Cardiac Muscle
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
40 Terms
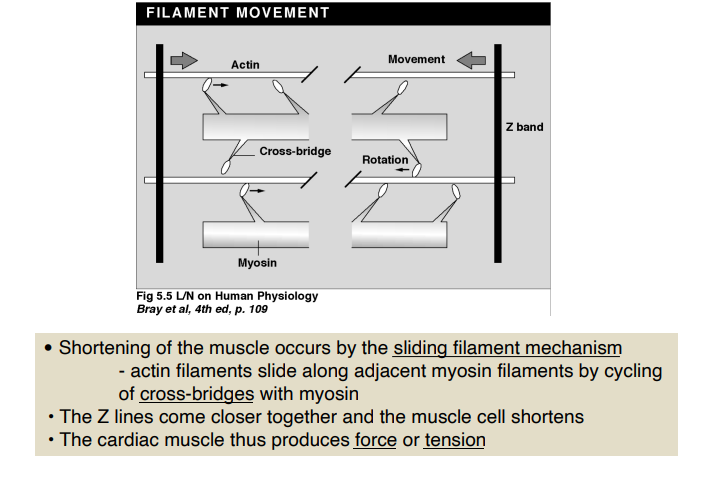
Mechanism by which muscles shorten
What is the significance of cardiac muscle’s ability to increase its contractile force with a slight increase in its length
It underlies its ability to control stroke volume
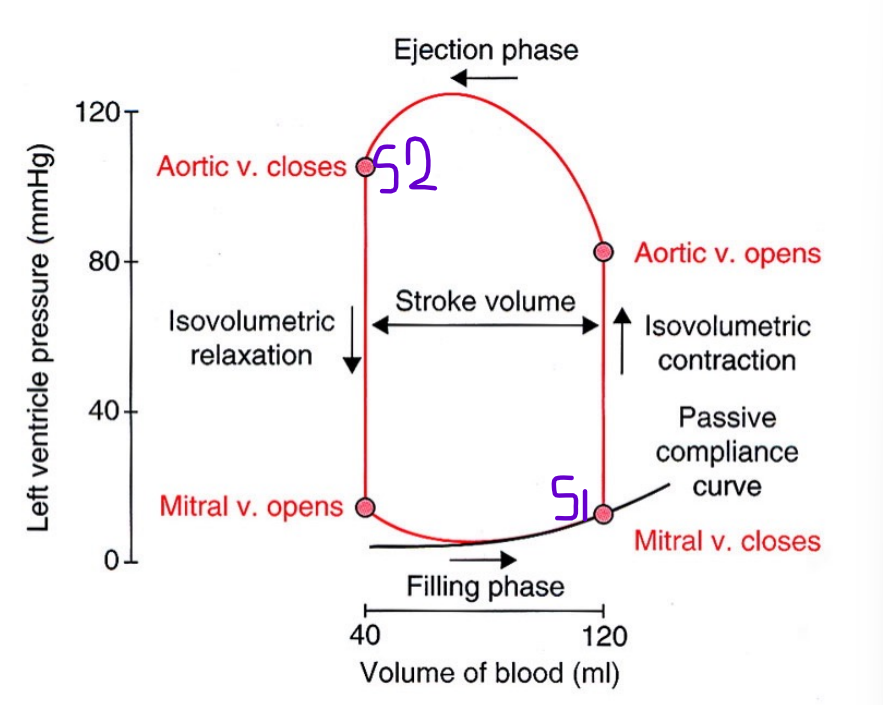
Stroke Volume
the volume of blood ejected from the heart during a single beat
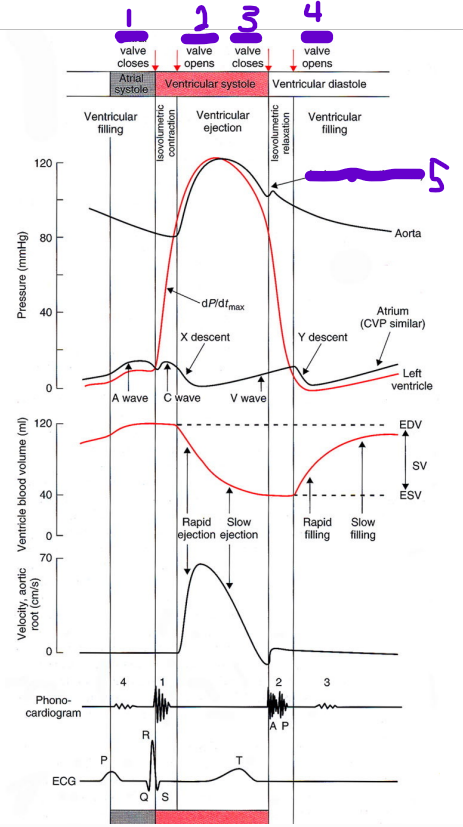
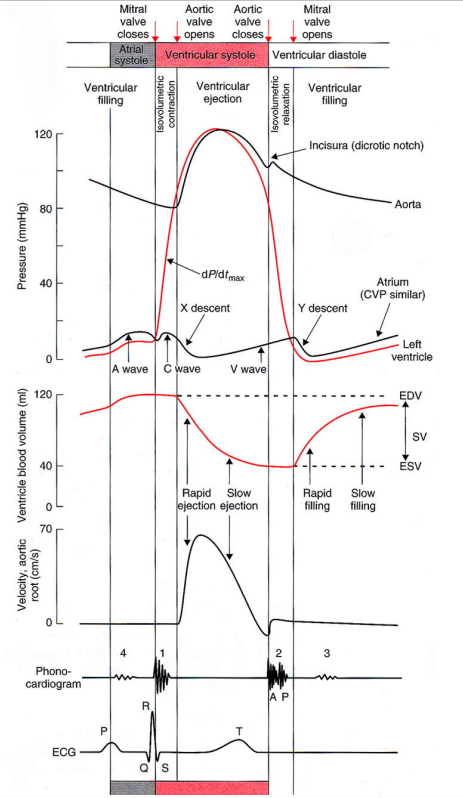
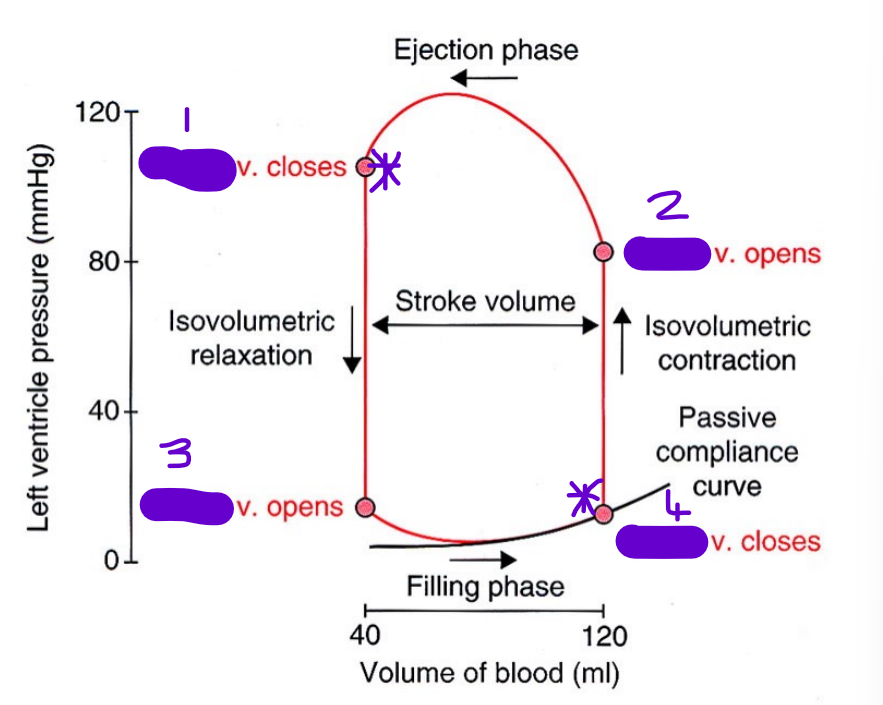
What heart sounds are heard at each of the stars *
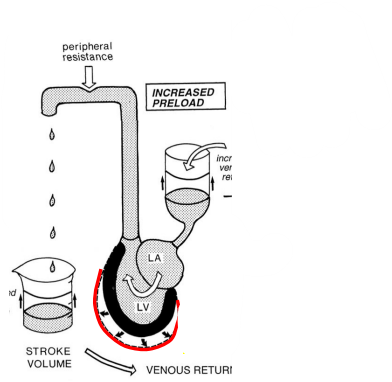
Preload
stretched condition of the heart muscle at the end of diastole (EDV)
What does this represent
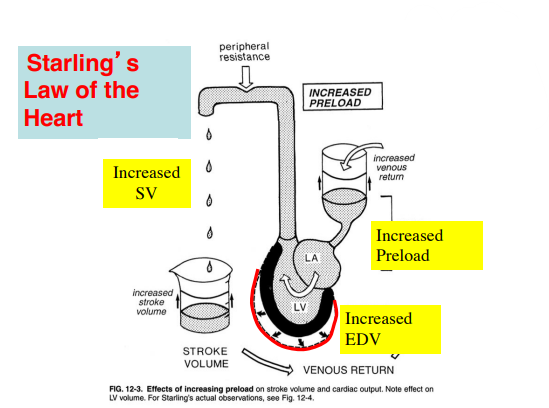
Starling's Law of the Heart states that the greater the stretch of the heart muscle (myocardium) during diastole, the greater the force of contraction during systole.
What does the starling curve represent
SV’s relationship with EDV
Every point on the starling curve has the same contractility
(Starling's Law of the Heart states that the greater the stretch of the heart muscle (myocardium) during diastole, the greater the force of contraction during systole.)
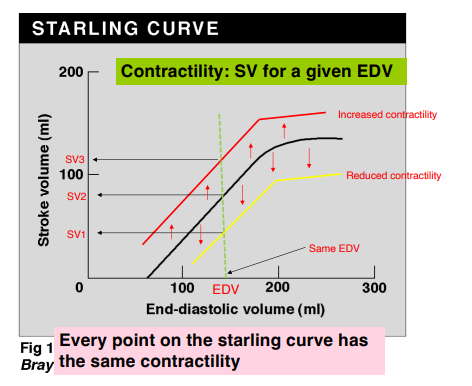
SV increases/decreases with EDV
Increases
Between what parameters does SV increase with EDV, why
90-200
EDV below 70ml - no SV
EDV above 200ml - SV no further increase - cardiac muscle overstretched
Other than an increased EDV, what can increase SV
An increase in contractility
dP/dtmax
The maximum rate at which VP rises
What is dP/dtmax used to measure
Myocardial contractility
Inotropic agents
Agents that cause an increase/decrease in contractility
Agents that cause an increase in contractility are said to have a positive inotropic effect
Agents that cause a decrease in contractility are said to have a negative inotropic effect
Examples of positive inotropic agents & how they work
noradrenaline, adrenaline : increase Ca2+ influx and uptake by the SR
increased intracellular Ca2+ (also increased extracellular but that’s not the point)
- digoxin : increases intracellular Ca2+ (blocks the Na/K pump which slows Na-Ca exchange)
Examples of negative inotropic agents
hypoxia
drugs: calcium channel blockers, beta adrenergic blockers
Structure of myosin
Thick filament
Contains 2 heads with ATPase activity
Structure of thin cardiac myofilament
Made up of actin, tropomysoin & troponin (TN)
Components of troponin complex
TN-T
TN-I
TN-C
(TIC)
Role of each of the components of troponin complex
TN-T: structural (TNT would cause structural damage🧨)
TN-I: Controls binding of Ca2+ to TN-C (I = In between - goes in between T & C)
TN-C: Ca2+ binding
What are the steps that lead to myosin binding to actin
Ca2+ concentration rises and Ca2+ binds to TN-C
Conformation change in tropomyosin
Myosin-binding site on actin is exposed and myosin binds to actin
How do Ca2+ ions come to enter muscle cells
Cells depolarised
Membrane potential rises
Threshold - L-type Ca channels open
Ca2+ ions enter cell
Explain the calcium-induced calcium release (CICR) mechanism in relation to contraction
The Ca2+ ions that enter the cell are only about 25% the amount of calcium needed to induce contraction.
the Ca2+ ions that enter cell “triggers” release of Ca2+ ions from the sarcoplasmic reticulum (SR)
This is enough Ca2+ to cause contraction
How does calcium cause muscle contraction
Ca2+ ions bind to troponin C in troponin complex
Tropomyosin moves
Actin-myosin interaction occurs
Muscle contraction occurs
RYR
Ryanodine receptor
Giant protein with a terminal foot with a T-shaped tube in its centre through which Ca2+ ions are released
(Ryan releases Calcium!)
Where is the density of RYR high
near L-type Ca channels
distance between the Ca channels and the RYR is long/short
short (nm)
Facilitates CICR (Calcium-induced calcium release)
How does calcium relate to muscle relaxation
High Ca2+ conc. inactivates RYR.
The Ca2+ channels close - No further Ca2+ entry (cessation of calcium entry)
No CICR release from SR
(negative feedback)
3 mechanisms by which intracellular Ca2+ is reduced by the cell
In order of importance:
SERCA (SR ATP-dependent Ca pump) pumps Ca2+ ions from the cytoplasm into the SR stores
Sodium-calcium (Na+-Ca2+) exchanger in the cell membrane powered by the Na+ gradient
Cell membrane ATP-dependent Ca pump
What regulates SERCA
SERCA is regulated by the regulatory protein, Phospholamban (PLN), which inhibits Ca2+ uptake by the SR while in its dephosphorylated state
Effect of sympathetic stimulation of cardiac muscle
an increase in active tension
an increase in the rate of tension development
an increase in the rate of tension relaxation
Example of sympathetic stimulation of cardiac muscle
β-adrenergic stimulation
What activates protein kinase A (PKA)
cAMP
(PKA loves going camping!)
What does PKA phosphorylate in muscle cells
L-type calcium channel
Phospholamban (PLN)
Troponin I
Role of PLN in relaxation
PLN reduces inhibition of SERCA which increases the uptake of calcium into the SR, causing relaxation
(PLN ↑SERCA ↑Relaxation ↑Contraction)
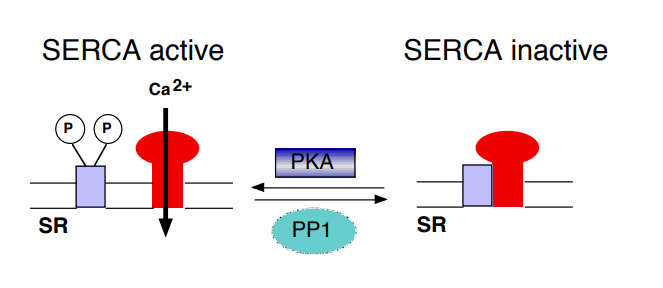
How does PLN phosphorylation promote the rate of contraction
PLN phosphorylation promotes the rate of contraction because it increases uptake of calcium into the SR causing relaxation but it also means the SR is loaded with Ca for the next contractions
Role of troponin I in relaxation
troponin I inhibits the binding of calcium to troponin C, causing relaxation
(TN-I is In control of C)
Effect of increased intracellular Ca2+ concentration on muscle cells
increases the force of contraction - positive inotropic effect
Starling’s Law of the Heart
Increased filling of the ventricle causes an increase in SV
Increased muscle fibre length increases the force of contraction
How does Starling’s Law of the Heart work
Increased stretching of the muscle fibre increases the sensitivity of troponin C for Ca2+ • A stronger force of contraction for a given Ca2+ concentration