Human Physiology Neuromuscular Disorders
1/76
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
77 Terms
What are neuromuscular disorders?
A group of medical conditions that impair muscle function either directly (muscle pathologies) or indirectly (nerve or neuromuscular junction pathologies).
How can neuromuscular disorders affect muscles directly?
Through pathologies of voluntary muscle.
How can neuromuscular disorders affect muscles indirectly?
Through pathologies of nerves or the neuromuscular junction (NMJ).
What are the four basic types of neuromuscular disorders?
Disorders involving damage to:
Lower motor neurons
Peripheral nerves
Neuromuscular junction (NMJ)
Muscle
How are the structures of the nervous system connected?
They are intimately connected, working together to control body functions.
What are the two main parts of the nervous system?
The central nervous system (CNS) and the peripheral nervous system (PNS).
What structures make up the central nervous system (CNS)?
The brain and spinal cord.
What structures make up the peripheral nervous system (PNS)?
Nerves that connect the brain and spinal cord with muscles, glands, and sense organs.
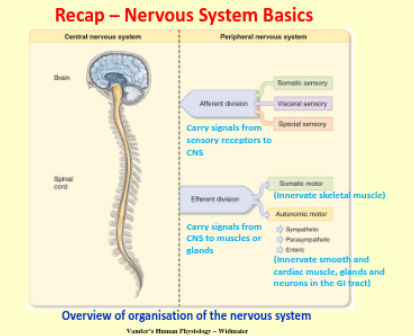
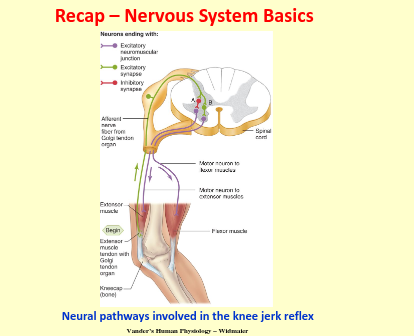
Recap — Nervous system basics
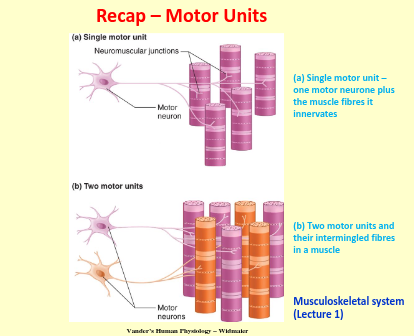
Recap - motor units
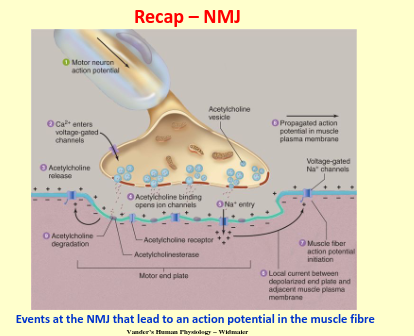
Recap - NMJ
What are the four basic types of neuromuscular disorders?
Disorders involving damage to:
Lower motor neurons
Peripheral nerves
Neuromuscular junction (NMJ)
Muscle
Which type of neuromuscular disorder involves damage to nerve cells that control voluntary muscle movement?
Lower motor neuron disorders.
Which type of neuromuscular disorder affects the nerves that connect the CNS to muscles and organs?
Peripheral nerve disorders.
Which type of neuromuscular disorder affects the connection between nerves and muscles?
Neuromuscular junction (NMJ) disorders.
Which type of neuromuscular disorder directly affects the structure and function of muscles?
Muscle disorders
What is motor neurone disease (MND)?
A progressive degeneration of upper and lower motor neurons in the brain and spinal cord.
How common is motor neurone disease (MND)?
It is a rare condition, affecting approximately 2 in 100,000 people each year.
Who is most commonly affected by motor neurone disease (MND)?
Males over the age of 50.
What causes motor neurone disease (MND)?
The cause is unknown, though 5% of cases have a family history.
What is the average survival time after diagnosis with motor neurone disease (MND)?
Around 3 years, though some patients may live up to 10 years or longer (e.g. Prof Stephen Hawking).
What are the main symptoms of motor neurone disease (MND)?
Weakness and wasting of muscles in the limbs, trunk, and neck.
How does motor neurone disease (MND) affect speech and swallowing?
It can cause bulbar muscle palsy, leading to difficulties with speaking, swallowing, and chewing
Why do respiratory problems occur in motor neurone disease (MND)?
Because the nerves and muscles that control the lungs are affected.
Does motor neurone disease (MND) affect the sensory system (sight, hearing, sensation)?
No
Is there a cure for motor neurone disease (MND)?
No, treatment focuses on relieving symptoms and slowing disease progression.
What medication is used to slow the progression of MND?
Riluzole, which reduces motor neurone sensitivity to glutamate.
What types of drugs help manage symptoms of MND?
Drugs to reduce muscle spasticity (stiffness) and drooling.
How can breathing and nutrition be supported in MND patients?
Ventilatory support for breathing and gastrostomy for feeding.
What therapies can help improve quality of life for MND patients?
Physiotherapy, occupational therapy, and speech therapy.
What does the term "neuropathy" mean?
"Nerve disease" – damage to one or more nerves of the peripheral nervous system (PNS).
What is mononeuropathy?
Damage to a single nerve, often due to compression (e.g. carpal tunnel syndrome).
What is mononeuritis multiplex?
Damage to several nerves, often due to conditions like vasculitis
What is polyneuropathy?
Damage affecting many nerves, as seen in conditions like Guillain-Barré syndrome.
How do peripheral nerve disorders present clinically?
Symptoms depend on the affected nerves and may include weakness, numbness, tingling, or pain.
What is the major peripheral nerve of the upper limb that innervates most flexor muscles in the anterior forearm?
The median nerve.
Which muscles does the median nerve innervate?
The majority of flexor muscles in the anterior forearm and some intrinsic hand muscles.
What sensory areas does the median nerve supply?
The thumb and most fingers (except the little finger and part of the ring finger).
What condition can result from compression of the median nerve in the carpal tunnel?
Carpal tunnel syndrome (CTS).
Where can the median nerve be compressed in the upper limb?
At the wrist (carpal tunnel) or at other points along its anatomical course.
CTS
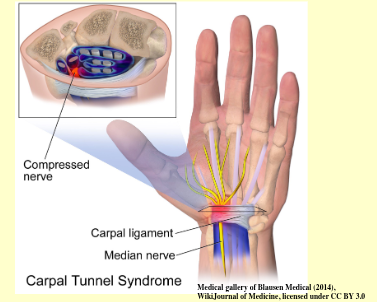
Recall the risk factors to CTS
• Strenuous, repetitive work e.g. using vibrating tools, manual labour
• Arthritis (can cause swelling of wrist joint and tendons)
• Pregnancy (hormonal changes / fluid retention)
• Diabetes
• Obesity
• Hand injuries e.g. sprain, fracture or crush injury
What are the main symptoms of carpal tunnel syndrome (CTS)?
Tingling, numbness, and pain in one or both hands.
When do the symptoms of carpal tunnel syndrome (CTS) tend to be worse?
Symptoms are often worse at night or early in the morning.
What type of hand weakness is commonly associated with carpal tunnel syndrome (CTS)?
Weakness in the hand, particularly in gripping and performing fine motor tasks
What is a common sign of muscle damage in carpal tunnel syndrome (CTS)?
Wasting away (atrophy) of the muscles at the base of the thumb (thenar eminence).
What is one non-invasive treatment for carpal tunnel syndrome (CTS)?
Wrist splints to keep the wrist in a neutral position and reduce pressure on the median nerve.
What type of injections can help alleviate symptoms of carpal tunnel syndrome (CTS)?
Local steroid injections to reduce inflammation and swelling
What surgical treatment can relieve pain in carpal tunnel syndrome (CTS)?
CTS release surgery, which relieves pain by reducing pressure on the median nerve.
What does the name "Myasthenia Gravis" mean?
It is derived from the Greek words for "severe muscle weakness."
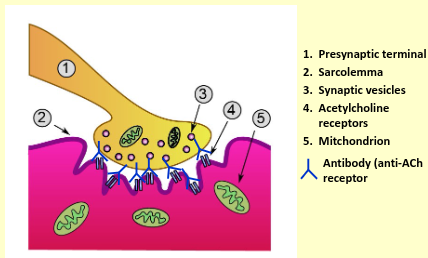
How does neuromuscular transmission fail in Myasthenia Gravis (MG)?
Transmission fails due to autoimmune attack on the nicotinic acetylcholine (ACh) receptors at the motor end plate.
What is the cause of Myasthenia Gravis (MG)?
It is an autoimmune disease where about 90% of patients produce antibodies against their own ACh receptors.
What happens when antibodies bind to acetylcholine (ACh) receptors in Myasthenia Gravis (MG)?
The binding interferes with the normal actions of ACh at the neuromuscular junction (NMJ).
How does Myasthenia Gravis (MG) affect the motor end plate?
The motor end plate is damaged, further impairing neuromuscular transmission
Pathophysiology of MG
How common is Myasthenia Gravis (MG)?
It is an uncommon disease with a prevalence of approximately 4 in 100,000.
What age group is most commonly affected by Myasthenia Gravis (MG)?
It mainly occurs in young females, with a peak age of incidence around 30.
Can Myasthenia Gravis (MG) affect older adults?
Yes, it can also be late onset, affecting elderly men over the age of 60.
What are two conditions associated with Myasthenia Gravis (MG)?
Hyperplasia (enlargement) of the thymus gland and thymoma (a tumour of the thymus).
What is a common symptom of Myasthenia Gravis (MG)?
Fatiguability in many muscles.
Which muscles are commonly affected in Myasthenia Gravis (MG)?
Eyes: Diplopia (double vision), ptosis (drooping eyelid), eye closure weakness.
Bulbar muscles: Problems with speaking, swallowing, and chewing.
Limbs and neck: Weakness in arms, legs, and neck.
Respiratory muscles: Respiratory difficulties
Recall the different treatments of MG
• Corticosteroids
• Immunosuppressive drugs
• Acetylcholinesterase inhibitors
• Removal of antibodies by plasma exchange
• Thymectomy
What is Duchenne Muscular Dystrophy (DMD)?
A progressive degeneration and weakness of muscles.
How is Duchenne Muscular Dystrophy (DMD) inherited?
It is an X-linked inherited disease, usually affecting boys.
What is the prevalence of Duchenne Muscular Dystrophy (DMD)?
It affects 1 in 3,500 to 5,000 male births (~100 boys born with DMD per year in the UK).
What causes Duchenne Muscular Dystrophy (DMD)?
A mutation in the dystrophin gene, leading to an absence or non-functioning dystrophin protein.
What is dystrophin?
Dystrophin is a large protein that connects the cytoskeleton of muscle fibres to the surrounding extracellular matrix through the cell membrane.
What role does dystrophin play in muscle fibres?
It maintains the structural integrity of muscle fibres.
What happens in the absence of dystrophin in muscle cells?
Without dystrophin, muscle fibres become susceptible to cell membrane rupture and cell death.
What are some common symptoms of Duchenne Muscular Dystrophy (DMD) in children?
Difficulty walking, running, or jumping
Difficulty standing up
Inability to climb stairs without support
Mild developmental delay
By what age do children with Duchenne Muscular Dystrophy (DMD) generally require a wheelchair?
By their teens
What is the typical life expectancy for individuals with Duchenne Muscular Dystrophy (DMD)?
Generally, they live up to 30 years of age.
What is Gower’s sign in Duchenne Muscular Dystrophy (DMD)?
It refers to the need for a boy with DMD to use his arms to go from lying to standing, as the muscles of the hip girdle and trunk are the first to weaken.
Is there a cure for Duchenne Muscular Dystrophy (DMD)?
No, there is currently no cure. Treatment focuses on managing the condition.
What therapies can help manage Duchenne Muscular Dystrophy (DMD)?
Physiotherapy and occupational therapy.
What type of support might be required for individuals with Duchenne Muscular Dystrophy (DMD)?
Ventilatory support to assist with breathing.
How do corticosteroids help in the treatment of Duchenne Muscular Dystrophy (DMD)?
Corticosteroids improve muscle strength and slow muscle weakness.