bio 251 jjc final with complete expert curated questions and answers (with Diagrams)
1/45
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
46 Terms
steroid hormones work? (Receptor location
steroid hormones exert their effects by diffusing through cell membranes and binding to intracellular receptors located in the cytoplasm or nucleus. This binding initiates a cascade of events that lead to changes in gene expression and ultimately result in the hormone's specific physiological effects.
What are the stimuli for hormone release? - Humoral, hormonal and neural.
Humoral Stimuli: Changes in blood levels of ions/nutrients.
Hormonal Stimuli: Hormones triggering other hormones.
Neural Stimuli: Direct nervous system stimulation.
Know the hormones that are especially important to normal growth, and know their roles
-Growth Hormone (GH) and Insulin-Like Growth Factor 1 (IGF-1): Directly stimulate growth in bones and tissues.
-Thyroid Hormones (T4 and T3): Regulate metabolism and enhance the effects of GH.
-Insulin: Provides energy and building blocks for growth and works with GH.
-Parathyroid Hormone (PTH) and Vitamin D: Maintain calcium levels for bone growth.
-Sex Hormones (Estrogens and Androgens): Promote growth and maturation during puberty.
-Cortisol: Regulates metabolism but can inhibit growth if levels are too high.
Know the general adaptation syndrome (stress response) and homeostatic responses
-General Adaptation Syndrome (GAS): Describes the body’s response to prolonged stress in three stages—Alarm, Resistance, and Exhaustion.
-Homeostatic Responses: Involve various mechanisms and feedback loops to maintain stability in the internal environment, including temperature regulation, blood pressure regulation, fluid balance, and acid-base balance.
human growth hormone (hGH)
hormone produced by the pituitary gland; stimulates cell reproduction and growth
Thyroid hormone function and know that it is stored in the 'colloid' inside the follicles.
Thyroid hormones (T4 and T3) regulate metabolism, growth and development, protein, carbohydrate, and lipid metabolism, cardiovascular function, and nervous system activity. They are synthesized and stored in the colloid within thyroid follicles. The colloid serves as a reservoir for these hormones, allowing the thyroid gland to release them into the bloodstream as needed to maintain physiological balance.
Know the layers of adrenal cortex and what they secrete
Zona Glomerulosa: Produces aldosterone, which regulates blood pressure and electrolyte balance.
Zona Fasciculata: Produces cortisol, which regulates metabolism, stress response, and inflammation.
Zona Reticularis: Produces androgens, which contribute to sexual development and function.
Know the important components and major functions of blood.
Plasma: The liquid matrix that transports nutrients, hormones, and waste products.
Red Blood Cells: Transport oxygen and carbon dioxide.
White Blood Cells: Provide immune defense against infections.
Platelets: Involved in blood clotting and preventing blood loss.
What is serum
plasma without clotting factors
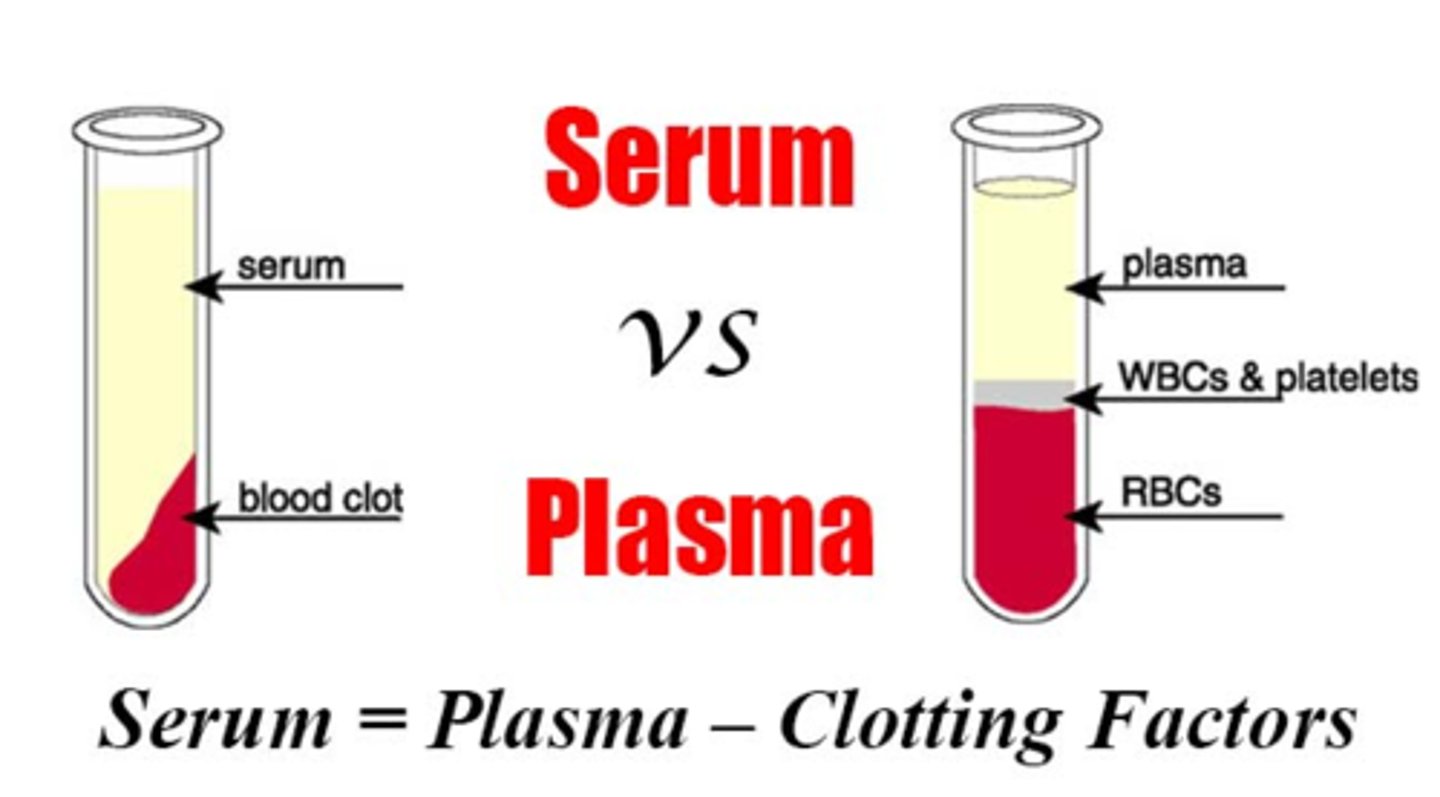
Know what is formed elements
Red Blood Cells (RBCs) or Erythrocytes
White Blood Cells (WBCs) or Leukocytes
Platelets or Thrombocytes
Process of hemostasis. - positive feedback
Platelet activation and aggregation result in the release of more platelet activators, which further stimulates platelet activation and aggregation. This positive feedback loop amplifies the hemostatic response, leading to the rapid formation of a stable platelet plug and blood clot.
Know to trace the flow of blood through the heart, identifying the major blood vessels, chambers and heart valves
Blood flows through the heart in a continuous loop, starting with deoxygenated blood entering the right atrium, traveling through the right ventricle to the lungs for oxygenation, returning to the left atrium, and then being pumped out to the body through the left ventricle and aorta. Along the way, blood passes through various chambers and valves, ensuring a unidirectional flow and efficient circulation throughout the body.
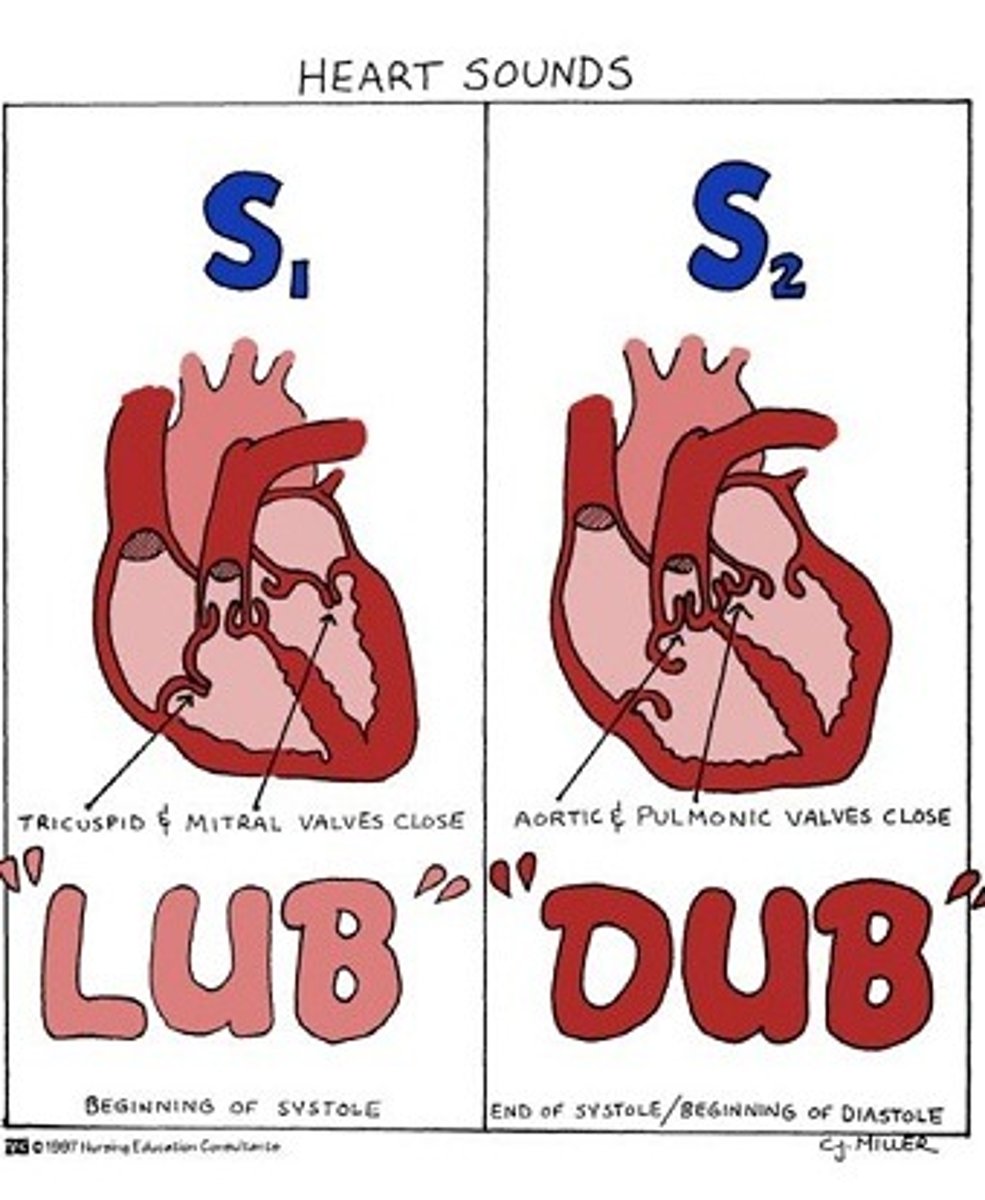
Know the major events of the cardiac cycle, including systole, diastole, and the heart sounds in detail
The cardiac cycle consists of atrial and ventricular systole followed by diastole, allowing for the coordinated filling and ejection of blood from the heart chambers. Heart sounds, particularly S1 and S2, correspond to the closure of heart valves and mark the beginning and end of systole. Additional heart sounds (S3 and S4) may indicate abnormal conditions and provide diagnostic information about heart function.
Know the electrical events of normal electrocardiogram. - P, QRS, T waves
The normal ECG reflects the electrical activity of the heart during one cardiac cycle. The P wave represents atrial depolarization, the QRS complex represents ventricular depolarization, and the T wave represents ventricular repolarization. Understanding these waves and intervals is crucial for interpreting ECGs and diagnosing various cardiac conditions.
Know the cardiac output and factors affecting cardiac output.
Cardiac output is determined by the heart rate and stroke volume, which are influenced by various factors including autonomic nervous system activity, venous return, blood volume, and hormonal factors. Understanding these factors is essential for evaluating cardiovascular function and diagnosing and managing cardiovascular diseases.
autonomic activity on heart function
The autonomic nervous system plays a vital role in regulating heart function. Sympathetic activation increases heart rate, contractility, and vascular tone, while parasympathetic activation decreases heart rate. The balance between sympathetic and parasympathetic activity is crucial for maintaining cardiovascular homeostasis and adapting to changing physiological demands.
ECG tracing, waves and what they represent
The ECG tracing consists of several waves and intervals that correspond to specific electrical events occurring in the heart during each cardiac cycle. Understanding the morphology and significance of these waves is essential for interpreting ECGs and diagnosing various cardiac conditions.
Heart sounds and what causes them
lup
-caused by closing of the bicuspid and tricuspid valve
dup
-caused by closing of aortic and pulmonary valve
What is Tachycardia and Bradycardia
Tachycardia is when the heart rate is too high Bradycardia is when it's too low
The differences between the structure of arteries and veins. Layers of blood vessels.
Arteries and veins have distinct structural differences reflecting their roles in the circulatory system. Arteries have thicker walls, higher blood pressure, and no valves, while veins have thinner walls, lower blood pressure, and contain valves to aid in venous return.
Which hormones are involved in compensatory mechanism in hemorrhage., short term and long term regulation
Short-term regulation involves:
Epinephrine and norepinephrine increasing heart rate and vasoconstriction.
Vasopressin conserving water and causing vasoconstriction.
Renin-Angiotensin-Aldosterone System (RAAS) increasing blood volume and pressure.
Long-term regulation involves:
Erythropoietin stimulating red blood cell production.
Atrial natriuretic peptide (ANP) promoting vasodilation and sodium excretion.
Aldosterone retaining sodium and water in the kidneys.
Components of the lymphatic system.
-Fluid (lymph)
-Vessels that transport lymph
- Organs containing lymphoid tissues
The lymphatic system does not have a pump; the movement of fluids in this system occurs via the pressure gradient product by skeletal muscle action, respiratory movement and contraction of smooth muscle in the vessel walls
Anaphylaxis
Severe allergic reaction
AIDS - which cells are affected
HIV attacks and destroys the CD4 cells (CD4 T lymphocyte) of the immune system. CD4 cells are a type of white blood cell that play a major role in protecting the body from infection.
Parts of the upper and lower respiratory tracts.
pic
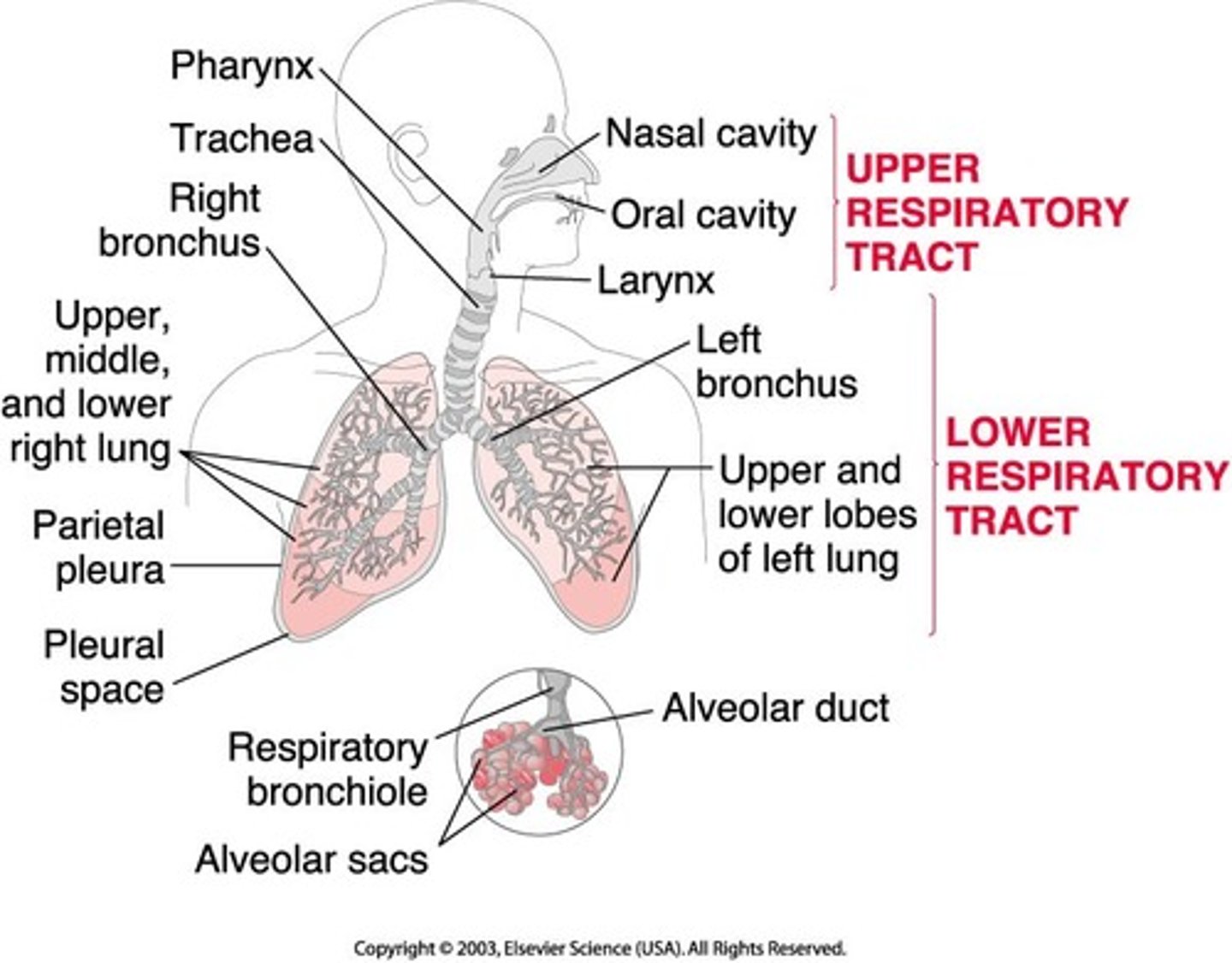
Larynx, its major cartilages and the functions of the larynx
The larynx, also known as the voice box, is a cartilaginous organ in the front of the neck that is part of the respiratory tract. It has several functions, including:
Protecting the lower respiratory tract: The larynx prevents food from entering the trachea while breathing.
Producing sound: The larynx contains the vocal cords, which manipulate pitch and volume.
Regulating thoracic pressure: The larynx helps regulate pressure in the chest.
Cough reflex: The larynx is involved in the cough reflex
Ventilation
movement of air in and out of the lungs
the mechanics of inspiration and expiration
volume changes during ventilation, rely on skeletal muscle of thoracic cavity; lungs cannot change their volume on their own
Muscles involved in Eupnea and hyperpnea.
In eupnea, the primary muscles involved in breathing include the diaphragm, external intercostal muscles, and accessory muscles like the internal intercostal muscles and the abdominal muscles.
During hyperpnea, additional muscles may become involved to increase the depth and rate of breathing. These may include the sternocleidomastoid muscles, scalene muscles, and the pectoralis minor muscles, which help elevate the rib cage further and increase lung volume.
Know the relationship between hemoglobin saturation and pH
Hemoglobin is the protein in red blood cells responsible for transporting oxygen from the lungs to tissues throughout the body. Its affinity for oxygen is influenced by several factors, including pH.
Secretions of cells of gastric glands - chief cells , parietal cells and mucous neck cells
-Chief cells secrete pepsinogen, which is converted to pepsin, aiding in protein digestion.
-Parietal cells produce hydrochloric acid, creating an acidic environment necessary for pepsin activation, and intrinsic factor, essential for vitamin B12 absorption.
-Mucous neck cells secrete mucus and bicarbonate ions, providing a protective layer over the stomach lining and neutralizing acid to prevent self-digestion.
Major secretions of Pancreas and Liver and their actions.
Pancreatic Juice:Enzymes: Pancreatic juice contains several digestive enzymes:Amylase: Breaks down carbohydrates (starches) into smaller sugars like maltose and glucose.Lipase: Digests fats (triglycerides) into fatty acids and monoglycerides.Proteases (e.g., trypsin, chymotrypsin): Break down proteins into peptides and amino acids.Bicarbonate: Pancreatic juice is rich in bicarbonate ions, which neutralize the acidic chyme from the stomach, creating an optimal pH environment for pancreatic enzyme activity in the small intestine.
Liver:
Bile:Bile Salts: Bile salts aid in emulsification, breaking down large fat globules into smaller droplets, which increases the surface area for lipase activity, facilitating fat digestion.Bilirubin: A waste product of red blood cell breakdown, bilirubin gives bile its characteristic yellow-green color. It is eventually excreted in feces.Cholesterol: Bile also contains cholesterol, which is necessary for the formation of bile acids, but excess cholesterol can contribute to gallstone formation.Bile Pigments: Apart from bilirubin, bile contains other pigments like biliverdin, which are byproducts of hemoglobin breakdown.
Functions of different enzymes found in the intestines.
Amylase: Breaks down carbohydrates into simpler sugars.
Lipase: Digests fats into fatty acids and monoglycerides.
Proteases: Break down proteins into peptides and amino acids.
Peptidases: Further break down peptides into individual amino acids.
Sucrase, Lactase, Maltase: Break down disaccharides into monosaccharides.
Nucleases: Break down nucleic acids into nucleotides.
Know what is HDL and LDL and their role
HDL and LDL are lipoproteins involved in cholesterol transport in the bloodstream. HDL plays a protective role by removing excess cholesterol from peripheral tissues and transporting it to the liver for excretion, while LDL transports cholesterol to peripheral tissues, where it can contribute to the formation of arterial plaque when levels are elevated.
Know the basic steps of cellular respiration
cellular respiration is a multi-step process that begins with glycolysis in the cytoplasm and is completed through the citric acid cycle and oxidative phosphorylation in the mitochondria. It involves the sequential breakdown of glucose and other organic molecules to produce ATP, NADH, and FADH2, ultimately generating the energy needed for cellular activities.
Why protein catabolism is not preferred source of energy
the body typically prioritizes carbohydrates and fats for energy due to their greater energy efficiency and the preservation of vital protein functions. Ensuring an adequate intake of carbohydrates and fats in the diet helps spare protein from being used as a primary energy source, preserving muscle mass and supporting overall health.
Know the parts of Juxtaglomerular apparatus and the functions
the macula densa, juxtaglomerular cells, and extraglomerular mesangial cells. The macula densa monitors tubular fluid composition, signaling for changes in renal blood flow and glomerular filtration rate (GFR). Juxtaglomerular cells secrete renin in response to stimuli like decreased blood pressure, initiating the renin-angiotensin-aldosterone system (RAAS) to regulate blood pressure and fluid balance. Extraglomerular mesangial cells play a supportive role in blood flow regulation. Overall, the JGA is crucial for renal autoregulation, systemic blood pressure control, and electrolyte balance.
Know the significance of hormones ADH and aldosterone in the urinary functions
ADH and aldosterone are hormones that work together to regulate urinary functions and maintain proper fluid and electrolyte balance in the body. ADH controls water reabsorption in the kidneys, while aldosterone regulates sodium reabsorption and potassium excretion, both of which are essential for maintaining blood pressure and preventing dehydration.
Know the external and internal urethral sphincter and what controls them
the external urethral sphincter is under voluntary control and helps maintain urinary continence, while the internal urethral sphincter is under involuntary control and helps regulate the flow of urine from the bladder into the urethra. These sphincters are controlled by different parts of the nervous system and play complementary roles in the micturition process.
Normal constituents of urine and normal urine volume per day.
the average adult typically produces around 1 to 2 liters of urine per day. This volume helps to eliminate waste products from the body and maintain proper hydration levels.
-
Water: The main component of urine, typically comprising around 95% of its volume.
Electrolytes: These include ions such as sodium, potassium, chloride, and bicarbonate, which are essential for maintaining electrolyte balance in the body.
Urea: A waste product formed from the breakdown of proteins in the liver, urea is the primary nitrogenous waste excreted in urine.
Creatinine: A waste product generated from the breakdown of creatine phosphate in muscle metabolism, creatinine is excreted by the kidneys at a relatively constant rate.
Uric acid: Another nitrogenous waste product resulting from the breakdown of nucleotides, uric acid is excreted in urine.
Ammonia: Formed from the breakdown of proteins and amino acids, ammonia is excreted in small amounts in urine.
Other waste products: These may include bilirubin, which is a breakdown product of heme from aged red blood cells, and small amounts of various hormones, drugs, and metabolites.
How is blood pH maintained? Know the major buffers
This is achieved through the coordination of buffer systems, such as bicarbonate, protein, and phosphate buffers, which resist changes in pH by absorbing or releasing hydrogen ions. The respiratory system regulates pH by adjusting carbon dioxide levels, while the renal system excretes excess acids or bases. Together, these mechanisms maintain blood pH within a narrow range, ensuring proper bodily function.
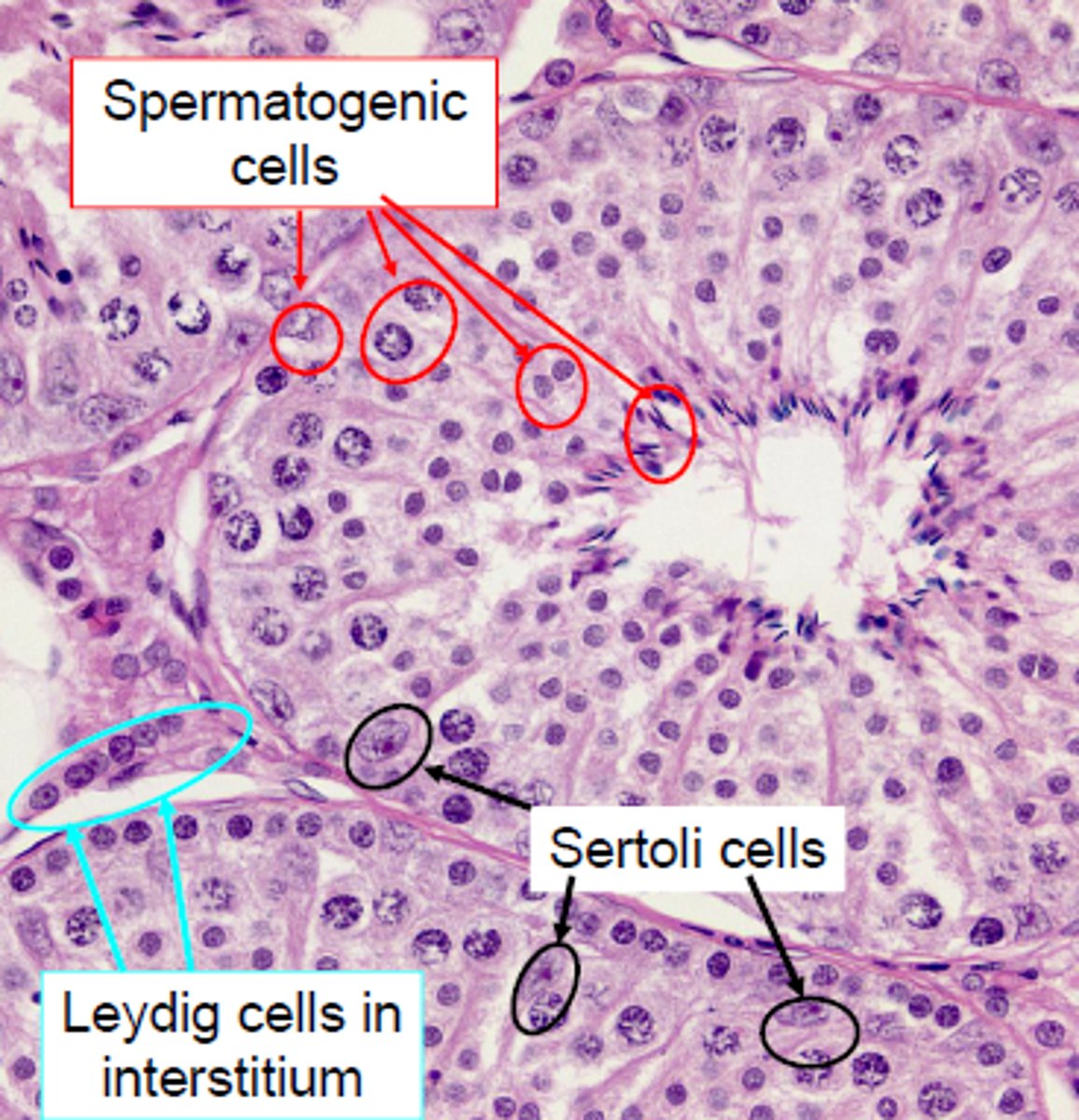
Know the cells producing testosterone
Leydig cells, interstitial cells
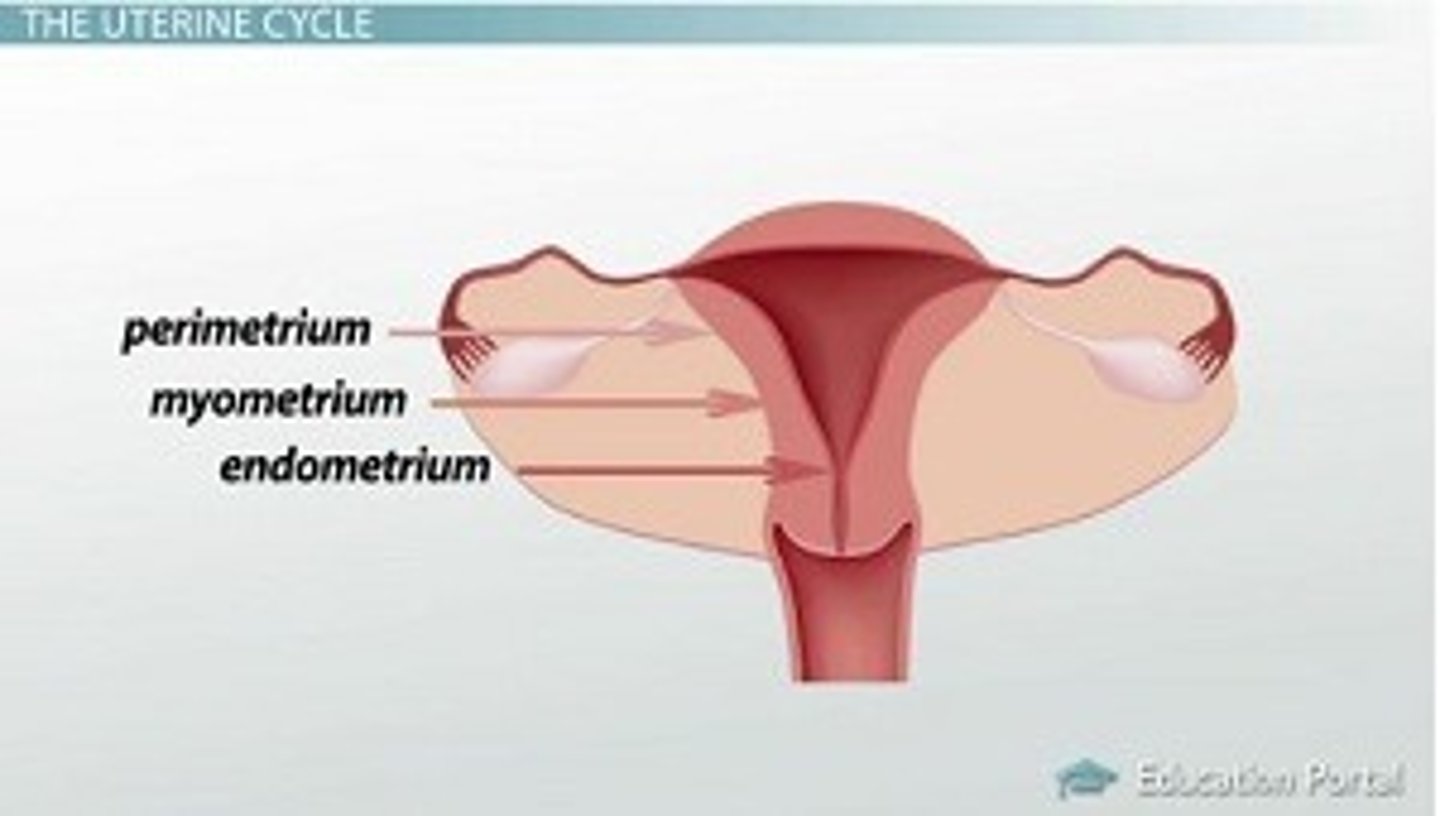
Layers of uterus.
perimetrium, myometrium, endometrium
Functions of FSH, LH, GnRH, estrogens and progesterone in females
Follicle-Stimulating Hormone (FSH) stimulates ovarian follicle growth and estrogen production, while Luteinizing Hormone (LH) triggers ovulation and promotes the formation of the corpus luteum, which produces progesterone. Gonadotropin-Releasing Hormone (GnRH) from the hypothalamus controls FSH and LH release. Estrogens are vital for secondary sexual characteristics and menstrual cycle regulation, while progesterone prepares the uterus for potential pregnancy. These hormones work harmoniously to regulate the menstrual cycle, ovulation, and reproductive processes.
Know the phases of menstrual cycle and the major events in each phase
Menstrual
The lining of the uterus sheds, which can last 3 to 5 days.
Follicular
The level of estrogen rises, which causes the lining of the uterus to thicken. This phase usually lasts 10-22 days, but this can vary from cycle-to-cycle.
Ovulation
A sudden increase in luteinizing hormone (LH) causes your ovary to release an egg, which can be fertilized by a man's sperm if present. This phase usually lasts 16 to 32 hours.
Luteal
The level of progesterone rises to help prepare your uterine lining for pregnancy. This phase lasts about 14 days.
three stages of labor - dilation, expulsion and placental
Stage 1: Dilation: This stage begins with the onset of regular uterine contractions and ends when the cervix is fully dilated to around 10 centimeter
Stage 2: Expulsion: This stage begins when the cervix is fully dilated and ends with the birth of the baby.
Stage 3: Placental: After the baby is born, the uterus continues to contract to expel the placenta (afterbirth) and the remaining membranes from the uterine wall.