Radiographic Technique of the Femur, Knee, Tibia & Fibula
1/50
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
51 Terms
List the 2 main projections for imaging the Tibia & Fibula.
- Antero-posterior (AP)
- Lateral
What are appropriate clinical indications for plain radiography of the Tibia & Fibula?
- Trauma
- Pain
- ? Presence of disease
- Foreign bodies

What artefacts should be removed from the patient before imaging the Tibia & Fibula?
- jewellery e.g. ankle bracelets
- thick clothing e.g. trousers/jeans
- patient to put on a gown
When imaging the Tibia & Fibula, the image receptor should be placed ____________ .
DIAGONALLY (corner to corner)
When imaging the Tibia & Fibula, which two joints should always be included in the same image (especially in trauma)?
- ANKLE joint
- KNEE joint
In order to get both the ankle & knee joints within the field of view, what should we do when imaging the Tib/Fib?
Might need to increase SID distance to get both joints within field of view
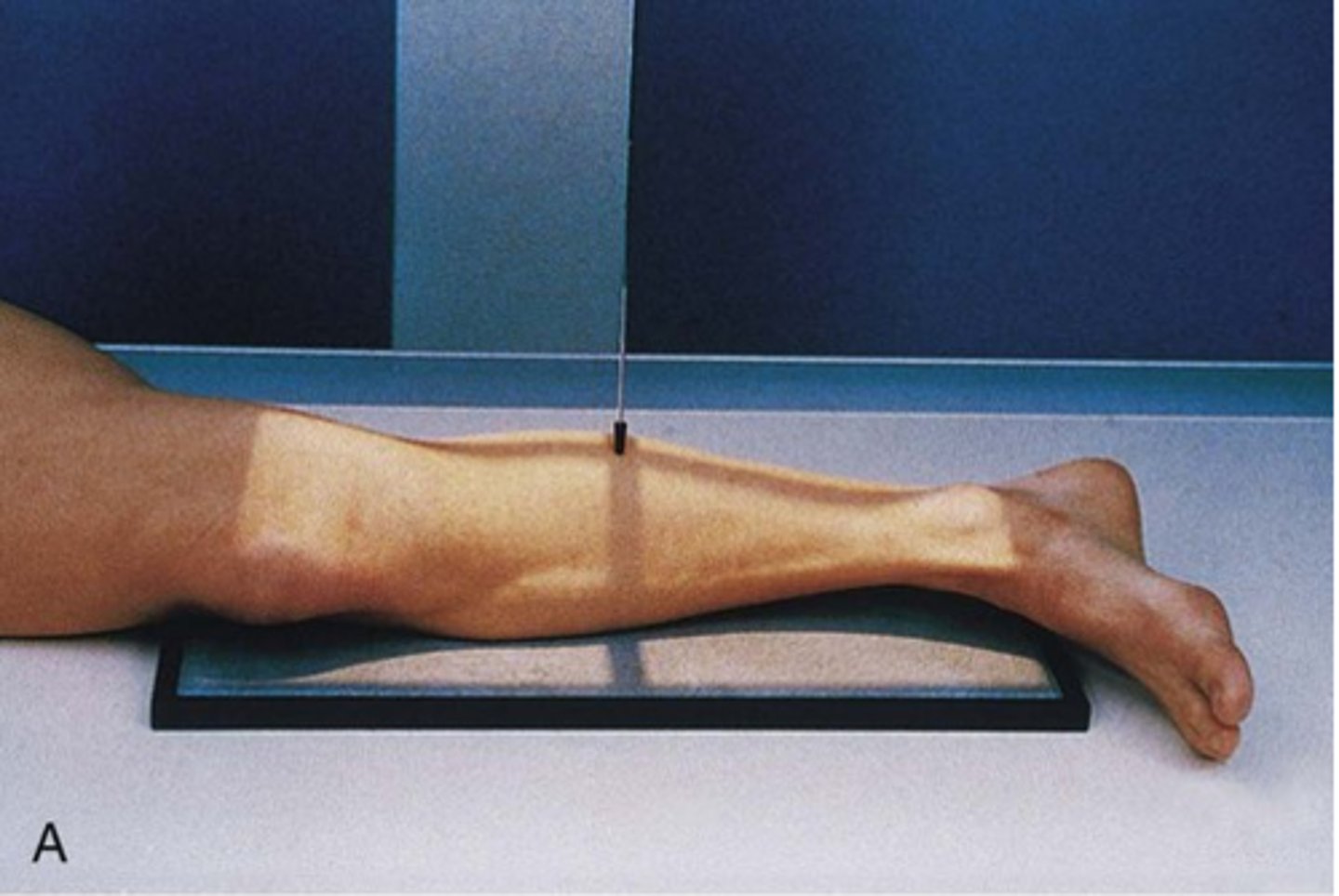
Describe, in detail, the positioning of the PATIENT for an AP TIBIA & FIBULA projection.
1. Patient sits upright or lies supine on the x-ray couch with the affected leg extended.
2. The posterior aspect of the affected leg should be in contact with the IR.
3. The limb is rotated medially until the medial and lateral malleoli are equidistant from the image detector. The condyles of the knees should also be equidistant to the image detector.
4. The ankle is also dorsi-flexed (toes pointing upwards) to open up the mortise joint.

How should we position the X-RAY TUBE for an AP projection of the TIBIA & FIBULA?
SID
Central ray
Centring point
SID: 100 - 115cm (115cm may be needed for patients with long legs)
Central ray: perpendicular to the IR
Centring point: in the midline of the limb, midway between the knee and ankle joint
How should we COLLIMATE when doing an AP projection of the TIBIA & FIBULA?
- to include the entire length of the tibia and fibula bones and lateral soft tissue borders. The knee and ankle joint must also be included.

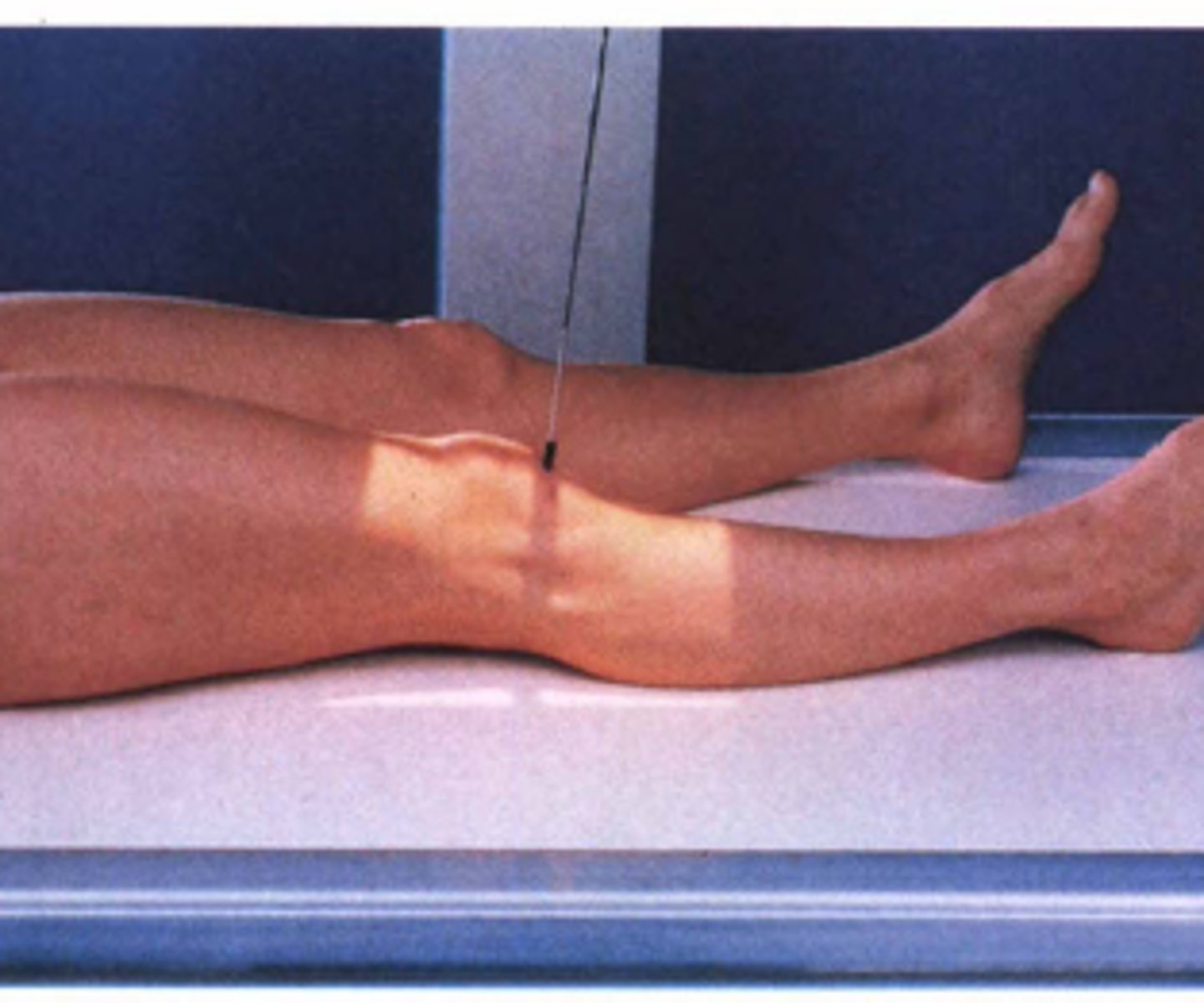
Describe, in detail, the positioning of the PATIENT for a LATERAL TIBIA & FIBULA projection.
1. From the AP position, the patient turns onto the affected side. Lateral aspect of the leg in contact with the IR.
2. The knee joint is flexed.
3. The malleoli should be superimposed (in practice the toes are slightly elevated). The condyles of the knee should also be superimposed.
4. The foot is dorsi-flexed (bringing the plantar aspect 90° to the image detector).
5. The long axis of the tibia should be parallel to the image detector.
How should we position the X-RAY TUBE for a LATERAL projection of the TIBIA & FIBULA?
SID
Central ray
Centring point
SID: 100 - 115cm
Central ray: perpendicular to the IR
Centring point: in the midline; midway between the knee and ankle joint
How should we COLLIMATE when doing a LATERAL projection of the TIBIA & FIBULA?
- to include the entire length of the tibia and fibula bones and lateral soft tissue borders. The knee and ankle joint must also be included.

How is radiation protection provided for the patient during radiography of the tib/fib?
▪ Positive patient identification
▪ Correct clinical indications
▪ Appropriate clinical indications
▪ Collimation
▪ ALARP
▪ Good accurate technique
What is a Maisonneuve fracture? Why is this important when imaging the Tib/Fib?
- Fracture at the medial malleolus with a fracture of the proximal fibula.
- It is important to ensure that all of the anatomy is included in the image so that both fractures can be viewed.
- If the patient's ankle joint is painful, ask the patient if they also have pain at the top of the fibula. This could mean that they have a possible maisonneuve fracture.

What is a spiral fracture? Why is it important when imaging the Tib/Fib?
- a fracture that twists around the shaft of the bone.
- The full extent of the fracture might not be realised without full-length imaging. This is why it is important to include all of the anatomy when imaging the tib/fib.

When imaging the Tib/Fib in trauma cases, a _____ projection might be used if the patient cannot rotate their leg.
HBL (horizontal beam lateral)
List the main projections for imaging the Knee.
- Antero-posterior (AP)
- Lateral
- Skyline
What are appropriate clinical indications for plain radiography of the knee?
- Trauma
- Pain
- Arthritis (Rheumatoid & Osteoarthritis)
How should the patient be prepared before taking their KNEE x-ray?
- removal of artefacts e.g. thick clothing such as trousers/jeans
- patient to put on a gown
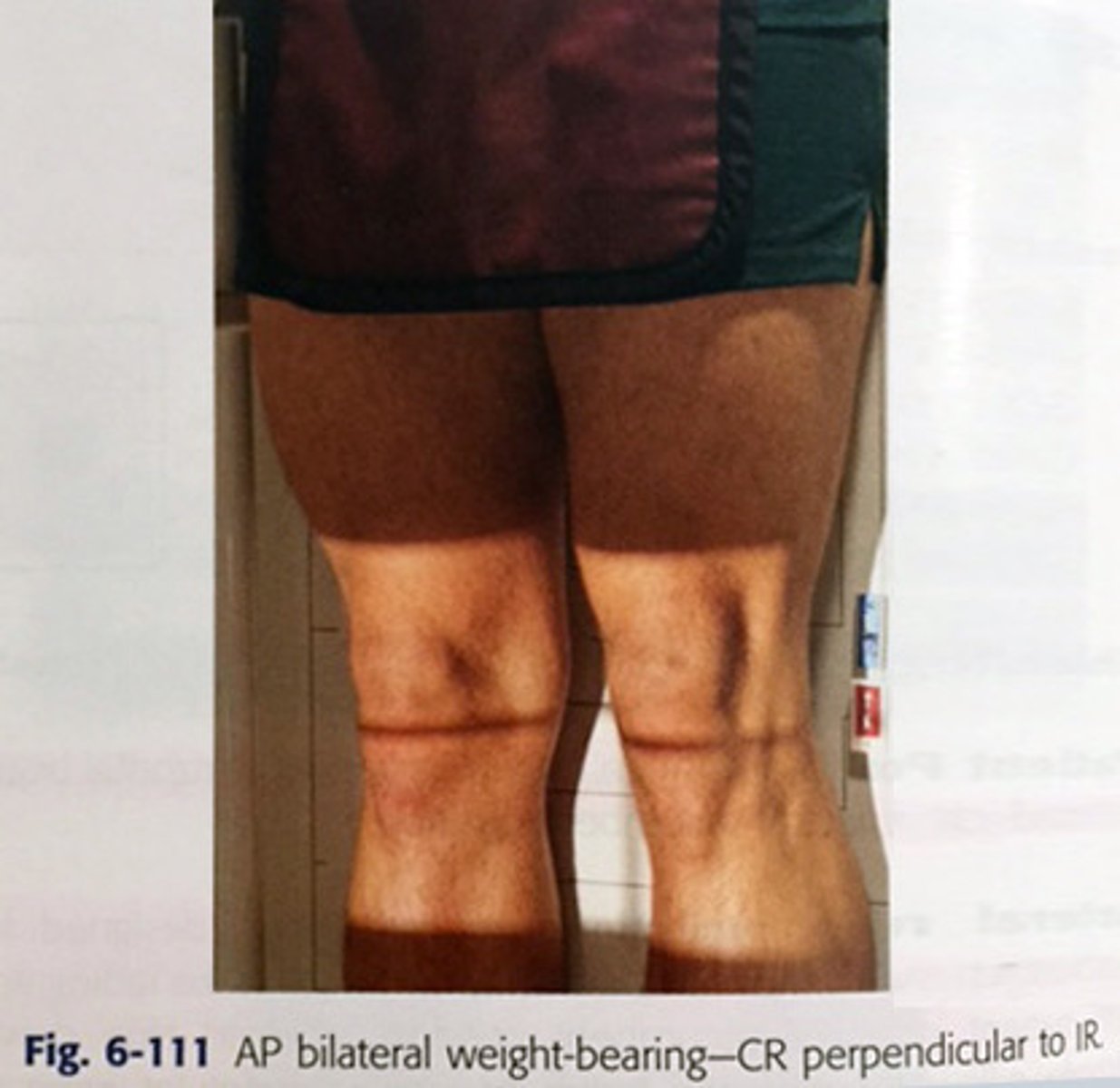
Describe, in detail, the positioning of the PATIENT for an AP KNEE WEIGHT-BEARING projection.
1. Patient stands with the posterior aspect of the knee joint in contact with the upright bucky (no grid required).
2. Patient's weight should be evenly distributed.
3. The lower leg is rotated until the patella is centralised and the femoral condyles equidistant to the IR.
4. Make sure that the patient's leg is fully extended and that they are standing up straight against the bucky.
Describe, in detail, the positioning of the PATIENT for an AP KNEE projection (ON THE X-RAY COUCH).
1. Patient lies supine or sits upright on the x-ray couch.
2. Legs extended with the posterior aspect of the affected knee joint in contact with the IR.
3. The lower leg is rotated until the patella is centralised and the femoral condyles should be equidistant to the IR.
4. Make sure the patient's feet are facing forwards; for some patients the toes may need to be turned inwards (but not always).
How should we position the X-RAY TUBE for an AP KNEE projection?
SID
Central ray
Centring point
SID: 100 - 115cm
Central ray: perpendicular to the IR.
Centring point: 2.5cm BELOW the apex of the patella.
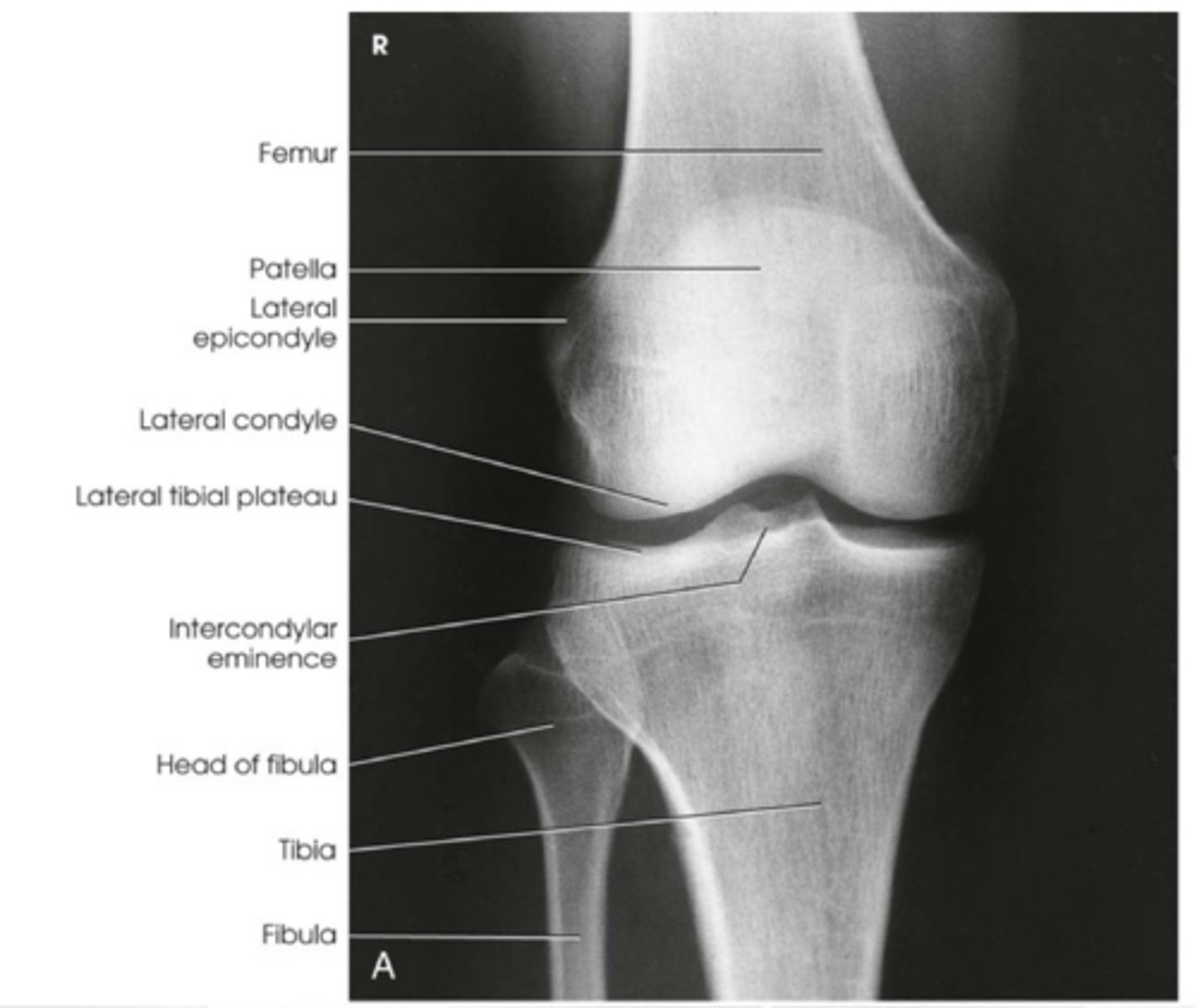
How should we COLLIMATE when doing an AP KNEE projection? What structures should be included in the image?
- to include: the knee joint, distal third of the femur, proximal third of the tibia and fibula and lateral soft tissue borders.
ALSO:
▪ Head of the fibula should be partially obscured by the tibia
▪ Shafts of the tibia and fibula should be separated
▪ Joint space should be clear
▪ Patella centralised
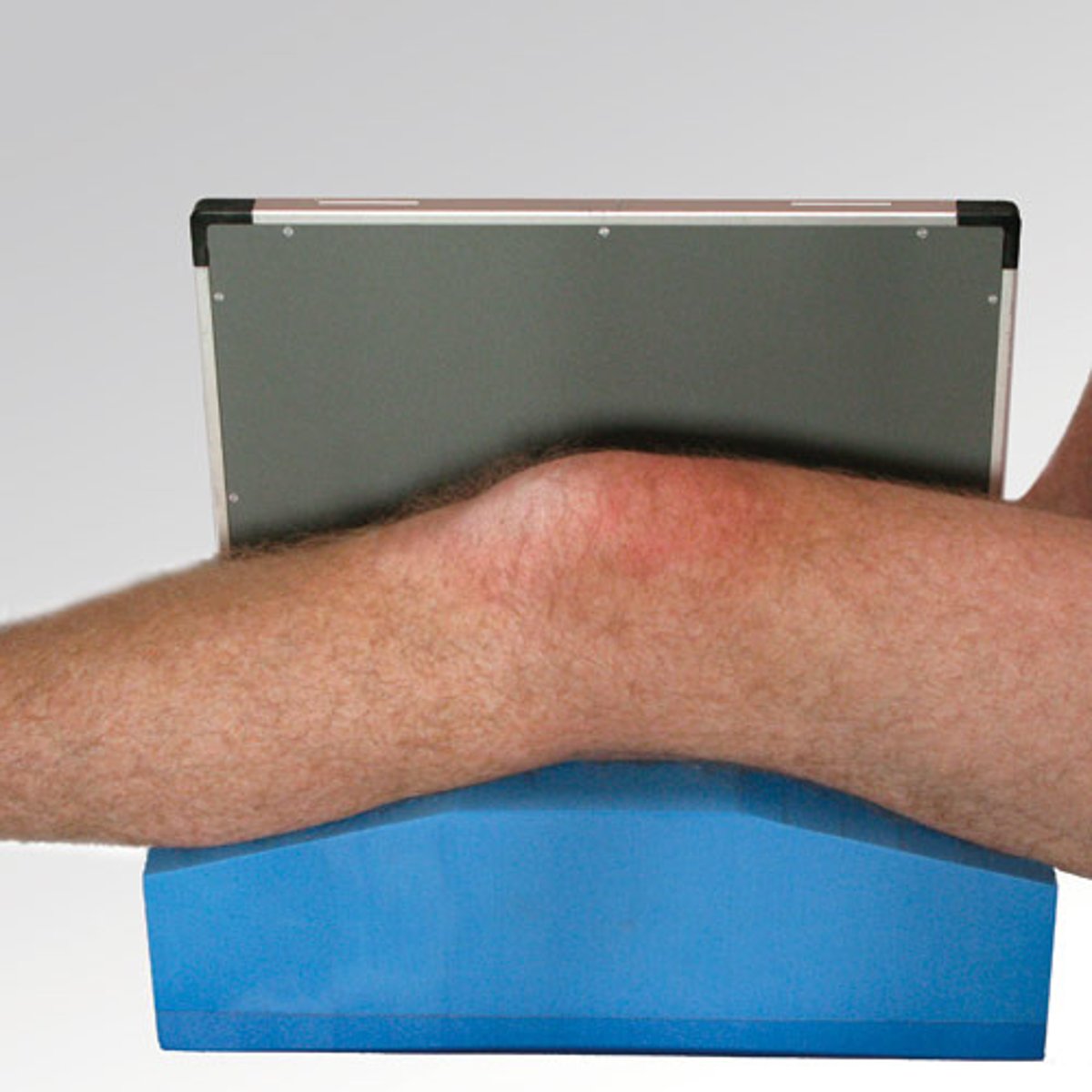
Describe, in detail, the positioning of the PATIENT when doing a supine LATERAL KNEE (non-trauma) (position 1)
1. Patient lies supine on the x-ray couch and turns onto the affected side so that the lateral aspect of the knee is in contact with the IR.
2. The affected knee is flexed through either 45 or 90 degrees and the leg is turned to superimpose the femoral condyles.
3. A small pad should be placed under the ankle joint to ensure the tibia is parallel to the x-ray couch.
Describe, in detail, the positioning of the PATIENT when doing a supine LATERAL KNEE (non-trauma) (position 2)
1. Patient lies on the affected side to be examined and the knee is flexed at either 45 or 90 degrees.
2. The unaffected leg is brought in front of the one being examined.
3. A small pad should be placed under the ankle joint to ensure the tibia is parallel to the x-ray couch.
4. The femoral condyles of the knee being examined should be superimposed.

Describe, in detail, the positioning of the PATIENT for a LATERAL WEIGHT-BEARING KNEE projection.
1. From AP position the patient is turned towards their affected side to bring lateral aspect of lower leg into contact with the erect IR holder / erect bucky
2. The affected knee is flexed (a lunge) and the leg is turned until the lateral and medial femoral condyles are superimposed.
How should we position the X-RAY TUBE for a LATERAL KNEE projection?
SID
Central ray
Centring point
SID: 100 - 110cm
Central ray: perpendicular to IR
Centring point: 2.5cm BELOW and BEHIND the apex of the patella.
How should we COLLIMATE when doing a LATERAL KNEE projection? What structures should be included in the image?
- to include the knee joint, distal third of the femur, proximal third of the tibia and fibula and lateral soft tissue borders.
ALSO:
▪ The femoral condyles should be superimposed
▪ The patella should be clear of the femur
▪ Patellofemoral joint space demonstrated
▪ Approx 1/3rd of the head of fibula superimposed over the tibia
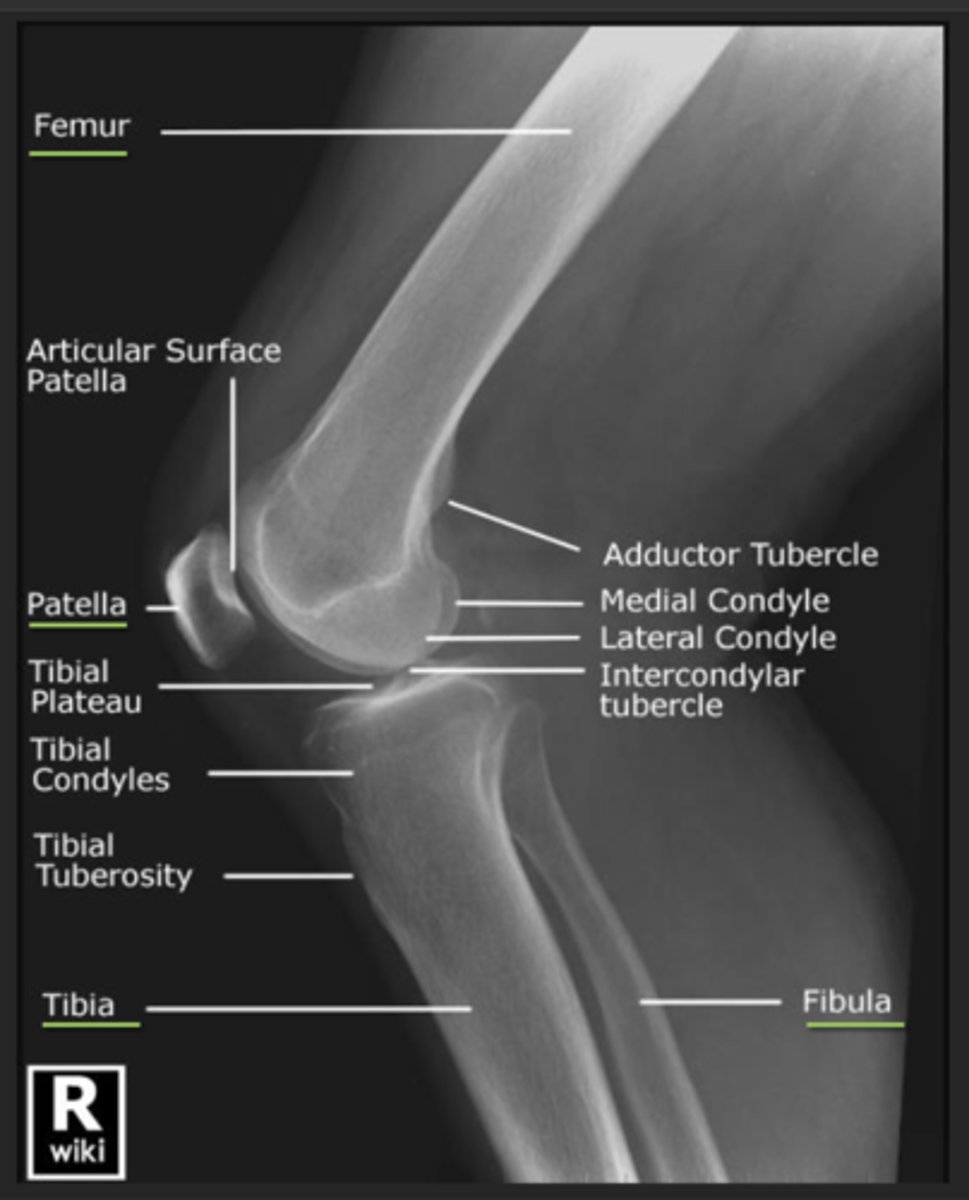
For a lateral knee projection, what else can sometimes be done to help superimpose the condyles?
- A 5 DEGREE CRANIAL ANGLE can sometimes help to superimpose the condyles.
When doing a lateral knee projection, how can you tell if there is OVER-ROTATION?
- fibula is projected too POSTERIOR.
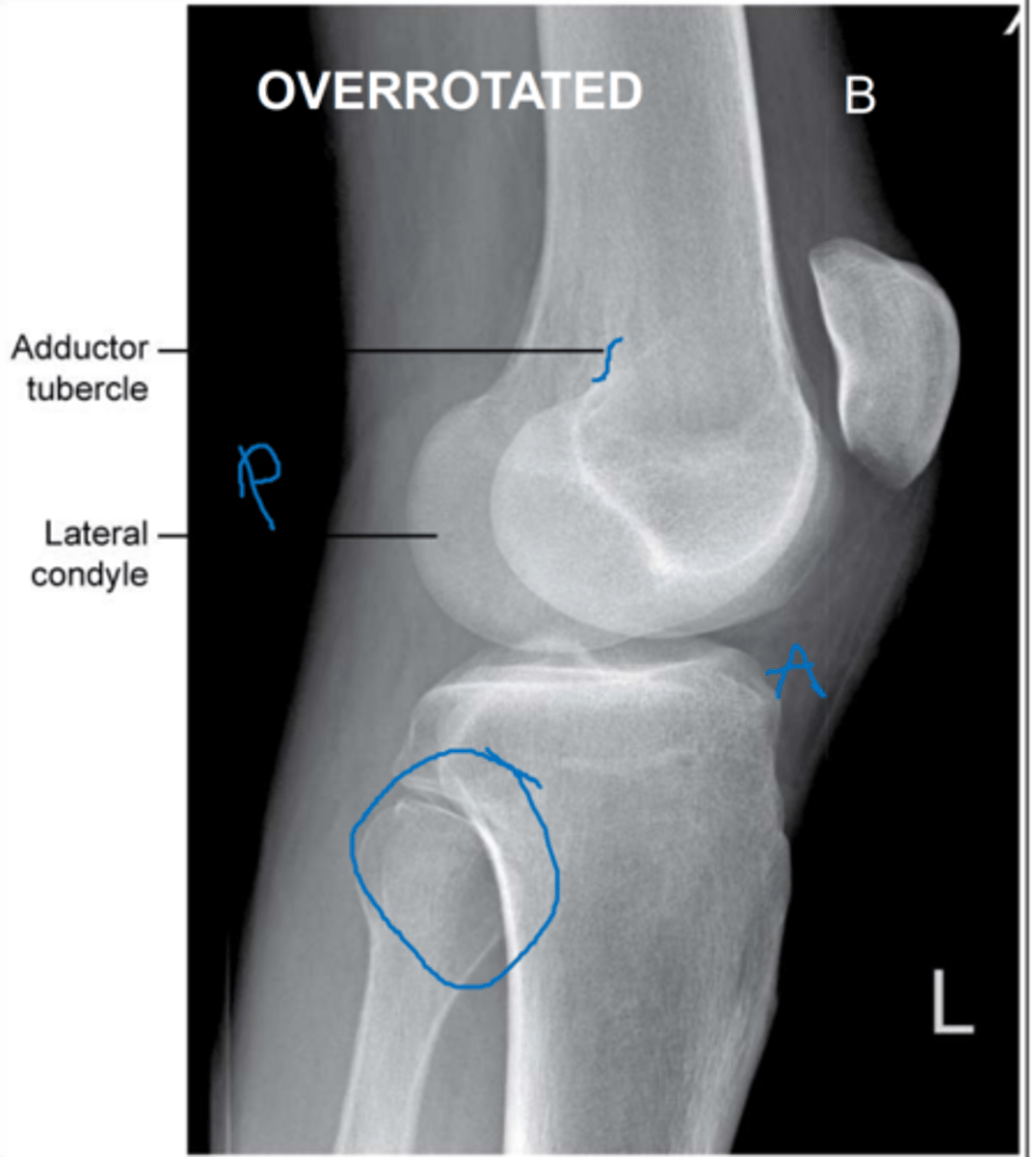
When doing a lateral knee projection, how can you tell if there is UNDER-ROTATION?
- fibula head is hidden behind the tibia
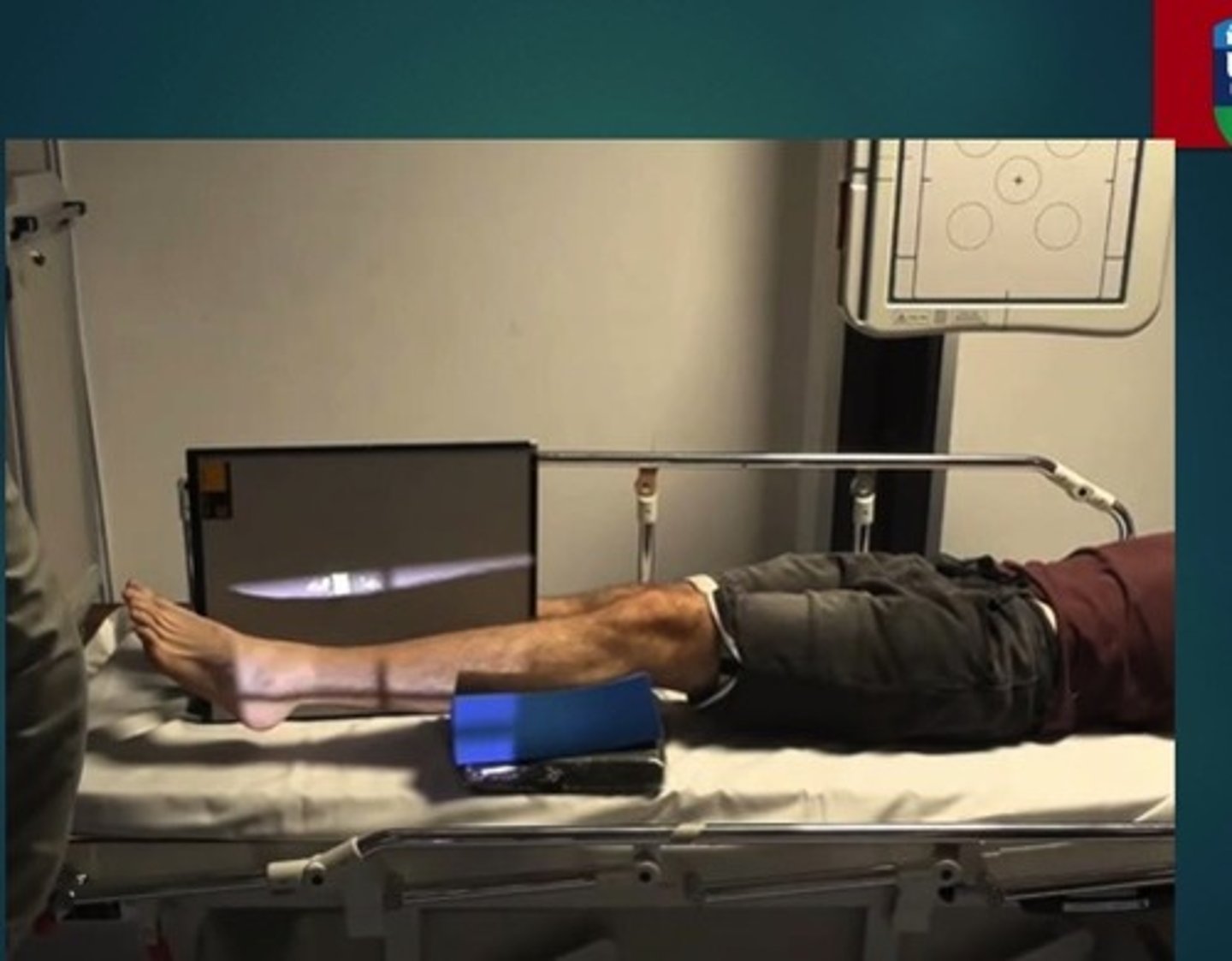
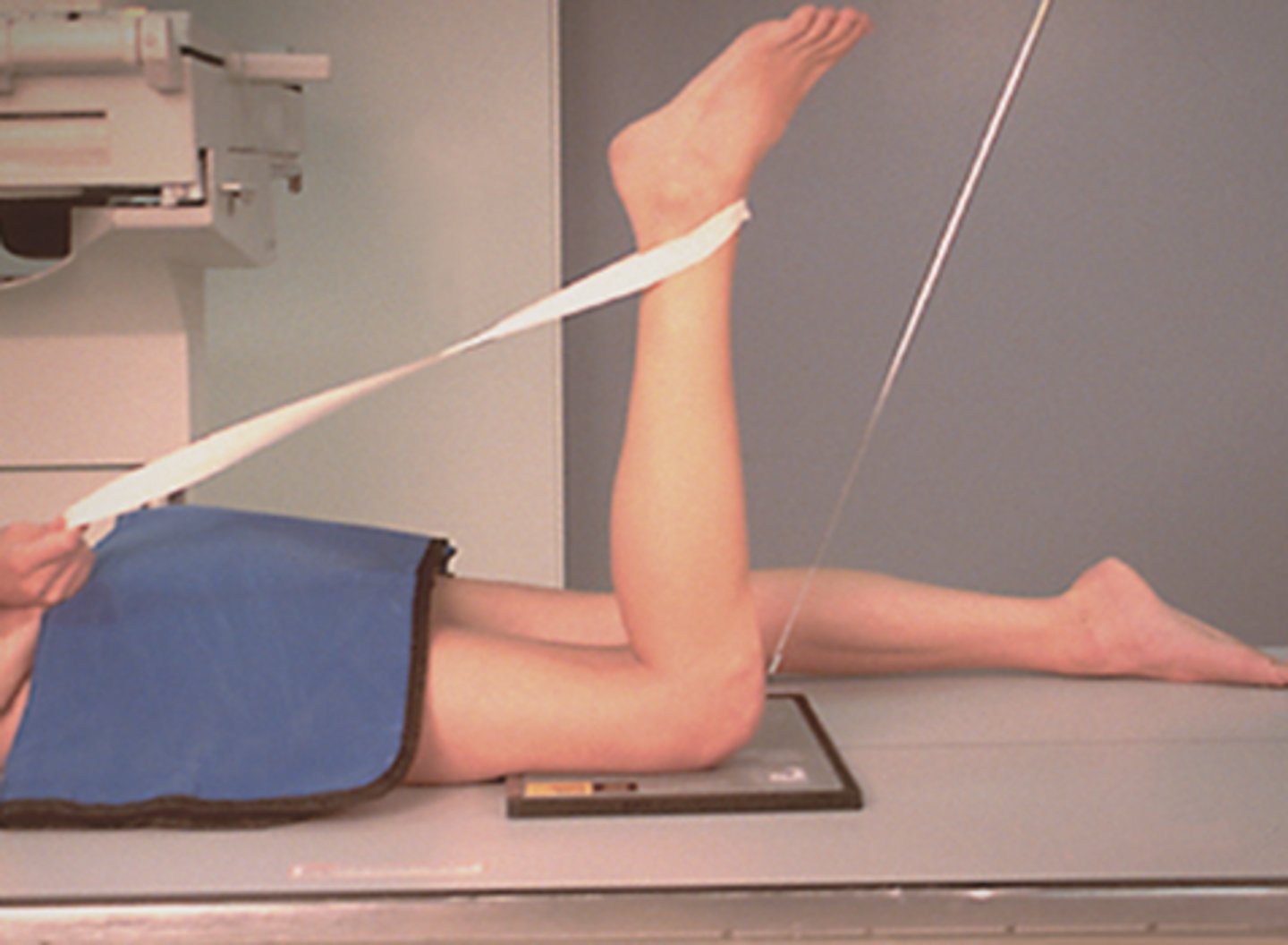
In which cases would you need to do a HBL projection of the KNEE?
- for TRAUMA patients; usually patients presented supine on a trolley.
- used to check for FRACTURES of the knee joint OR ruptured quadriceps tendon.
- may also be used to check for lipohaemarthrosis

When doing a HBL projection of the knee for trauma patients, why should the leg NOT be flexed at all?
- it could cause further damage in the knee joint & worsen the pain.
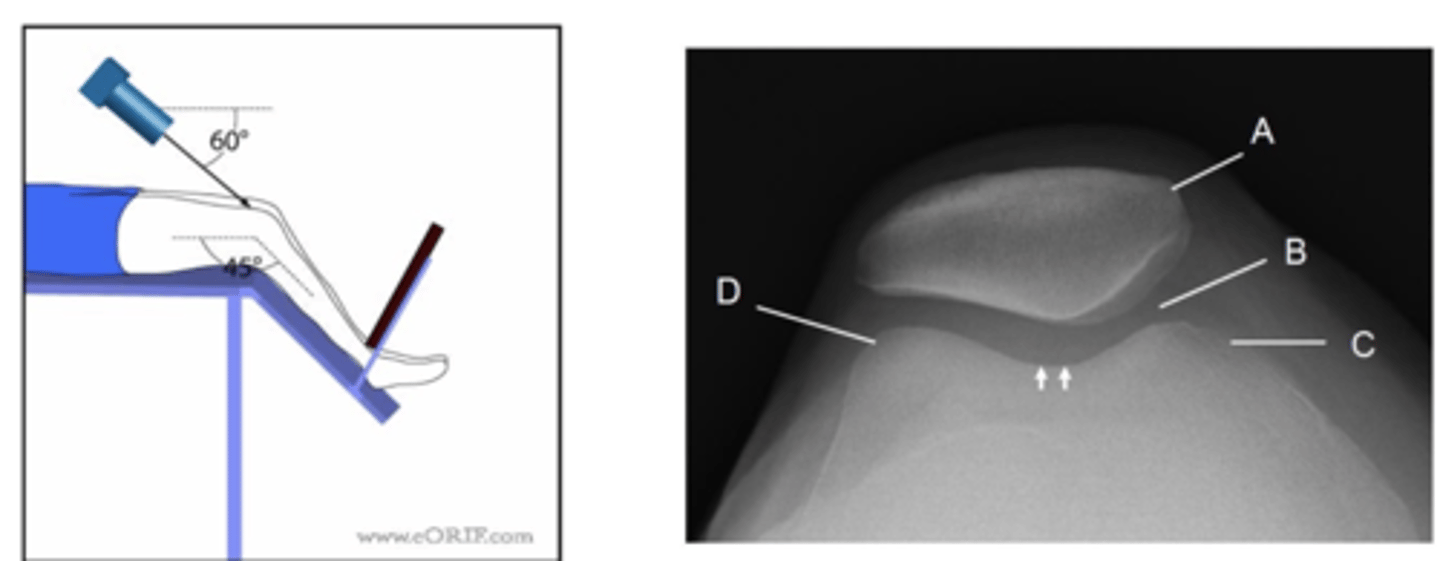
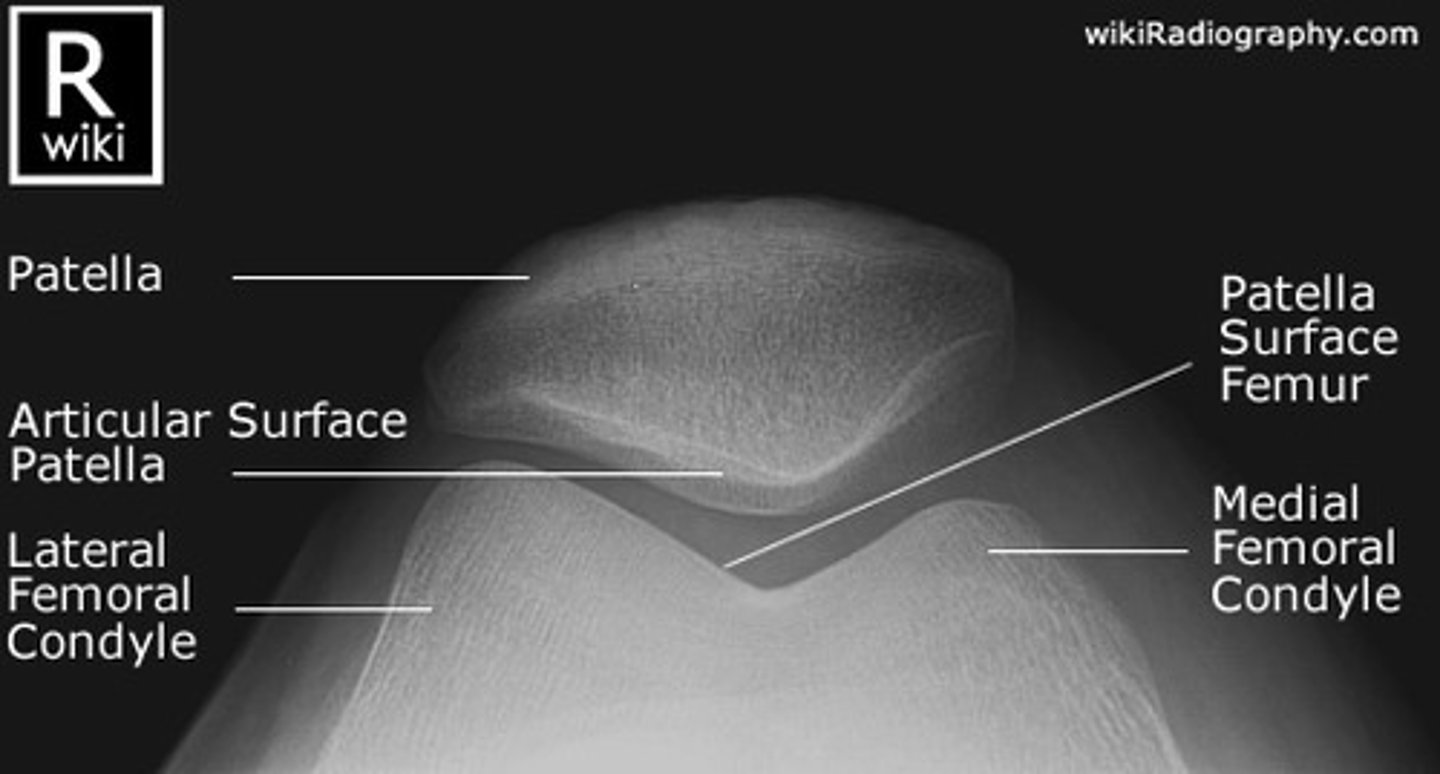
Describe, in the detail, how you would position the PATIENT for a SKYLINE projection of the knee (supero-inferior)
1. The patient sits on the x-ray couch with affected knee flexed over the edge.
2. If possible the knee should be flexed to 45 degrees.
3. Patient to lean back whilst keeping affected knee still to avoid primary beam.
4. The IR should be at the level of the inferior border of the tibial tuberosity
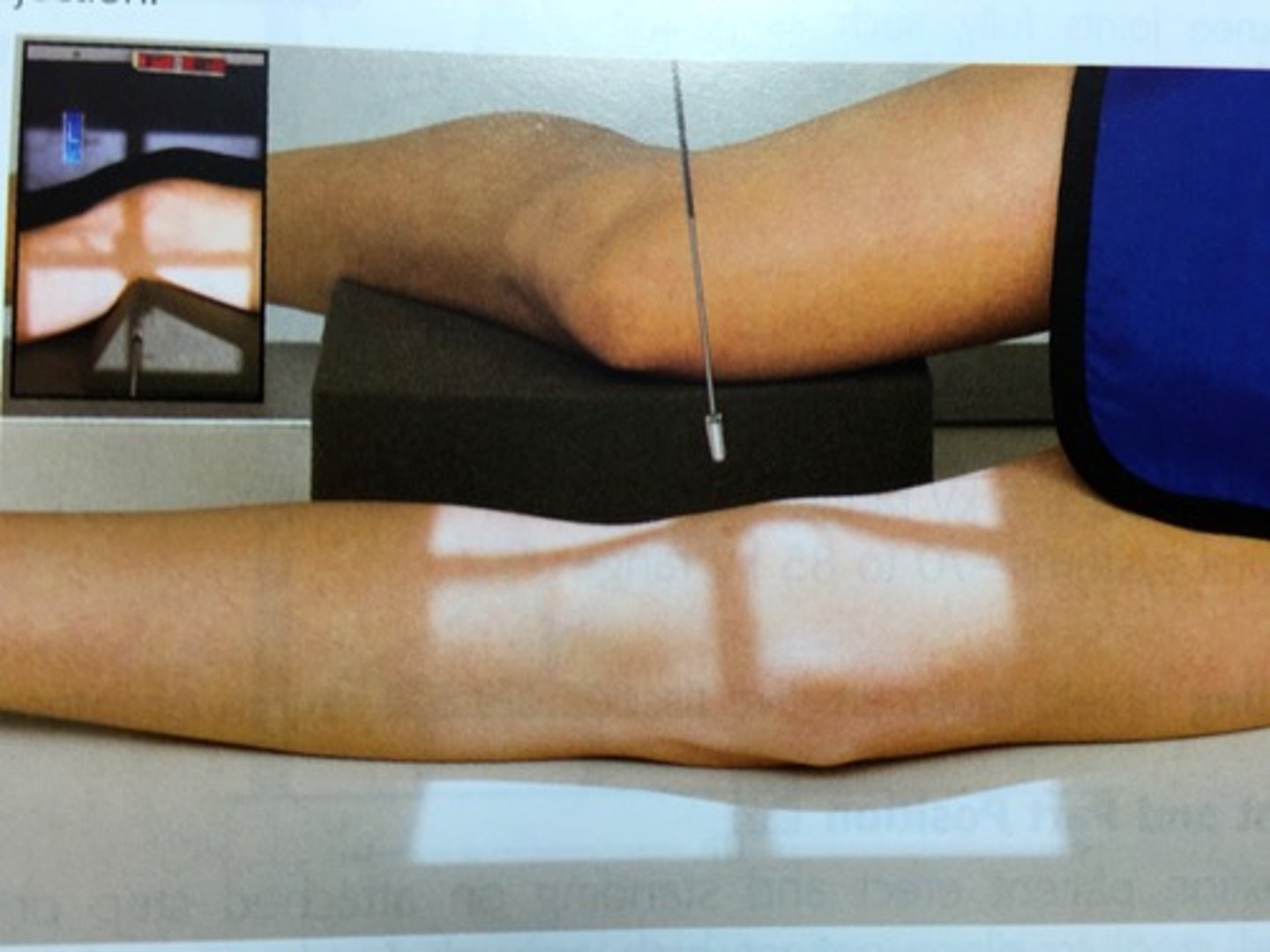
Describe, in the detail, how you would position the PATIENT for a SKYLINE projection of the knee (infero-superior prone)
▪ Patient lies prone.
▪ The IR can either be directly under the knee or in this case within the bucky (not using grid/AEC)
▪ Knee is flexed through 90 degrees.
How should you position the X-RAY TUBE for a infero-superior prone SKYLINE KNEE projection?
SID
Central ray
Centring point
SID: 115cm
Central ray: angled 15 degrees towards the knee (avoiding the toes)
Centring point: behind the patella
When imaging the knee, the rosenberg projection is often useful to perform in some cases. Explain why.
- this projection is more sensitive & specific for the actual knee joint space
- therefore it is useful for the assessment of knees with early degenerative changes.
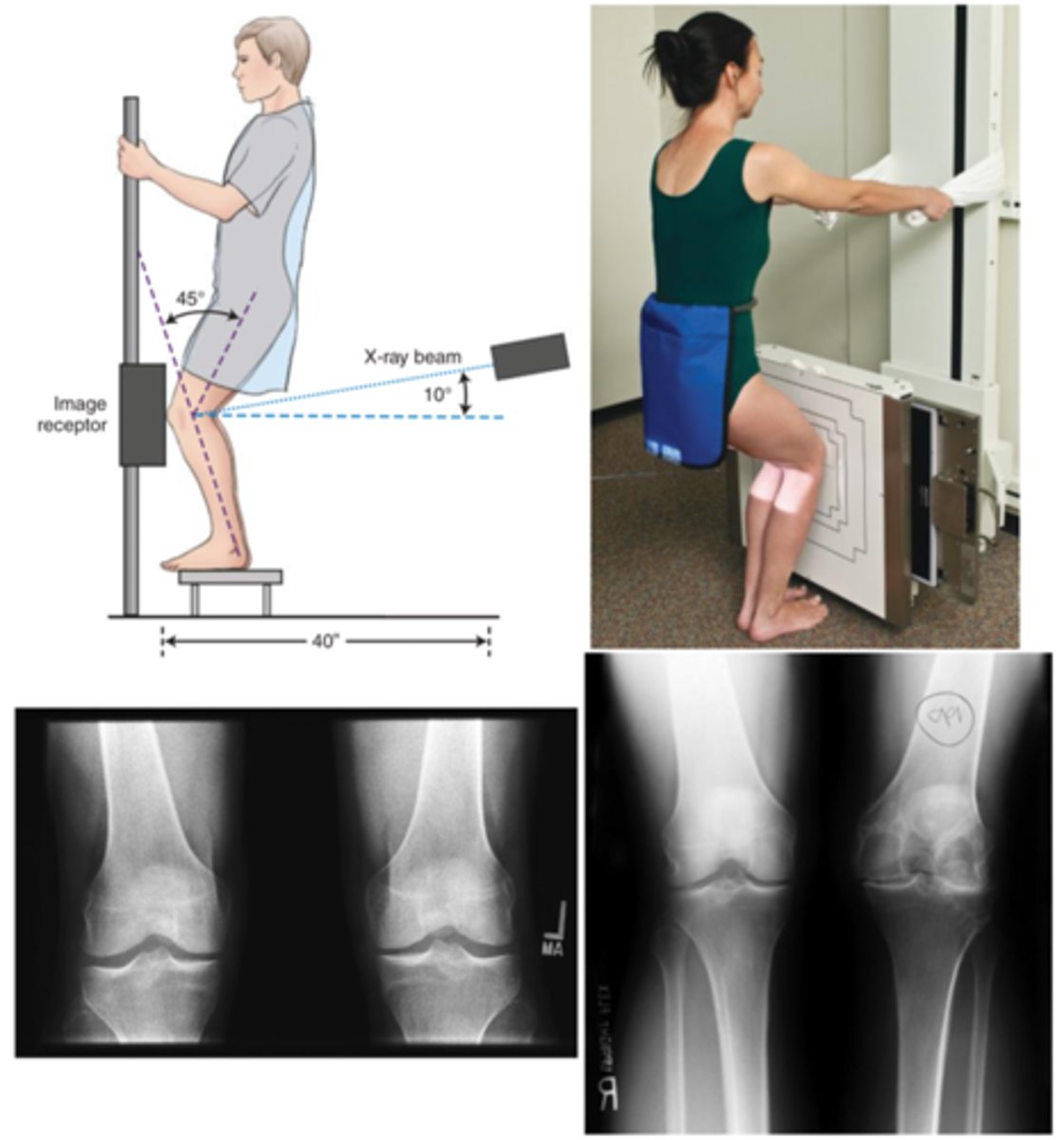
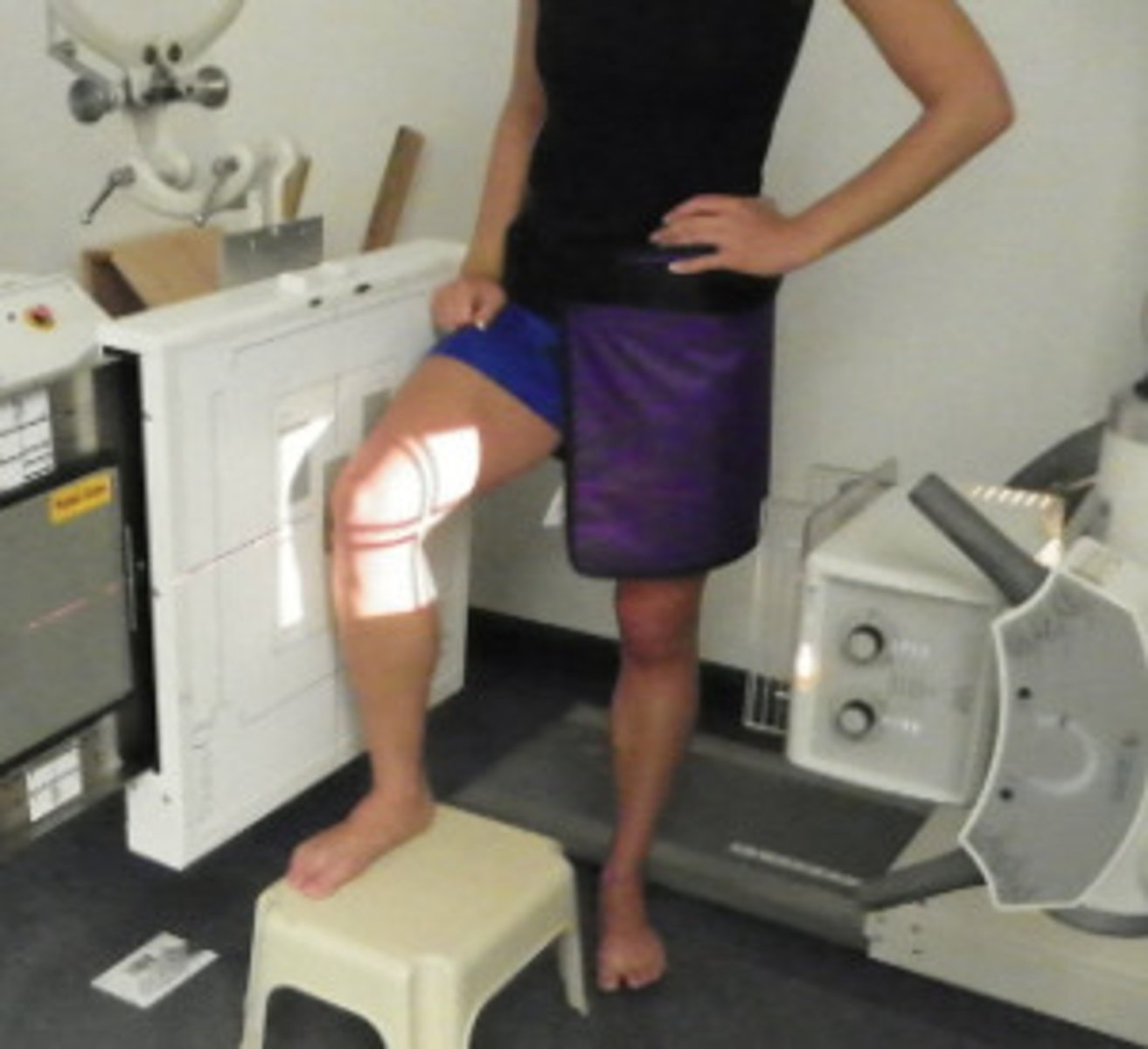
Describe, in detail, how a PATIENT should be positioned for a ROSENBERG KNEE projection.
1. The patient is weight-bearing in a PA position; patient to stand on a stool against the bucky.
2. Tibia should be touching & parallel with the IR.
3. Rotate lower leg to ensure centralisation of the patella.
4. Patient to hold the bucky column and then sit/squat back. Encourage weight distribution to the joint being imaged.

How should we position the X-RAY TUBE when doing a rosenberg projection of the KNEE?
SID
Central ray
Centring point
SID: 100 - 110cm
Central ray: 10 degree cranial angle
Centring point: 1.5cm distal to the apex of the patella
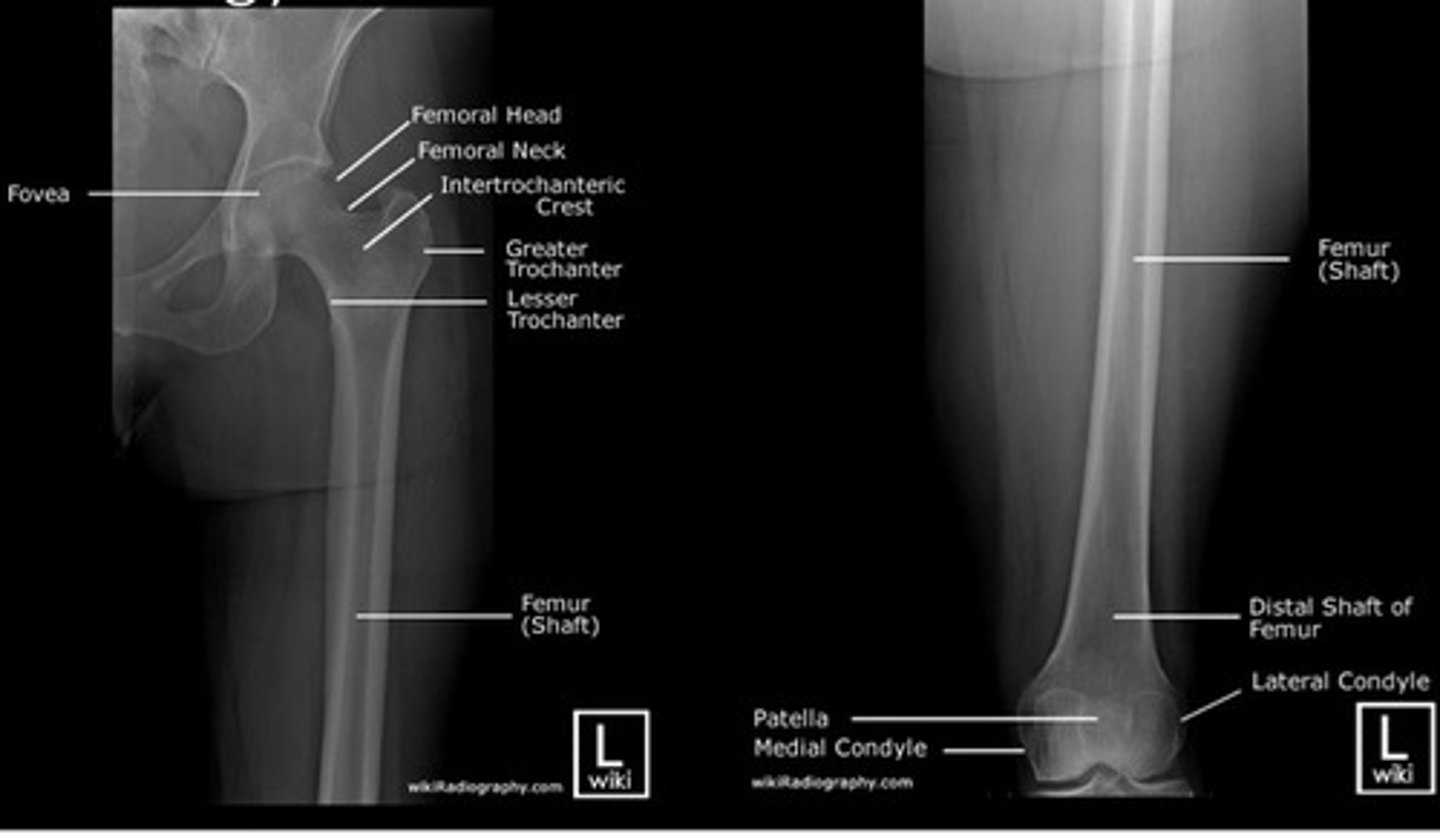
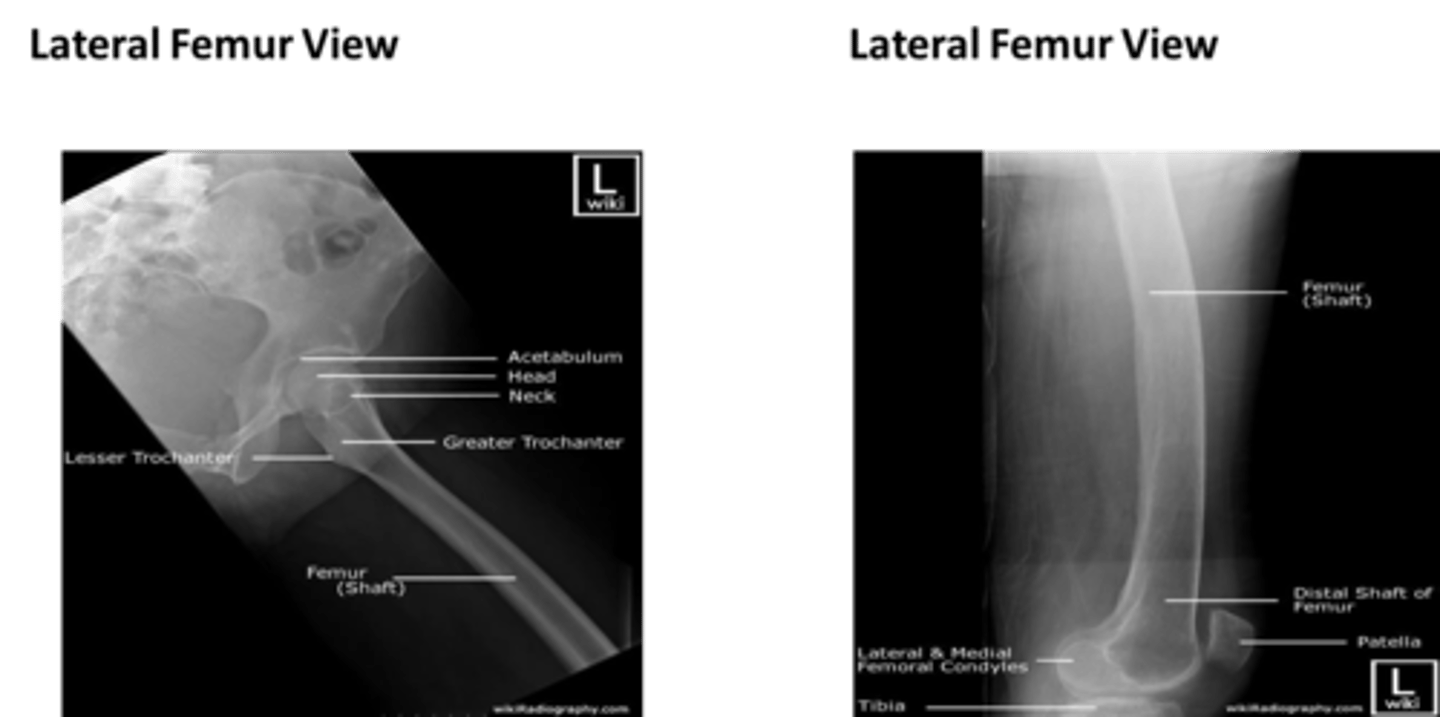
What are the main basic projections for imaging of the FEMUR?
- Antero-posterior (AP)
- Lateral
What are appropriate clinical indications for plain radiography of the femur?
- Trauma
- Pain
- Arthritis (Rheumatoid & Osteoarthritis)
- Foreign body
When imaging the FEMUR, should the image receptor be in a portrait or landscape position?
PORTRAIT (vertically)
When imaging the FEMUR, if you cannot get both the knee and hip joint on one image receptor what should you do?
- take TWO images; One from the hip down and one from the knee up (like a jigsaw puzzle)
For most adults we would use a grid for a FEMUR examination. Why and how?
- When imaging the femur, the image will need to include the hip joint (and the knee joint).
- the hip is generally a lot thicker & denser meaning that it may produce a lot of scatter radiation
- therefore, a GRID is needed when imaging the femur from the hip down due to the thick tissue density (of the hip)
(the denser the body part, the more scatter radiation will be produced; if the body part is > 10cm thick then a grid needs to be used).
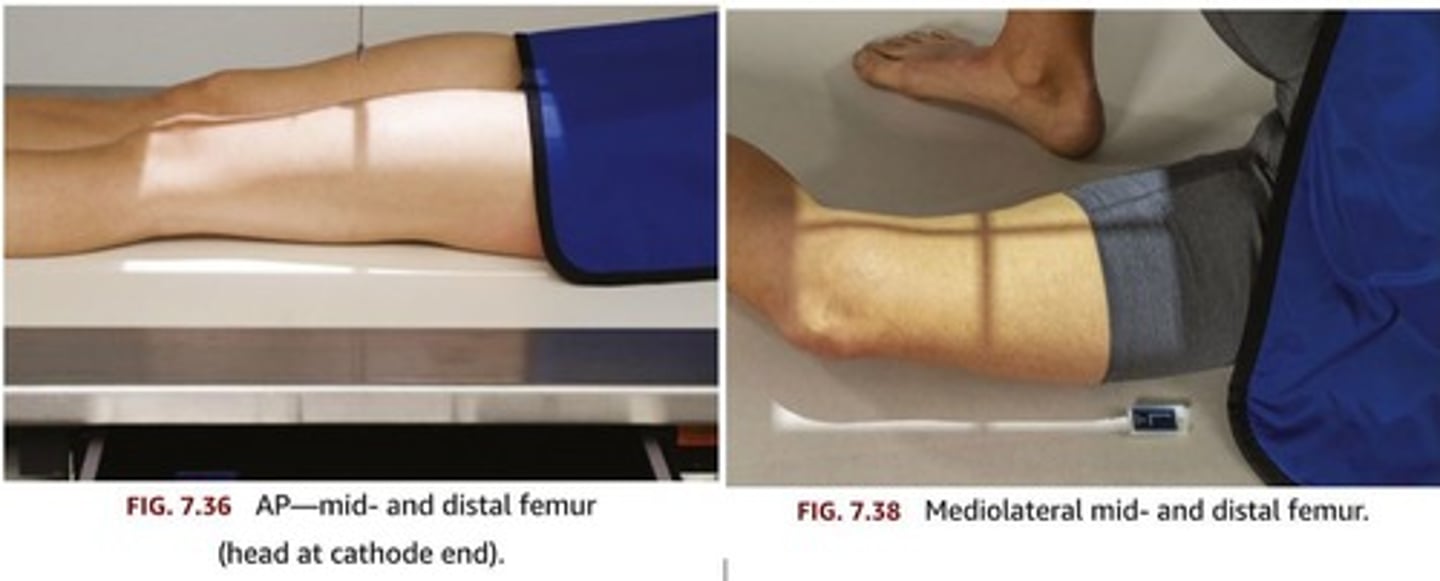
Describe, in detail, how a PATIENT should be positioned for an AP FEMUR projection.
1. Patient lies supine on the x-ray couch and the legs are extended.
2. Posterior aspect of the leg is in contact with the x-ray couch.
3. The IR is placed in the bucky. Make sure that the x-ray tube is locked in with the bucky system.
4. The leg is medially rotated to centralise the patella. The condyles should be equidistant to the IR.
If it is not possible to get both the hip and knee joint on the same IR, then this exposure should be hip down and then a second IR to do an 'out of bucky' knee up exposure.
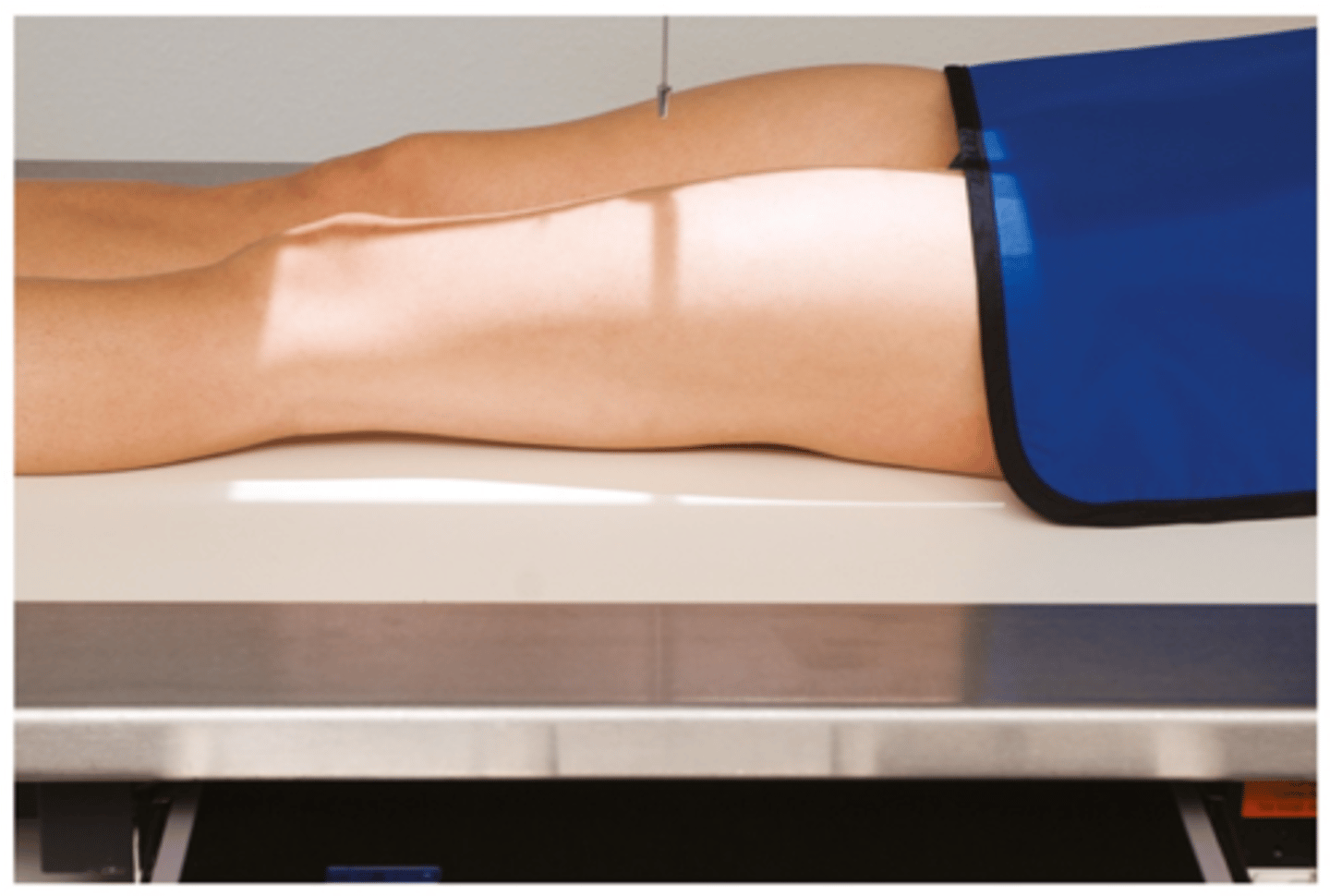
How should we position the X-RAY TUBE when doing an AP FEMUR projection?
SID
Central ray
Centring point
SID: 100 - 115cm
Central ray: perpendicular to the IR
Centring point: midline of the femur, midway between knee & hip joint.

How should we COLLIMATE when doing an AP FEMUR projection? What structures should be included in the image?
- to include the entire length of the femur and soft tissue borders. The knee and hip joint must be included.
Describe, in detail, how we should position the PATIENT when doing a LATERAL FEMUR projection.
1. Patient is turned onto the affected side, lateral aspect of the leg in contact with the IR.
2. Femur oriented diagonally across an IR if 'out of bucky'.
3. Knee joint flexed and condyles should be superimposed.
4. Pelvis rotated backwards to separate the thighs.
5. Hip down image on second IR in bucky (if not possible to get both joints on one IR)

How should we position the X-RAY TUBE when doing a LATERAL FEMUR projection?
SID
Central ray
Centring point
SID: 110 - 115cm
Central ray: 90 degrees to the IR
Centring point: midline of the thigh; midway between the hip & knee joint.
How should we COLLIMATE when doing a LATERAL FEMUR projection? What structures should be included in the image?
- to include the entire length of the femur and lateral soft tissue borders. The knee and hip joint must also be included.
State the criteria for assessing the radiographs of the knee, femur, tibia & fibula.
• Correct name and identification.
• Correct and original anatomical aspect markers in the primary beam.
• Good contrast and density.
• Evidence of collimation.
• No patient or IR artefacts.
• No movement unsharpness.
• Any pathology evident?
• Do you need to repeat any projections?
• Do you need to perform any further projections?