WEEK 4 - CARDIOVASCUALR CONDITIONS
1/22
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
23 Terms
Identify the main areas in the body that ischemia can occur and describe the associated signs & symptoms
A condition where the blood supply to an organ or tissue is restricted, typically due to narrowed or blocked blood vessels. This results in a lack of oxygen (hypoxia) and essential nutrients, leading to tissue damage.
Ischemia in the heart is called MYOCARDIAL ISCHEMIA with S/S of: angina, arrhythmias, dyspnoea and radiation of pain to other body parts.
Ischemia in the brain is called STROKE with S/S of: face drooping, arm weakness, speech difficulty
ischemia in the renal system called RENAL ISCHEMIA with S/S of: acute kidney injury, oliguria (decreased) or Anuria (absent) of urine.
Ischemia in the limbs is called the peripheral arterial disease with S/S of: pain, cramping, skin changes (cyanotic, purple)
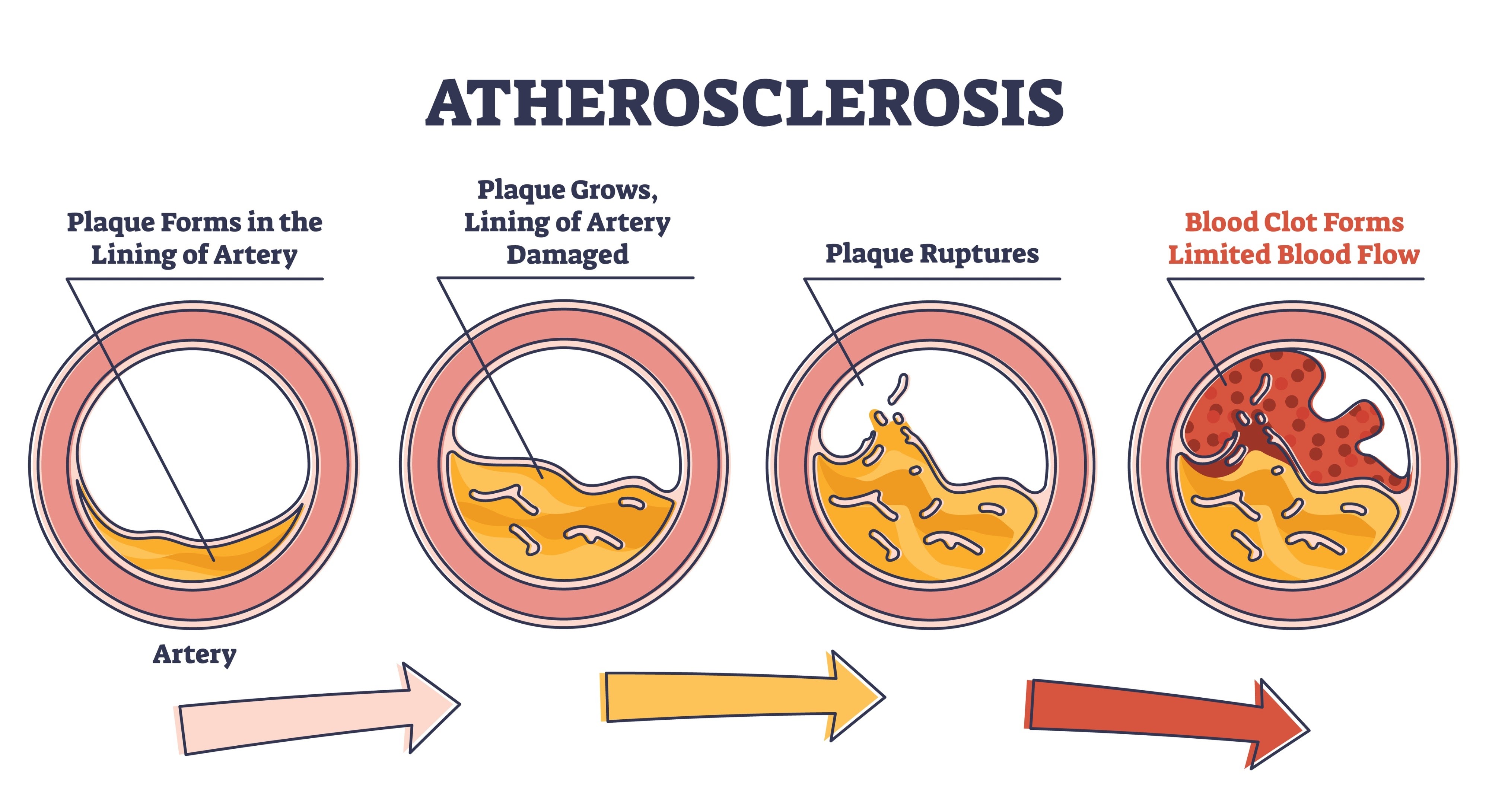
Explain the pathophysiology of atherosclerosis.
It is the progressive thickening and narrowing of an artery wall due to the accumulation of fatty substances, such as high cholesterol, smoking, and high blood sugar.
Atherosclerosis is the leading cause of many diseases, like cardiac arrest, stroke,and peripheral vascular disease
Identify the relevant nursing assessments and management of a patient with peripheral artery disease
Pain AX
skin Ax
Neurovascular obs
Ensure there’s enough O2 supply
encourage circulation and perfusion - walking, warmth, avoid constriction
IV fluids
Medication administration - antiplatelets (reduce chances of blood clot), statins (reduce hyperlipidemia)
high or semi-Fowler’s position
monitoring obs
Identify and describe the varying causes of stroke
STROKE - BLOOD SUPPLY TO THE BRAIN IS BLOCKED OR REDUCED BY:
ISCHEMIC STROKE (blockage) - most common, when a blood vessel supplying the brain is narrowed or blocked, cutting off oxygen and nutrient supply. It can be due to a thrombotic (blood clot), or an Embolic (a mobile blood clot or a piece of plaque)
HAEMORRHAGE STROKE (bleeding) - a blood vessel in the brain leaks or ruptures —> blood spills into the brain tissue or the surrounding areas. The pooling of blood creates pressure that damages brain cells. It can be due to intracerebral (within the brain tissue) or subarachnoid (the area between the brain and the tissue that covers it).
TRANSIENT ISCHEMIC ATTACK OR TIA (‘mini-stroke’) - temporary blockage of blood flow (ischemia) to the brain, similar to an ischemic stroke.
Identify the non-modifiable or modifiable risk factors associated with stroke
MODIFIABLE - atherosclerosis risk factors including: hypertension, atrial fibrillation, diabetes, smoking, and hyperlipidemia, sedentary lifestyle
NON-MODIFIABLE - Age, family history/ genetics, race/ethnicity, gender, prior stroke or TIA
Discuss angina and myocardial infarction in relation to Acute Coronary Syndrome.
BOTH ANGINA AND MYOCARDIAL INFARCTION ARE CONDITIONS THAT FALL UNDER THE UMBRELLA TERM ACUTE CORONARY SYNDROME.
UNSTABLE AGINA (UA): when there’s a significant yet incomplete blockage of a coronary artery. The blood flow is restricted but not cut off completely = the heart muscles is inured but does not die.
MYOCARDIAL INFARCTION (“HEART ATTACK”): occurs when ischemia (thrombus) is severe enough and prolonged enough to cause irreversible necrosis of the heart muscle cell.
Angina (specifically Unstable Angina) is a warning sign of ACS where the heart is starved of oxygen but survives. Myocardial Infarction is the progression of ACS, where the heart tissue actually dies due to the severity and duration of the ischemia.
What is the difference between STEMI and NSTEMI?
NSTEMI - partial blockage or intermittent occlusion, NO ST elevation, causes necrosis of the innermost layer of the heart.
STEMI - Complete or sustained blockage of the coronary artery, ST elevation shows on ECG, causes full-thickness (transmural) necrosis of the heart.
Compare and contrast the nursing management of a patient experiencing unstable angina vs ST elevation myocardial infarction (STEMI)
UNSTABLE ANGINA:
vitals signs, pain Ax, ECG, cardiac Ax (inspection, palpation, auscultation)
Pain management - Nitrates
ongoing monitoring - ECG, Vitals, Cardiac enzymes
Medications - antiplatelet (aspirin), beta blocker 1 (metoprolol), statins (atorvastatin).
interventions - telemetry, possible coronary angiograph, lifestyle changes (diet, exercise)
MI (STEMI):
initial Ax - rapid ax, 12-lead ECG, IV access, labs, O2 administration
Pain management - morphine, nitrates, O2 if hypoxia
Ongoing monitoring - ECG, O2 stats, Vitals, Troponin levels, rhythm checks.
medications - antiplatelet and thrombolysis (dissolves dangerous blood clot with clot-busting drugs) or primary PCI (percutaneous coronary intervention) urgently.
intervention - immediate reperfusion (PCI or thrombolysis) or ICU care.
Explain three (3) key education points that you would discuss with a person to reduce their risk of acute coronary syndrome
LIEFESTYLE MODIFICATIONS:
quit smoking, reduce alcohol consumption, reduce saturated fatty foods, engage in regular exercise
MEDICATION ADHERENCE:
Emphasise the importance of taking prescribed meds (anti-hypertensives, statins, antiplatelets) on time.
RECOGNISE SYMPTOMS EARLY ON:
educate on the warning signs of ACS (e.g, chest pain, SOB, sweating excessively, nausea) and the importance of seeking help when these symptoms initially begin.
A patient is admitted to hospital with an acute coronary syndrome. The nurse knows that this diagnosis indicates that the patient has experienced
unstable angina or a myocardial infarction
Describe the normal conduction pathway of the heart
SINOATRIAL (SA) NODE: The heart’s natural pacemaker.
located in the upper wall of the Right Atrium
initiates the electrical impulse at the rate of 60 to 100 beat per min.
cause both left and right atria to contract (atrial systole)—→ means pushing blood into ventricles
ATRIOVENTRICULAR (AV) NODE: The gatekeeper.
located at the lower part of interatrial septum above the tricuspid valve.
Delays electrical impulse (~0.1 sec) to allow ventricles time to fill completely.
It’s the heart’s backup peacemaker - which can generate (40 -60 bpm) if SA node fails.
BUNDLE OF HIS (ATRIVENTRICULAR BUNDLE): Main pathway for impulse to reach ventricles
passes through the fibrous skeleton connecting the atria and ventricles
the impulse exists the AV node and travels down the bundle of his to reach the ventricles.
RIGHT AND LEFT BUNDLE BRANCHES: The split of bundle of his —> either left or right bundle branches which is along the interventricular septum
carry the impulse towards the Apex of the heart, delivering it to both ventricles.
PURKINJE FIBERS:
spread throughout the ventricular walls.
rapidly transmit the impulse to the ventricular muscles causing coordinated contraction from the Apex upwards to the pulmonary artery and aorta.
Explain the cardiac conduction system in relation to an ECG
P WAVE (ATRIAL DEPOLARISATION): originates from SA node and spreads through both atria —→ causing the atria to contract.
PR INTERVAL (AV NODAL DELAY): The impulse reaches the AV node and is deliberately delayed before the ventricles are activated.
QRS COMPLEX (VENTRICULAR DEPOLARISATION): The impulse travels the bundle branches and the Purkinje fibres —→ causing electrical activation (depolarisation) of the ventricles, causing them to contract.
T WAVE (VENTRICULAR REPOLARISATION): Ventricular cells are returning to their resting electrical state (repolarisation) —→ preparing for the next impulse.
ST SEGMENT: the time between the end of ventricular depolarisation and the start of ventricular repolarisation

WHAT IS THIS ECG READING?
Atrial fibrillation (AF) usually The atria not contracting effectively instead they fibrillate or quiver
Rhythm: irregularly irregular (no consistent R-R interval).
P wave: absent
PR interval: not measurable
QRS complex: normal, unless there’s a conduction delay.
Rate: depends if controlled AFib (< 100bpm), uncontrolled or rapid ventricular rate (RVR) is (>100bpm).

WHAT IS THIS ECG READING?
VENTRICULAR TACHCARDIA: electrical impulses spread abnormally and slowly through the ventricular muscle —→ ineffective atrial contraction and poor ventricular filling. highly dangerous if sustained.
rhythm: regular
Rate: 100 - 250 bmp
P wave: usually absent or not related to QRS (AV dissociated)
QRS complex: Wide (>0.12 sec) and bizarre in shape
T wave: often opposite direction to QRS
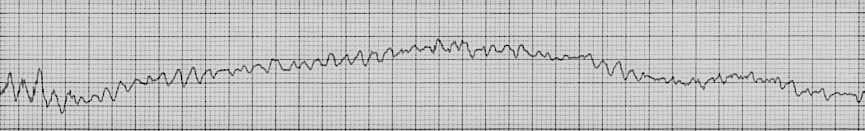
WHAT IS THIS ECG READING?
VENTRICULAR FIBRILLATION (VF): multiple chaotic and disorganized electrical impulses arising from the ventricular muscle fiber.
Rhythm: chaotic, disorganized - no identifiable rhythm
Rate: not measurable
P wave: Absent
QRS complex: absent, replaced by irregular, rapid fibrillatory waves
T wave: not identifiable
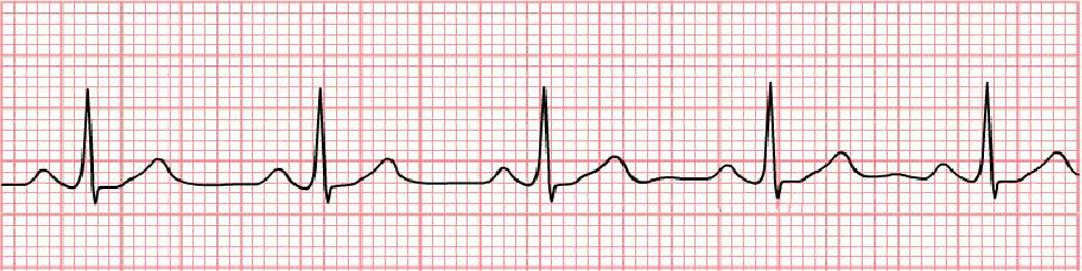
WHAT IS THIS ECG READING?
NORMAL SINUS RHYTHM:
Rhythm: regular
rate: 60 100 bpm
P wave: present
QRS complex: normal or present
T wave: identifiable
WHAT ARE THE SHOCKABLE RHYTHMS?
Ventricular fibrillation (VF)
pulseless ventricular tachycardia (VT)
What is the main indication for performing 12 lead ECG?
baseline history of pt’s heart rhythm
patient complaining of chest pain
irregular heart rate - either too low or two high
pre-surgery
Pm history or Fm history of heart complications
Serial ECG - for consistent monitoring
electrolyte imbalance
Identify the key risks associated with a 12 lead ECG?
Interferences:
sweat
hair
metal contact
movement
allergic to the lead sticky tape
What are the nursing Ax or interventions for performing an ECG?
Patient privacy
Spine position
explanation of privacy
reassurance
encourage little to no movement
What is the role of telemetry monitoring?
used to continuously observe vital signs especially in critical care or cardiac units
enables early interventions —> hence rapid response to life - threatening changes.
What’s the difference between an ECG and a continuous telemetry monitoring?
Both are cardiac monitoring
ECG provides a snapshot of the heart’s electrical activity at a specific time
Telemetry is an ongoing rea-time monitoring of the heart rate and rhythm
WHAT DOES DRSABCD STANDS FOR?
DANGER - environmental hazards (water or power cords) or manual handling
RESPONSE - Command them to say their name or squeeze your hands. or produce a painful stimuli like squeezing of the trapezius
SEND FOR HELP - emergency buzzer, ambulance 000
AIRWAY - make sure their airways is clear
BREATHING - look for the rise of chest or shoulders, listen or feel their breathing with your finger or cheek.
CPR/ CIRCULATION - chest compression rate is 100 -120 per min, depth would be more than 5 cm in adults or 1/3 depth of their chest. Chest compression ratio is 30 by 2.
DEFIBRILLATE - VF is the most common cause of adult cardiac arrest.