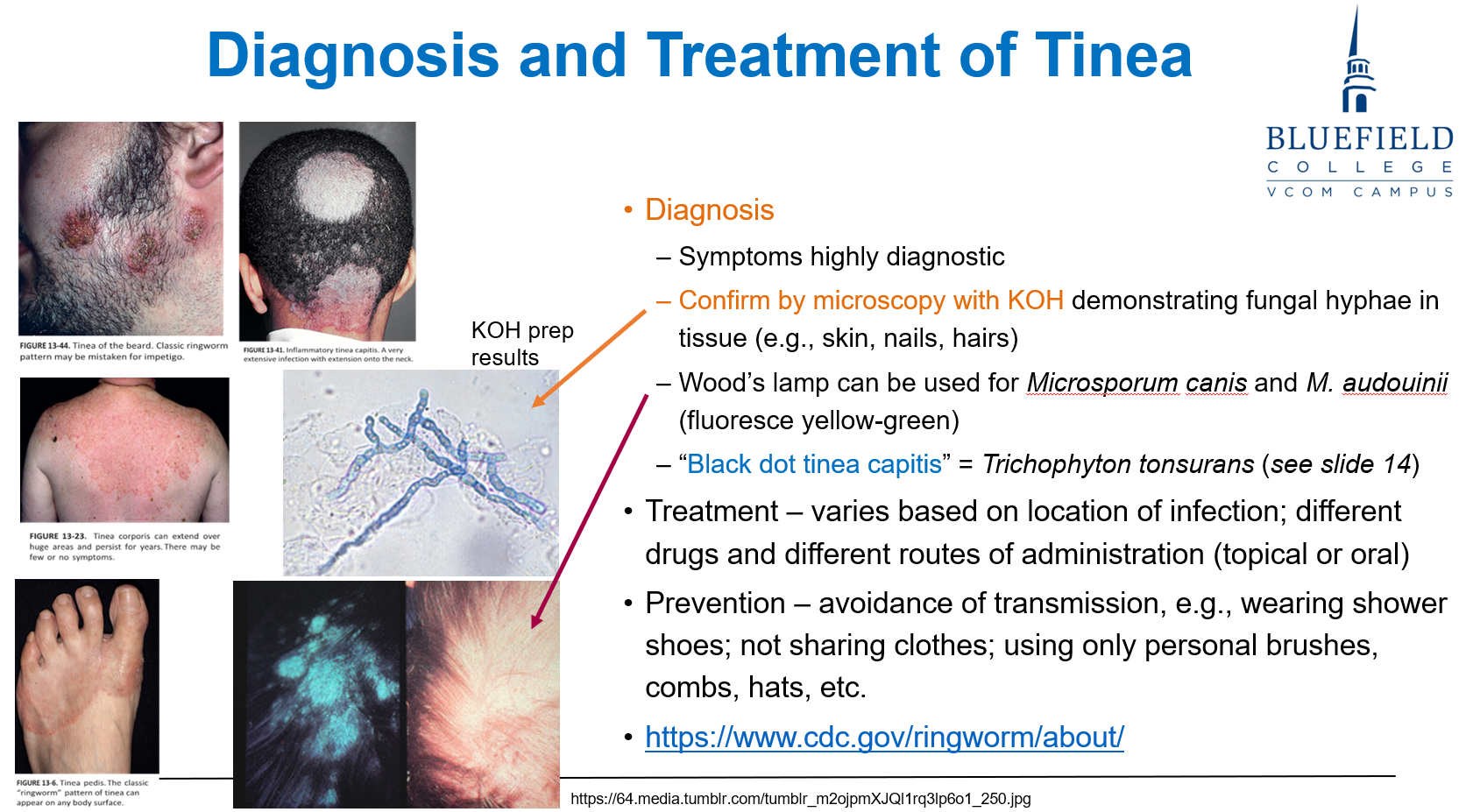
A child presents with scalp scaling and hair loss. Which organism fluoresces under Wood’s lamp?
A. Trichophyton rubrum
B. Candida albicans
C. Sporothrix schenckii
D. Microsporum canis
E. Malassezia furfur
D. Microsporum canis
Microsporum species, such as M. canis, fluoresce yellow-green under UV light.
Which activity is most likely to lead to infection with Sporothrix schenckii?
A. Swimming in freshwater lakes
B. Gardening with rose bushes
C. Eating undercooked shellfish
D. Caring for feral cats
E. Walking barefoot on sand
B. Gardening with rose bushes
S. schenckii is transmitted via rose thorns or soil inoculation.
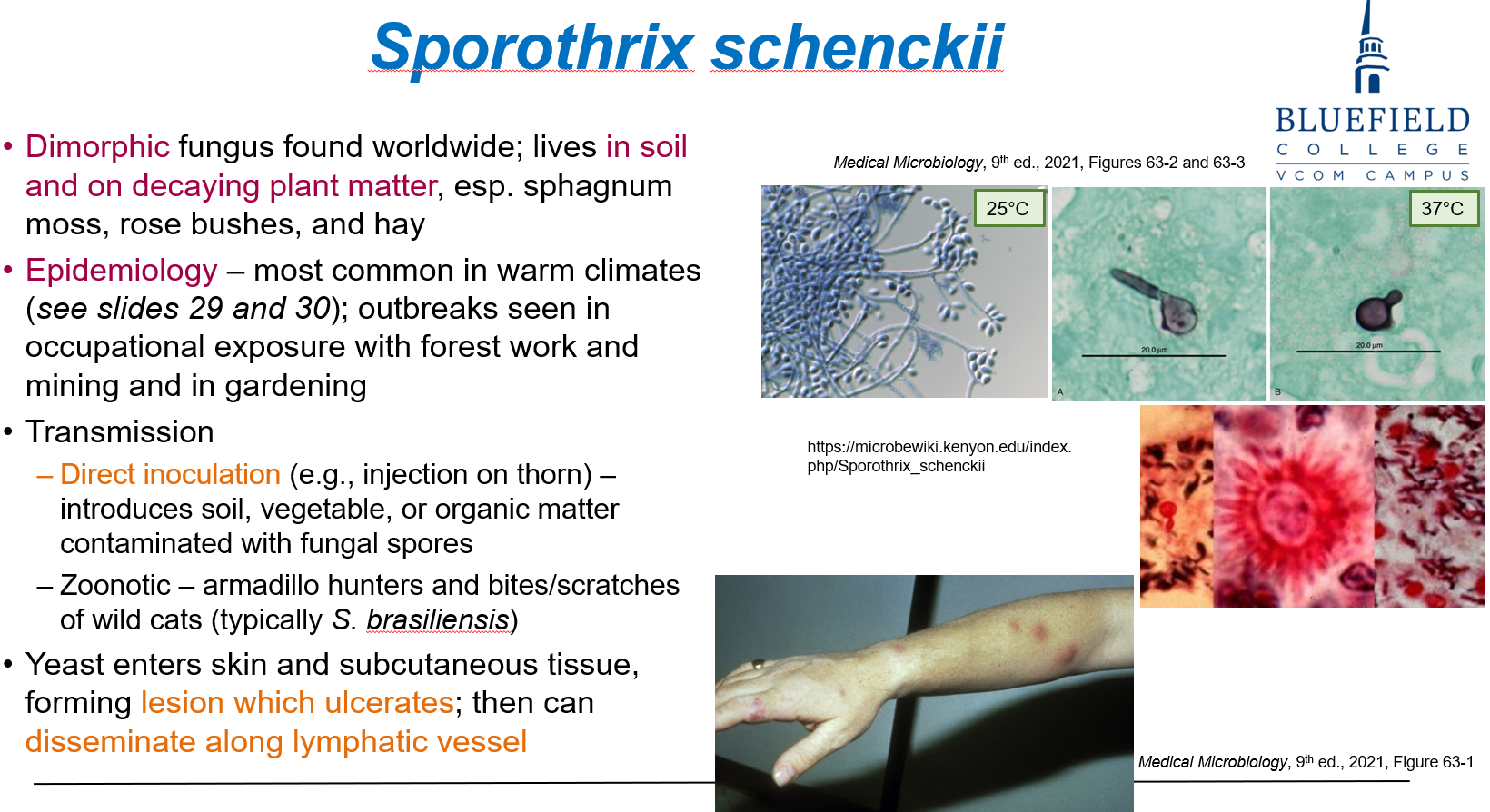
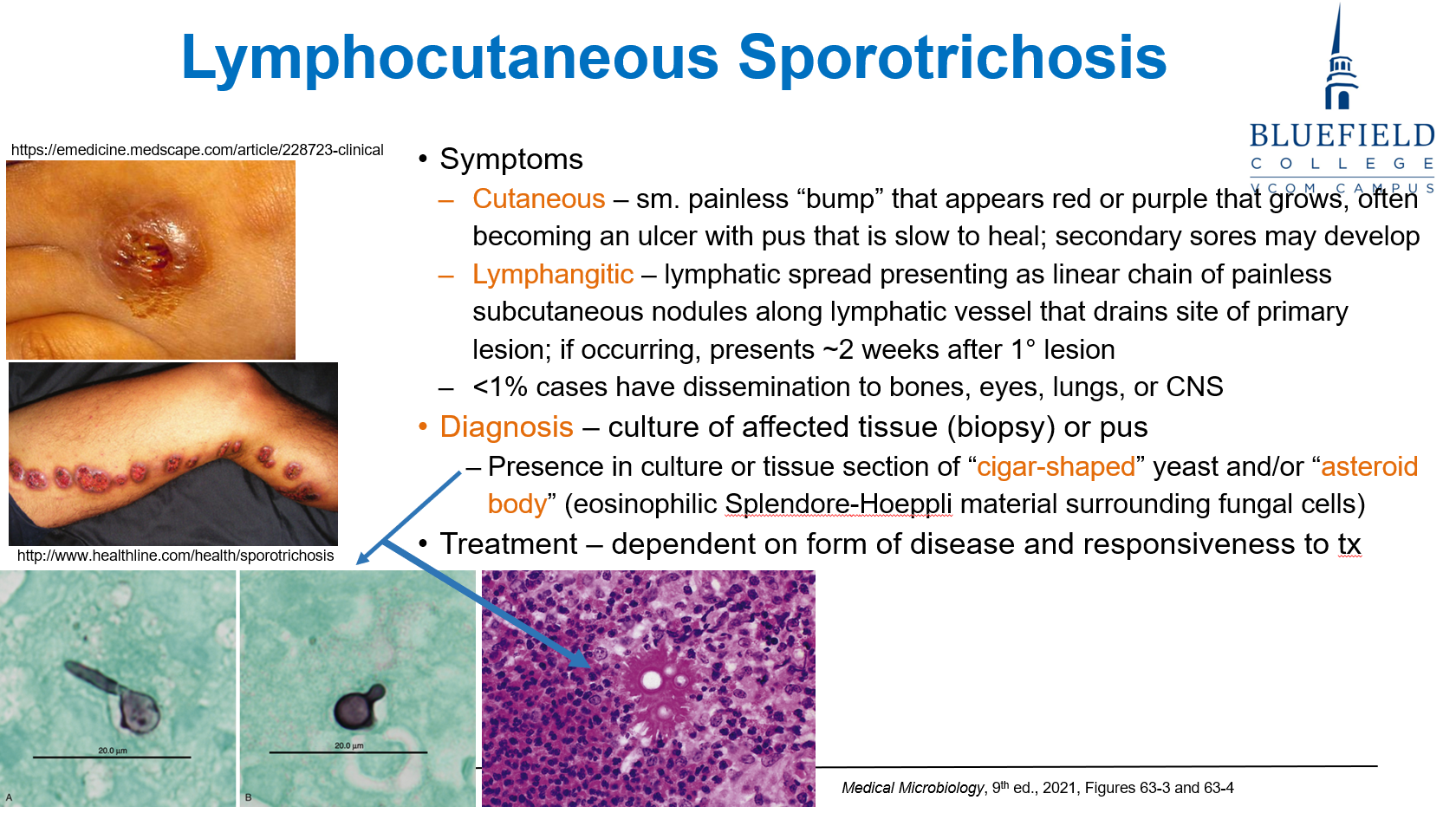
Which best describes lymphocutaneous sporotrichosis?
A. Erythematous patches with central vesicles
B. Systemic fungemia with liver abscesses
C. Ulcerated lesion with nodules along lymphatics
D. Necrotic skin plaque with crusting
E. Pustules on oral mucosa
C. Ulcerated lesion with nodules along lymphatics
Sporothrix spreads along lymphatics, forming subcutaneous nodules.
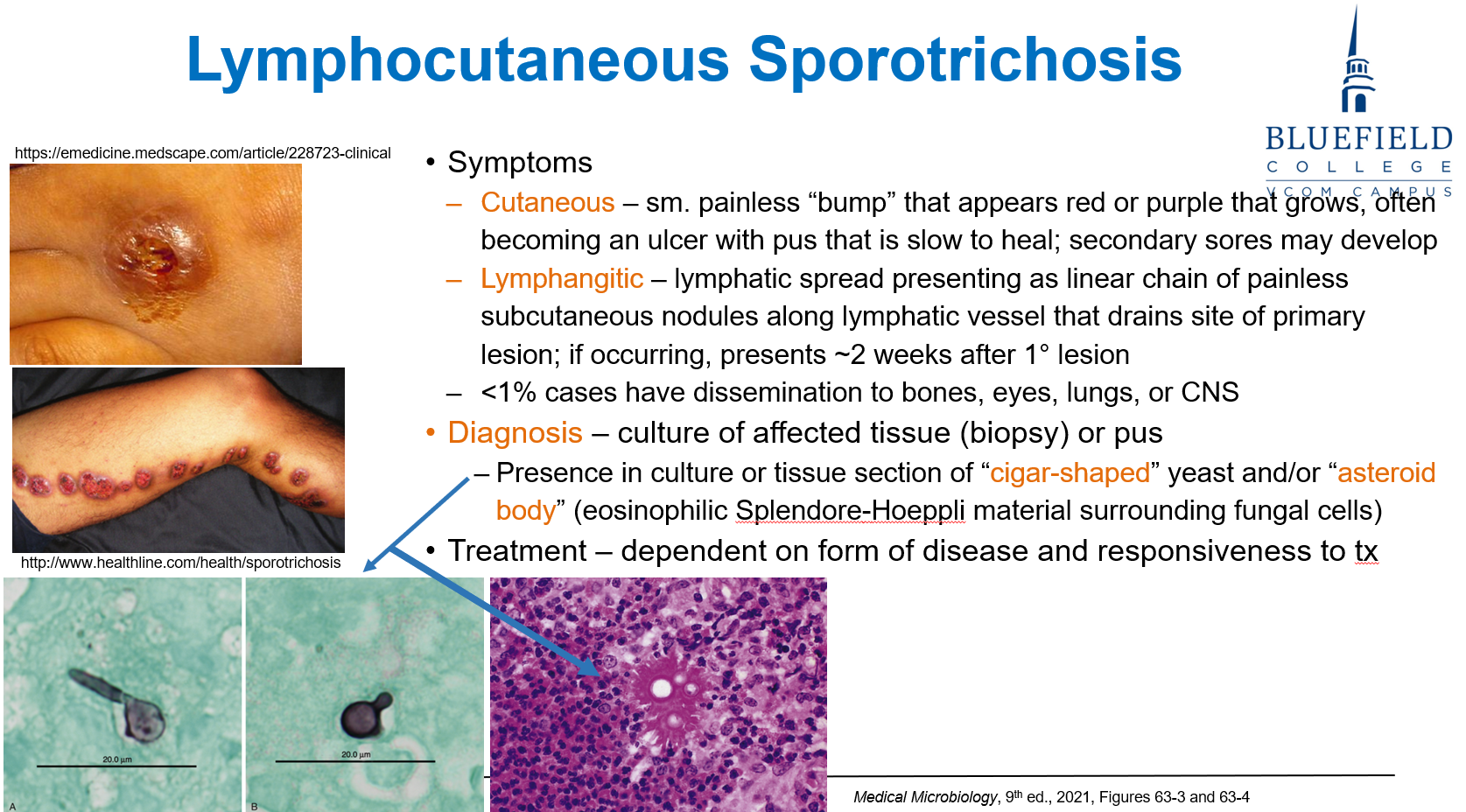
What is a diagnostic feature seen in sporotrichosis tissue samples?
A. Broad-based budding
B. Medlar bodies
C. Spaghetti and meatballs
D. Asteroid bodies
E. Narrow-based budding
D. Asteroid bodies
Sporothrix schenckii forms cigar-shaped yeast surrounded by Splendore-Hoeppli material, forming asteroid bodies.
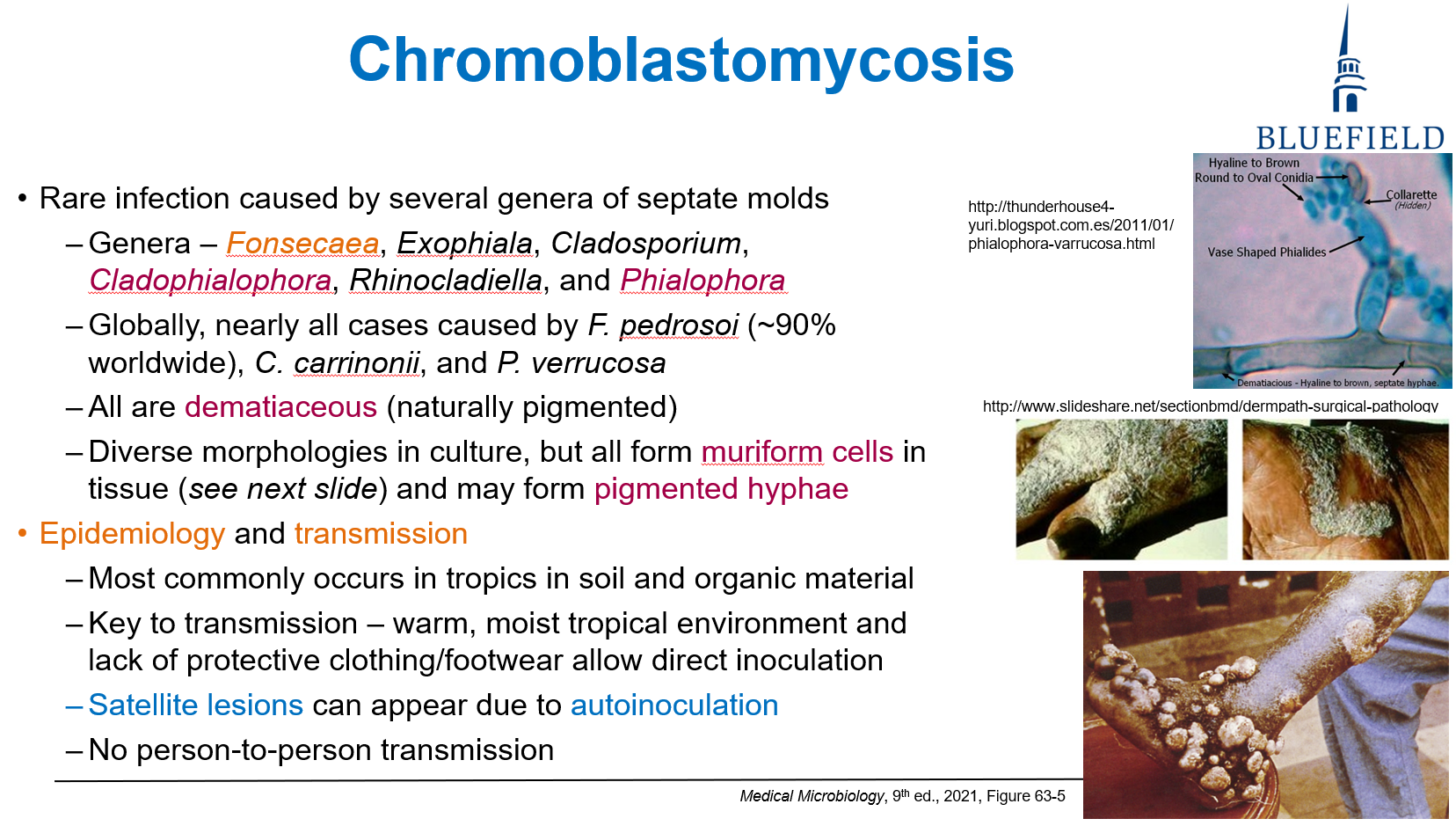
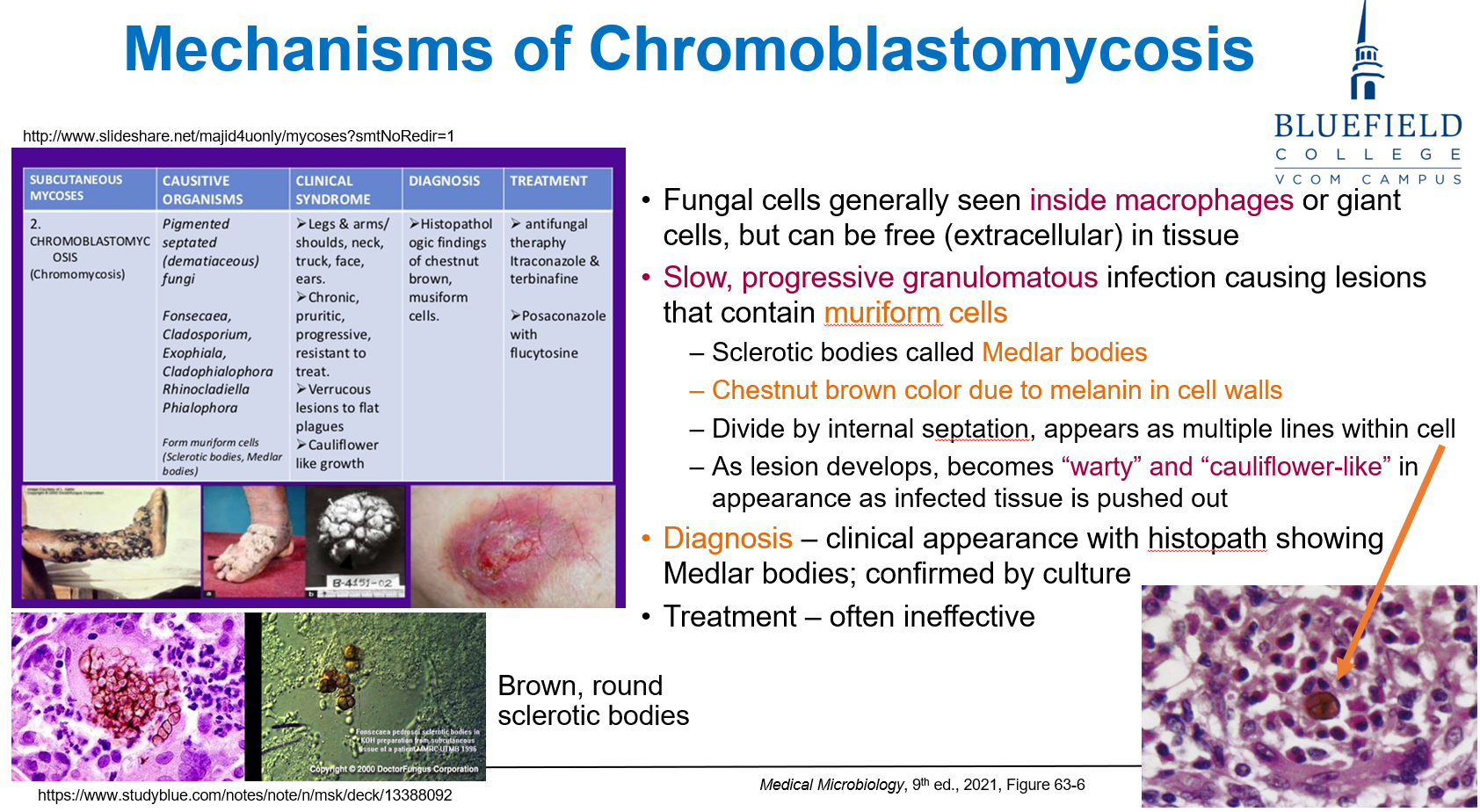
What characteristic fungal cell is found in chromoblastomycosis?
A. Spherule
B. Germ tube
C. Medlar body
D. Cystic body
E. Encapsulated yeast
C. Medlar body
Medlar bodies are pigmented muriform cells seen in chromoblastomycosis.
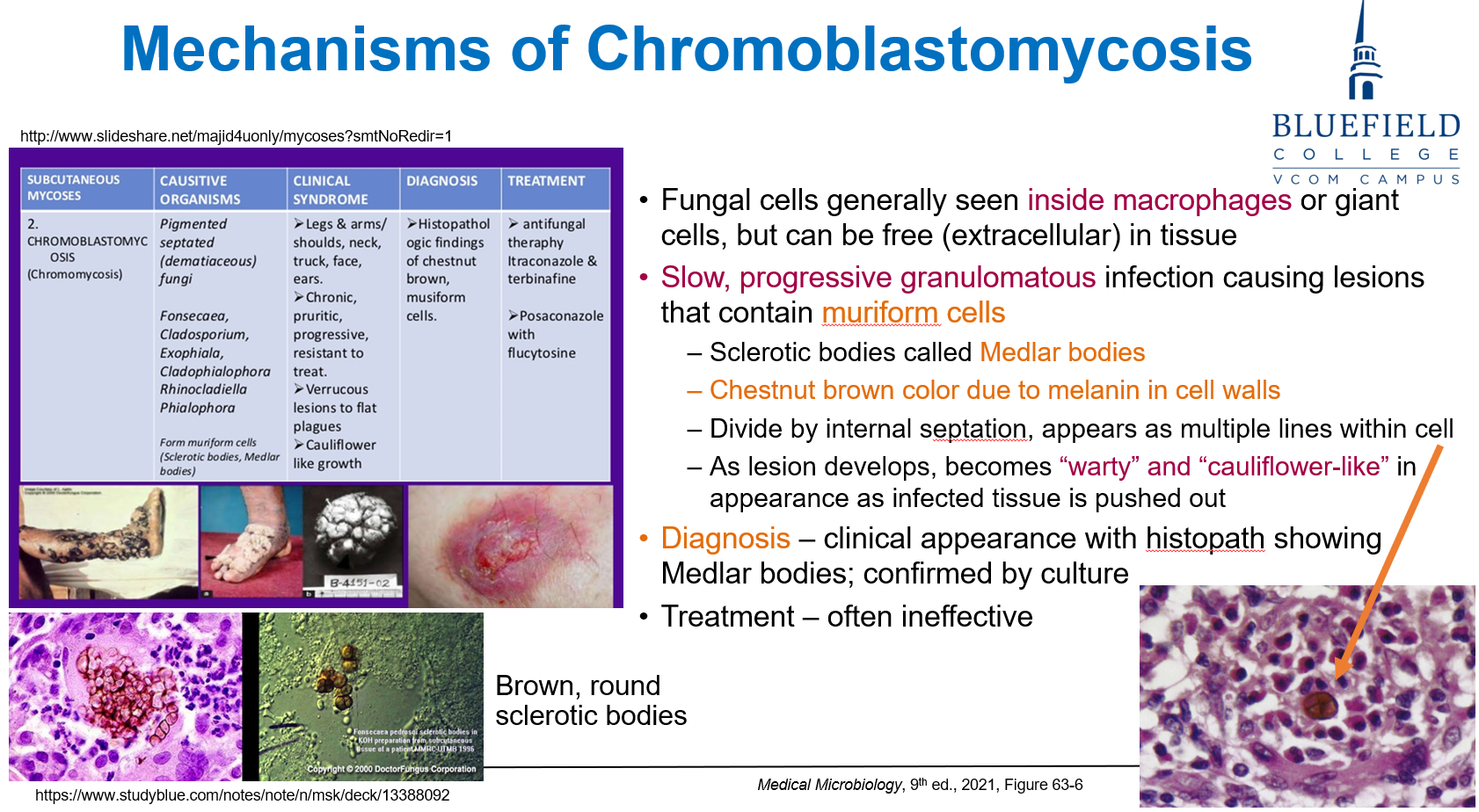
Where are Fonsecaea pedrosoi infections most commonly acquired?
A. Cold, dry climates
B. Urban environments
C. Tropical, humid regions
D. Healthcare settings
E. Industrial factories
C. Tropical, humid regions
Chromoblastomycosis is found in tropical, humid areas and often acquired via skin inoculation.
How do Medlar bodies appear microscopically?
A. Blue-purple round spores with a thick wall
B. Septate hyphae branching at acute angles
C. Brown pigmented fungal cells with internal septation
D. Clear capsule with central budding
E. Granular spores surrounded by eosinophilic halo
C. Brown pigmented fungal cells with internal septation
Medlar bodies are chestnut brown, with brick-wall internal septation.
Which is the best initial test to confirm tinea infection?
A. Fungal PCR
B. Serology
C. KOH microscopy
D. Immunofluorescence
E. Skin culture with silver stain
C. KOH microscopy
KOH prep is used to visualize hyphae from infected skin, hair, or nails.
A patient has thickened, brittle toenails with yellow discoloration. Which organism is most likely?
A. Candida tropicalis
B. Trichophyton rubrum
C. Aspergillus flavus
D. Histoplasma capsulatum
E. Cryptococcus neoformans
B. Trichophyton rubrum
T. rubrum is the most common cause of onychomycosis and tinea unguium.
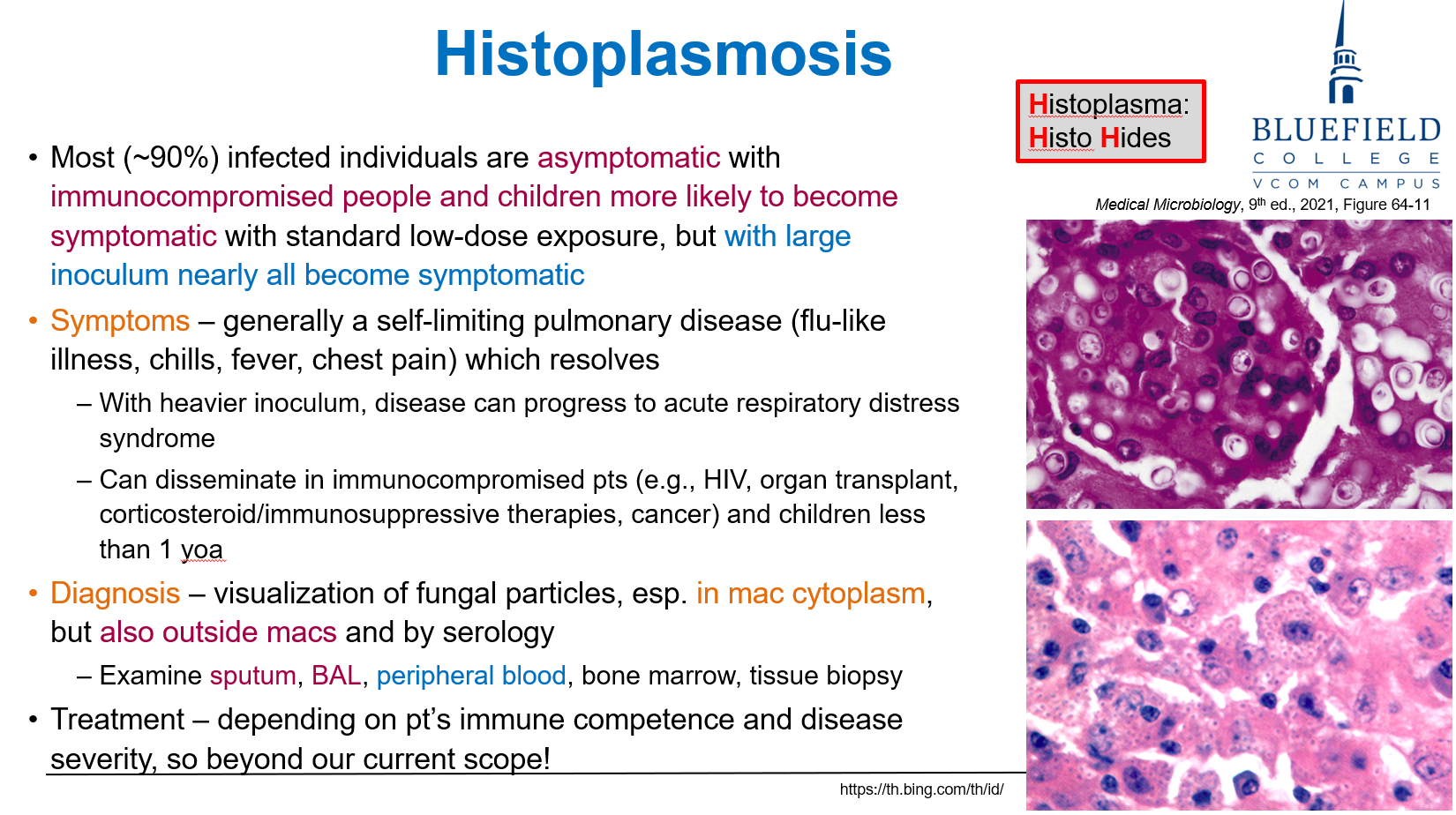
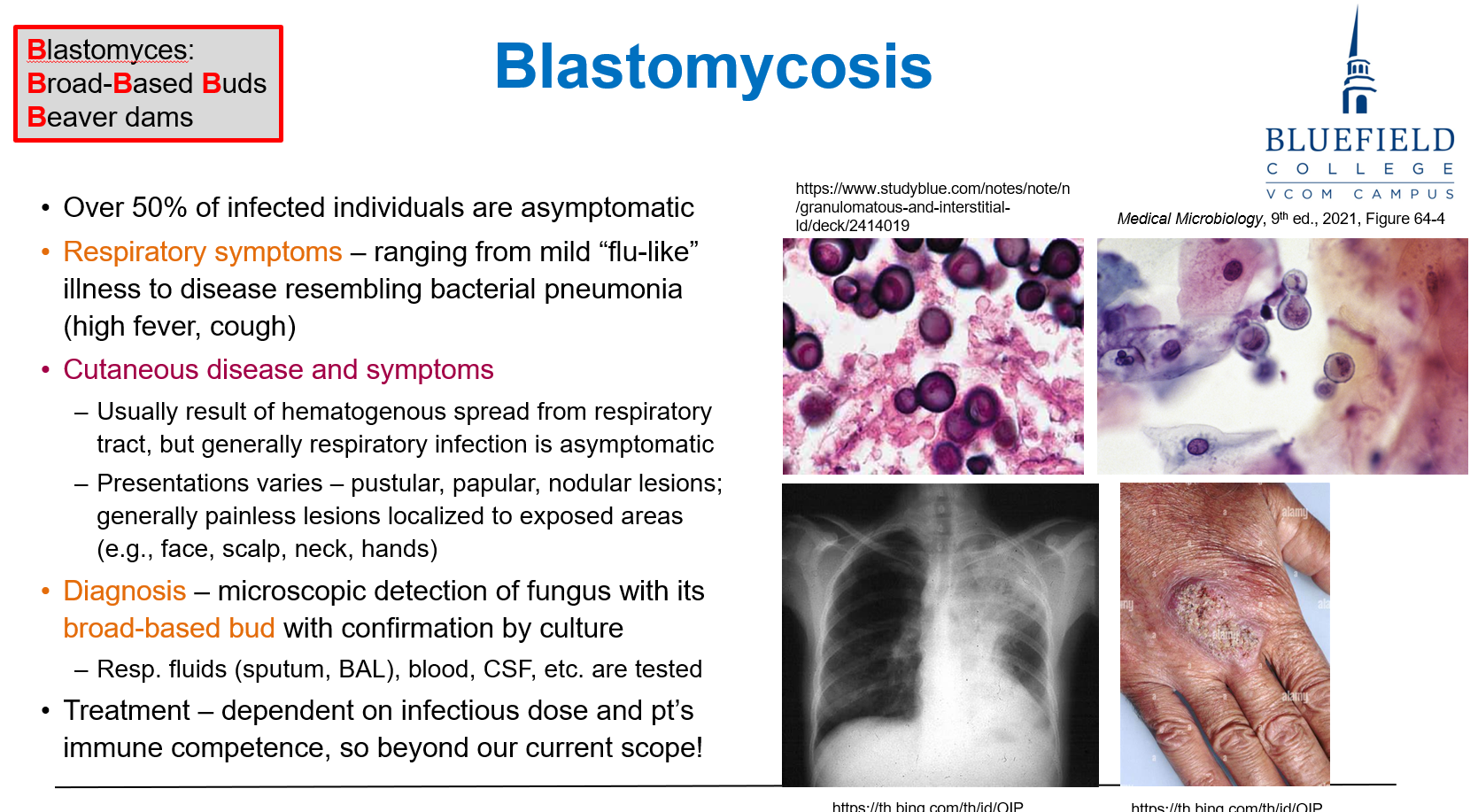
A biopsy of lung tissue in a patient with flu-like symptoms reveals small intracellular yeast within macrophages. What is the most likely pathogen?
A. Aspergillus fumigatus
B. Histoplasma capsulatum
C. Blastomyces dermatitidis
D. Cryptococcus neoformans
E. Pneumocystis jirovecii
B. Histoplasma capsulatum
Histoplasma is a dimorphic fungus that survives intracellularly in pulmonary macrophages.
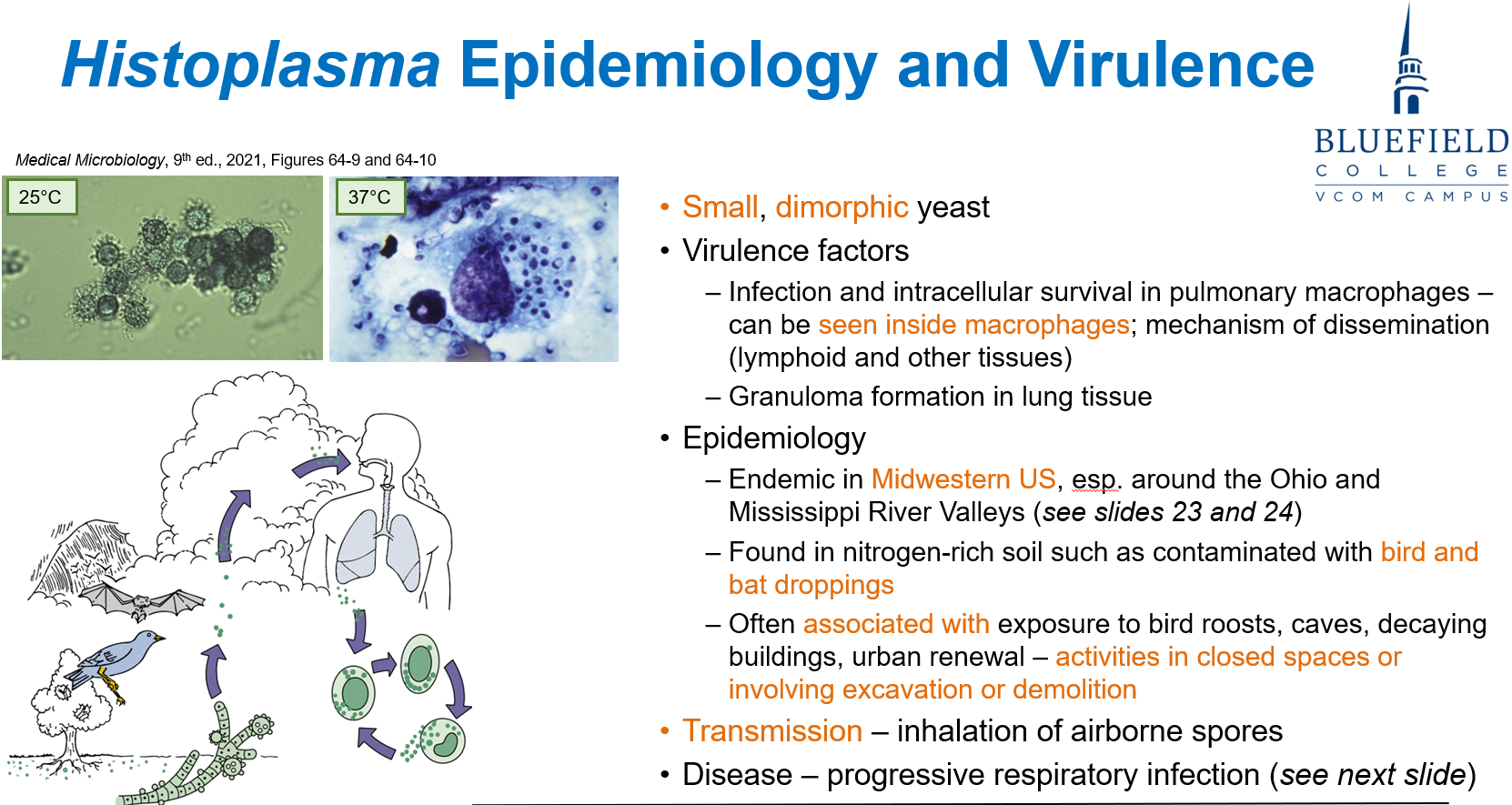
Which of the following regions in the U.S. is Histoplasma most endemic?
A. Pacific Northwest
B. Ohio and Mississippi River Valleys
C. Rocky Mountains
D. Midwestern US
E. Southern California
D. Midwestern US
Histoplasma is endemic to the Midwest, especially near bird/bat droppings in river valleys.
What is the most likely mode of transmission for Histoplasma capsulatum?
A. Direct contact with animal feces
B. Inhalation of airborne spores
C. Skin penetration through thorns
D. Contaminated food ingestion
E. Sexual contact
B. Inhalation of airborne spores
Transmission occurs via inhalation of spores from nitrogen-rich soil.
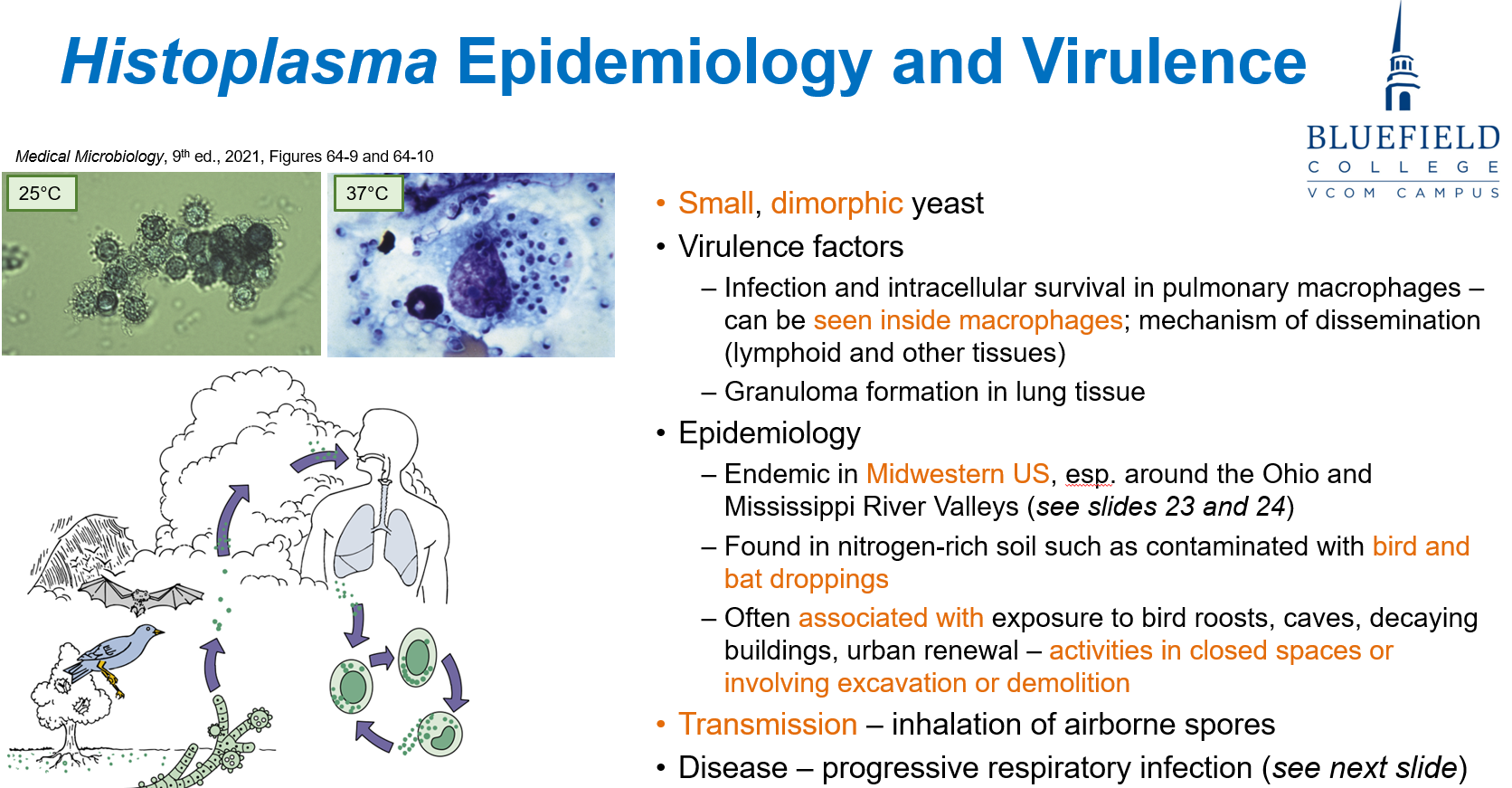
Which of the following individuals is at greatest risk for disseminated histoplasmosis?
A. Healthy adult hiker
B. Diabetic patient with neuropathy
C. Child under 1 year of age
D. Asthmatic using an inhaler
E. Vaccinated adolescent
C. Child under 1 year of age
Children and the immunocompromised are most at risk for disseminated histoplasmosis.
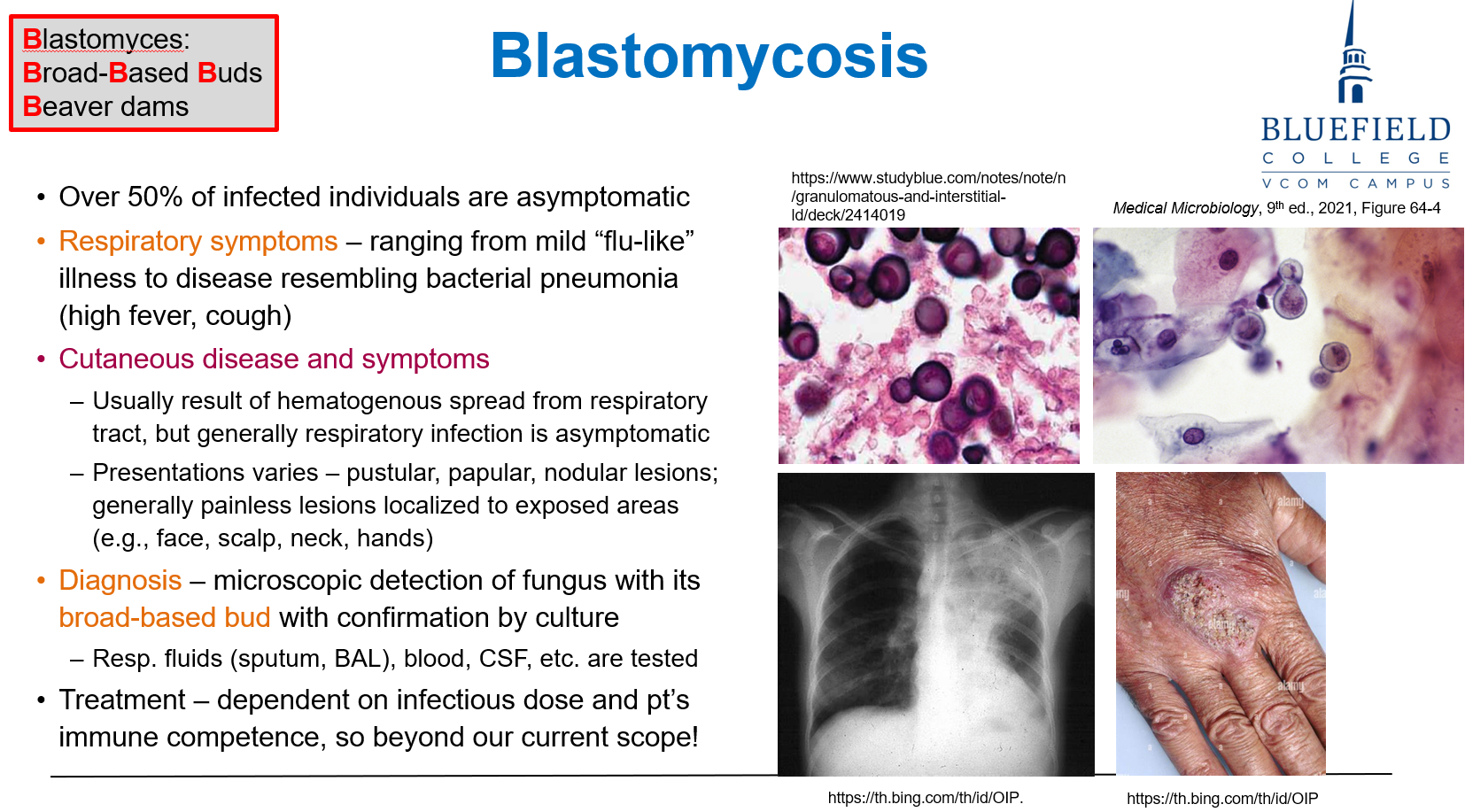
What is the characteristic morphology of Blastomyces dermatitidis at body temperature?
A. Septate hyphae
B. Broad-based budding yeast
C. Narrow-based budding yeast
D. Spherules containing endospores
E. Cup-shaped cysts
B. Broad-based budding yeast
Blastomyces forms broad-based buds in tissue at 37°C.
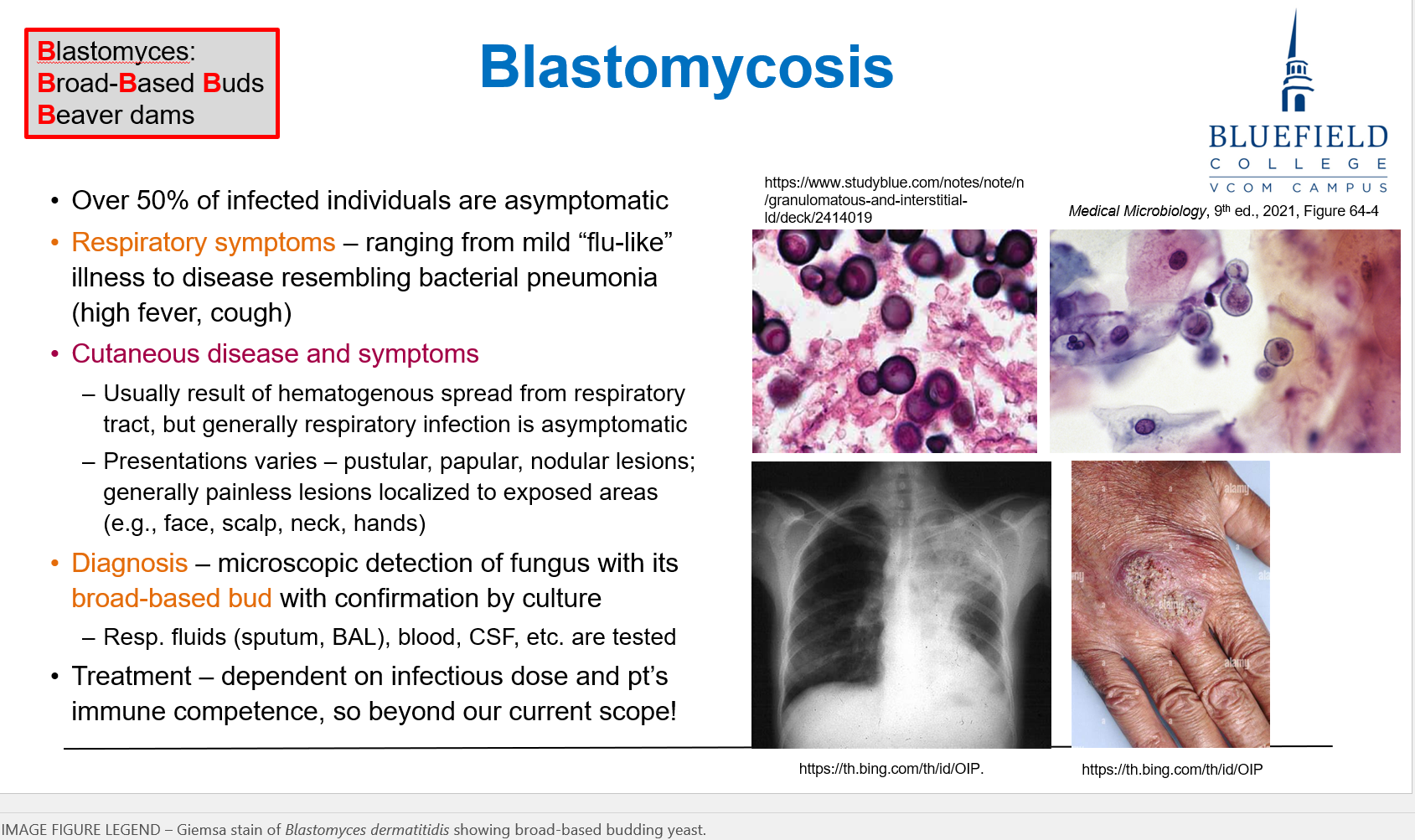
A 50-year-old hunter in the Mississippi Valley presents with cough and skin lesions. What is the most likely source of his infection?
A. Drinking from a freshwater stream
B. Inhalation of spores from moist soil
C. Tick bite
D. Contact with infected person
E. Consumption of raw meat
B. Inhalation of spores from moist soil
Blastomyces is found in decaying wood/soil, and spores are inhaled.
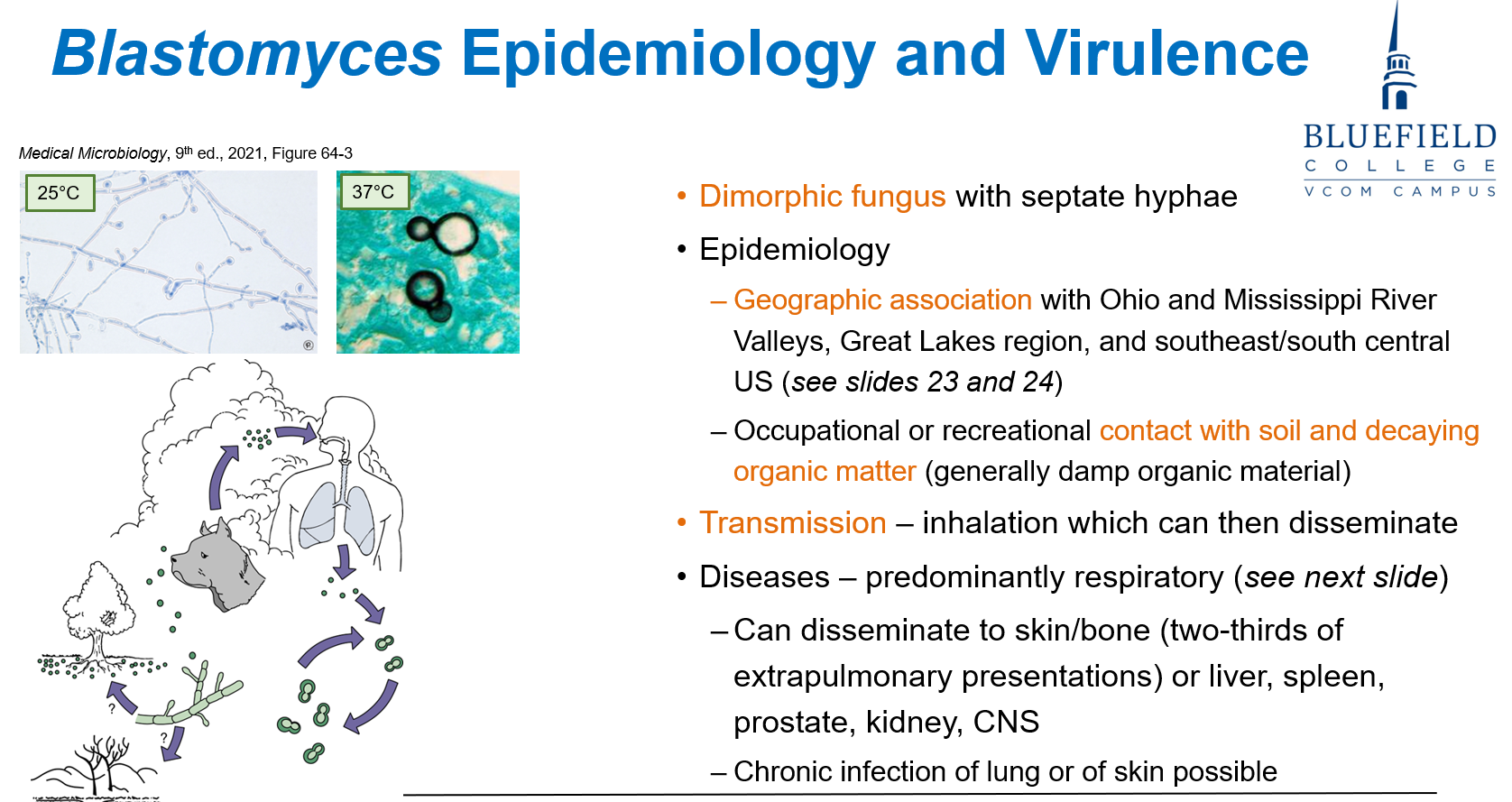
What is the most likely explanation for skin lesions in blastomycosis?
A. Local skin trauma with fungal inoculation
B. Autoimmune vasculitis
C. Hematogenous spread from lungs
D. Mycotoxin-induced damage
E. Direct inoculation through insect bite
C. Hematogenous spread from lungs
Cutaneous blastomycosis occurs via bloodstream dissemination from lung.
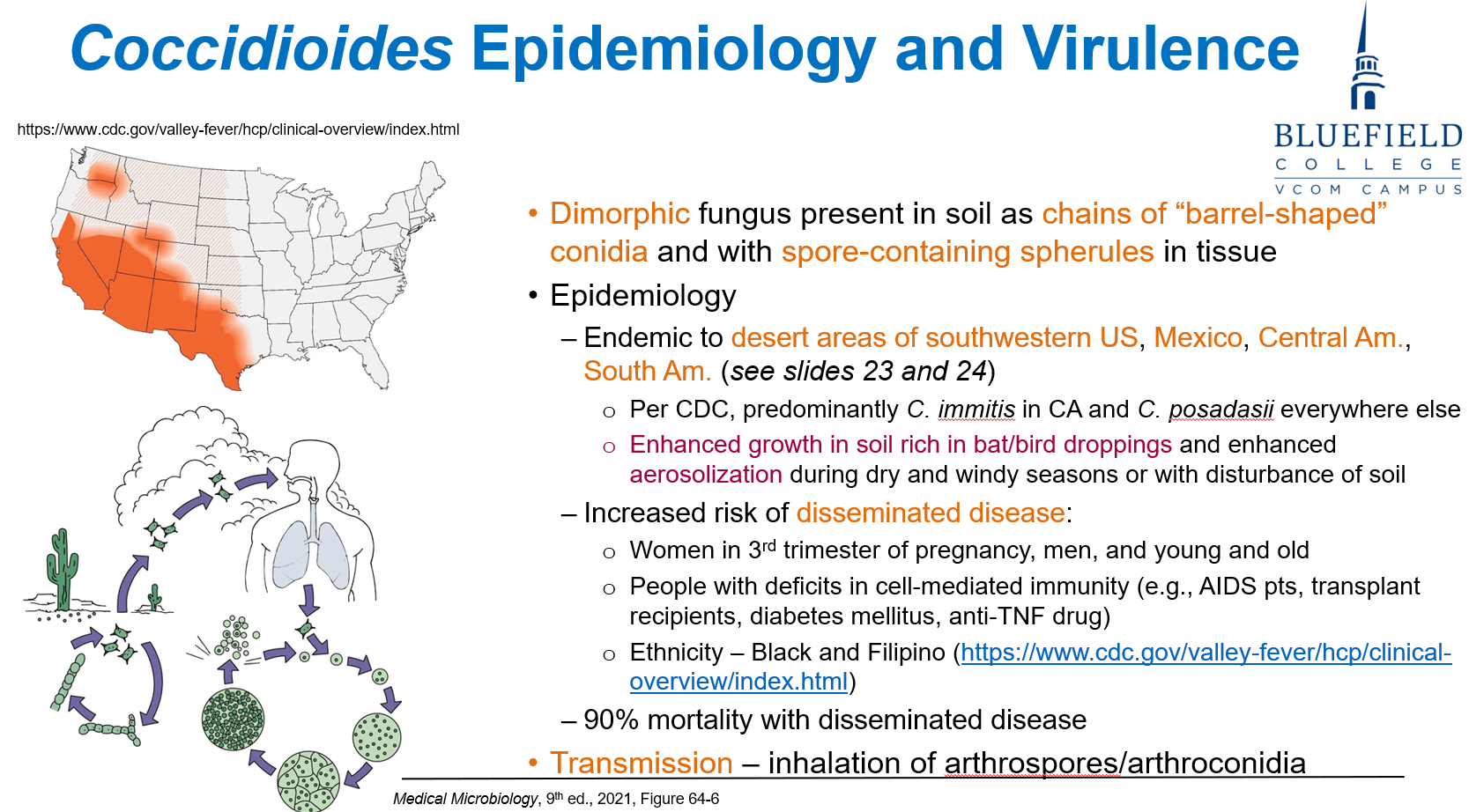
What is the morphological form of Coccidioides in human tissue?
A. Conidiophores
B. Spherules filled with endospores
C. Broad-based budding yeasts
D. Septate hyphae branching at 45°
E. Cigar-shaped yeast
B. Spherules filled with endospores
In tissue, Coccidioides forms spherules containing endospores.
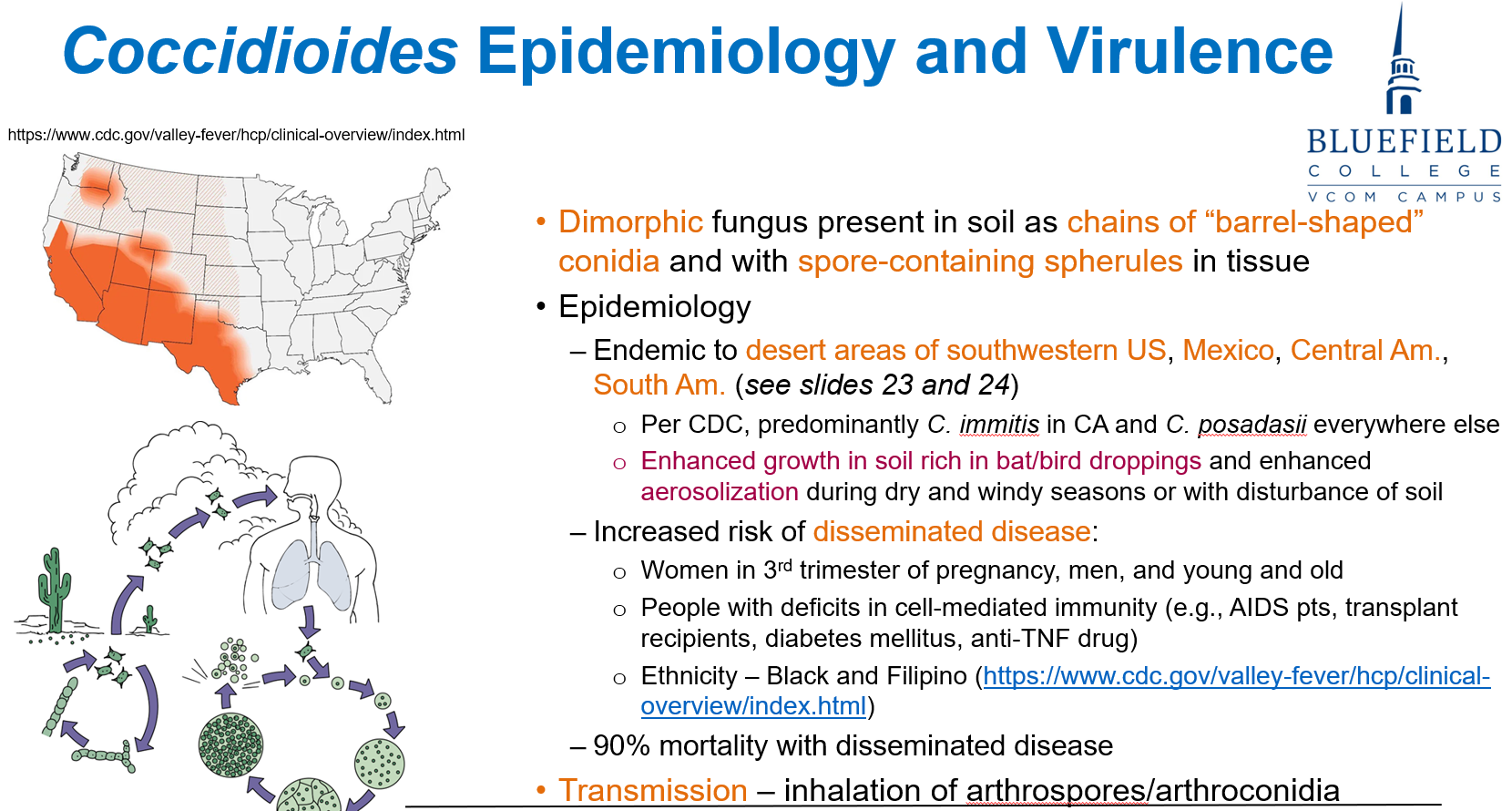
Which group is at highest risk for disseminated Coccidioides infection?
A. Caucasian women in their 20s
B. Male construction workers in Phoenix, AZ
C. Healthy children in Ohio
D. Elderly Canadians
E. Pregnant women in 1st trimester
B. Male construction workers in Phoenix, AZ
Men, immunocompromised, and 3rd-trimester pregnancy are at high risk, especially in SW U.S.
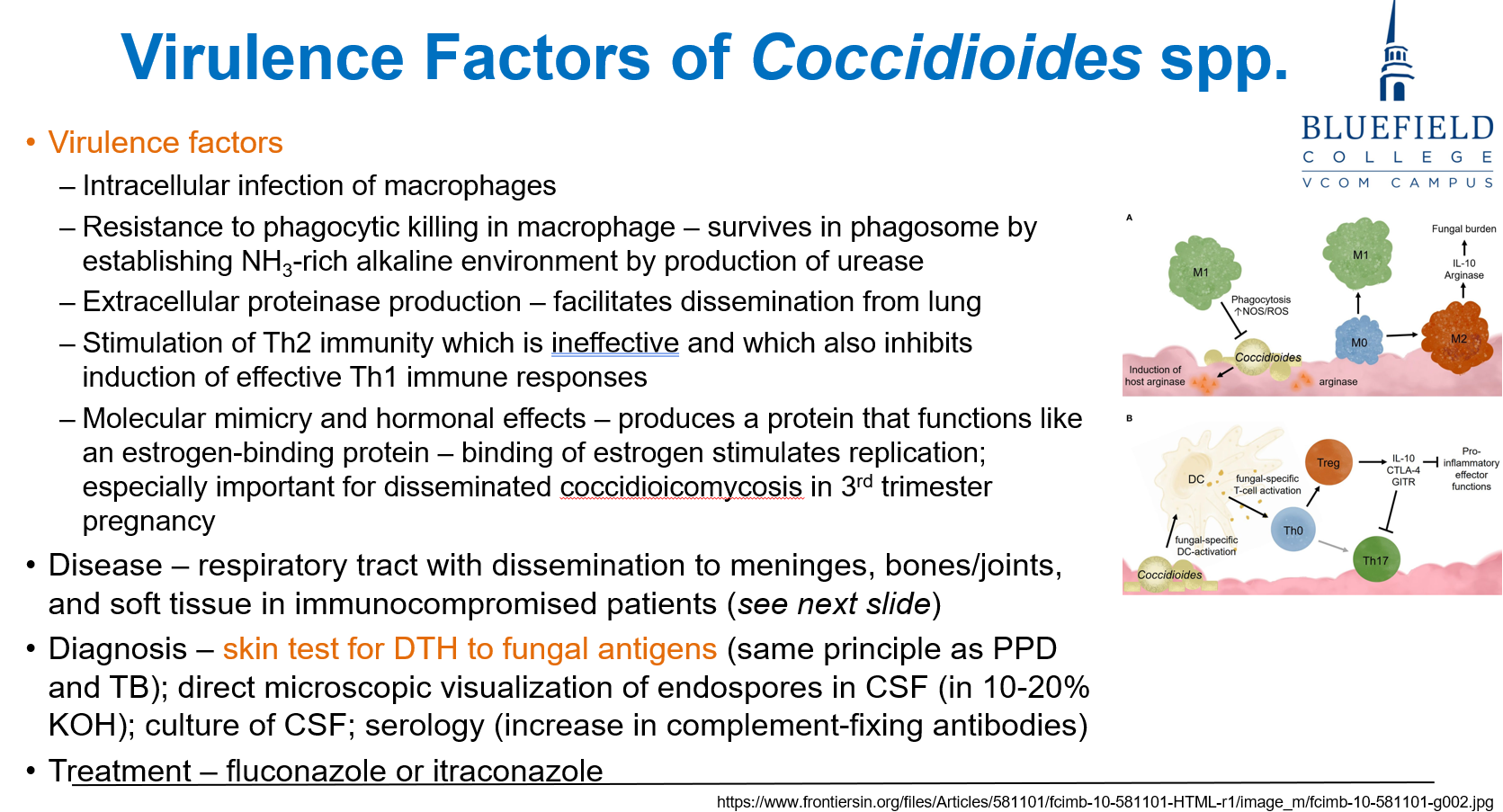
Which of the following contributes to immune evasion by Coccidioides?
A. Production of aflatoxin
B. Antibody suppression by endotoxin
C. Urease production raising phagosome pH
D. Activation of IL-17 signaling
E. Capsule formation
C. Urease production raising phagosome pH
Coccidioides survives in macrophages by using urease to neutralize acidic phagosome.
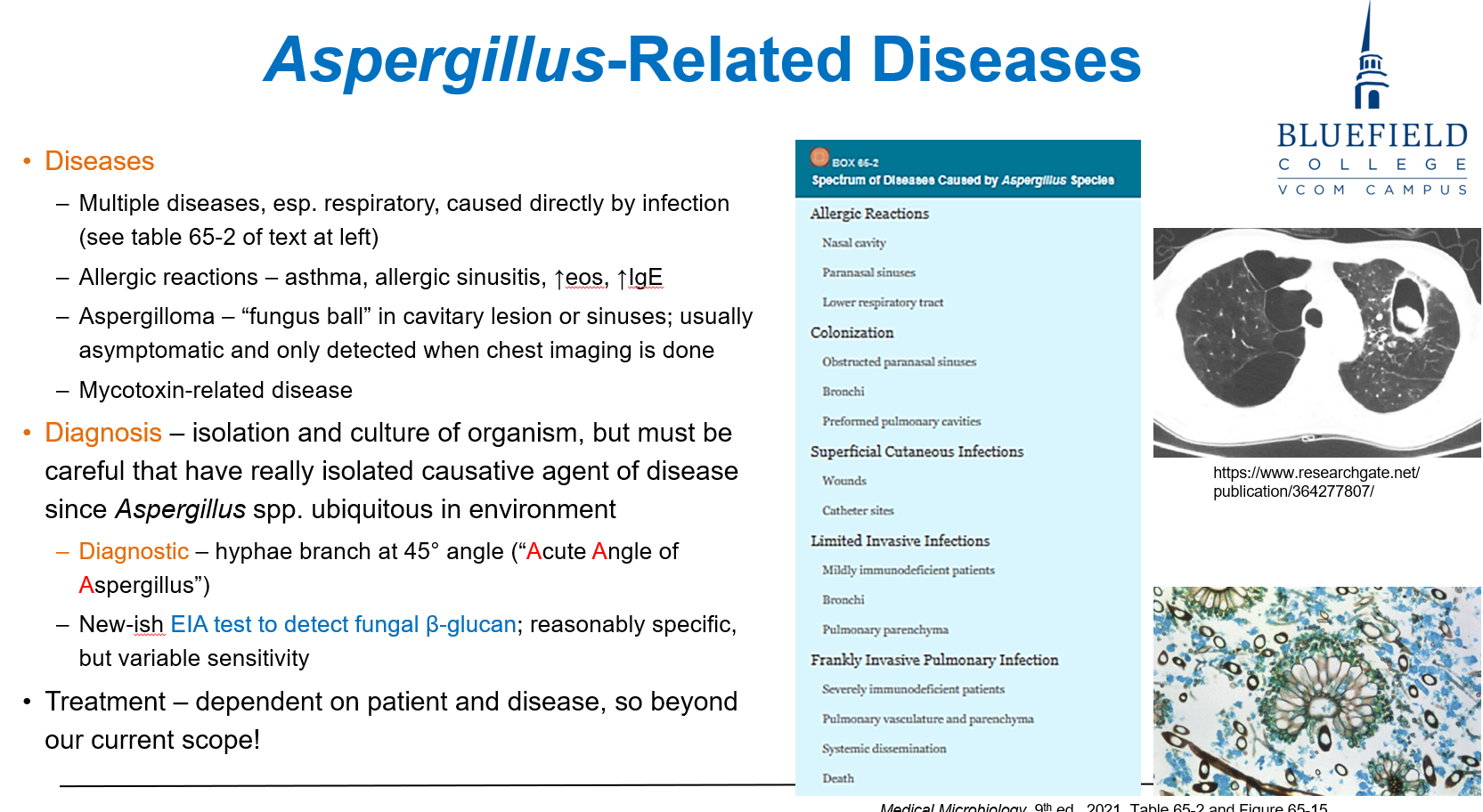
Which of the following describes Aspergillus morphology in tissue?
A. Encapsulated yeast with narrow budding
B. Broad-based budding yeast
C. Septate hyphae branching at 45° angles
D. Barrel-shaped arthroconidia
E. Round, thick-walled muriform cells
C. Septate hyphae branching at 45° angles
Aspergillus has septate hyphae with acute (45°) angle branching.
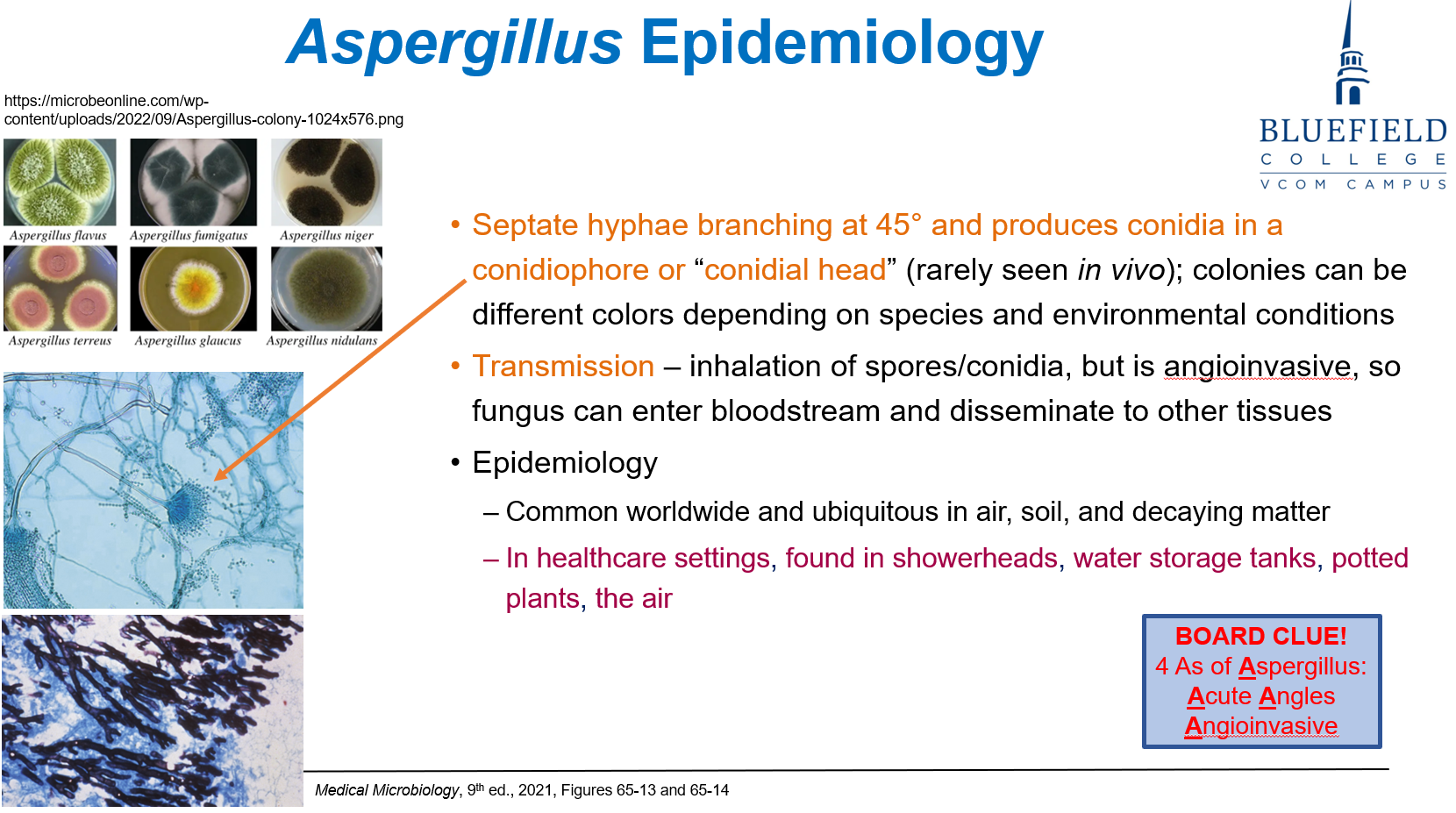
Where is Aspergillus most likely to be found?
A. IV tubing
B. Operating room walls
C. Water tanks and potted plants
D. Refrigerated medications
E. Catheters and drains
C. Water tanks and potted plants
Aspergillus thrives in damp, organic environments like plants, tanks, and humidifiers.
Which of the following conditions is associated with Aspergillus?
A. Cystitis and urethritis
B. Allergic bronchopulmonary aspergillosis
C. Necrotizing fasciitis
D. Oral thrush
E. Erythema multiforme
B. Allergic bronchopulmonary aspergillosis
Aspergillus can cause hypersensitivity reactions including allergic bronchopulmonary disease.
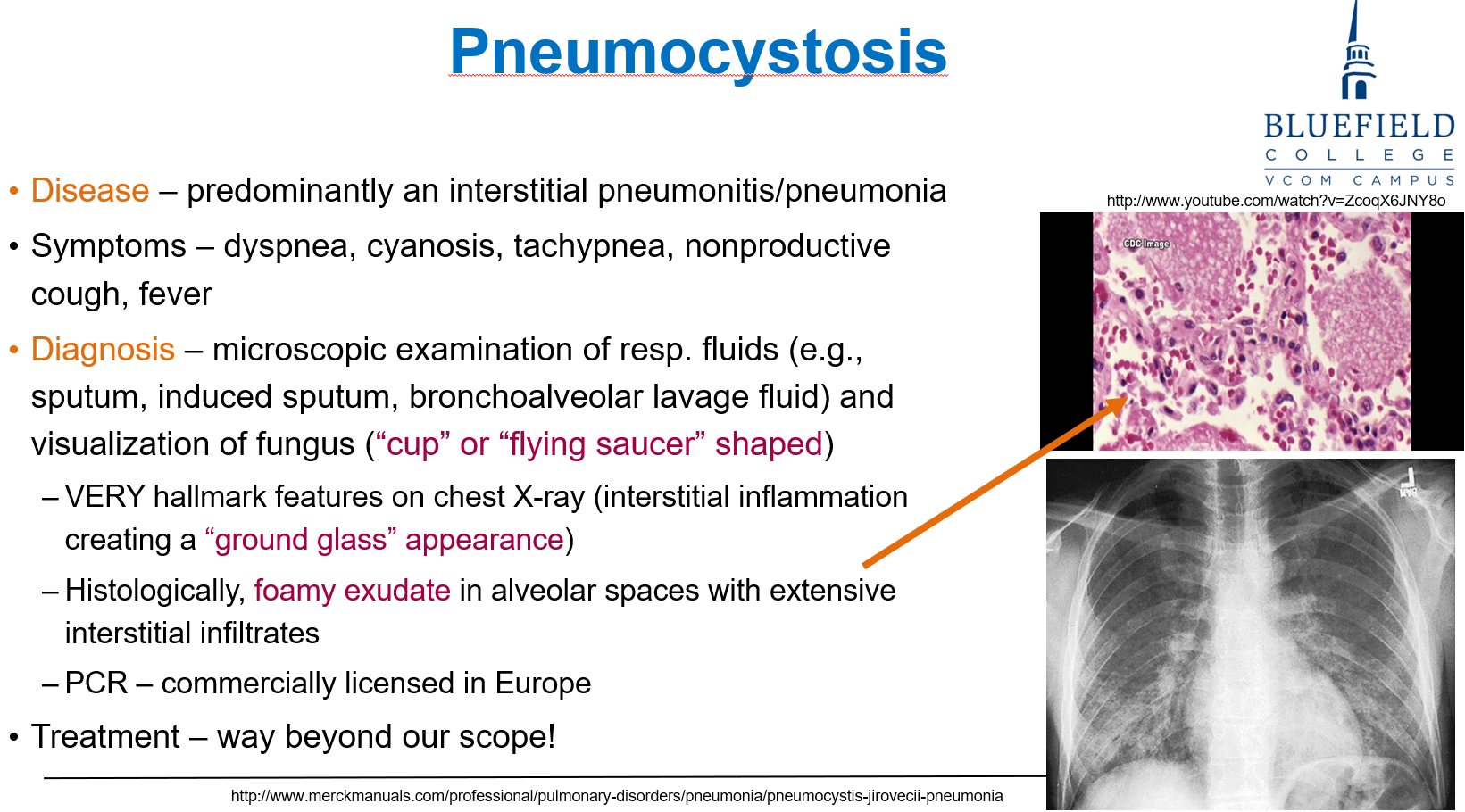
Which of the following is most commonly affected by Pneumocystis jirovecii?
A. Children with asthma
B. Adults with cystic fibrosis
C. Organ transplant recipients
D. HIV patients with CD4 <200
E. Healthy elderly
D. HIV patients with CD4 <200
Pneumocystis is the most common AIDS-defining infection with CD4 < 200 cells/μL.
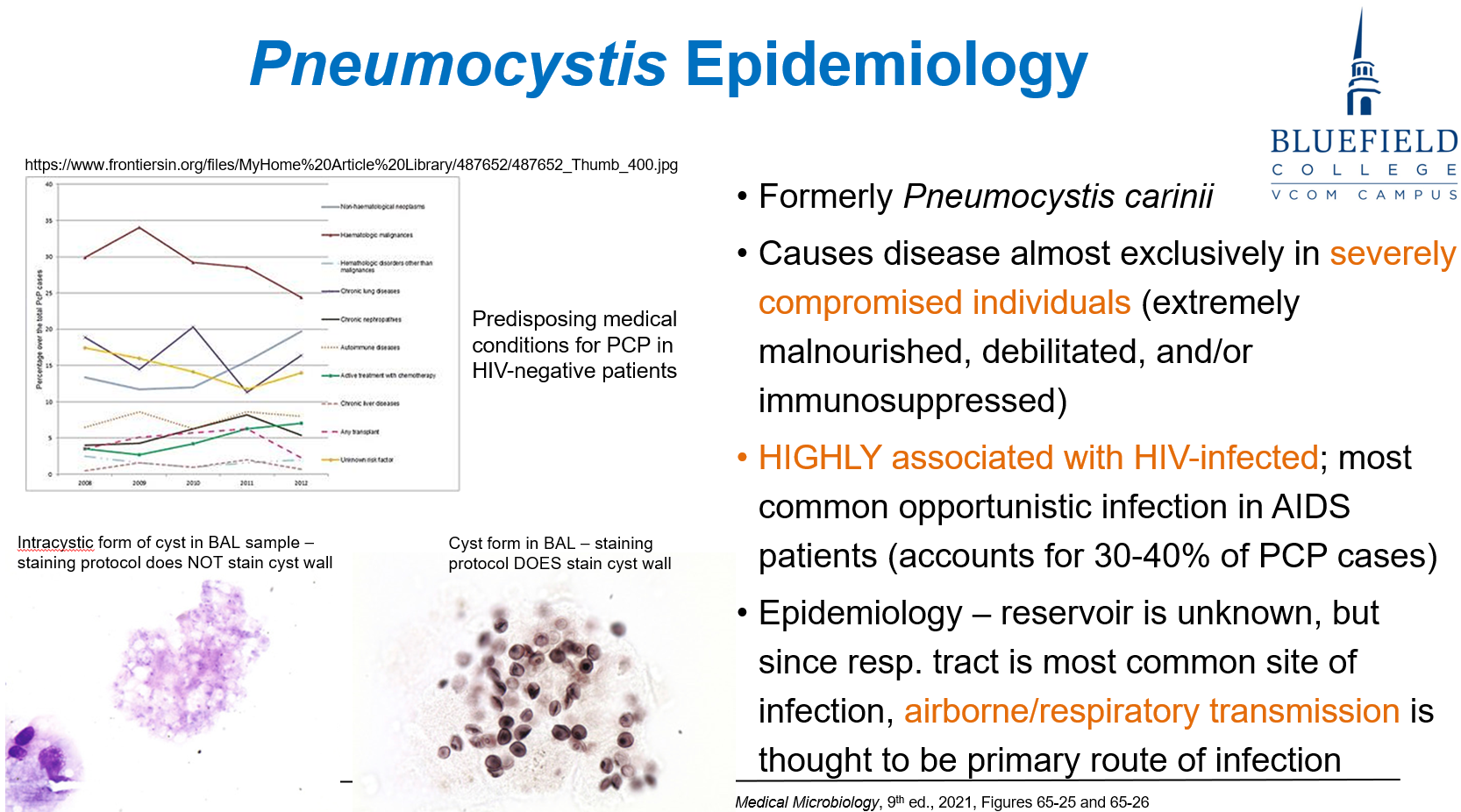
What is a distinguishing microscopic feature of Pneumocystis jirovecii?
A. Cigar-shaped yeast with asteroid body
B. Spherule filled with endospores
C. Cup- or flying saucer-shaped cysts
D. Muriform cells with septations
E. Broad-based budding yeast
C. Cup- or flying saucer-shaped cysts
Pneumocystis appears as cup-shaped organisms on silver stain.
Which test is most specific for diagnosing Coccidioides infection?
A. India ink stain
B. Giemsa stain of urine
C. Histology showing spherules in tissue
D. Eosinophil count
E. Tuberculin skin test
C. Histology showing spherules in tissue
Coccidioides is best diagnosed by visualizing spherules on histopathology.
Which of the following is diagnostic of Blastomyces infection?
A. Narrow-based budding in CSF
B. Encapsulated yeast in India ink
C. Broad-based budding yeast on KOH
D. Spherules filled with endospores
E. Giemsa stain showing muriform cells
C. Broad-based budding yeast on KOH
Blastomyces is identified by broad-based budding yeast.
Which environmental setting most commonly harbors Histoplasma?
A. Freshwater ponds with leeches
B. Sand dunes with mites
C. Soil enriched with bird and bat droppings
D. Refrigerated meat and dairy
E. Decaying wood in pine forests
C. Soil enriched with bird and bat droppings
Histoplasma grows in nitrogen-rich soil, especially with bird or bat droppings.
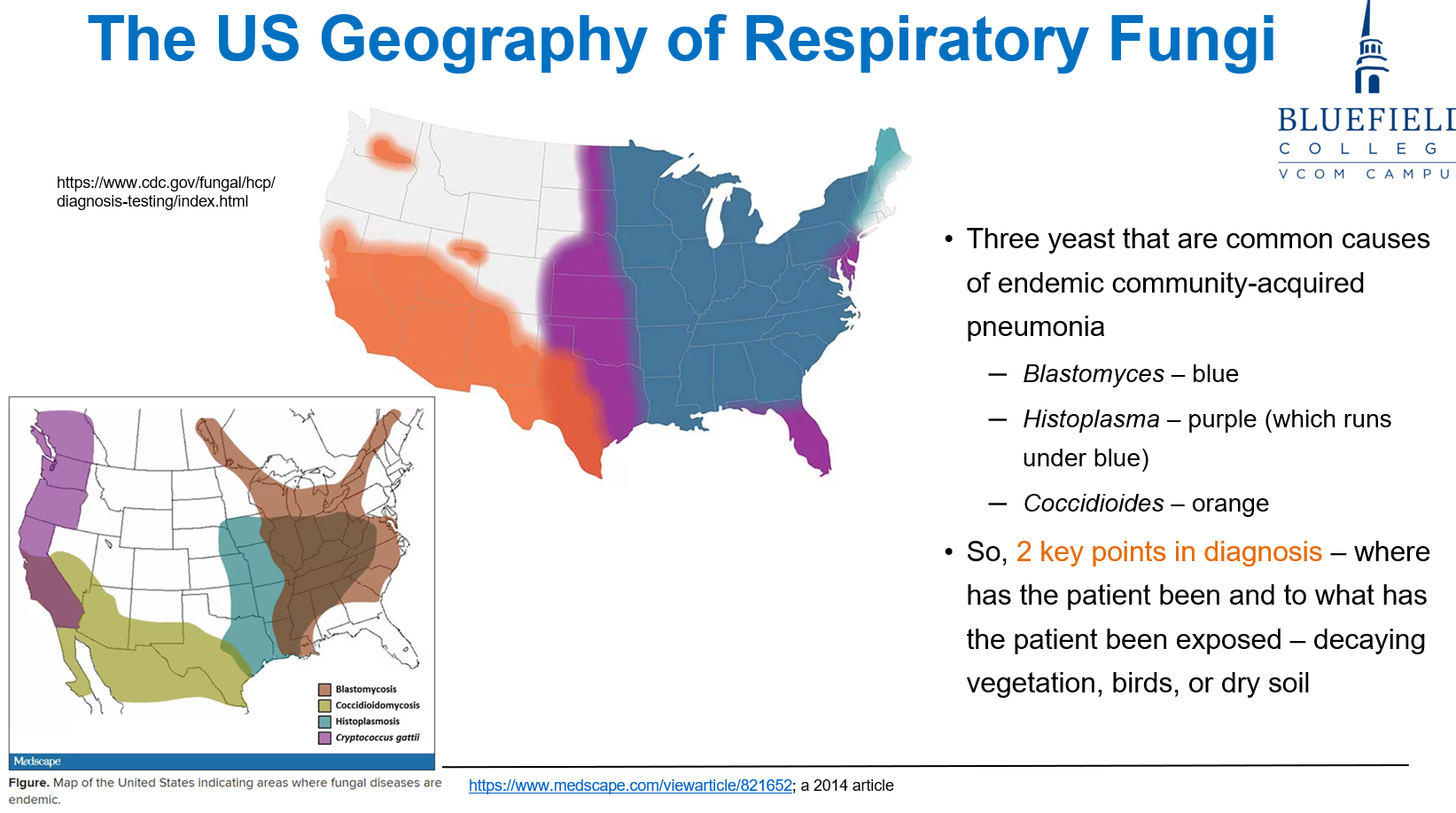
What are the two most important questions when evaluating a potential fungal infection?
A. What medications are they on? & What is their blood type?
B. Do they have pets? & Do they live alone?
C. What’s their immune status? & What did they eat?
D. Where have they been? & What have they been exposed to?
E. Did they travel abroad? & Do they have fever?
D. Where have they been? & What have they been exposed to?
Environmental and geographic exposure history are key in fungal diagnosis.
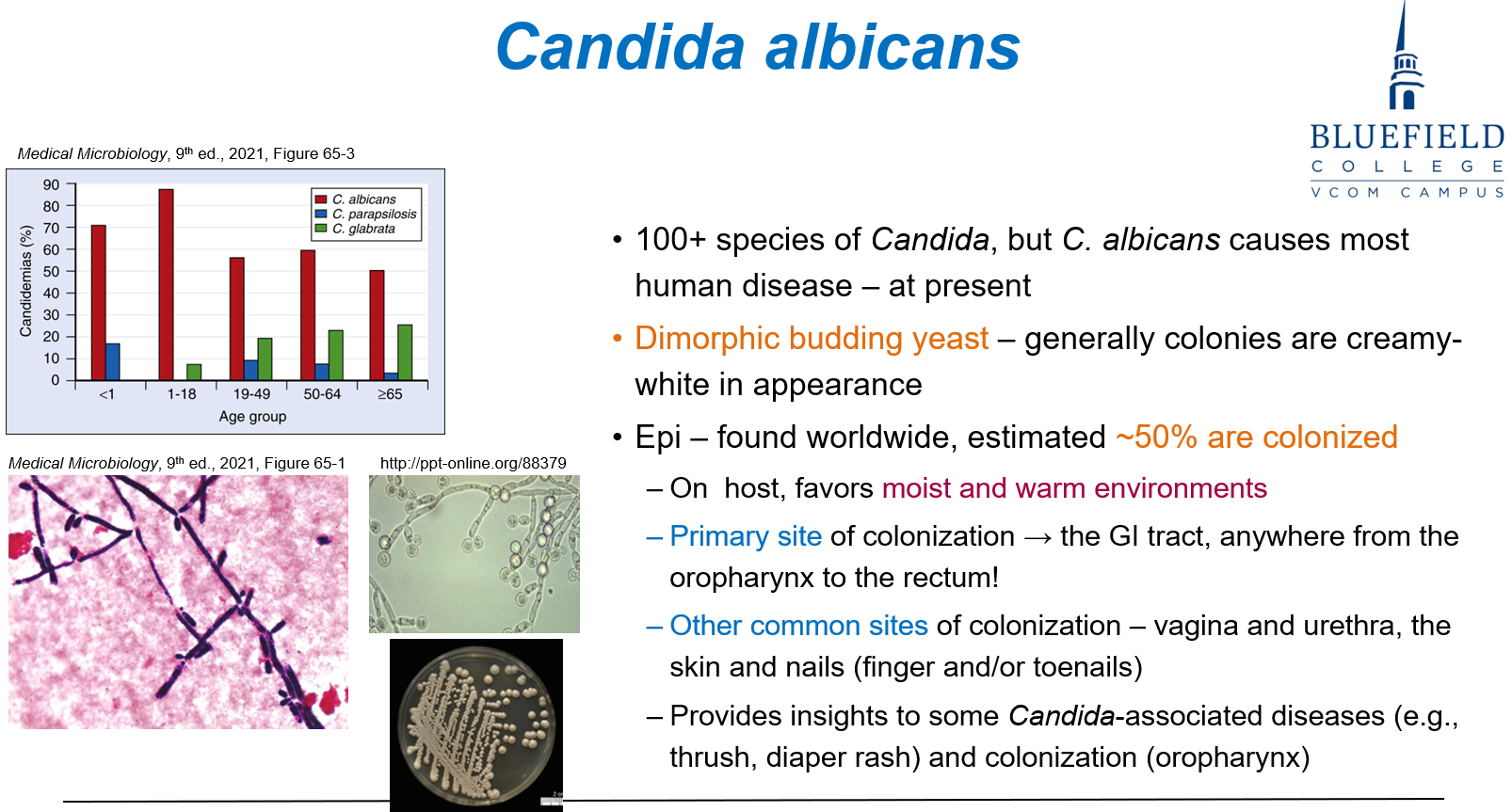
What percentage of people are estimated to be colonized with Candida albicans?
A. 10%
B. 25%
C. 50%
D. 75%
E. 100%
C. 50%
Approximately 50% of individuals are colonized with Candida, often without symptoms.
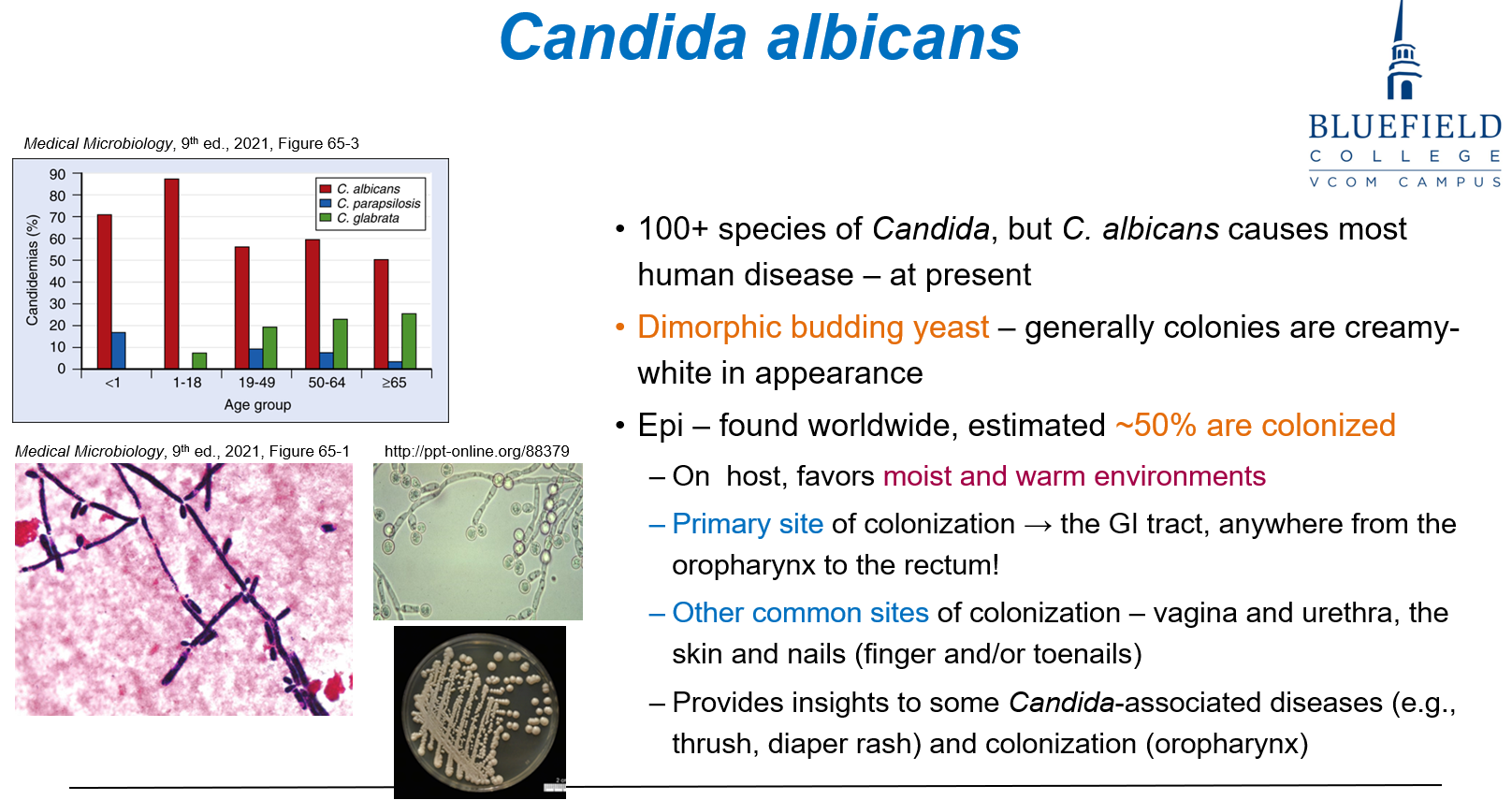
Which of the following best describes Candida albicans?
A. Encapsulated dimorphic yeast with narrow budding
B. Broad-based budding dimorphic fungus
C. Dimorphic budding yeast with creamy-white colonies
D. Spherule-forming mold with creamy-white colonies
E. Non-pigmented septate mold
C. Dimorphic budding yeast with creamy-white colonies
C. albicans is a dimorphic yeast forming creamy-white colonies on culture.
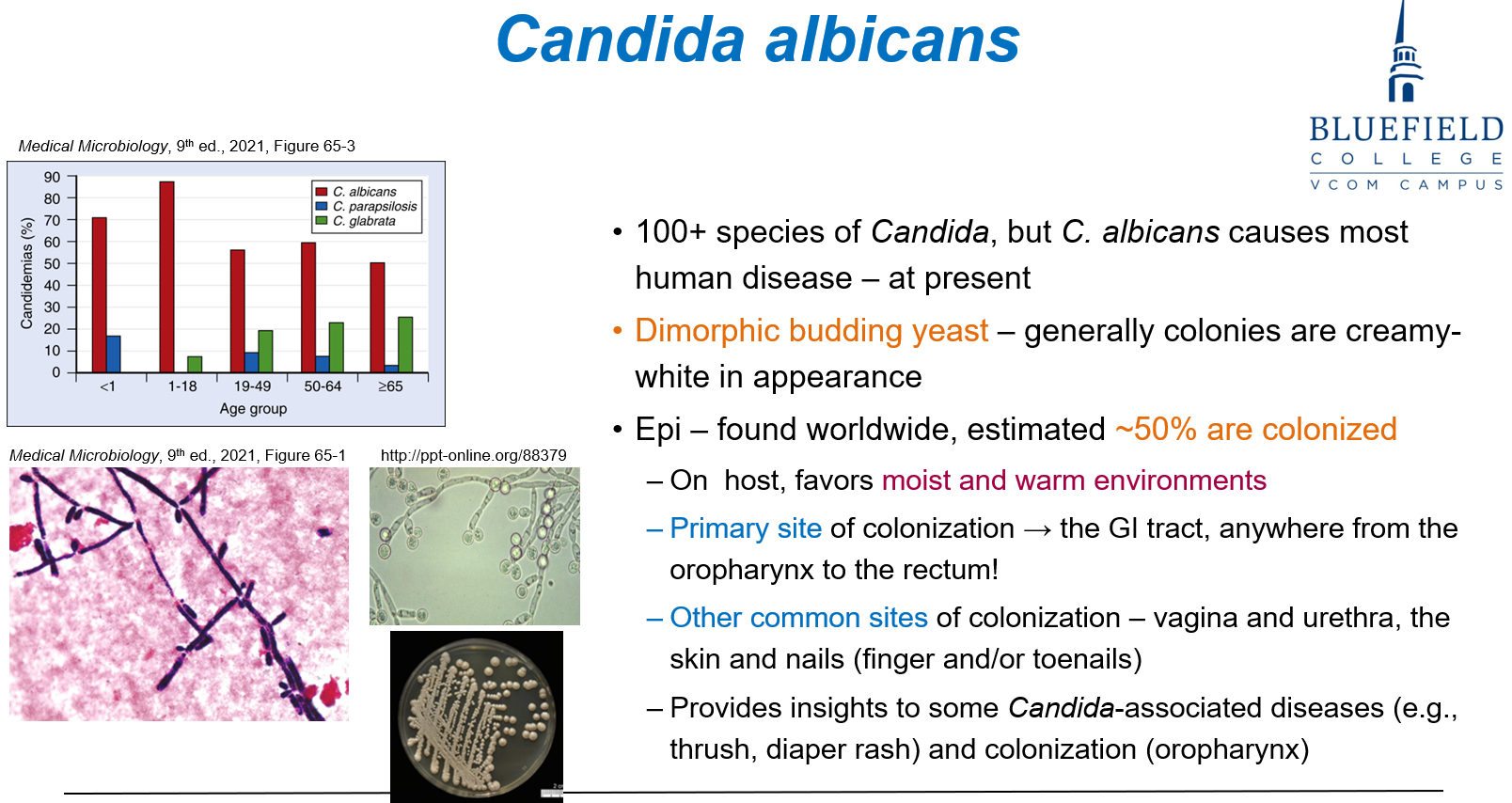
What is the primary site of colonization for Candida albicans?
A. Skin
B. Vagina
C. Urethra
D. GI tract
E. Nasal cavity
D. GI tract
Candida albicans predominantly colonizes the GI tract, including the oropharynx to rectum.
Which of the following is not typically caused by Candida?
A. Vulvovaginitis
B. Oral thrush
C. Pneumonia
D. Erythema nodosum
E. Intertrigo
D. Erythema nodosum
Candida causes mucocutaneous infections like thrush and intertrigo, not immune-mediated rashes like erythema nodosum.
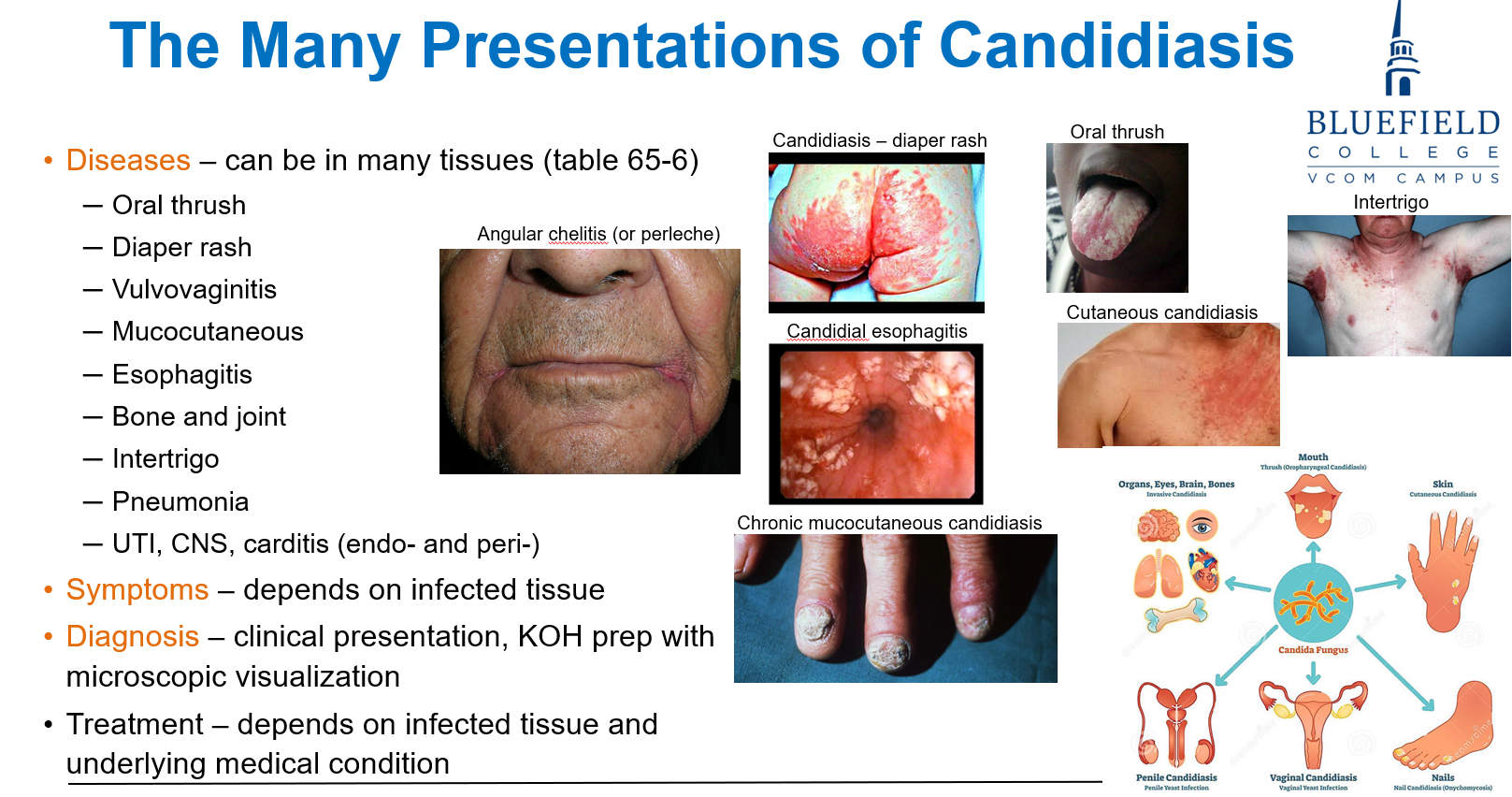
What is the most appropriate initial diagnostic tool for Candida infections?
A. Silver stain
B. KOH prep of scrapings
C. India ink of CSF
D. CT scan
E. Blood PCR
B. KOH prep of scrapings
KOH microscopy helps visualize yeast and pseudohyphae in skin, mucosa, or nails.
Which of the following best describes endogenous Candida infection?
A. Inhalation of environmental spores
B. Auto-inoculation from colonized GI tract
C. Bloodborne infection from mosquitoes
D. Transplacental transfer
E. Pet exposure
B. Auto-inoculation from colonized GI tract
Endogenous infections originate from normal flora, especially from the GI tract.
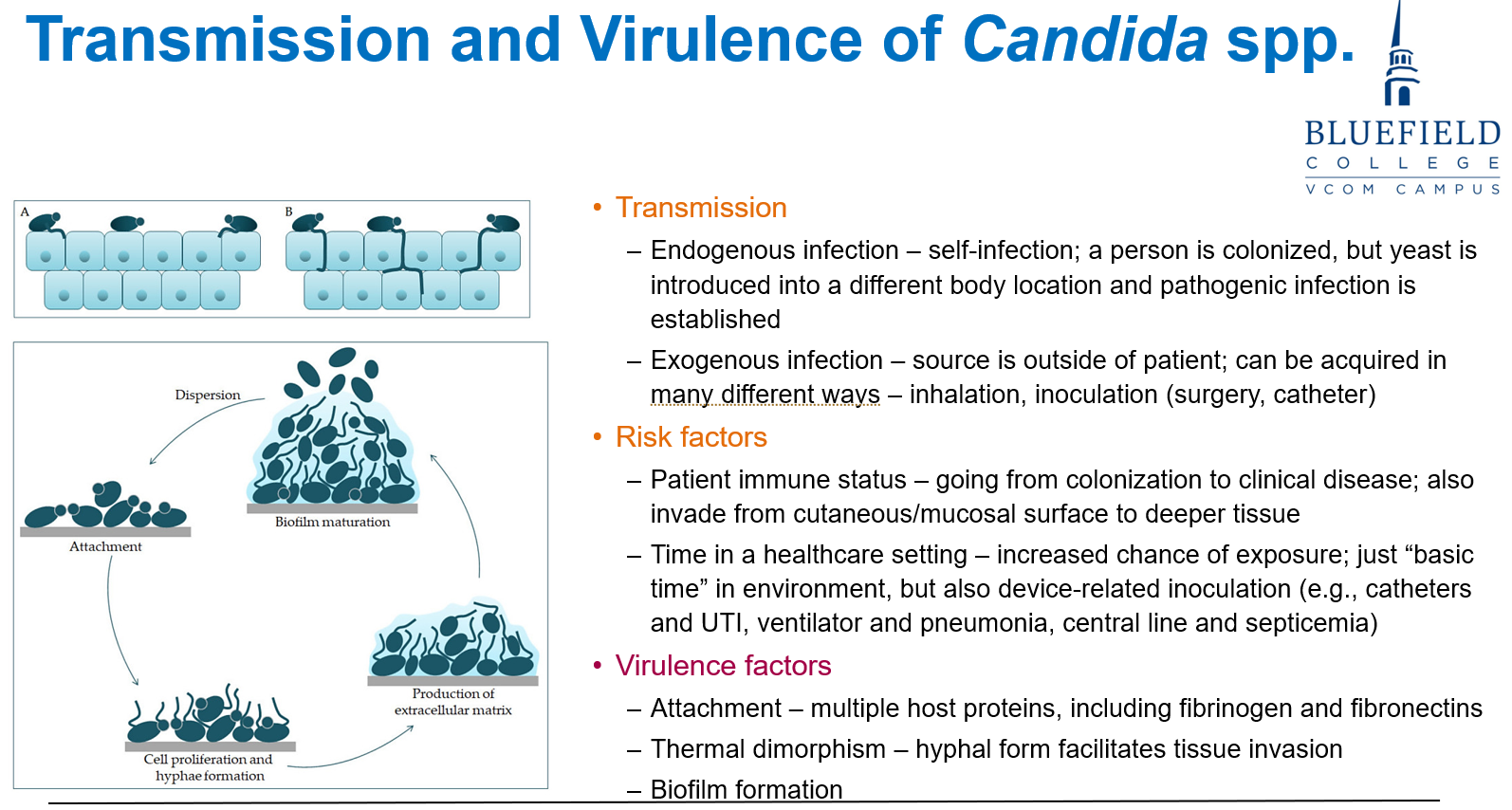
Which of the following is a key virulence factor for Candida albicans?
A. Mycotoxin secretion
B. Capsule formation
C. Yeast-to-hyphae dimorphism
D. Resistance to β-lactam antibiotics
E. Melanin pigment production
C. Yeast-to-hyphae dimorphism
Candida's ability to switch to hyphal forms facilitates tissue invasion. Candida can change from a round shape to long, thread-like forms called hyphae. This helps it push into and spread through tissues, making infections worse.
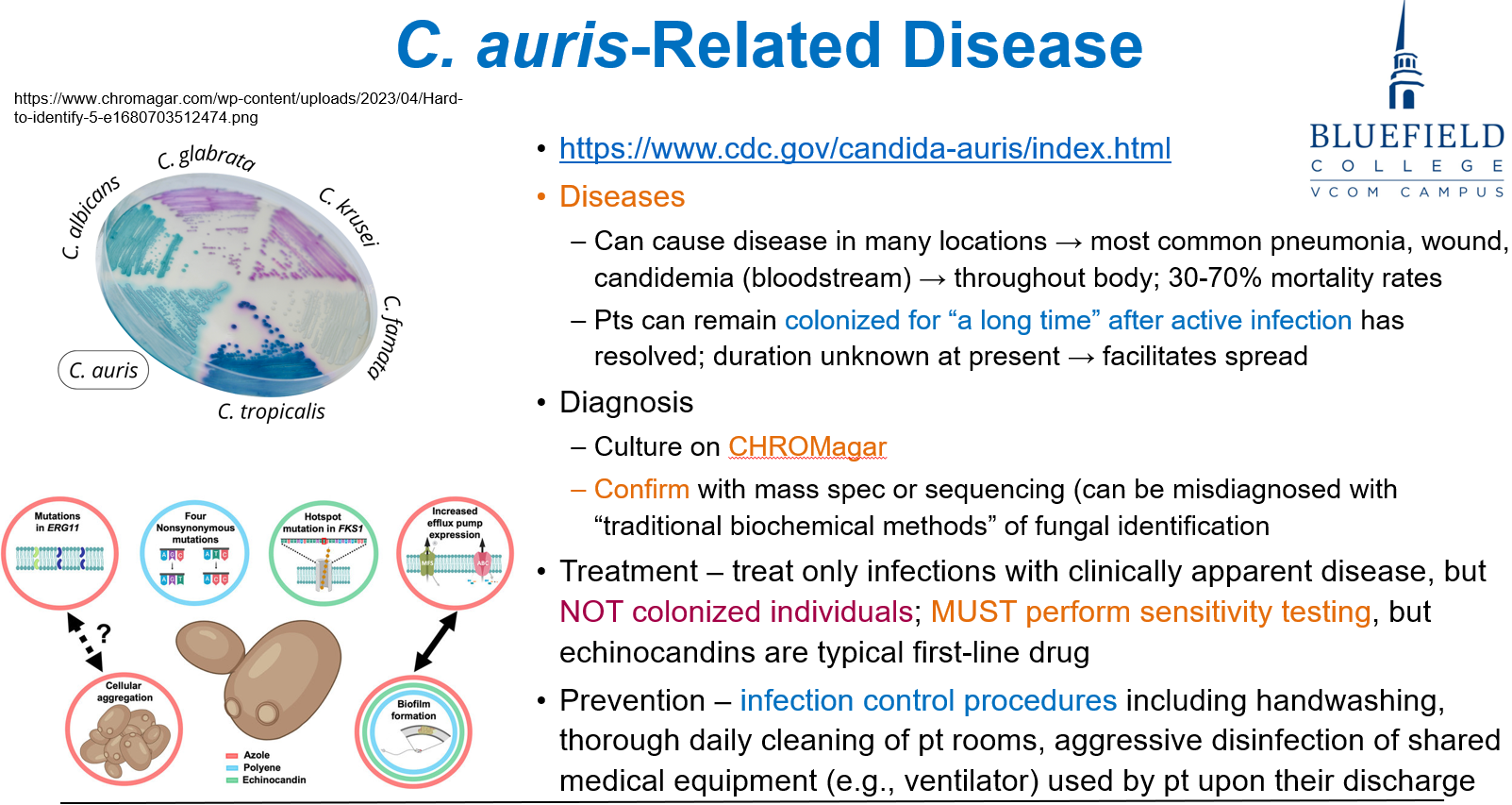
Which factor makes Candida auris particularly dangerous in healthcare settings?
A. Poor growth in lab culture
B. Rapid development of germ tubes
C. Frequent misidentification as bacterial infection
D. High environmental stability and drug resistance
E. Endemic transmission via food
D. High environmental stability and drug resistance
C. auris is drug-resistant, highly transmissible, and persists on surfaces.
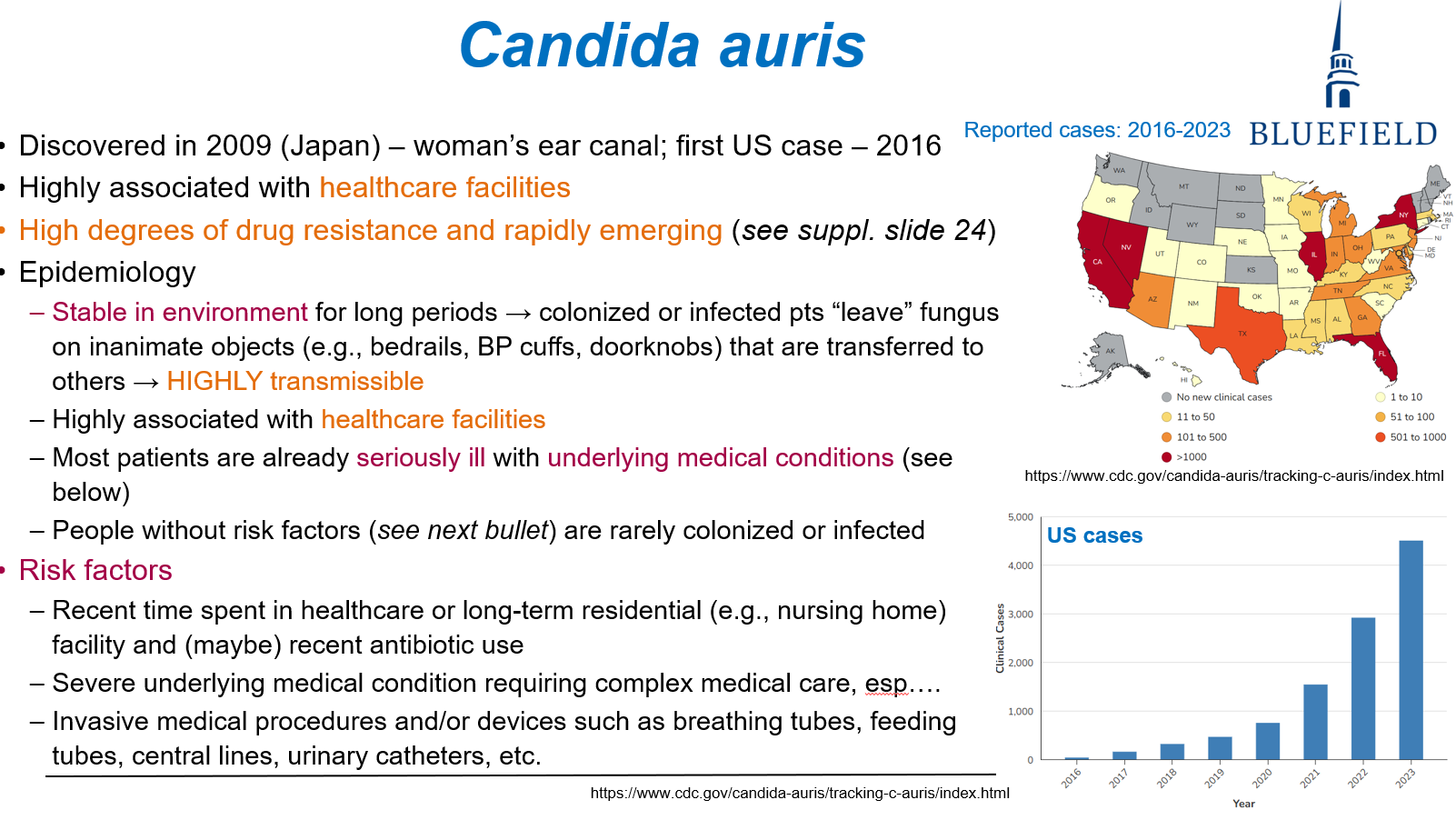
What is the first-line antifungal treatment for symptomatic Candida auris infections?
A. Fluconazole
B. Itraconazole
C. Amphotericin B
D. Echinocandins
E. Voriconazole
D. Echinocandins
Echinocandins are preferred due to their efficacy and resistance patterns of C. auris.
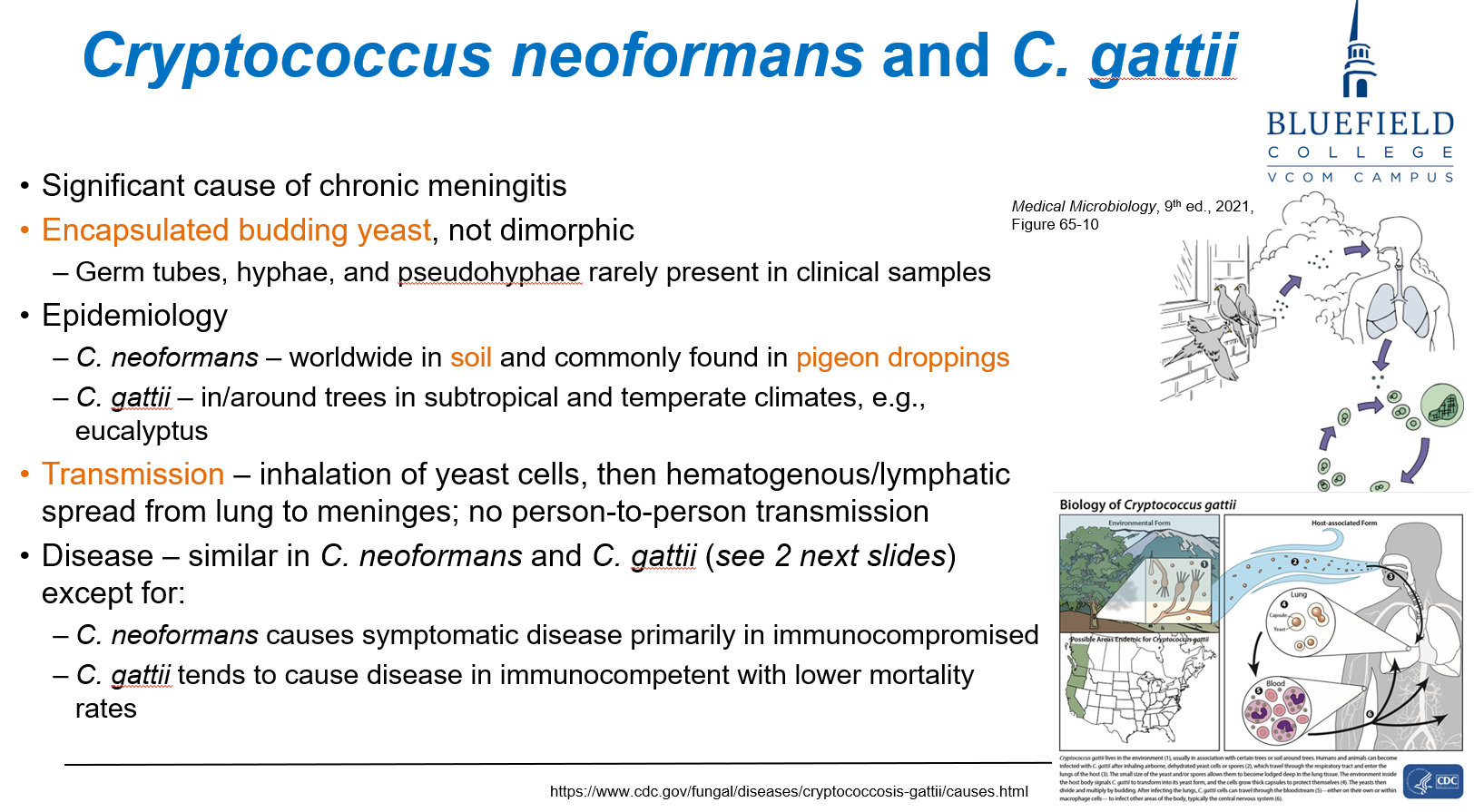
What is the key microscopic feature used to identify Cryptococcus species?
A. Germ tubes
B. Branching hyphae
C. Encapsulated budding yeast
D. Barrel-shaped conidia
E. Broad-based budding
C. Encapsulated budding yeast
Cryptococcus is recognized by its thick polysaccharide capsule, visible with India ink.
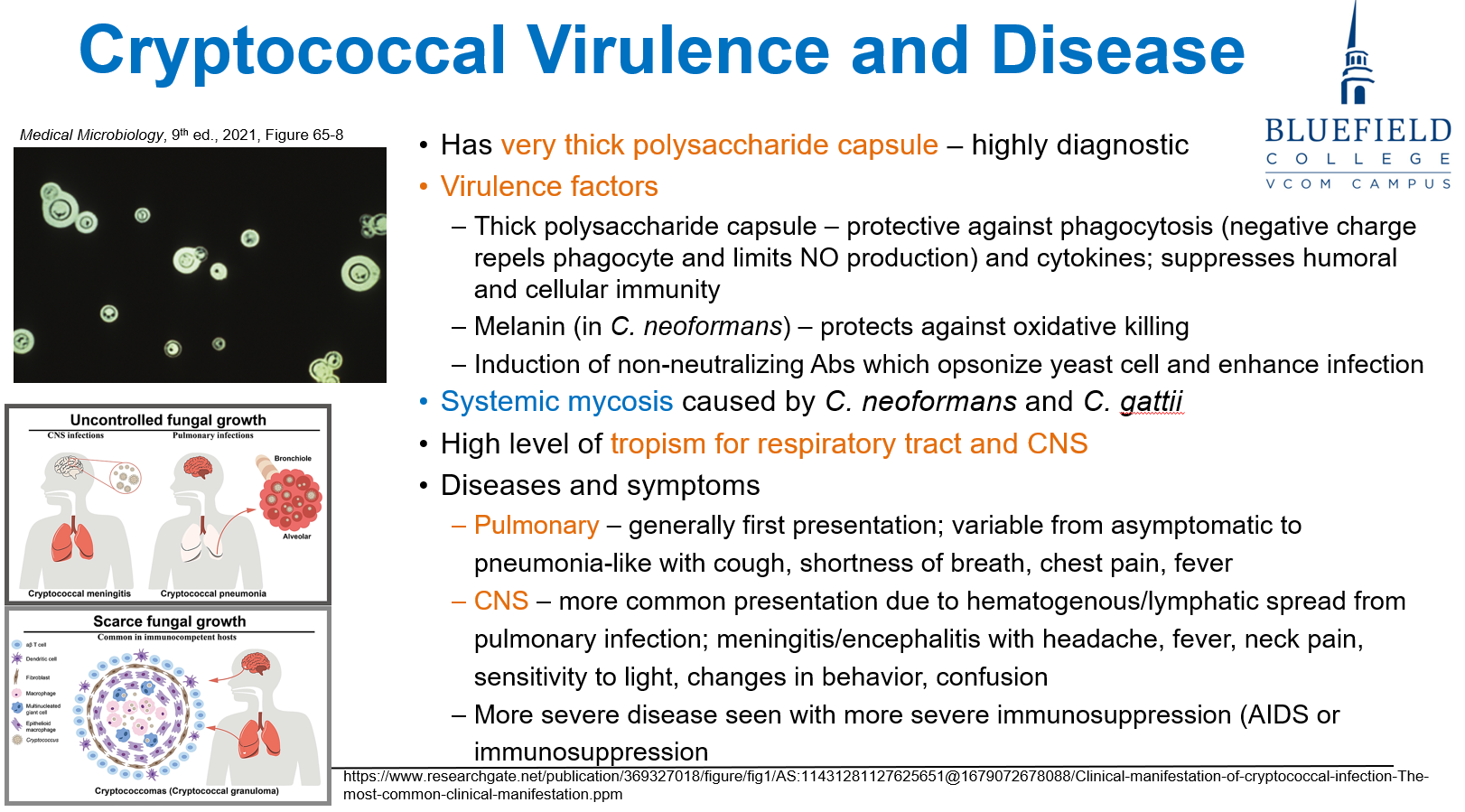
Where is Cryptococcus neoformans most commonly found?
A. Decaying vegetables
B. Dust in dry climates
C. Pigeon droppings and soil
D. Human mucosal flora
E. Contaminated lakes
C. Pigeon droppings and soil
Cryptococcus thrives in soil enriched with bird droppings, especially pigeons.
Which of the following symptoms is most consistent with cryptococcal meningitis?
A. Black eschar on nasal bridge
B. Eosinophilic asthma
C. Visual hallucinations and hyperactivity
D. Headache, neck stiffness, and photophobia
E. Ascending flaccid paralysis
D. Headache, neck stiffness, and photophobia
Disseminated Cryptococcus often infects the CNS, causing meningitis.
What radiologic or histologic finding is characteristic of Cryptococcus in the brain?
A. Ring-enhancing abscess
B. Ground-glass opacity
C. Soap bubble lesions
D. Butterfly glioma pattern
E. Honeycomb lung appearance
C. Soap bubble lesions
Clusters of yeast create "soap bubble" lesions in the basal ganglia and brain parenchyma.
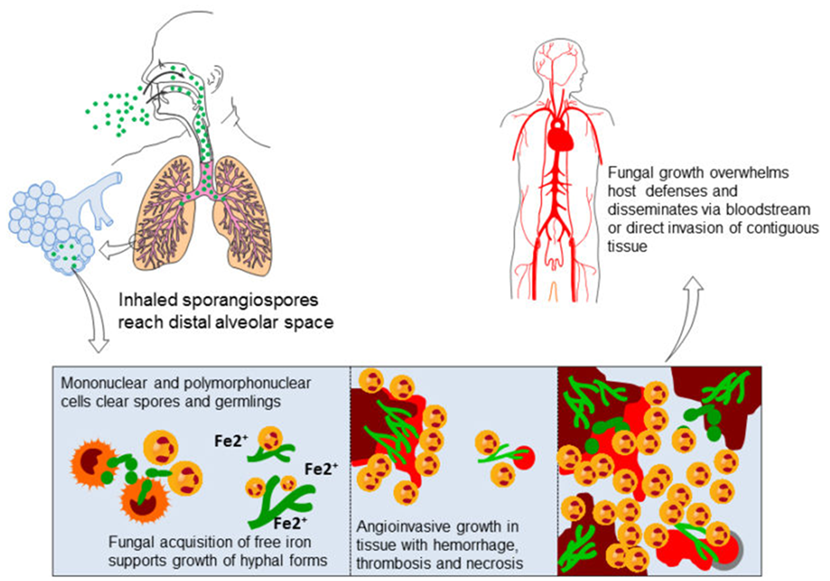
What best describes the hyphae of Mucor and Rhizopus species?
A. Septate, acute-angle branching
B. Septate, right-angle branching
C. Broad, non-septate, irregularly shaped hyphae
D. Encapsulated round yeast forms
E. Cigar-shaped budding yeasts
C. Broad, non-septate, irregularly shaped hyphae
Mucor and Rhizopus produce broad, non-septate hyphae with wide-angle branching.
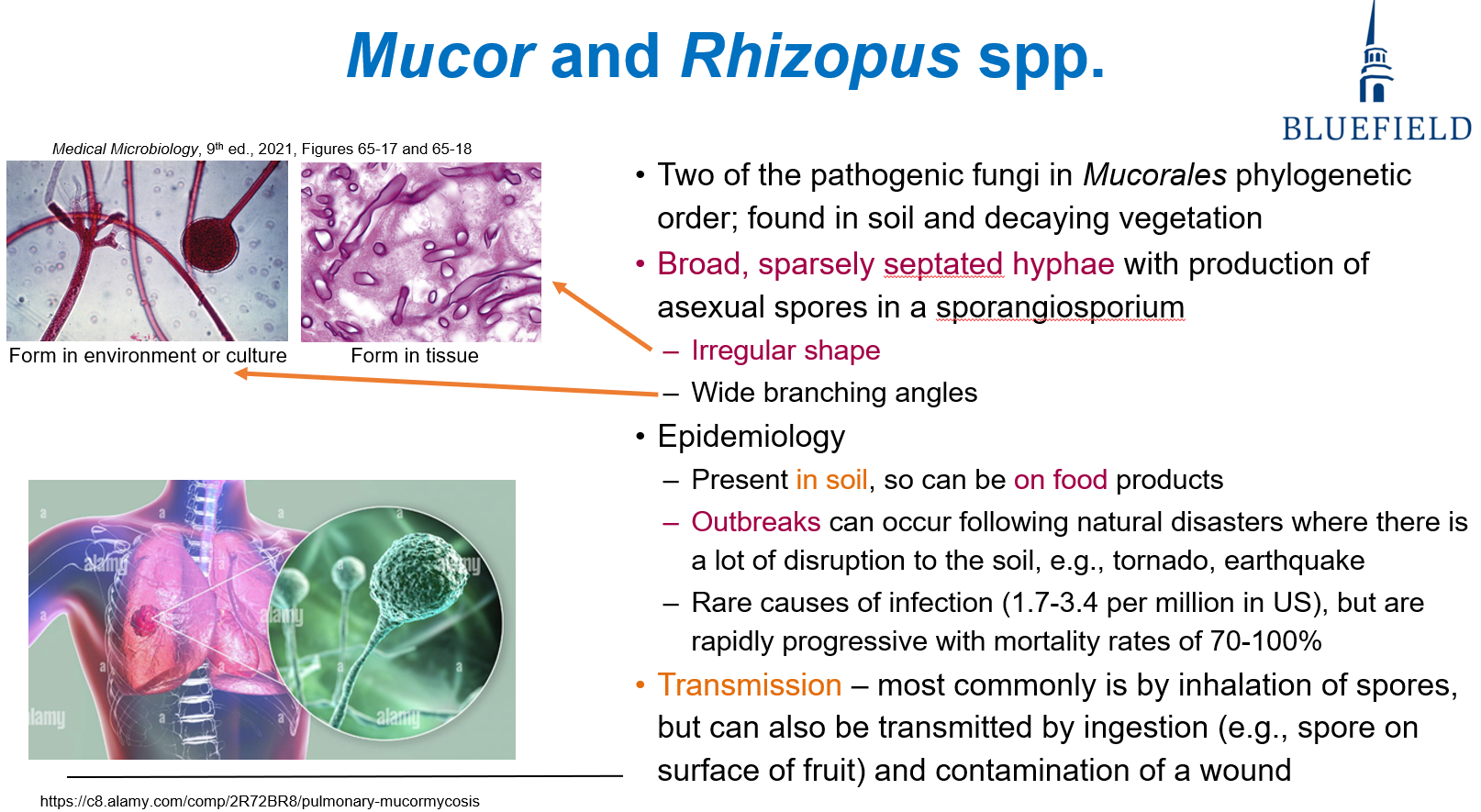
What is the most common route of transmission for mucormycosis?
A. Contaminated water
B. Inhalation of spores from soil
C. Arthropod bites
D. Sexual contact
E. Blood transfusion
B. Inhalation of spores from soil
Airborne spores from soil or decaying matter are the main transmission route.
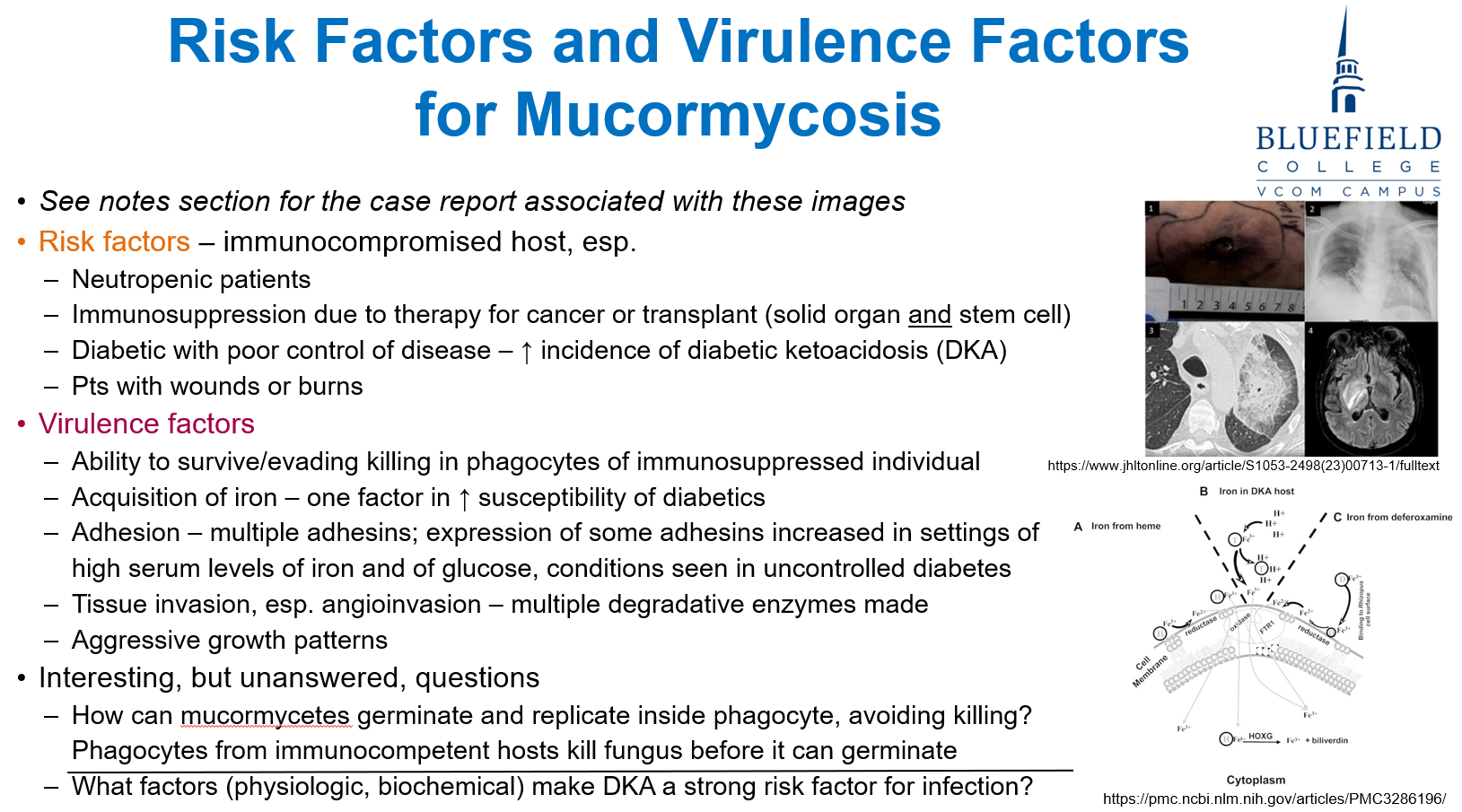
Why are diabetic patients particularly vulnerable to mucormycosis?
A. Defective complement pathways
B. Increased skin colonization
C. Elevated serum iron and glucose promote fungal growth
D. Greater spore inhalation rates
E. Preexisting lung fibrosis
C. Elevated serum iron and glucose promote fungal growth
Iron and glucose enhance Mucor adhesion and invasion, especially in diabetic ketoacidosis.
Which clinical syndrome is most characteristic of mucormycosis in a diabetic patient?
A. Pneumonitis with hemoptysis
B. Rhinocerebral infection with facial swelling and black eschar
C. Interstitial nephritis
D. Oral thrush with leukoplakia
E. Generalized lymphadenopathy
B. Rhinocerebral infection with facial swelling and black eschar
Rhinocerebral mucormycosis is common in DKA, presenting with facial necrosis and vision changes.
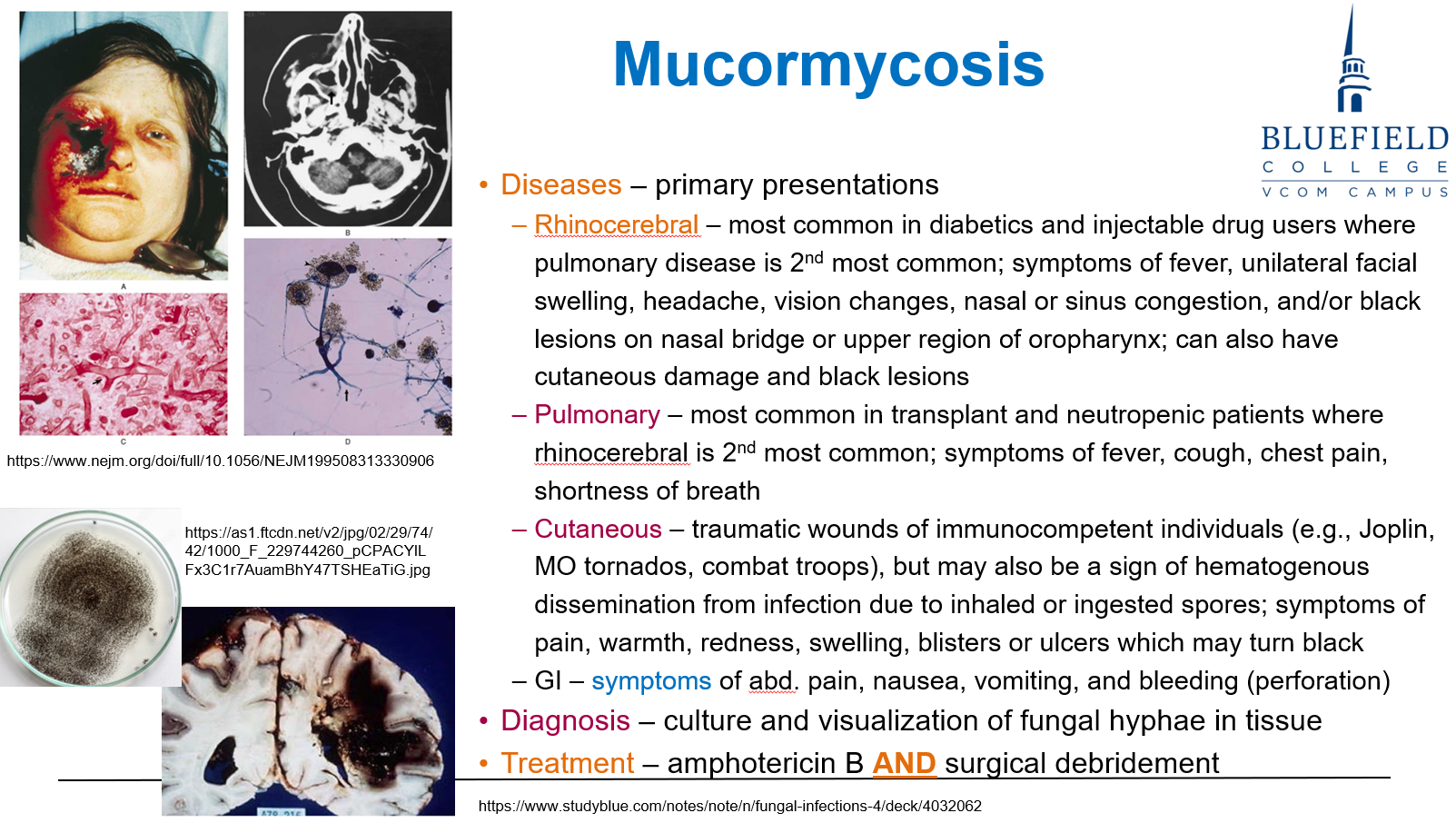
What is the best initial therapy for mucormycosis?
A. Fluconazole alone
B. Voriconazole plus corticosteroids
C. Amphotericin B plus surgical debridement
D. Echinocandins only
E. Observation and immune support
C. Amphotericin B plus surgical debridement
Aggressive treatment with Amphotericin B and debridement is needed due to rapid invasion.
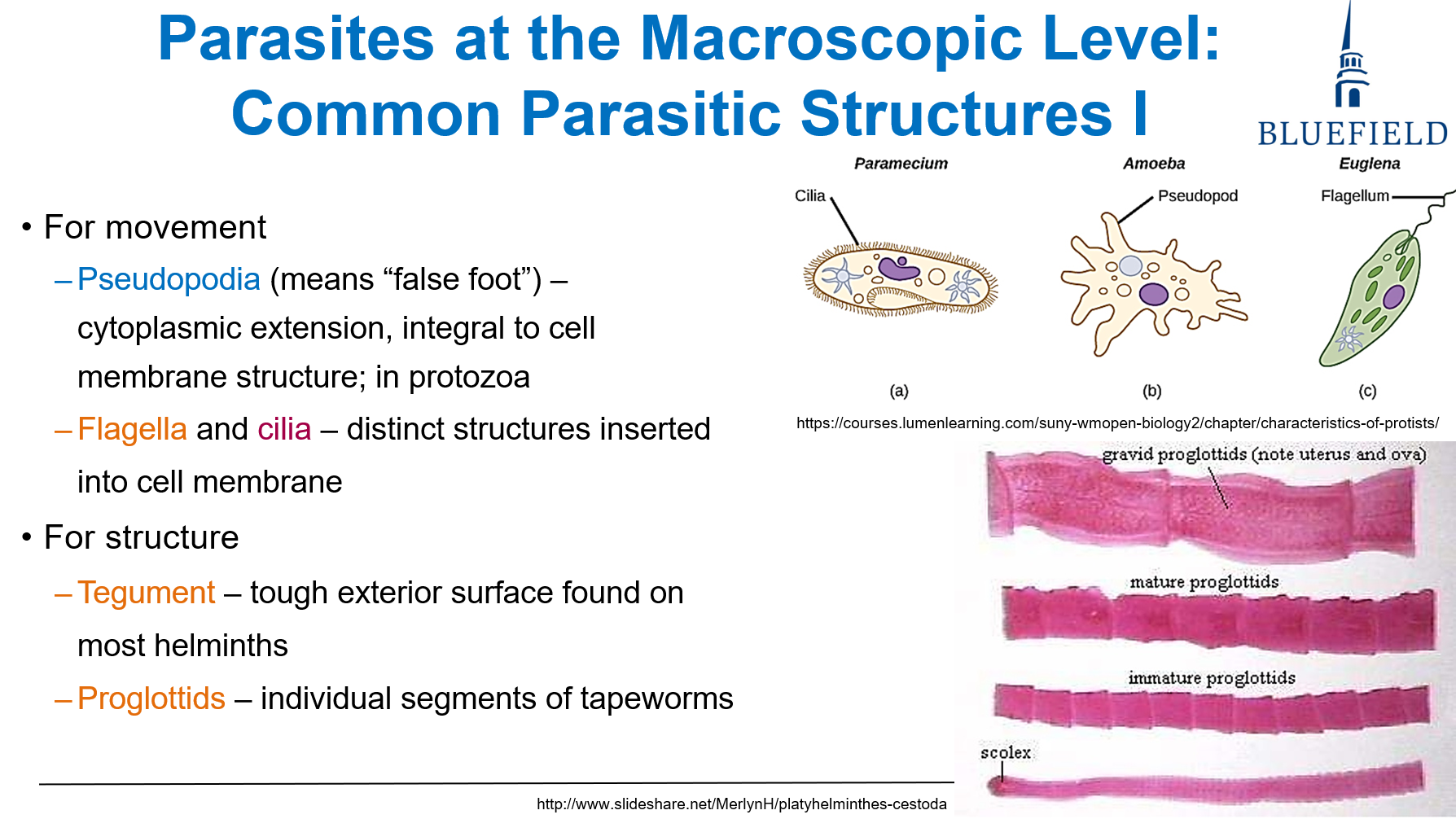
What helminth structure protects against environmental stress?
A. Proglottid
B. Scolex
C. Spicule
D. Tegument
E. Operculum
D. Tegument
The tegument is the outer protective surface of helminths that provides defense and absorption.
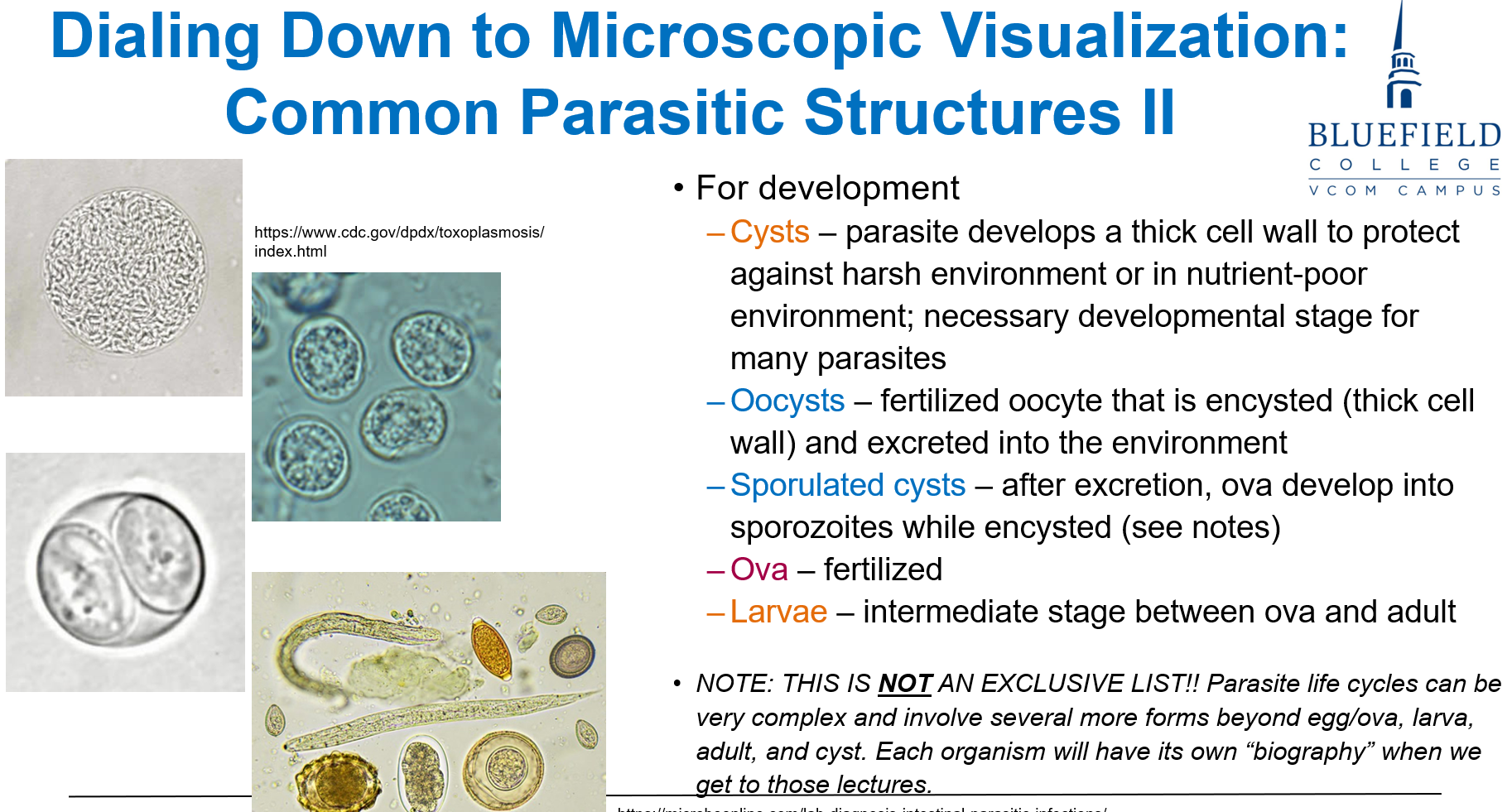
What is the primary role of cyst formation in parasites?
A. Promote reproduction
B. Release toxins
C. Facilitate feeding
D. Survive harsh conditions
E. Digest host tissues
D. Survive harsh conditions
Cysts allow parasites to endure low-nutrient or hostile environments and facilitate transmission.
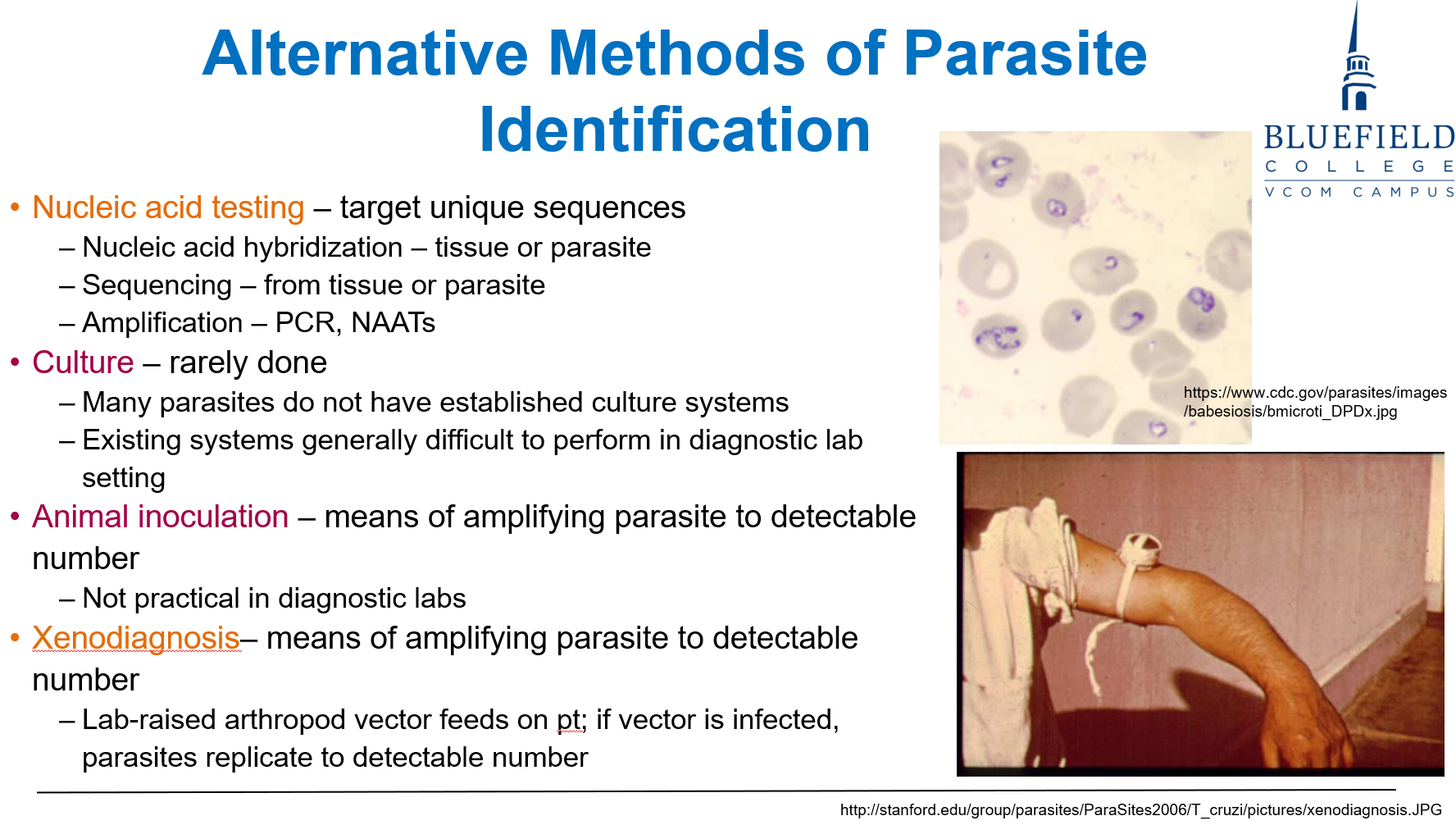
What does nucleic acid testing detect to identify parasites?
A. Protein adhesins
B. Hemolysin activity
C. Host antibodies
D. Unique genetic sequences
E. Spore wall thickness
D. Unique genetic sequences
PCR and NAATs target parasite DNA or RNA, allowing accurate identification.
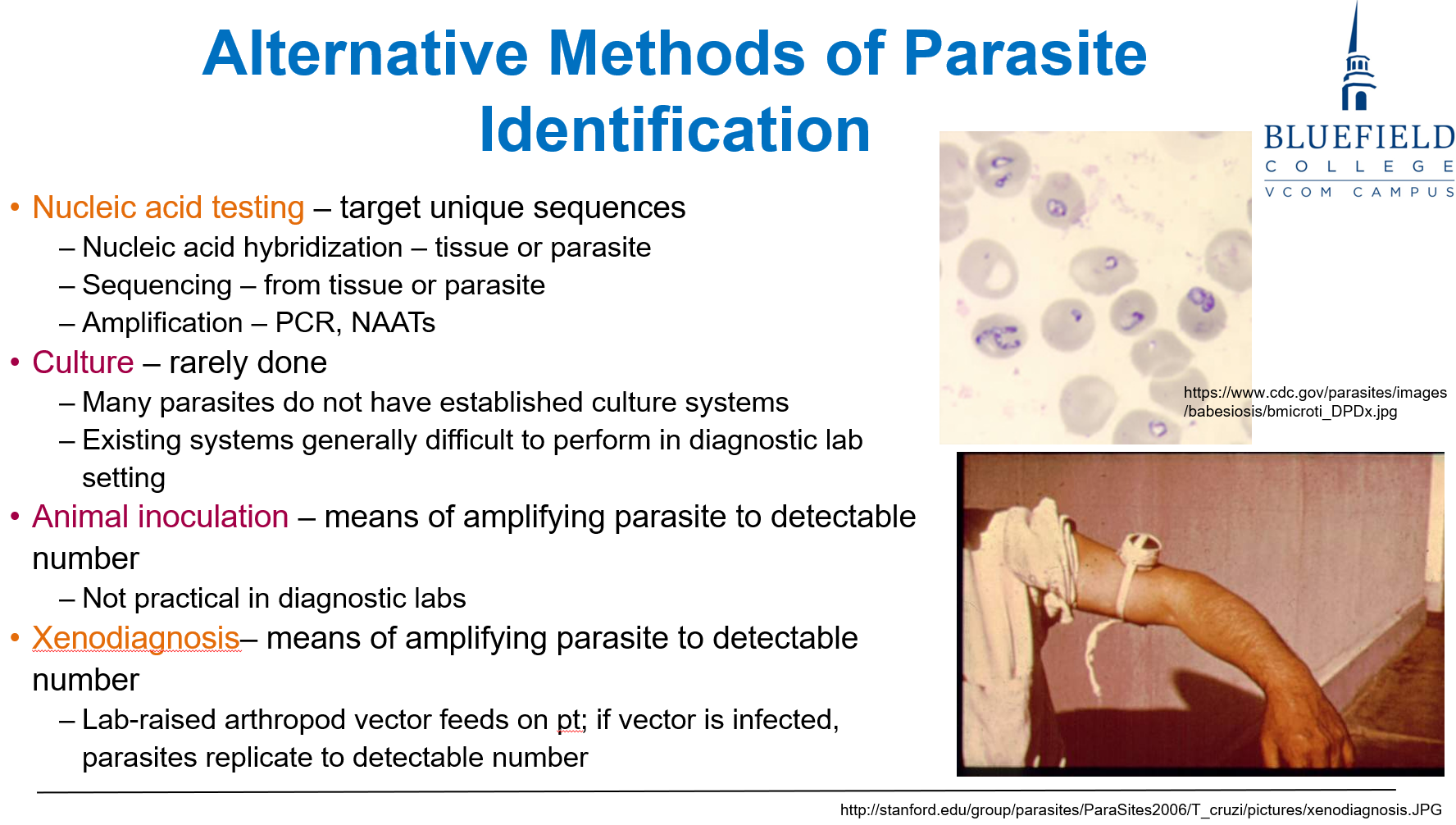
Why is xenodiagnosis used in parasitology?
A. To isolate toxins
B. To test vaccines
C. To amplify parasites
D. To treat parasites in vitro
E. To monitor resistance
C. To amplify parasites via vector infection
Xenodiagnosis uses arthropods to detect parasites by letting them feed on a patient and examining them afterward.
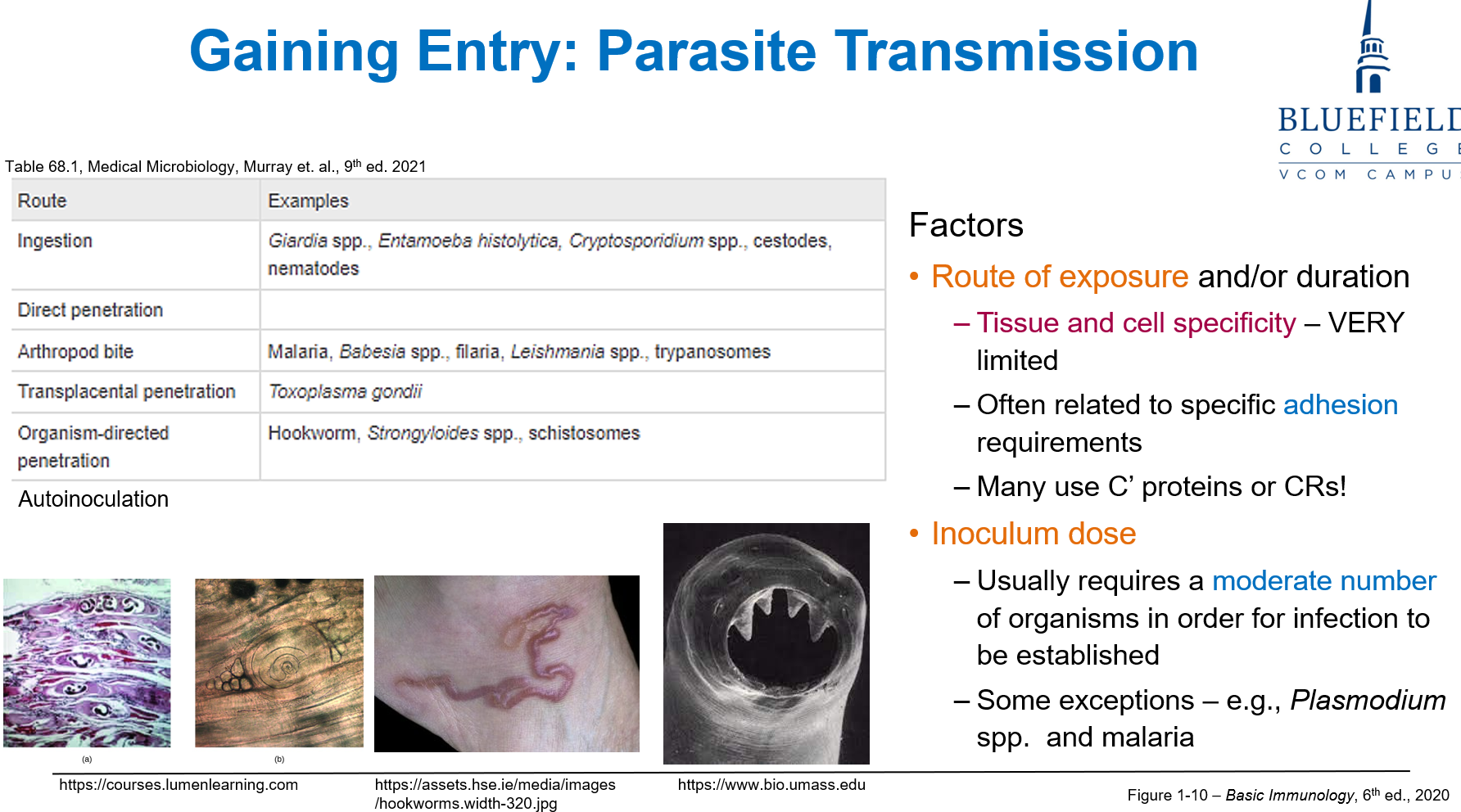
Why is tissue and cell specificity important in parasitic infection?
A. Only certain drugs work on specific tissues
B. Parasites bind specific host molecules for attachment
C. It limits parasite movement
D. Host response is uniform across tissues
E. Parasites replicate only in blood
B. Parasites bind specific host molecules for attachment
Parasites require specific tissues using adhesins and receptors to initiate infection.
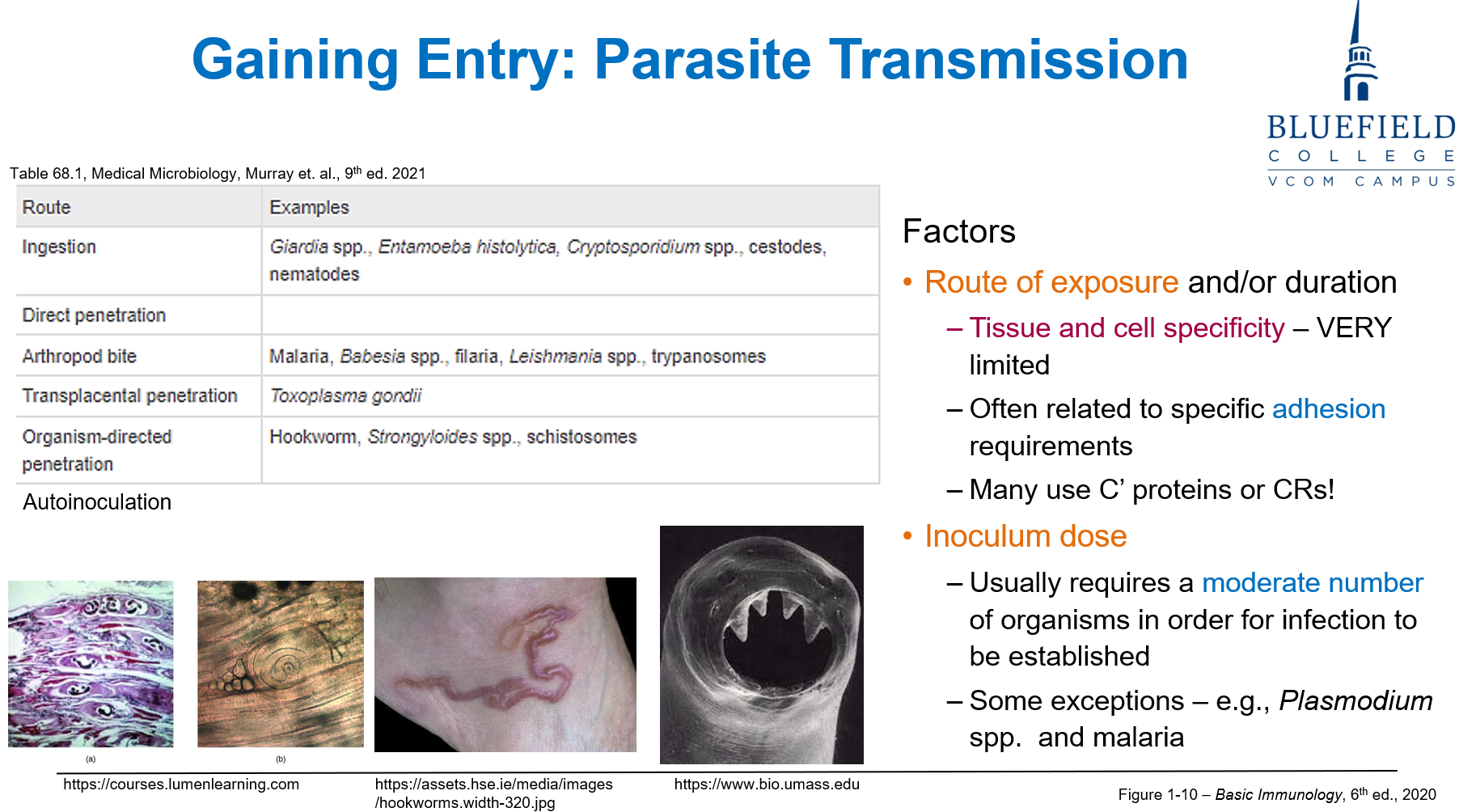
Which parasite can establish infection with a very low inoculum dose?
A. Fasciola hepatica
B. Taenia saginata
C. Trichuris trichiura
D. Plasmodium spp.
E. Necator americanus
D. Plasmodium spp.
Some parasites like Plasmodium and malaria can infect with few organisms, though others require larger doses.
What best describes schizogony in parasites?
A. Cyst release
B. Egg fertilization by sperm
C. Multiple nuclear divisions before cytoplasmic separation
D. Segment shedding by worms
E. Single-cell fission
C. Multiple nuclear divisions before cytoplasmic separation
Schizogony is an asexual replication process producing many daughter cells in protozoa.
A protozoan parasite survives outside the host by forming a metabolically inactive structure with a thick wall. Which of the following best describes the advantages of cyst formation for the parasite?
A. Enhances rapid replication and triggers inflammatory cytokine production
B. Promotes antigen recognition for early host immune priming
C. Reduces antigen exposure and enables survival in hostile environments
D. Facilitates intracellular motility and phagosome escape
E. Increases susceptibility to antimicrobial drugs by halting metabolism
C. Reduces antigen exposure and enables survival in hostile environments
Cyst formation allows parasites to become metabolically inactive, limit antigen production, and resist environmental stress, aiding transmission to new hosts.
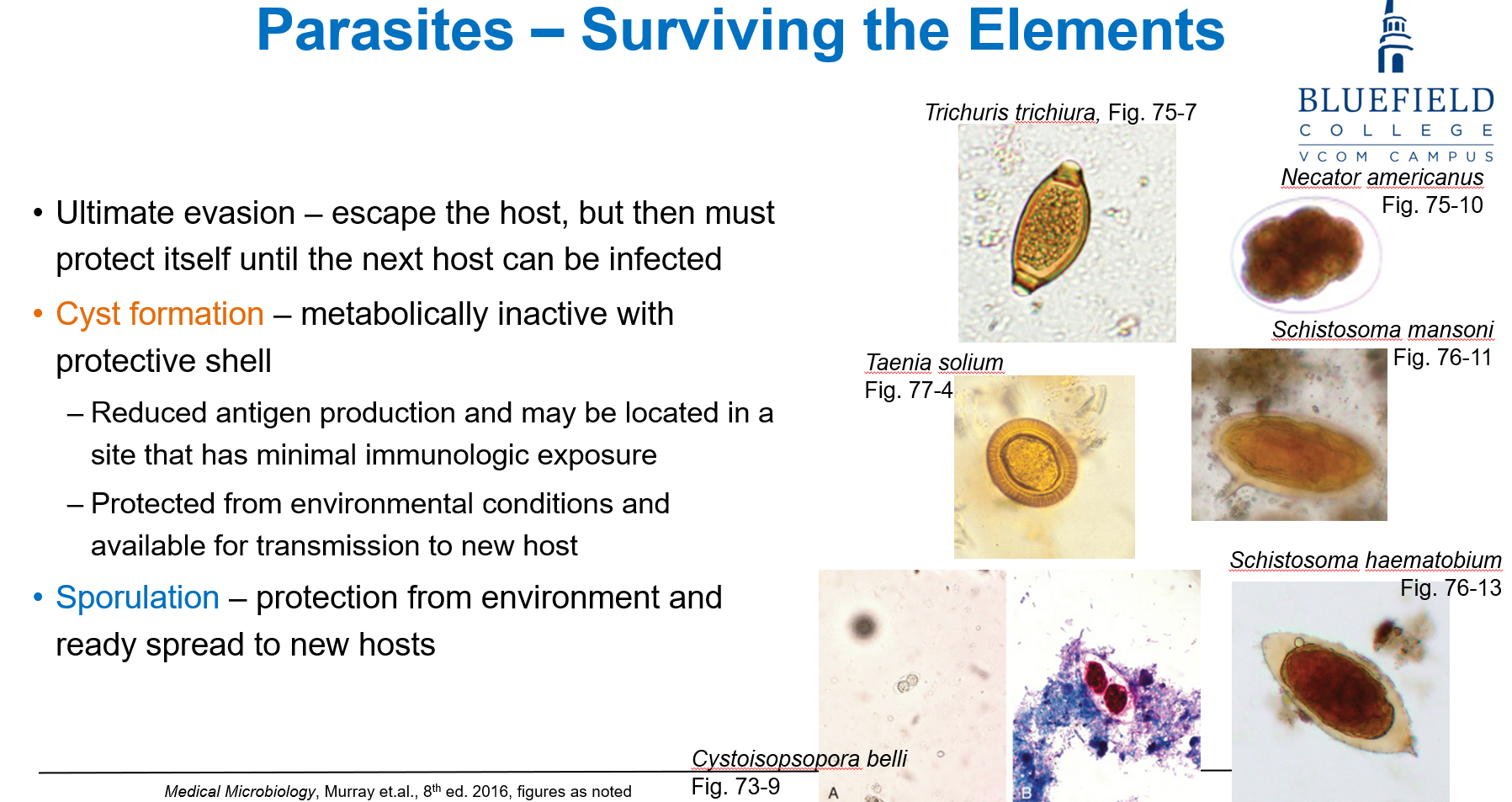
Which of the following stages is most helpful in fecal diagnosis?
A. Larval form
B. Adult worms
C. Proglottids
D. Cyst
E. Sclerotic body
D. Cyst
Cysts in stool samples are common diagnostic markers, especially for protozoa.
How do parasites avoid immune recognition via antigenic variation?
A. Kill immune cells
B. Block cytokine receptors
C. Shed or alter surface proteins
D. Mimic antibody structure
E. Trigger apoptosis
C. Shed or alter surface proteins
Antigenic variation enables parasites to evade detection by frequently changing surface antigens.
Which is a mechanical method of parasite-induced tissue damage?
A. Enzyme secretion
B. Host cell lysis by toxins
C. Penetration and migration through tissues
D. Mycotoxin release
E. Complement activation
C. Penetration and migration through tissues
Mechanical damage involves movement and attachment, disrupting host structures.
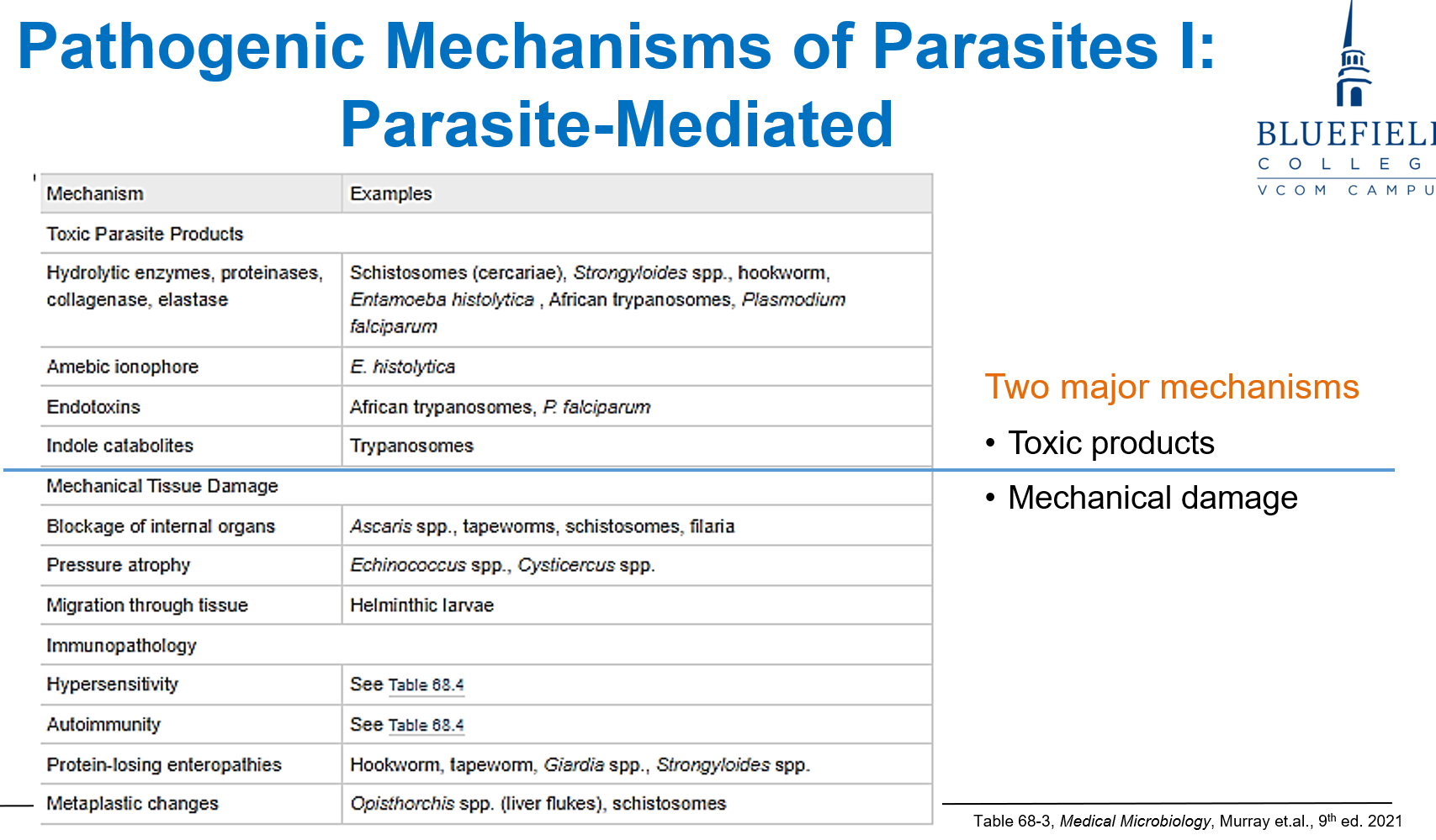
Which antiparasitic drug acts by inhibiting microtubule formation?
A. Metronidazole
B. Mebendazole
C. Chloroquine
D. Amphotericin B
E. Erythromycin
B. Mebendazole
Mebendazole disrupts microtubule polymerization, impairing parasite mobility and function.
“bend”
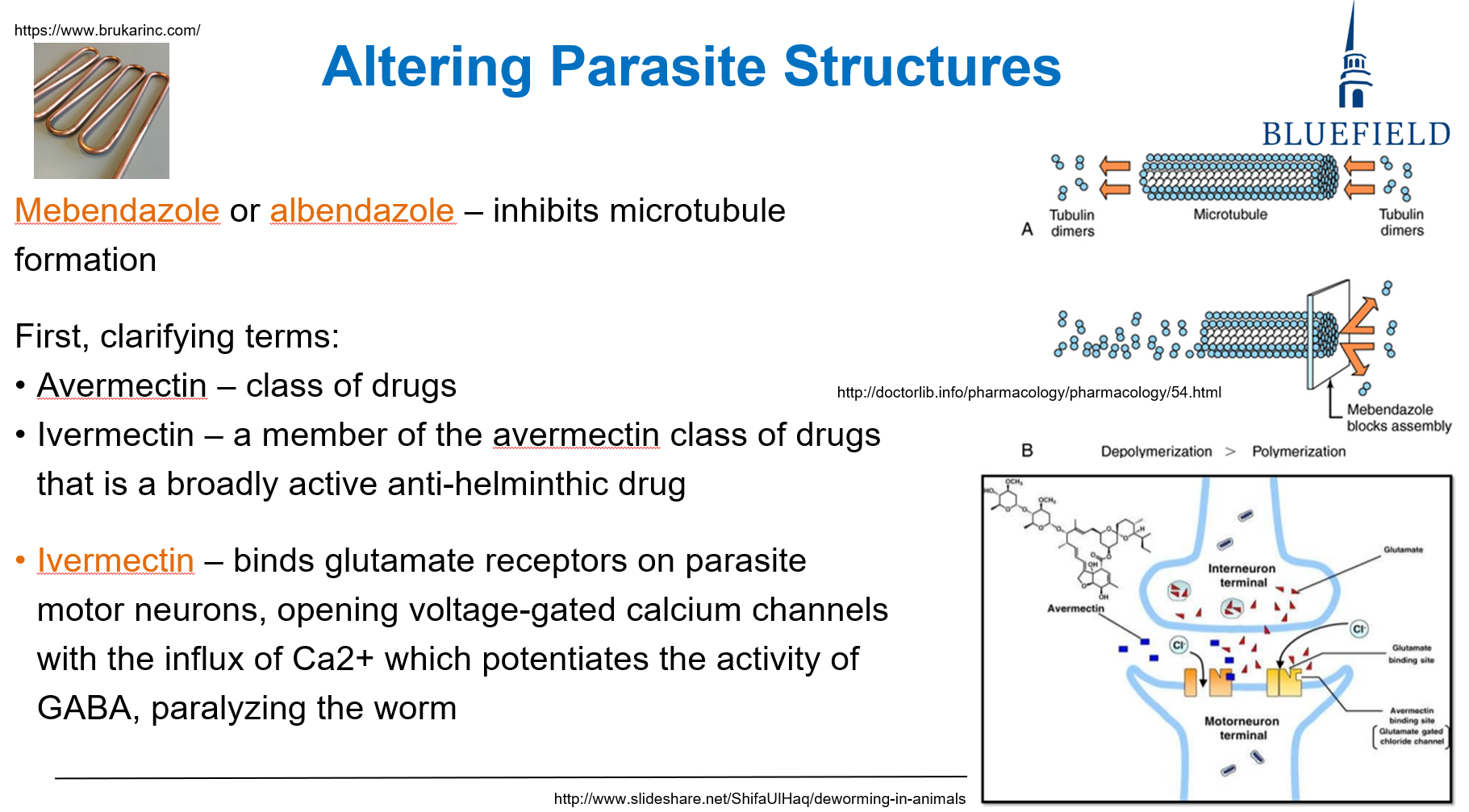
Which of the following targets parasite DNA synthesis?
A. Chloroquine
B. Nitazoxanide
C. Pyrimethamine
D. Ivermectin
E. Griseofulvin
C. Pyrimethamine
Pyrimethamine inhibits folate metabolism, preventing DNA replication in protozoa.